Abstract
Background
Acetabular protrusio is an uncommon finding in hip arthritis. Several reconstructive approaches have been used; however the best approach remains undefined.
Questions/purposes
Our purposes in this study were to (1) describe the THA survivorship for protrusio as a function of the acetabular component, (2) evaluate survivorship of the cup as a function of restoration of radiographic hip mechanics and offset, and (3) report the long-term clinical results.
Methods
One hundred twenty-seven patients (162 hips) undergoing primary THA with acetabular protrusio were retrospectively reviewed. The mean age of the patients at surgery was 66 ± 13 years, and the mean followup was 10 ± 6 years (range, 2–25 years).The cup fixation was uncemented in 107 (83 with bone graft) and cemented in 55 hips (14 with bone graft). Preoperative and postoperative radiographs were reviewed for restoration of hip mechanics and offset.
Results
The THA survival from aseptic cup revision at 15 years was 89% (95% CI, 75%–96%) for uncemented compared with 85% (95% CI, 68%–94%) for cemented cups. The risk of aseptic cup revision significantly increased by 24% (hazards ratio, 1.24; 95% CI, 1.02–1.5) for every 1 mm medial or lateral distance away from the native hip center of rotation to the prosthetic head center. Harris hip scores were improved by mean of 27 ± 20 points (n = 123) with a higher postoperative score for uncemented bone grafted compared with solely cemented cups (81 ± 16 versus 71 ± 20 points).
Conclusions
Restoring hip center of rotation using an uncemented cup with or without bone graft was associated with increased durability in our series. There was a 24% increase in the risk of aseptic cup revision for every 1 mm medial or lateral distance away from the native hip center to the prosthetic head center.
Level of Evidence
Level III, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Acetabular protrusio, also known as arthrokatadysis or Otto pelvis, was first described by the German pathologist Otto in 1824 according to Dunlop et al. [5] and Pomeranz [14]. It is a relatively rare radiographic finding but has been associated with multiple etiologies, most commonly inflammatory arthritis, and also is seen in patients undergoing THA for end-stage osteoarthritis. Radiographically, acetabular protrusio is present when the medial aspect of the femoral head lies medial to the ilioischial line on the AP pelvic radiograph. Armbuster et al. [1] and Guerra et al. [7] reviewed more than 300 pelvic radiographs and defined protrusio as the medial aspect of the head past the ilioischial line greater than 6 mm in females and 3 mm in males.
In cases of acetabular protrusio and end-stage arthritis, THA is the preferred surgical treatment. Studies have shown satisfactory outcomes at midterm in this patient population [6, 11, 15, 18]. As with other potential causes leading to arthritis, the aim of THA is to restore function and improve pain while restoring hip mechanics and abductor function. Higher loosening and revision rates for femoral stems and cups have been reported when cemented cups are placed superior or lateral to the anatomic position [13, 23]. This may not be the case with uncemented THAs [4, 17]. Schutzer and Harris [17] reported results of superiorly placed uncemented cups, and this mixed group of primary and revision THAs did not show an increased failure rate; at a mean followup of 3.3 years (range, 2–5.3 years), there was no cup revision for loosening in their series. They suggested that superior placement of an uncemented cup did not seem to negatively affect the outcome of acetabular reconstruction provided that the component was not lateralized.
The results of THA in patients with acetabular protrusio warrant further study. Specifically, the fate of the cup at long term as a function of its position at the time of implantation has not been reported to our knowledge. The aims of our study were to (1) describe the THA survivorship for protrusio as a function of the acetabular component, (2) evaluate the survivorship of the cup as a function of restoration of radiographic hip mechanics and offset, and (3) report the long-term clinical results.
Patients and Methods
This study was approved by the institutional review board at Mayo Clinic. All patients with an associated diagnosis of protrusio acetabuli undergoing primary THA between 1973 and 2009 were identified from the institutional registry [2]. We identified 206 hips in 155 patients with this diagnosis. We excluded patients who did not have a minimum of 2 years clinical followup (11 hips), hips with missing preoperative (12 hips) or intraoperative radiographs (one hip), hips in which the head did not protrude past the ilioischial line on preoperative radiographs (14 hips), bipolar and ringed acetabular components used at the time of THA (four hips), or hips that were revised for deep infection (two hips).
The final cohort consisted of 127 patients (162 hips) including 112 female patients who underwent primary THA. We confirmed the diagnosis, defining protrusio acetabuli as a hip in which the medial aspect of the femoral head was medial to the ilioischial line of Kohler.
The cup was an all-polyethylene cemented in 55 hips. Of these hips, 14 had acetabular reconstruction with concomitant bone graft. In the remaining 107 hips, the cups were uncemented; 83 of these hips required concomitant bone graft for acetabular reconstruction. All grafts except one were autograft femoral heads. Cemented fixation was performed mostly until the mid-1980s, while uncemented fixation performed mostly in late 2000s. The femur stem was cemented in 122 hips, whereas uncemented stems were inserted in the 40 remaining hips.
The femoral head protruded on average 7 ± 5 mm (range, 1 – 30 mm). The mean age of the patients at the time of arthroplasty was 66 ± 13 years (range, 17–89 years). The minimum followup was 2 years, with a mean of 10 ± 6 years (range, 2–25 years). The most common etiology of protrusio acetabuli was idiopathic in 117 hips, whereas 38 hips had an underlying inflammatory component (Table 1).
Table 1.
Patient demographics and outcomes
| Variable | Uncemented reconstruction | Cemented reconstruction | ||
|---|---|---|---|---|
| Using bone graft | No bone graft | Using bone graft | No bone graft | |
| Number of hips | 83 | 24 | 14 | 41 |
| Females (hips) | 93 | 50 | ||
| Age (years)*, (range) | 70 ± 14 (18–89) | 65 ± 12 (17–85) | ||
| Etiology (hips) | Idiopathic (61) Inflammatory (19) Genetic (2) Postinfectious (1) |
Idiopathic (17) Inflammatory (4) Postinfectious (1) Metabolic (1) Postradiation (1) |
Idiopathic (11) Inflammatory (3) |
Idiopathic (28) Inflammatory (12) Metabolic (1) |
| Preoperative HHS* | 52 ± 13 | 49 ± 10 | 45 ± 9 | 52 ± 1 |
| Reported HHS | 59 | 17 | 13 | 35 |
| Number of revised cups | 5 | None | None | 6 |
| Cup revision indications (hips) | Instability (1) | None | None | Aseptic loosening (6) |
| Linear wear and modular exchange (1) | ||||
| Aseptic loosening (3) | ||||
| Cup survival from aseptic revision | ||||
| 10 years¥ | 95 (85–98) | 92 (77–97) | ||
| Cup at risk | 43 | 30 | ||
| 15 years¥ | 89 (75–96) | 85 (68–94) | ||
| Cup at risk | 23 | 16 | ||
| Time (in years) to latest followup* | 9 ± 5 | 8 ± 6 | 11 ± 6 | 12 ± 7 |
| Postoperative HHS* | 81 ± 16 | 77 ± 14 | 74 ± 19 | 71 ± 20 |
| Reported HHS | 78 | 24 | 14 | 40 |
| Change in HHS* | 30 ± 18 | 30 ± 13 | 30 ± 18 | 19 ± 25 |
| Reported HHS | 58 | 17 | 13 | 35 |
| Time (in years) to latest radiographic evaluation* | 9 ± 6 | 7 ± 6 | 4 ± 6 | 9 ± 9 |
| Cups without radiolucent lines (hips) | 60 | 19 | 11 | 21 |
HHS = Harris hip score; * Values expressed as mean ± SD; ¥ Kaplan-Meier estimates with lower and upper 95% CI in parentheses.
Surgical reports were reviewed for details regarding intraoperative hip reconstruction, type of implants used, and whether femoral head autograft or allograft had been used.
A detailed radiographic analysis was conducted of preoperative, intraoperative, and postoperative radiographs until latest followup or failure. Hard-copy radiographs were digitized and analyzed on an in-house computerized radiographic system. Radiographs were calibrated for magnification and all measurements were made by one author (YMB) after proper instruction by the senior author (RJS). Radiographic measurements on preoperative radiographs (Fig. 1) included: (1) distance of the medial aspect of the femoral head to the ilioischial line (protrusio); (2) native hip center of rotation (Ranawat triangle method) [15]; (3) distance of the femoral head center to the native hip center of rotation on X and Y axes; and (4) measurement of femoral offset [3]. Radiographic measurement of postoperative radiographs (< 2 months from surgery) (Fig. 1) included: (1) native hip center of rotation (Ranawat triangle method); (2) distance of the prosthetic femoral head center to the native hip center of rotation on X and Y axes; and (3) measurement of femoral offset. Latest followup radiographs were assessed for (1) bone graft incorporation to the surrounding native acetabular floor [22] if used; and (2) evidence of radiographic loosening of the cup according to Hodgkinson et al. [9] for cemented cups and Udomkiat et al. [20] for uncemented cups.
Fig. 1A–B.
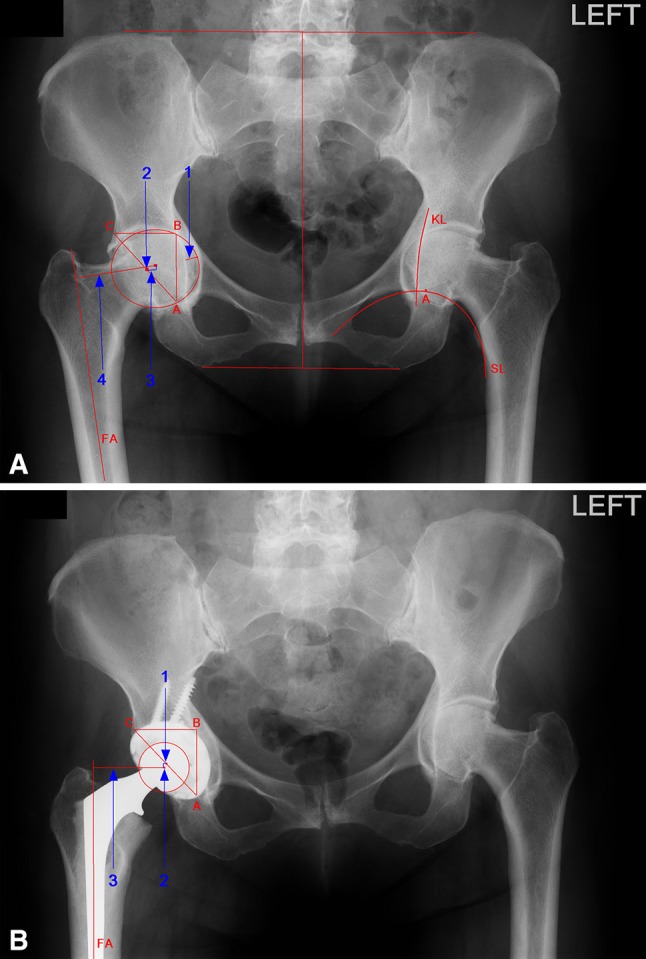
(A) Preoperative and (B) postoperative pelvic AP radiographs are shown for a patient with bilateral idiopathic protrusio acetabuli. The patient had a right THA with bone autograft for the acetabular reconstruction. The two horizontal lines shown in Illustration A mark the height of the pelvis. One-fifth of this distance determines the approximate height of the acetabulum (AB line). On the right side in Illustration A, point A is located 5 mm lateral to the intersection of Kohler’s line (KL) and Shenton’s line (SL). On the left side a similar point is marked A. The perpendicular line is drawn through point A, and point B is marked at one-fifth the height of the pelvis. The second perpendicular line then is drawn laterally from point B to a distance equal to AB. This marks point C. By joining points A and C, the isosceles triangle is completed. The midpoint of the AC line is the native hip center of rotation or the approximate femur head center which represents the reference point (0, 0). The femur offset is represented with a perpendicular line on the femur axis (FA) to the center of rotation (femur head center preoperatively and prosthetic femur head center postoperatively).
There were different types of uncemented cup designs implanted during the study period. The first-generation designs included Charnley (Howmedica, Mahwah, NJ, USA), Aufranc Turner (Howmedica), Elliptical (Implex Corp, Allendale, NJ, USA), and Ti-Bac Cups (Zimmer, Warsaw, IN, USA). The second-generation designs included the Harris-Galante (HG)-I (Zimmer), Harris-Galante (HG)-II (Zimmer), Omnifit (Osteonics, Mahwah, NJ, USA), ReflectionTM (Richards, [Smith & Nephew], Andover, MA, USA), Porous-Coated Anatomic (Howmedica), and Press-Fit Condylar (Johnson and Johnson, Warsaw, IN, USA). The third-generation designs included Pinnacle® (DePuy, Warsaw, IN, USA), Trilogy® (Zimmer), Hedrocel® (Implex Corp), TridentTM (Osteonics), Trabecular Metal Modular (Zimmer), and Tritanium® Hemispherical Cluster (Stryker, Mahwah, NJ, USA).
Need for additional revision procedure was recorded from medical records and the joint registry. The Harris hip score was calculated preoperatively and at latest followup [8].
Continuous variables (Harris hip scores, radiographic parameters) were compared between different reconstruction techniques using a pooled t-test, analysis of variance (ANOVA), and Tukey-Kramer honestly significant difference (HSD) t-test for multiple level comparisons. Matched pairs analysis was used to compare preoperative and postoperative continuous variables (Harris hip scores, radiographic parameters). Kaplan-Meier survival analyses were used to estimate the THA survivorship using aseptic cup revision for any reason as an end point at 10 and 15 years. Comparison of Kaplan-Meier survival curves for stratified factors (underlying etiology, cup fixation, and cup design) was performed with the log-rank test. Cox proportional hazards models were used to assess the effect of continuous variables (distance between the prosthetic femur head center to the native hip center of rotation on X and Y axes) on the cup survival from aseptic revision [19]. Significance was set at a probability less than 0.05. JMP® was used for statistical analysis (Version 9.0.1; SAS Institute Inc, Cary, NC, USA).
Results
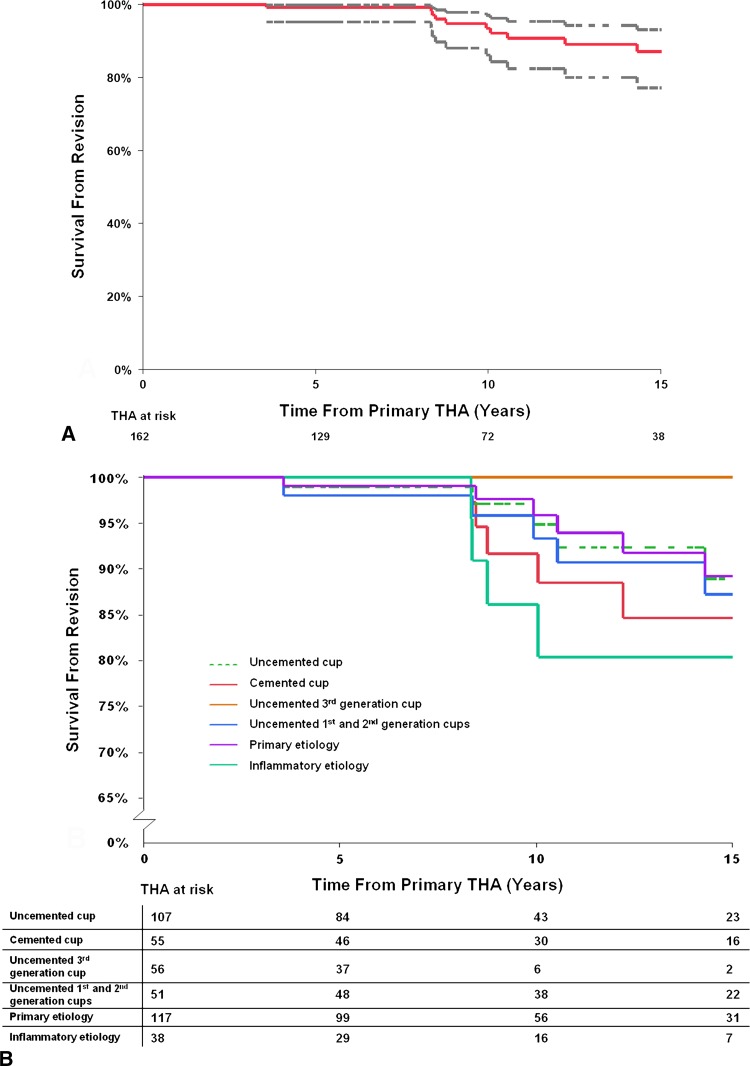
As a function of cup reconstruction type, there were no detected differences in survivorship between cemented and uncemented cups with the numbers available. The THA survival rates from aseptic cup revision at 10 and 15 years were 95% (95% CI, 85%–98%) and 89% (95% CI, 75%– 96%) for uncemented compared with 92% (95% CI, 77%–97%) and 85% (95% CI, 68%–94%) for cemented cups (p = 0.4). Furthermore, there were no detected differences between different uncemented cup designs and cemented cups (p = 0.5) (Fig. 2). Eleven aseptic cup revision procedures were performed at latest followup (Table 2).
Fig. 2A–B.
(A) A Kaplan-Meier survival curve for 162 THAs using aseptic cup revision for any reason as an end point is shown. The dashed lines represent the 95% CI. (B) A Kaplan-Meier survival curve for THA using aseptic cup revision for any reason as an end point based on etiology of protrusio, cup fixation, and uncemented cup design generation is shown.
Table 2.
Revision procedures for the patient cohort*
| Procedure | Number of THAs |
|---|---|
| Aseptic loose stem component | 8 |
| Aseptic loose cup component | 6 |
| Aseptic loose cup and stem components | 3 |
| Linear wear and modular exchange | 1 |
| Instability | 1 |
| Total | 19 |
* 162 hips.
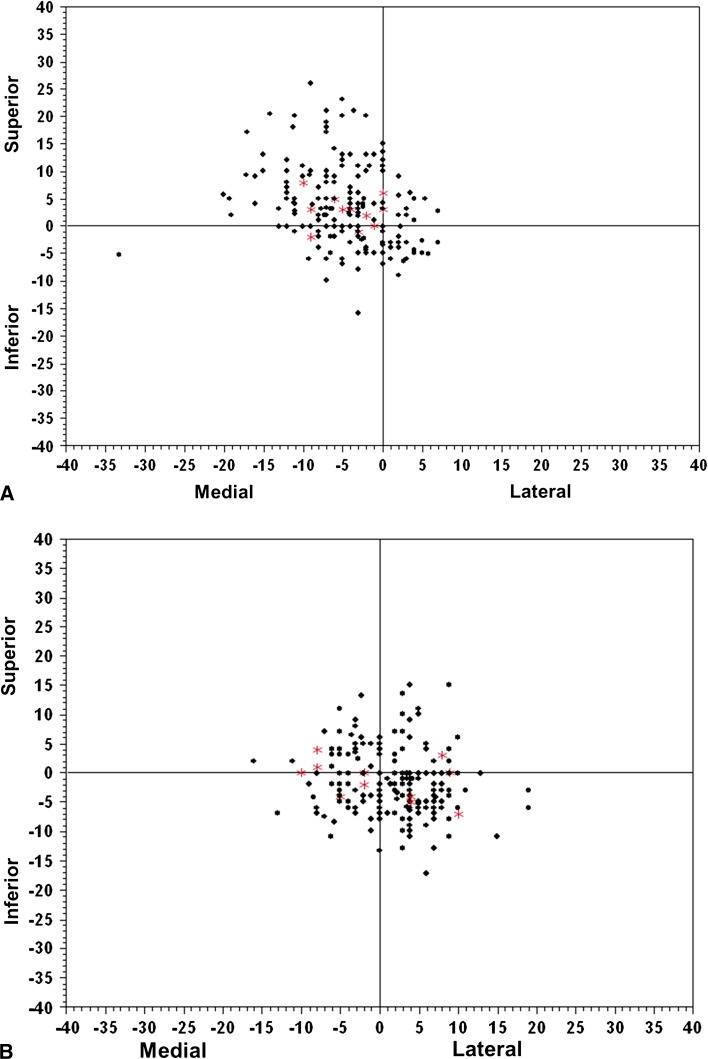
The risk of aseptic cup revision significantly increased by 24% (hazard ratio [HR]; 1.24; 95% CI, 1.02–1.5; p = 0.03) for every 1 mm medial or lateral away from the native hip center of rotation to the prosthetic femur head center. With the numbers available, there was no detected difference in the risk of aseptic cup revision if the cup was placed superior or inferior from the native hip center of rotation postoperatively (HR, 0.8; 95 CI %, 0.6–1.01; p = 0.07). The radiographic hip mechanics and femoral offset were restored with the different surgical techniques used. The femoral offset significantly decreased by 4 ± 9 mm (p < 0.001) and the hip center of rotation significantly improved by 11 ± 6 mm (p < 0.001) (Fig. 3). Higher restoration of the hip center was obtained when bone graft was used for acetabular reconstruction (Appendix 1).
Fig. 3A–B.
(A) Preoperative femur head center of rotation and (B) postoperative prosthetic femur head center of rotation are shown relative to the native hip center of rotation (0, 0) based on the Ranawat triangle method. *Preoperative and postoperative centers of rotation for the revised cups.
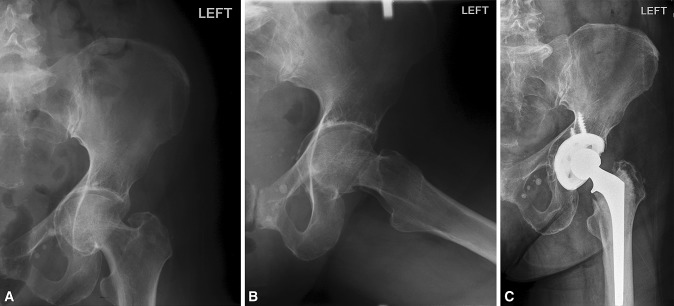
There were significant improvements in pain and function at final followup (Fig. 4). The mean preoperative Harris hip score improved from 51 ± 12 to 77 ± 18 points at latest followup (p < 0.001) (Table 1).
Fig. 4A–C.
(A) AP and (B) oblique view radiographs of the left hip of a 65-year old woman with idiopathic protrusio acetabuli are shown. The patient underwent a left THA using uncemented cup fixation with bone autograft for the acetabular reconstruction. (C) She had satisfactory radiographic 10-year followup.
Discussion
Protrusio is a rare finding in patients undergoing THA for end-stage hip arthritis. At the time of THA, restoring the hip center of rotation is ideal in hopes of improving function and obtaining a durable reconstruction. We found these reconstructions to be durable using either cemented or uncemented acetabular components, but better results were obtained when the hip center was restored within 7 mm of its native location.
There are numerous limitations to our study. First, there is inherent limitation to the measurements performed. The differences are small and we did not perform intraobserver or interobserver reliability of the radiographic parameters to determine their accuracy. However, all measurements were performed by one author (YMB) after proper training by the senior author (RJS) and review of multiple preoperative and postoperative radiographs. Second, restoration of the hip center of rotation was achieved at the index reconstruction through preoperative planning and intraoperative adjustment by using trial components along with radiographs but no specific reconstruction technique other than each surgeon’s philosophy (bone grafting the wall or not), and attempting to restore the hip center was used as an indication. Third, there is heterogeneity of the study population in terms of the multiple etiologies for the protrusio, different surgeon experience with reconstruction, different techniques for acetabular reconstruction (cemented, uncemented, with or without bone graft), and different implants used during the study period that could account for the differences. However, despite the use of early-generation designs, the results were mostly satisfactory in this patient population, and we found no differences in survivorship with the numbers available. Finally, we chose to evaluate only the acetabular reconstruction and its failures, but femoral component failure also could result from a poorly performed reconstruction.
This study showed satisfactory survivorship of the THA performed for protrusio at 15 years. Long-term survival rates from aseptic cup revision for uncemented and cemented fixation were 89% and 85%, respectively. Similar results have been reported by other authors. Ranawat et al. [15] reported the results of 35 cemented THAs without use of bone graft for acetabular reconstruction, performed for rheumatoid arthritis. They reported one acetabular and three femoral component failures at a mean of 4 years followup. Rosenberg et al. [16] reported on 36 cemented cups with use of bone graft for acetabular reconstruction, performed for rheumatoid arthritis. They reported 90% (95% CI, 77%– 100%) THA survivorship at 12 years mean followup using revision as the end point. Wilson and Scott [21] reported on 22 bipolar cups with bone grafting for the acetabular reconstruction. They were performed for rheumatoid arthritis in 16 hips and osteoarthritis in six hips. None was revised at a mean of 4.5 years followup. Mullaji and Marawar [12] also reported their results on 30 cementless porous-coated hemispheric cups with bone grafting for acetabular reconstruction. These were performed for inflammatory arthritis in 25 hips and osteoarthritis in five hips. None had failed at a mean followup of 4.2 years (range, 2–10 years). Matsuno et al. [10] reported on 15 hips with rheumatoid arthritis which were treated with HG cementless porous-coated cups and supported by an acetabular rim ring and bone grafting. None had failed at a mean followup of 4.5 years (range, 2–7 years).
A previous report on restoring center of rotation recommend against placement of cemented cups superior and lateral to the native hip center [13]. This may not be the case with uncemented fixation as previously reported [4, 17]. In our study, for every 1 mm the cup was placed lateral or medial away from the native hip center of rotation, there was a 24% increase in risk of aseptic cup revision. There was no detected difference in the risk for superior or inferior cup placement. The aim of the reconstruction therefore should be to restore the hip center. Whether bone graft should be used depends on how medial the center of rotation is and whether an uncemented cup that will fit the anterior and posterior dimension of the acetabulum will restore the hip center by the effect of its size and position alone. Lateralized hips were equally at risk of failure, so bone graft when not needed should be avoided. Restoring femur offset and the hip center of rotation in hips with protrusio are equivalent.
Significant improvements in pain and function were seen with THA for protrusio in our patients, and similar improvements were reported by others. Mullaji and Marawar [12] reported a mean Harris hip score of 85 with 90% excellent or good results. Matsuno et al. [10] reported satisfactory clinical results using the Japanese Orthopaedic Association (JOA) hip score. In our series, the clinical and functional results were excellent for uncemented cups, but the results were not as good as those seen with cemented cups alone without bone graft. This could represent worse clinical results owing to lack of restoration of hip mechanics that can lead to impaired function and limp.
To our knowledge, this is the largest series on the topic of THA for protrusio acetabuli. The survivorship of THAs from aseptic cup revision performed for protrusio acetabuli is satisfactory at 15 years independent of type of reconstruction or implant used. Uncemented cup fixation with or without graft has provided excellent results and is our preferred reconstruction technique. Despite that different implant designs were replaced for different etiologies by different surgeons in our study cohort, our findings show that the surgeon should aim to restore the normal hip center of rotation, taking care not to overlateralize it. Paying proper attention to the surgical technique at the time of acetabular reconstruction leads to predictable clinical results at long-term followup.
Acknowledgments
We thank Ross A. Dierkhising MS, for statistical support and Youlonda Lochler BS, for providing the study cohort.
Appendix 1
Preoperative and postoperative radiographic measurements
| Parameters | Uncemented reconstruction | Cemented reconstruction | ||
|---|---|---|---|---|
| Using bone graft | No bone graft | Using bone graft | No bone graft | |
| Preoperative | ||||
| Degree of protrusion; femur head beyond ilioischial line | 8 (5) | 6 (5) | 10 (5) | 6 (4) |
| Femoral offset (center of rotation to shaft axis) | 45 (8) | 43 (6) | 46 (6) | 47 (6) |
| Distance of COR (femur head center) to NHC on X* | −5 (7) | −4 (5) | −7 (5) | −5 (5) |
| Distance of COR (femur head center) to NHC on Y† | +3 (6) | +1 (6) | +6 (7) | +5 (9) |
| Direct distance of COR (femur head center) to NHC | 9 (6) | 8 (4) | 11 (6) | 10 (7) |
| Postoperative | ||||
| Femoral offset (center of rotation to shaft axis) | 41 (7) | 42 (10) | 36 (8) | 41 (8) |
| Distance of COR (prosthetic head center) to NHC on X* | +3 (5) | −1 (6) | +1 (6) | +1 (5) |
| Distance of COR (prosthetic head center) to NHC on Y† | −2 (5) | −2 (5) | −0.4 (6) | +1 (6) |
| Direct distance of COR (prosthetic head center) to NHC | 7 (4) | 7 (4) | 7 (3) | 7 (4) |
| Change | ||||
| Femoral offset (center of rotation to shaft axis) difference | −3 (9) | −0.1 (11) | −10 (8) | −6 (8) |
| Shifted distance of COR (femur head center → prosthetic femur head center) on X§ after reconstruction | +8 (7) | +3 (6) | +8 (6) | +5 (7) |
| Shifted distance of COR (femur head center → prosthetic femur head center) on Y‡ after reconstruction | −5 (6) | −3 (6) | −7 (5) | −4 (6) |
| Direct shifted distance of COR (femur head center → prosthetic femur head center after reconstruction; hip center difference) | 12 (6) | 8 (5) | 12 (6) | 10 (6) |
Parameters were measured in millimeters and expressed as the mean, with the standard deviation in parentheses; COR = center of rotation; NHC = native hip center of rotation (0, 0) or approximate femur head center based on Ranawat triangle method; * negative value indicates COR is medial to NHC, positive value indicates COR is lateral to NHC; † negative value indicates COR is inferior to NHC, positive value indicates the COR is superior to NHC; § negative value indicates COR was medially shifted, positive value indicates COR was laterally shifted; ‡ negative value indicates COR was inferiorly shifted, positive value indicates COR was superiorly shifted.
Footnotes
Funding for this study was received from CTSA Grant Number UL1 TR000135 (RJS) from the National Center for Advancing Translational Sciences (NCATS), a component of the National Institutes of Health (NIH). Its contents are solely the responsibility of the authors and do not necessarily represent the official view of NIH.
One of the authors (RJS) certifies that has or may receive payments or benefits, in any one year, an amount in excess of USD 10,000 from Biomet Inc (Warsaw, IN, USA).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Armbuster TG, Guerra J, Jr, Resnick D, Goergen TG, Feingold ML, Niwayama G, Danzig LA. The adult hip: an anatomic study. Part I: the bony landmarks. Radiology. 1978;128:1–10. doi: 10.1148/128.1.1. [DOI] [PubMed] [Google Scholar]
- 2.Berry DJ, Kessler M, Morrey BF. Maintaining a hip joint registry for 25 years: Mayo Clinic experience. Clin Orthop Relat Res. 1997;344:61–68. doi: 10.1097/00003086-199711000-00007. [DOI] [PubMed] [Google Scholar]
- 3.Charles MN, Bourne RB, Davey JR, Greenwald AS, Morrey BF, Rorabeck CH. Soft-tissue balancing of the hip: the role of femoral offset restoration. Instr Course Lect. 2005;54:131–141. [PubMed] [Google Scholar]
- 4.Dearborn JT, Harris WH. High placement of an acetabular component inserted without cement in a revision total hip arthroplasty: results after a mean of ten years. J Bone Joint Surg Am. 1999;81:469–480. doi: 10.2106/00004623-199904000-00004. [DOI] [PubMed] [Google Scholar]
- 5.Dunlop CC, Jones CW, Maffulli N. Protrusio acetabuli. Bull Hosp Jt Dis. 2005;62:105–114. [PubMed] [Google Scholar]
- 6.Gates HS, 3rd, McCollum DE, Poletti SC, Nunley JA. Bone-grafting in total hip arthroplasty for protrusio acetabuli: a follow-up note. J Bone Joint Surg Am. 1990;72:248–251. [PubMed] [Google Scholar]
- 7.Guerra J, Jr, Armbuster TG, Resnick D, Goergen TG, Feingold ML, Niwayama G, Danzig LA. The adult hip: an anatomic study. Part II: the soft-tissue landmarks. Radiology. 1978;128:11–20. doi: 10.1148/128.1.11. [DOI] [PubMed] [Google Scholar]
- 8.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51:737–755. [PubMed] [Google Scholar]
- 9.Hodgkinson JP, Shelley P, Wroblewski BM. The correlation between the roentgenographic appearance and operative findings at the bone-cement junction of the socket in Charnley low friction arthroplasties. Clin Orthop Relat Res. 1988;228:105–109. [PubMed] [Google Scholar]
- 10.Matsuno H, Yasuda T, Yudoh K, Yonezawa T, Nakazawa F, Murata T, Kimura T. Cementless cup supporter for protrusio acetabuli in patients with rheumatoid arthritis. Int Orthop. 2000;24:15–18. doi: 10.1007/s002640050004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McCollum DE, Nunley JA, Harrelson JM. Bone-grafting in total hip replacement for acetabular protrusion. J Bone Joint Surg Am. 1980;62:1065–1073. [PubMed] [Google Scholar]
- 12.Mullaji AB, Marawar SV. Primary total hip arthroplasty in protrusio acetabuli using impacted morsellized bone grafting and cementless cups: a medium-term radiographic review. J Arthroplasty. 2007;22:1143–1149. doi: 10.1016/j.arth.2006.11.005. [DOI] [PubMed] [Google Scholar]
- 13.Pagnano W, Hanssen AD, Lewallen DG, Shaughnessy WJ. The effect of superior placement of the acetabular component on the rate of loosening after total hip arthroplasty. J Bone Joint Surg Am. 1996;78:1004–1014. doi: 10.2106/00004623-199607000-00004. [DOI] [PubMed] [Google Scholar]
- 14.Pomeranz MM. Intrapelvic protrusion of the acetabulum (Otto pelvis). 1932. Clin Orthop Relat Res. 2007;465:6–15. doi: 10.1097/BLO.0b013e31815760f0. [DOI] [PubMed] [Google Scholar]
- 15.Ranawat CS, Dorr LD, Inglis AE. Total hip arthroplasty in protrusio acetabuli of rheumatoid arthritis. J Bone Joint Surg Am. 1980;62:1059–1065. [PubMed] [Google Scholar]
- 16.Rosenberg WW, Schreurs BW, de Waal Malefijt MC, Veth RP, Slooff TJ. Impacted morsellized bone grafting and cemented primary total hip arthroplasty for acetabular protrusion in patients with rheumatoid arthritis: an 8- to 18-year follow-up study of 36 hips. Acta Orthop Scand. 2000;71:143–146. doi: 10.1080/000164700317413102. [DOI] [PubMed] [Google Scholar]
- 17.Schutzer SF, Harris WH. High placement of porous-coated acetabular components in complex total hip arthroplasty. J Arthroplasty. 1994;9:359–367. doi: 10.1016/0883-5403(94)90045-0. [DOI] [PubMed] [Google Scholar]
- 18.Sotelo-Garza A, Charnley J. The results of Charnley arthroplasty of hip performed for protrusio acetabuli. Clin Orthop Relat Res. 1978;132:12–18. [PubMed] [Google Scholar]
- 19.Therneau TM, Grambsch PM. Modeling Survival Data: Extending the Cox Model. New York, NY: Springer; 2000. [Google Scholar]
- 20.Udomkiat P, Wan Z, Dorr LD. Comparison of preoperative radiographs and intraoperative findings of fixation of hemispheric porous-coated sockets. J Bone Joint Surg Am. 2001;83:1865–1870. doi: 10.2106/00004623-200112000-00015. [DOI] [PubMed] [Google Scholar]
- 21.Wilson MG, Scott RD. Bipolar socket in protrusio acetabuli: 3–6-year study. J Arthroplasty. 1993;8:405–411. doi: 10.1016/S0883-5403(06)80040-9. [DOI] [PubMed] [Google Scholar]
- 22.Winter E, Piert M, Volkmann R, Maurer F, Eingartner C, Weise K, Weller S. Allogeneic cancellous bone graft and a Burch-Schneider ring for acetabular reconstruction in revision hip arthritis. J Bone Joint Surg Am. 2001;83:862–867. [DOI] [PubMed]
- 23.Yoder SA, Brand RA, Pedersen DR, O’Gorman TW. Total hip acetabular component position affects component loosening rates. Clin Orthop Relat Res. 1988;228:79–87. [PubMed] [Google Scholar]