Abstract
Objective
Despite successes in efforts to integrate HIV testing into routine care in emergency departments, challenges remain. Kiosk-facilitated, directed HIV self-testing offers one novel approach to address logistical challenges.
Methods
Emergency department patients, 18–64 years, were recruited to evaluate use of tablet-based-kiosks to guide patients to conduct their own point-of-care HIV tests followed by standard-of-care HIV tests by healthcare workers. Both tests were OraQuick Advance tests.
Results
Of 955 patients approached, 473 (49.5%) consented; 467 completed the test, and 100% had concordant results with healthcare workers. Median age was 41 years, 59.6% were female, 74.8% were African-American, and 19.6% were White. In all, 99.8% of patients believed the self-test was “definitely” or “probably” correct; 91.7% of patients “trusted their results very much”; 99.8% reported “overall” self-testing was “easy or somewhat easy” to perform. Further, 96.9% indicated they would “probably” or “definitely” test themselves at home were the HIV test available for purchase; 25.9% preferred self-testing versus 34.4% who preferred healthcare professional testing (p > 0.05).
Conclusion
Tablet-based kiosk testing proved to be highly feasible, acceptable, and an accurate method of conducting rapid HIV self-testing in this study; however, rates of engagement were moderate. More research will be required to ascertain barriers to increased engagement for self-testing.
Keywords: Human immunodeficiency virus, screening
Introduction
In 2012, the Centers for Disease Control and Prevention (CDC) reported that the estimated incidence of HIV had remained relatively constant between 2008 and 2010, with approximately 50,000 new HIV infections per year.1 Unfortunately, of the approximately 1.1 million infected individuals in the United States, approximately 20% remain unaware of their HIV infection.2 These persons remain at high risk for unknowingly transmitting the infection to their sex partners. Blacks/African Americans continue to have the highest rate of new infections, accounting for 44% of new infections overall, at a rate of 68.9/100,000 population, 7.9 times higher than the rate observed in Whites (8.7/100,000).1 Particularly at risk are men who have sex with men (MSM), with rates of new infections in that group increasing 12% between 2008 and 2010.1 In response, the CDC has recommended increasingly intensive national screening guidelines, recommending that HIV tests should be performed annually on all men and women between the ages of 13 and 64 years.3,4
The newest 2006 CDC guidelines, which advocate routine HIV testing in all healthcare settings, provide explicit recognition of the importance of emergency departments (EDs) as EDs represent one of the most common sites of missed opportunity for identifying patients with unrecognized HIV infection.4,5 A large number of studies reporting implementation of HIV screening guidelines in EDs have since been reported; practically speaking, however, rates of testing penetration in EDs have fallen short of recommendations, with most ED programs testing less than 10% of all ED patients. Data from prior studies have shown that, when routine screening programs are implemented in EDs, only about 10% of the total ED population is generally tested.6,7
New approaches for addressing the practical challenge of increasing rates of tests offered without increasing burden on indigenous staff are required; such methods should be adapted to the practice reality and limited resources of busy episodic ED healthcare settings. We hypothesized that offering patients the opportunity to conduct HIV self-testing might offer one practical solution. Previous formative studies from our group have shown that HIV self-testing was highly acceptable and feasible, when patients were offered the option to conduct self-testing.8,9 In this study, we aimed to determine whether incorporation of a tablet-based kiosk, which could streamline the self-testing process by providing instructions to patients on the process of self-testing and allowing a mechanism for patients to self-enter demographic information, would be feasible and acceptable to patients and would yield accurate test results relative to testing performed by a healthcare worker (HCW).
Methods
Setting
The Johns Hopkins Hospital ED is an inner-city ED, with 60,000 visits/year; the population is socioeconomically disadvantaged, with greater than 75% African Americans.
Study design and participants
From February 2012 to August 2012, all patients aged 18–64 years who met our inclusion criteria for participation for our voluntary HIV testing program were approached for consent to participate in a study evaluating feasibility, accuracy, and acceptability of HIV self-testing in the ED. Patients were eligible if they were not in extremis, were able to provide informed consent, did not have a previous HIV diagnosis, and had not been tested in the previous 6 months. The Institutional Review Board of Johns Hopkins University approved the study, with written consent required for participation.
HIV test and procedure
The platform used for self-testing was the oral fluid OraQuick Advance HIV1/2 test (OraSure, Bethlehem, PA) point-of-care test (POCT). This same test is used in the ED for standard-of-care (SOC) HIV testing routinely. The HCW testing facilitator and the research assistant (RA) approached eligible patients in the ED. The HCW testing facilitator first ascertained patient’s interest in receiving an HIV test; for those who were interested the HCW testing facilitator explained that a research study was being done to explore the feasibility, acceptability, and accuracy of self-testing in the ED. For those patients who expressed interest in participating, the RA explained that the self-test was identical to the SOC test, with the only difference being that the patient themselves would perform the test. Those patients who declined participation in the study received an SOC HIV test. For those patients who expressed interest in participating in the study, the RA explained the purpose and details of the study, confirmed that the patient understood the procedures associated with participation, and obtained the patient’s written consent for participation.
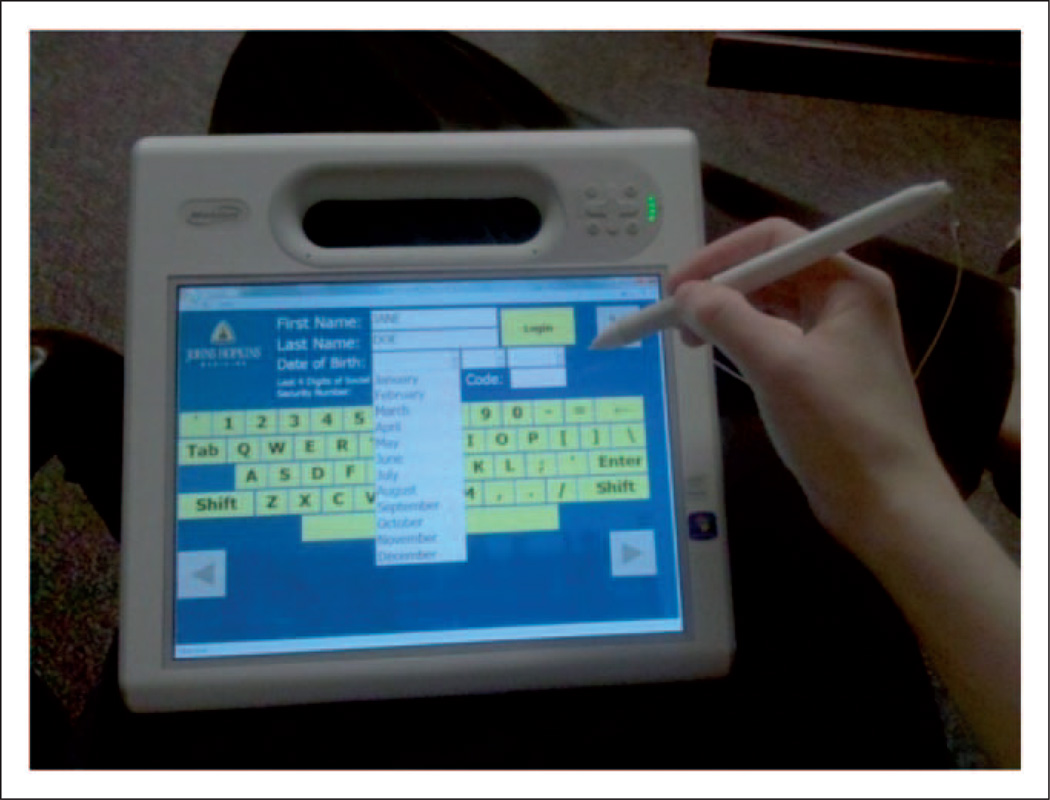
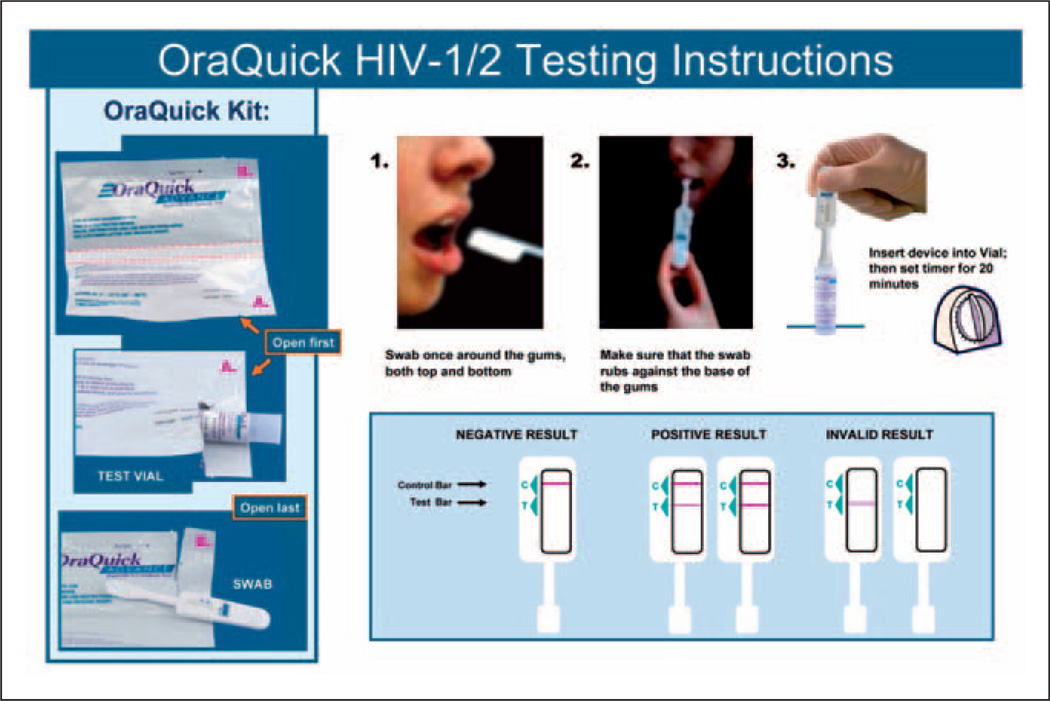
Consented patients were then given a mobile touch-screen tablet-based kiosk by the RA (Figure 1). Participating patients were then asked to follow the directions on the kiosk which included entering his/her demographics (i.e. gender, age, race, insurance status, level of education) and previous preventive screening experiences, on the touch-screen computer kiosk tablet. The tablet-based kiosk provided a 3-screen overview of the self-testing process. Patient’s were then given a large plasticized card as an easy-to-read visual aid with simple step-by-step directions and diagrams for performance of self-testing (including how to collect oral fluid, how to transfer the oral swab to the test vial, time to wait to read test results) and how to interpret test (with visual examples of positive and negative results) (Figure 2). Patients’ interpretations of results were recorded by the RA. A short questionnaire was then administered by the RA to assess patient’s satisfaction with the self-testing process and perceptions about results.
Figure 1.
Mobile tablet-based kiosk.
Figure 2.
HIV oral HIV self-test instructions.
After the self-testing was completed, the HCW testing facilitator performed a standard of care POC HIV test, similar to what is done for any patient who receives an HIV test in the ED. The SOC HIV results were made available (in 20 minutes), as per usual SOC testing protocol. In case of any discrepant results between the two HIV tests, the SOC test was recorded in the patient’s chart. If there was a result that was self-test positive and SOC negative, a follow-up Western Blot HIV test was performed for definitive resulting.
Methods of measurement, test performance, and data collection
The primary outcome was patients’ perception of the HIV self-testing as assessed by the structured questionnaire administered by the RA. Perception included patient’s rating of acceptability of performing the test by themselves, the patient’s perception of confidence in the sample collection process and result reported, as well as patient’s overall satisfaction with performing their own test. A Likert scale format was used to grade responses. The secondary outcome was the rate of agreement between self-test results compared to the HCW-performed test. The questionnaire also included assessment of patient’s willingness to purchase the test, based on the possibility (at the time this study was conducted) that the test might soon be made available for purchase over-the-counter (OTC). For the self-test, the participant obtained his/her own sample, performed the test, and interpreted the results without instruction from the self-test study facilitator. The RA observed the performance of the self-test and recorded instances in which difficulties were encountered by patients (e.g. opening the test package).
Primary data analysis
Questionnaire results and observational information were recorded in an SPSS database. Data analysis was performed by SAS, version 9.1 (SAS Institute Inc., Cary, NC).
Results
Of 955 patients approached to participate in the study, 473 (49.5%) consented to participate in the HIV self-testing study. Of those 473, 467 (98.4%) completed the test. Three persons left the ED before completion of the test. The median age of the patients was 41 years, and 59.6% were female, 74.8% were African American, and 19.6% were White. Of patients performing a self-test, 100% had concordant results with those obtained by healthcare professionals. Only one newly diagnosed HIV infection was identified in a 48-year-old woman.
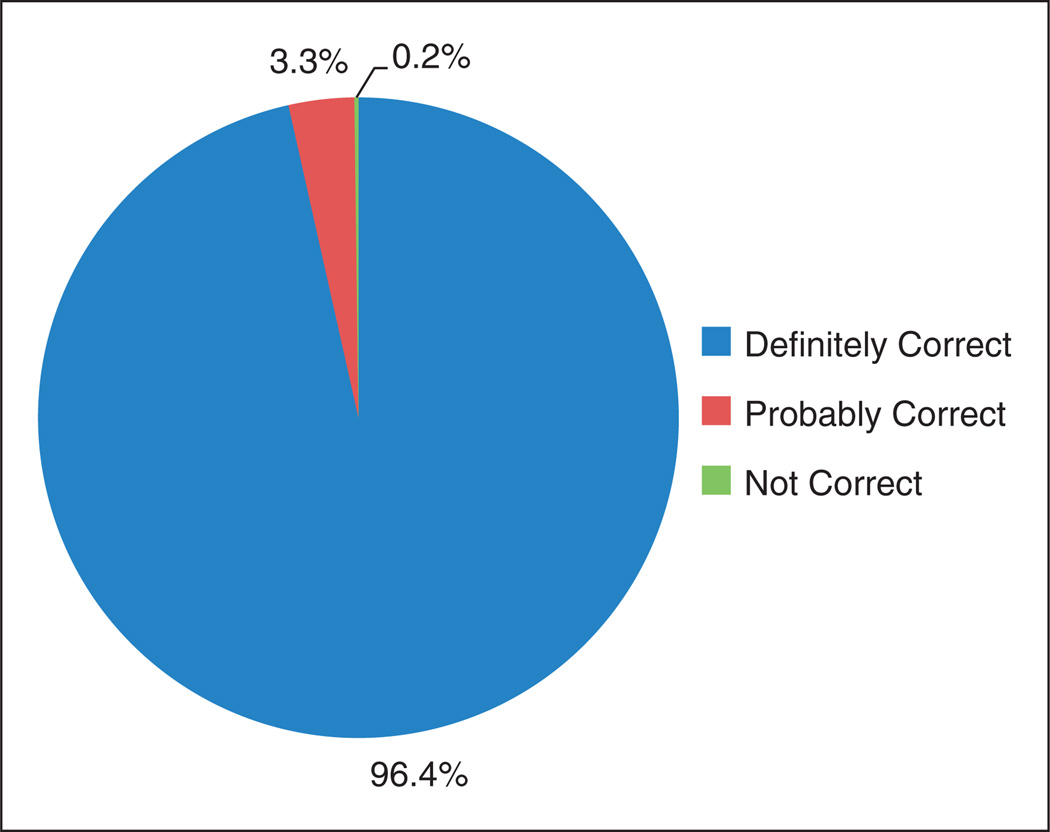
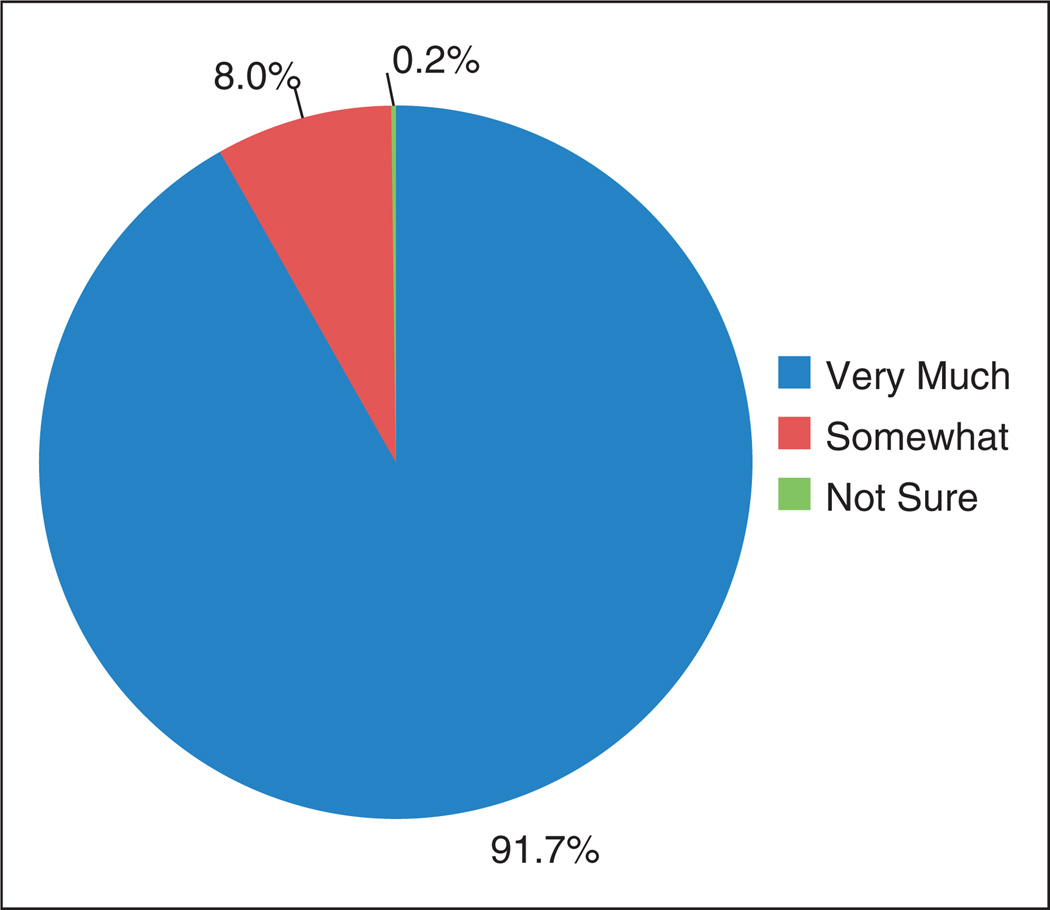
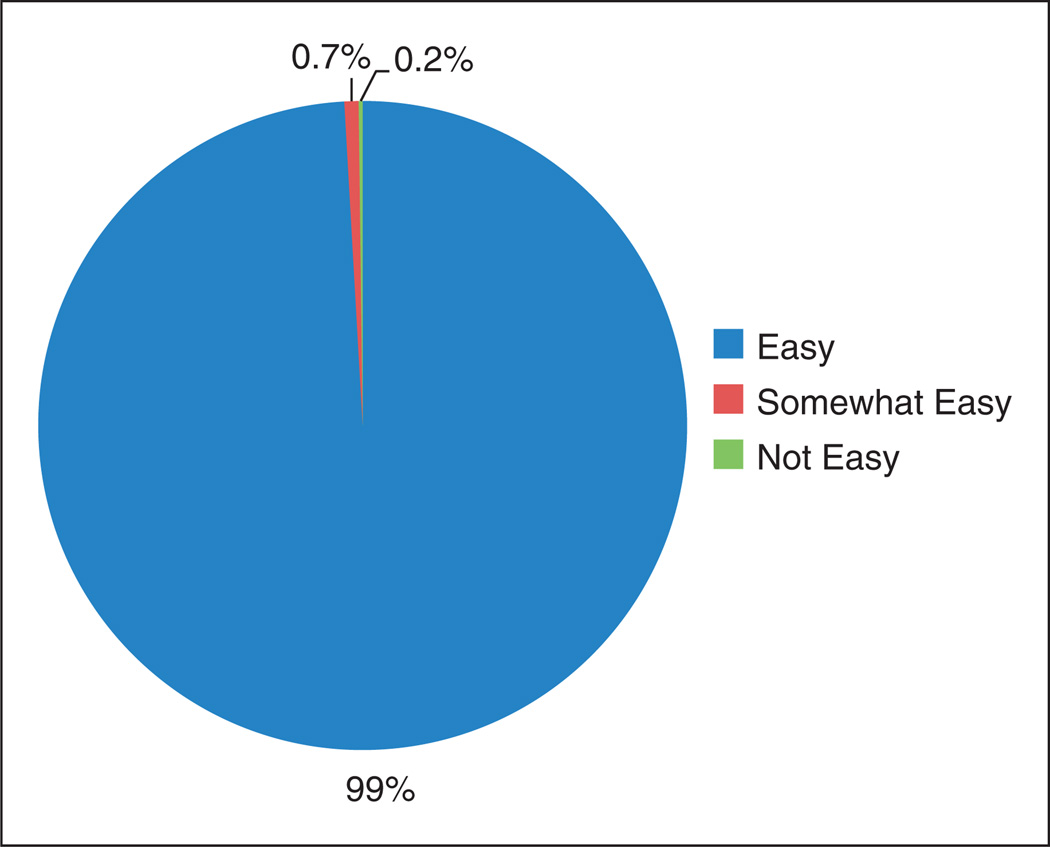
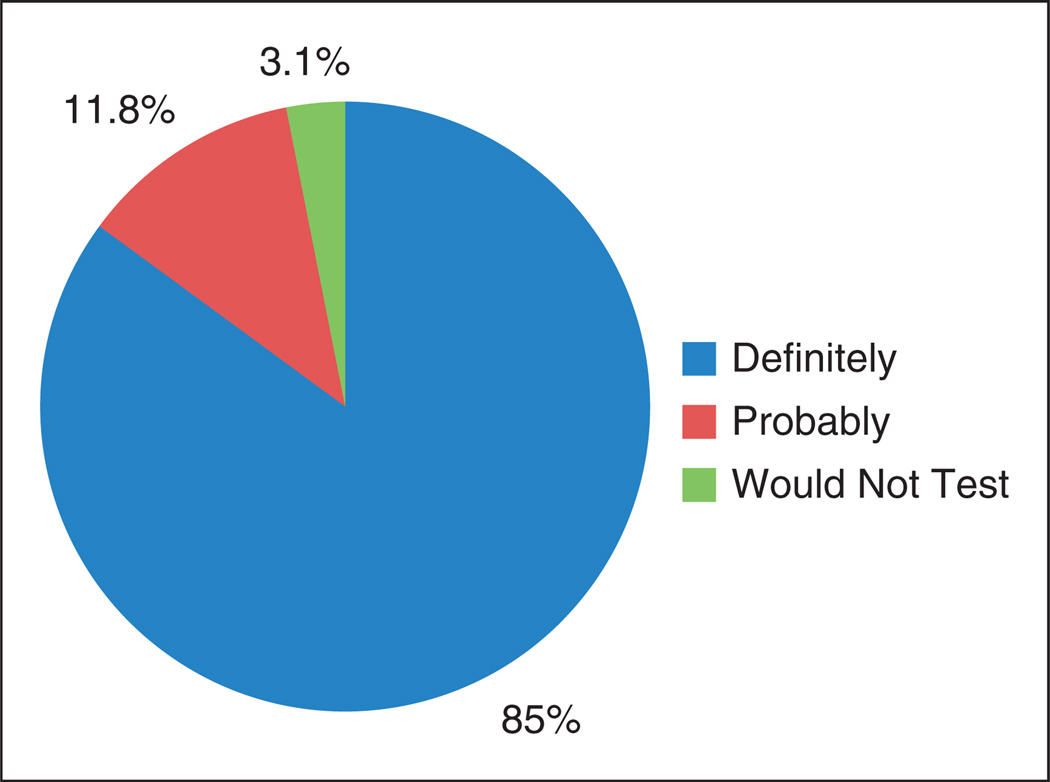
From the questionnaire data, 99.8% of patients reported that they believed that the POC self-test was “definitely” or “probably” correct, and 91.7% of patients indicated they “trusted their results very much” (Figures 3 and 4). Interestingly, 99.8% reported that “overall” it was “easy or somewhat easy” to perform the test. Of patients, 96.9% reported they would “probably” or “definitely” test themselves at home if the rapid HIV test were available OTC for purchase (Figures 5 and 6). Approximately 33% of patients answered that they would pay up to a maximum of $10 for the test, whereas only 32% stated they would pay up to a maximum of $30.
Figure 3.
Results about self-testing among participants recruited in the emergency room who were asked “Do you believe that the rapid HIV test result was correct for the sample that you collected?”.
Figure 4.
Results about self-testing among participants recruited in the emergency room who were asked “How much do you trust the result of the rapid HIV test that you collected?”.
Figure 5.
Results about self-testing among participants recruited in the emergency room who were asked “How easy was it for you to follow the instruction placard?”.
Figure 6.
Results about self-testing among participants recruited in the emergency room who were asked “Would you test yourself at home for HIV if the rapid HIV test were available over-the-counter (OTC)?”.
Overall, 25.9% of patients preferred self-testing for HIV and 34.4% preferred that a healthcare professional perform the HIV test (p > 0.05). The remaining patients answered “Either/No Preference.” Regarding preferred location for self-testing, 26.1% stated they would prefer self-testing at home and 32.8% indicated they would prefer performing the test in a clinic or an ED (p > 0.05).
Discussion
Innovative approaches to offering and providing HIV testing are needed, since approximately 20% of HIV-infected persons in the United States do not currently know their status, and current data supports value of early detection and diagnosis as a means to expedite early linkage into care and treatment. While EDs are widely recognized as a critical venue to provide HIV testing, significant logistical challenges remain, principally related to the practical limitation of already overburdened staff and resources.10 The use of the kiosk and HIV self-testing potentially can be cost saving, as it could save staff time needed to interact with patients to collect demographics and for performance of the test itself.
We observed that a significant proportion of patients in this ED (nearly 50%) were willing to use a tablet-based kiosk to guide them through HIV self-testing. Further patients reported an overall positive experience with the kiosk. The majority of the patients who self-tested believed their results were correct, reported that they trusted the test, and indicated that test samples were easy to collect and test results easy to read. Patients’ results were 100% concordant with those obtained by the RAs. Most stated they would test themselves at home if an OTC were available. Taken together, these data suggest fairly high acceptability of HIV self-testing in the ED setting as a potential method to get more persons tested, with less staff time required. Notably, however, overall rates of engagement were only moderate suggesting that many patients may prefer to have the clinicians conduct their test.
Our findings are consistent with results reported in previous studies conducted for HIV self-testing using POC tests in our ED setting, but without kiosk recruitment, where self-testing was acceptable, results were trusted, and results were accurate.8, Recently, Haukoos et al.10 reported that kiosks can be used in ED settings to offer and obtain consent for HIV screening. Challenges with regard to patient comprehension of opt-out consent were identified with that approach, however, suggesting additional research is required before kiosks can fully replace healthcare staff, at least for certain elements of the HIV-testing process.10 Further, full operational methods for implementing kiosk and self-testing into busy EDs will be challenging and requires additional evaluation of optimal methods and costs relative to existing models of testing.11,12
There are multiple limitations associated with this study. Since the offer for self-testing was done in the context of a research study, with consent, the findings may not reflect what would happen in a real-world operational program (potential enrollment biases). Rates of assistance by the research staff were not systematically collected and may not reflect a model in which no staff are available to assist. Further, the kiosk system was not fully integrated into ED flow and reporting results to clinicians; as extensive information technology and operational interfacing would be required to implement such changes. A further limitation of our study is the reproducibility of the 100% concordance observed here, which may change based on higher rates of positivity than those observed here. Additionally, given that patients who agreed to self-testing in the context of the study also underwent another test by the healthcare professional, willingness to perform self-testing observed here may not translate to willingness to perform the test at home, in a setting without access to HCWs for counseling and confirmatory testing. Finally, these results may not be generalizable to other ED populations or ED settings, which are dissimilar to ours.
More research will be required to learn how to overcome barriers to increase rates of engagement for HIV testing in EDs, as well as to determine the practical value of more widespread kiosk-facilitated HIV testing in the ED. In conclusion, this report of tablet-based kiosk-facilitated HIV self-testing could serve as a model for patient-directed HIV screening programs in acute care settings. Kiosks could also be adapted for other public health initiatives in both acute and routine clinical care venues, such as screening for sexually transmitted infections.
Acknowledgments
Funding
This study was supported by NIBIB, NIH U54EB007958; NIAID, NIH U01-068613.
Footnotes
Conflict of Interest
None declared.
References
- 1.Centers for Disease Control and Prevention. HIV Surveillance Report: Estimated HIV incidence in the United States, 2007–2010. HIV Surv Suppl Rep. 2012;17:1–26. [Google Scholar]
- 2.Hall H, Song R, hodes P, et al. Estimation of HIV incidence in the United States. JAMA. 2008;300:520–529. doi: 10.1001/jama.300.5.520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. Revised recommendations for HIV counseling, testing, and referral. MMWR. 2001;50:1–62. [Google Scholar]
- 4.Branson B, Handsfield H, Lampe M, et al. Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health-care settings. MMWR Recomm Rep. 2006;55:1–17. [PubMed] [Google Scholar]
- 5.Ehrenkranz PD, Ahn CJ, lay JP, et al. Availability of rapid human immunodeficiency virus testing in academic emergency departments. Acad Emerg Med. 2008;15:144–150. doi: 10.1111/j.1553-2712.2008.00028.x. [DOI] [PubMed] [Google Scholar]
- 6.Kelen GD, Rothman R. Emergency department-based HIV testing: too little, but not too late. Ann Emerg Med. 2009;54:65–71. doi: 10.1016/j.annemergmed.2009.03.027. [DOI] [PubMed] [Google Scholar]
- 7.White DE, Scribner AN, Schulden JD, et al. Results of a rapid HIV screening and diagnostic testing program in an urban emergency department. Ann Emerg Med. 2009;54:56–64. doi: 10.1016/j.annemergmed.2008.09.027. [DOI] [PubMed] [Google Scholar]
- 8.Gaydos CA, Hsieh Y-H, Harvey L, et al. Will patients “Opt-In” to perform their own rapid HIV test in the emergency department? Ann Emerg Med. 2011;58:S74–S78. doi: 10.1016/j.annemergmed.2011.03.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nour S, Hsieh Y-H, Jett-Goheen M, et al. Patients can accurately perform their own rapid HIV point-of-care test in the emergency department. Point Care J. 2012;11:176–179. doi: 10.1097/POC.0b013e3182666eb7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Haukoos J, Hopkins E, Bender B, et al. Use of kiosks and patient understanding of opt-out and opt-in consent for routine rapid human immunodeficiency virus screening in the emergency department. Acad Emerg Med. 2012;19:287–293. doi: 10.1111/j.1553-2712.2012.01290.x. [DOI] [PubMed] [Google Scholar]
- 11.Hsieh Y-H, Jung J, Shahan J, et al. Outcomes and cost analysis of three operational models for rapid HIV testing services in an academic inner-city emergency department. Ann Emerg Med. 2011;58:S133–S139. doi: 10.1016/j.annemergmed.2011.03.037. [DOI] [PubMed] [Google Scholar]
- 12.Haukoos JS, White DA, Lyons MS, et al. National Emergency Department HIV Testing Consortium. Operational methods of HIV testing in emergency departments: a systematic review. Ann Emerg Med. 2011;58:S96–S103. doi: 10.1016/j.annemergmed.2011.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]