Abstract
Background
The incidence of extrapulmonary tuberculosis (TB) has increased in the chemotherapeutic era owing to the increasing presence of immunodeficiency disorders. Pubic symphysis TB, although uncommon, is again important as these infections once were in the prechemotherapeutic era.
Case Description
We present the cases of four patients with pubic symphysis TB in which one patient had a horseshoe-shaped abscess in the pubic region and another had a double lesion of the pelvis leading to vertical shear-type pathologic displacement. Three patients were diagnosed by cytology and PCR. These patients were treated successfully with antituberculosis treatment with or without minimal surgical intervention despite their late presentation and advanced disease. The fourth patient remains under treatment and followup.
Literature Review
We identified 40 patients with TB of the pubic symphysis in the English language medical literature. Of these 40 patients, only five are from India despite TB being endemic in this country. Followup information is available for 32 of the 40 patients with followups ranging from 1 to 84 months (mean of approximataly 20 months).
Purposes and Clinical Relevance
We suspect TB of the pubic symphysis is increasing in frequency owing to drug resistance, use of biologics, immunomodulating drugs, and anticancer drugs. Therefore, it is important for clinicians to have a high index of suspicion in patients at risk. Initially patients may be asymptomatic or present with adductor region pain or spasm, sacroiliac strain, limp, or a hypogastric, inguinal, or thigh mass that mimics an inguinal hernia, genitourinary, abdominal, or thigh tumor.
Conclusion
It is important to diagnose and treat pubic TB early in the course of the disease before the destructive stage. After relevant investigations most patients can be treated with antitubercular drugs with or without a minor surgical procedure.
Electronic supplementary material
The online version of this article (doi:10.1007/s11999-013-3037-0) contains supplementary material, which is available to authorized users.
Introduction
Tuberculosis (TB) remains one of the most critical health problems in the developing world. Musculoskeletal TB accounts for 3% of all cases [41]. The increasing incidence of immunodeficiency disorders and use of tumor necrosis factor-alpha (TNF-α) antagonist predispose patients to TB even in the developed world. TB can involve uncommon sites of the body [3]. TB in drug users has a predilection for rare sites such as the pubic symphysis and the sacroiliac and sternoclavicular joints [24]. Pubic bone TB is uncommon (less than 1 % of all musculoskeletal TB) [41, 53] even in populations in countries where the incidence of TB is high. A high index of suspicion is required in patients at risk presenting with groin or adductor pain, a waddling, antalgic gait, or sacroiliac strain. TB of the pubis has a varied clinical presentation, initially being asymptomatic to the most common presentation of an abscess and swelling in the hypogastric, perineal, medial thigh, or ischiorectal area. The overall decrease in disease incidence (even in the Indian subcontinent), lack of awareness, tardy course, and varied clinical presentation may lead to failure of early recognition and advanced disease at the time of diagnosis. In such cases, extensive osteocartilaginous destruction at the symphysis eventually can lead to sacroiliac joint instability. We present some uncommon clinical manifestations and treatment of four patients with TB of the pubic symphysis.
Case Reports
Patient 1
A 49-year-old woman presented with swelling and pain in left groin for 1 year. The pain was continuous, dull and confined to the groin. She had no limitation of activities of daily living except that she had to abduct her limbs during micturition. She had no gynecologic complaints. She had a history of intermittent fever, weight loss, and a family history of pulmonary TB. On examination there was a large swelling present on the medial aspect of the left thigh extending from the groin to midthigh (Fig. 1A). A smaller swelling was discernible only on palpation on the medial aspect of the right upper groin area. The swelling was nontender with normal temperature of the overlying skin. The swelling was cross-fluctuant (pressing swelling medially on the left thigh led to a palpable impulse on the right upper groin area), nonreducible, and could not be transilluminated. There was no distal neurovascular deficit. The pubic bone was irregular and tender on palpation. AP-view radiographs of the pelvis showed erosion of the pubic rami on both sides with widening of the symphysis (Fig. 1B). MRI revealed a large horseshoe-shaped abscess in the intermuscular plane with erosion of the pubic bones (Fig. 1C–F). The abscess was 14 × 8 cm extending from the medial side of the left thigh to the upper groin of the right side as seen on axial sections; the other limb of the horseshoe, although slightly broken, extended to a satellite abscess on the medial aspect of the right midthigh (hyperintense on T2-weighted images and isointense to hypointense on T1-weighted images). Hematologic studies showed an elevated erythrocyte sedimentation rate (ESR) (32 mm in the first hour) and lymphocytosis; the total leukocyte count was 8000/mm3 (the differential leukocyte count includes polymorphonuclear leukocytes, 35%; lymphocytes, 58%; eosinophils, 2%; and monocytes, 5%).The Mantoux test was positive with 10 mm induration. The chest radiograph was normal. A blood sample showed strongly positive ELISA for immunoglobulin M (IgM) for TB. The aspirate from the swelling was positive for Mycobacterium tuberculosis by PCR and culture. A smear for an acid-fast bacillus also was positive. Needle cytology from the aspirate showed a caseating granulomatous lesion. Venereal Disease Research Laboratory test (VDRL), HIV, hepatitis B and C viral markers, and urinalysis were negative. Based on these findings a diagnosis of pubic bone TB was made. The abscess was aspirated and 1 g streptomycin was instilled. The patient was prescribed antituberculosis chemotherapy using four drugs (rifampicin, isoniazid, pyrazinamide, and ethambutol) for 3 months followed by three drugs (isoniazid, rifampicin, and pyrazinamide) for 4 months, and finally two drugs (isoniazid and rifampicin) for the subsequent 11 months. The abscess did not subside completely (Fig. 1G–H) after repeated aspirations and subsequently was drained surgically under cover of antituberculosis treatment. The patient’s symptoms improved with subsidence of swelling and healing of the bone lesion after 18 months of treatment. The patient currently is being followed up (3 years) for any recurrence.
Fig. 1A–H.
(A) A clinical photograph shows a large horseshoe-shaped abscess (white arrow) and small satellite abscess on the opposite thigh (black arrow) in Patient 1. (B) An AP view of the patient’s pelvis shows destruction and irregularity of the pubic symphysis (arrow). (C) A coronal T2-weighted MR image of the pelvis with both hips shows a large fluid collection that is hyperintense and extends from the left thigh (white arrow) to the upper medial right groin area and a satellite abscess which also is hyperintense on the right midthigh (black arrow). (D) A coronal T1-weighted MR image of the pelvis with both hips shows the above-mentioned fluid collections (white and black outlined arrow) as hypointense signal. Coronal (E) T2- and (F) T1-weighted images show the horseshoe-shaped collection marked as an inverted U. The arrows point to the abscess in both illustrations. (G) The mass was aspirated but (H) did not subside even after repeated aspiration.
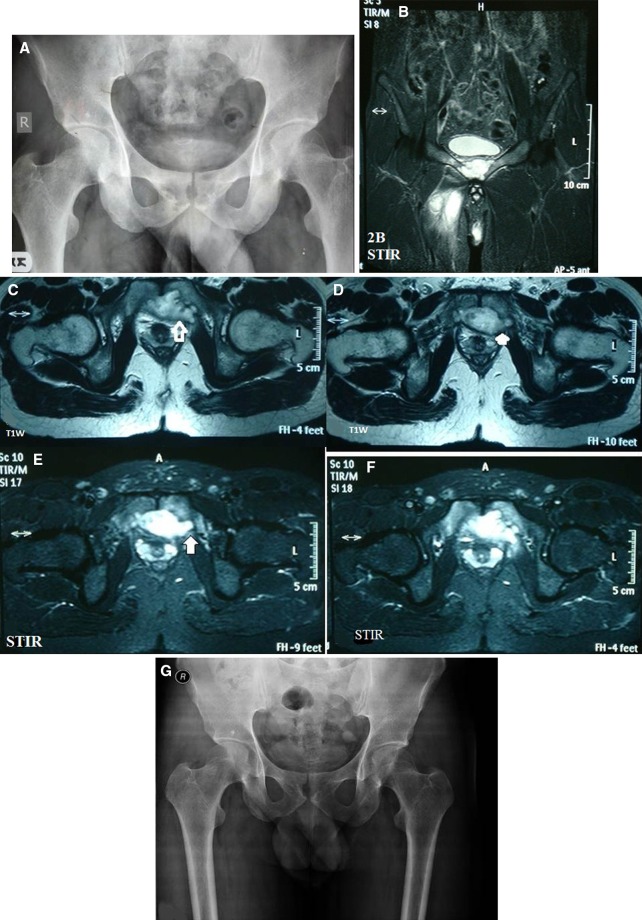
Patient 2
A 31-year-old man presented with difficulty in walking and pain in the pelvic region for the past 3 years. The pain was intermittent and mild to moderate in intensity. The patient had no history of fever but had gradual weight loss, frequency of micturition, and anorexia. Examination revealed tenderness over the pubic symphysis. Radiographs of the pelvis showed osteolysis of both pubic bones with widening of the symphysis (Fig. 2A). MRI of the pelvis showed a fluid collection measuring 45 × 34 mm behind the symphysis (Fig. 2B) which was hyperintense on T2-weighted (Fig. 2C–D) and STIR images (Fig. 2E–F). There was internal erosion of both superior pubic rami and the symphysis pubis. Hematologic studies showed an ESR of 8 mm in the first hour and C-reactive protein level of 8 mg/dL. The Mantoux test was positive with 10 mm induration. The ELISA IgM for Mycobacterium tuberculosis was positive. Needle cytology of the aspirate showed granulomatous pathologic features. PCR for Mycobacterium tuberculosis was positive. Based on these findings the patient was treated with our standard antitubercular treatment. On followup, after 21 months of treatment the patient is asymptomatic and is able to pursue his occupation. An AP radiograph showed bony healing (Fig. 2G).
Fig. 2A–G.
(A) The initial AP pelvic radiograph of Patient 2 shows destruction and rarefaction of the pubic bones; it appears as cup-shaped destruction and is more on the right side. (B) A T2-weighted coronal MR image of the pelvis shows a large fluid collection that is hyperintense extending from the medial side of the right thigh to the pubic symphysis. Axial T1-weighted MR images show destruction of the pubis and symphysis with a retropubic abscess that is hypointense (C) invading the pubic bone (arrow) on the left side and (D) pressing the bladder (arrow) posteriorly more on the left side. Axial MR STIR images of the pelvis show destruction of the pubis and symphysis that is hyperintense and (E) invading the pubic bone (arrow) on the left side and (F) presses the bladder (arrow) posteriorly more on the left side. (G) A followup radiograph obtained after a full course of antituberculosis treatment shows bony healing and the appearance of a white line of healing on the right side.
Patient 3
An 18-year-old girl presented with a 10-month history of pain and a 3-month history of a discharging sinus in the pubic area. The pain was gradual in onset. She had been treated for pain without relief and had a vulvar swelling which ruptured and discharged serosanguinous fluid. She described discharge of granular bone pieces from the sinuses. There was no history of trauma, gynecologic complaints, or pulmonary or extrapulmonary TB. She had a history of low-grade fever, reduced appetite, and weight loss. On examination, there were two discharging sinuses on either side of the vulva measuring 1 cm × 2 cm. On palpation the region of the sinuses was warm; the pubis was tender and the sinuses were adherent to the pubis with associated granulation and a serosanguinous discharge. The surrounding skin was indurated. Hematologic studies revealed hemoglobin of 10 g%, total leukocyte count of 9700 mm3 with lymphocytosis (55%), and elevated ESR (42 mm/first hour). The Mantoux test showed an induration of 20 mm. ELISA for IgM antibodies of Mycobacterium tuberculosis was strongly positive. Radiographs of the pelvis showed erosion of the symphysis. Biopsy of the sinus tract showed caseating granulomas with typical tubercular giant cells and a positive stain for acid fast bacillus. VDRL, HIV, hepatitis B and C viral markers, and urinalysis were negative. The patient was prescribed four drugs for antitubercular treatment. She showed no improvement in 6 weeks, therefore a sequestrectomy, excision of the sinus tract, and débridement were performed and the patient continued receiving four drugs (isoniazid, rifampicin, pyrazinamide, and ethambutol) for 3 months, three drugs (isoniazid, rifampicin, and pyrazinamide) for 4 months, and two drugs (isoniazid and rifampicin) for 11 months. The pain resolved and the sinus healed during the first 4 months of treatment. The patient’s general condition was improved at 18 months. New bone formation was seen on radiologic examination of the pubis. She has been asymptomatic for the last 5 years.
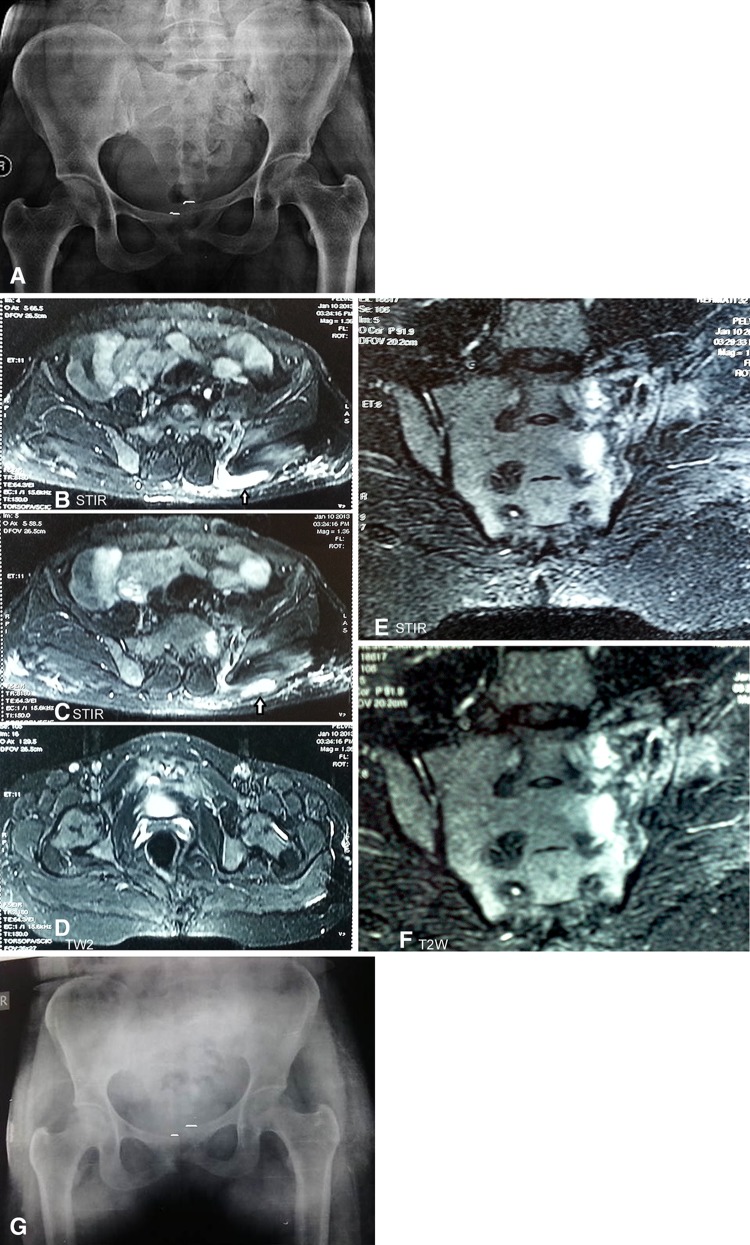
Patient 4
A 32-year-old woman with tubercular meningitis and receiving antitubercular therapy for 3 months was referred by her physician. She had an 11-month history of low back pain and pain in the pubic region. She was treated for these complaints previously with no relief. She had a short limb gait with an antalgic component. She had anorexia and weight loss. On examination there was tenderness over her lower back, left sacroiliac joint, and pubic symphysis. Her ESR was 50 mm in the first hour. Radiograph of the pelvis showed rarefaction of the pubic region, osteolysis of the pubic bones, and widening of the symphysis. There was widening and erosion of the left sacroiliac joint. The pelvis on the left side was shifted proximally (Fig. 3A). MRI showed focal destruction and subluxation with irregular articular margins with surrounding edema involving the pubic symphysis which was isointense on T1-weighted axial images and hyperintense on STIR images (Fig. 3B–C) and on T2-weighted images (Fig. 3D). There was a thick walled fluid collection in the sacroiliac joint and left gluteal muscle (Fig. 3B–C). On coronal images there was marrow edema and focal destruction of the left sacroiliac joint, left sacrum, and left iliac bone with periarticular soft tissue thickening (Fig. 3E–F). The patient continued to receive antituberculosis treatment, and was prescribed skeletal traction. She has received four drugs (isoniazid, rifampicin, pyrazinamide, and ethambutol) for 3 months, and three drugs (isoniazid, rifampicin, and ethambutol) for 3 months. An AP weightbearing pelvic radiograph showed stabilization of the pelvic shift (Fig. 3G). After 6 months of treatment she regained her appetite, her gait improved, and her pain decreased with apparent shortening of 1 cm.
Fig. 3A–G.
(A) An initial AP radiograph of the pelvis of Patient 4 shows destruction, irregularity, and disruption of the pubic symphysis and sacroiliac joint on the same side with vertical migration of the left hemipelvis. The white lines show the extent of proximal migration. (B) An axial STIR image shows destruction of the left sacroiliac joint as hyperintense signal with a small fluid collection under the skin on left side (arrow). (C) An axial STIR image at the level of the sacral promontory shows destruction of the left sacral ala and iliac crest as hyperintense signal with a small fluid collection under the skin on the left side (arrow). (D) An axial T2-weighted MR image shows destruction of the pubic symphysis and a retropubic fluid collection that appears hyperintense. (E) A coronal STIR image of the sacroiliac joint shows hyperintense signal changes in the marrow of the adjacent sacrum and iliac bone. (F) A coronal T2-weighted image shows hyperintense signal changes in the marrow of the adjacent sacrum and iliac bone with adjacent periarticular destruction involving the entire sacrum. (G) A followup weightbearing radiograph at 3 months shows the lesion has stabilized (with 1 cm shortening; the white lines show the extent of vertical migration which is less than before traction [Fig. 3A]).
Search Strategy and Criteria
We performed a systematic review of English and non-English articles of TB of the pubic symphysis reported from 1855 to 2012 using the terms, “tuberculosis AND (pubis OR pubic)” and “tuberculosis AND (pubis [ti] and OR pubic [ti])”in PubMed and Google. (Appendix 1. Supplemental materials are available with the online version of CORR). We identified 149 cases in the world medical literature. Many cases (109) [9, 12–15, 20, 23, 30, 32, 35, 38–40, 43, 44, 47–49, 54] were not published in English and we had incomplete information. We identified 40 cases published in the English literature [1–7, 10, 11, 17, 19, 21, 22, 25, 26, 28, 29, 31, 33, 34, 36, 37, 42, 45, 46, 50, 55]. Followup information is available for 32 patients [3, 4, 6, 7, 9,11, 25, 31, 36, 37, 46, 50 ]. Followup ranged from 1 to 84 months (mean of approximately 20 months).
Discussion
The pubic symphysis is a nonsynovial amphiarthrodial joint with a fibrocartilage disc between two pubic body bones lined by hyaline cartilage. The inferior pubic or arcuate ligament is the strongest stabilizing structure. The pubic symphysis receives its blood supply from the inferior epigastric, pudendal, medial circumflex femoral and obturator arteries [8].
TB of the pubic symphysis is mostly blood borne [3] (as in our Patient 4 with multisystem TB) and the infection spreads hematogenously to the metaphyseal bone and the fibrocartilage of the pubis. The other less common although important source of infection is locally through the adjacent genitourinary tract or related therapeutic procedures [5, 24]. The infection leads to destruction of bone and metaphyseal abscess formation causing loss of nutrition of the hyaline cartilage. A local purulent response may destroy the cartilage directly or by pressure [24]. Biomechanically the pubic symphysis and its ligaments act as a tension band to rotational forces applied to the pelvis in the upright position by the posterior sacroiliac ligament. Therefore, if the disease is not treated at an early stage, destruction of the symphysis and pubic bones can lead to secondary sacroiliac strain and eventually diastasis of the symphysis and pelvic instability (Patient 4) in late stages [6, 24]. No age subject is immune with ages ranging from 5 to 79 years. TB of symphysis pubis more commonly affects adults than children. The pubic bone is largely cartilaginous at birth and completely ossifies by adolescence [6, 24], therefore there is a decreased chance of infection in children. Büngner [13] stated that the histologic structure of the symphysis would prevent TB in children. Interestingly, male children are more commonly involved than females in the pediatric age group. The disease most commonly affects subjects 20 to 30 years of age of both sexes. The disease has bimodal predilection in females in the second to third and sixth to seventh decades of life.
Most patients presented with painful or painless swelling or a lump in the groin, pubic, inguinal, suprapubic, hypogastric, or symphyseal regions. The swelling sometimes extended to the thigh, vulva, mons pubis, and retroperitoneal areas. Presentation in the form of a horseshoe abscess is rare and has not been described. Pubic TB destroys the symphysis with cold abscess formation. The abscess spreads deep to membranous layer of the superficial fascia along the attached adductor muscles to the inner aspect of both thighs medial to Holden’s line producing a horseshoe-shaped abscess. Swelling typically is nontender, warm to cold, and may become firm with time. In these cases it may be mistaken for a hernia, lipoma, or soft tissue tumor depending on the location [7, 37]. Presumably this was the reason that the abscess was missed and mistaken as a lipoma in Patient 1. Other causes of horseshoe or inverted U-shaped abscesses are cystitis, perianal abscess, bilateral psoas abscess, or ischiorectal abscess attributable to spinal TB or TB of the hip tracking down the Scarpa’s triangle bilaterally. The swelling sometimes bursts leading to a discharging sinus with pus and/or with granular bone pieces and fistula. In these cases, TB should be considered before any other lesion (Patient 3). Patients may present with urinary complaints owing to perforation of an abscess in to the urinary bladder and result in osteuria [2] and pyuria [19].
Pain was the next common complaint. It has been described as dull to moderate and usually occurred in the symphyseal area, lower abdomen, pubic, inguinal, suprapubic, lumbar, hip, and pelvic regions. Pain may be associated with adductor spasm and extend to the knee. The patients may present with limp and an antalgic or waddling gait.
Constitutional symptoms usually are absent owing to the very slow disease process. Few patients reported substantial weight loss, similar to our patients. Other symptoms such as loss of appetite, fever, weakness, chronic cough, and enlarged lymph nodes also were reported.
The concomitant TB of other parts of the body, most frequently of the lung, was present in 10 patients. These cases may mimic metastatic bone disease in some patients leading to confusion and delay in diagnosis [50]. The sacroiliac joint was involved in three reported cases similar to our Patient 4.
MRI provides anatomic details of a soft tissue mass or an abscess, fistula tract, and osseous defects. The earliest changes which can be missed on the initial radiographs can be picked up by MRI as it shows bone marrow changes of infection early. These changes are isointense or hypointense on T1-weighted and hyperintense on T2-weighted and STIR images. It also helps in diagnosing atypical presentations, skip lesions, satellite fluid collections in other areas, and concomitant involvement of TB in other parts under examination (Patients 1 and 4). MRI may show an abscess or horseshoe-shaped abscess as hypointense on T1-weighted images and hyperintense on T2-weighted images and may exhibit peripheral rim enhancement on contrast.
The diagnostic hallmark of TB is characteristic histopathologic features and/or a positive smear for acid fast bacillus. It is prudent to perform an open biopsy (along with surgical débridement) in patients who do not respond to antituberculosis treatment in 6 weeks (Patient 3). A needle biopsy with or without fluoroscopic control is a simple diagnostic procedure that can be performed when there is an overt abscess, or abscess with thick debris or a small fluid collection. It is of therapeutic value in patients who need immediate decompression for symptomatic abscesses causing pressure on the adjacent structures. In addition, antitubercular drug sensitivity can be obtained from needle aspirate. A needle biopsy with saline irrigation may be used if the fluid yield is low. Despite positive histopathologic and cytologic analyses, acid-fast bacilli were reported only in five patients overall reported in the English literature. Culture of the aspirate or tissue was used for verification of TB in 15 cases. Aspiration cytology was conclusive for TB in our three patients. Recently PCR has been described as a diagnostic modality [46]; we also performed PCR of the aspirate or tissue to confirm the diagnosis. With equivocal biopsy results, PCR should be performed for a definite diagnosis of TB. It is 100% specific for Mycobacterium tuberculosis ruling out atypical infection [51].
With our literature review and our four patients, we found that the diagnosis of symphysis TB is delayed in many patients for months to years and these are patients who have been treated for other conditions [3, 7, 26, 38, 46]. A delay in diagnosis is attributed to lack of knowledge regarding this uncommon problem, vague symptoms and signs, and resemblance to other diseases of the pubic symphysis. Pubic TB should be differentiated from conditions such as osteitis pubis, a noninfective chronic inflammation of the pubic symphysis which is more common and closely mimics pubic TB [3, 6, 7, 46]. It is a self-limiting and more painful condition and occurs in patients with rheumatic disease, during pregnancy, in athletes, after gynecologic and urologic surgeries, and following trauma [18, 27, 50, 52]. These patients present with intense anterior and medial groin pain over the symphysis without an abscess formation. Initial radiographs may be normal or show patchy sclerosis, irregular cortical margins, or marked symmetric rarefaction of the pubis. Sequestrum formation unlike in tubercular infection is rare. On MRI subchondral bone marrow edema, fluid in the symphysis pubis joint, and periarticular edema are the most reliable indicators in initial cases. In patients with chronic disease, subchondral sclerosis, subchondral resorption, bony margin irregularities, and osteophytes (or pubic beaking) are the most reliable findings. Treatment is usually nonoperative in the form of rest, moist heat, and analgesics.
Twenty-seven patients have received antituberculous therapy with or without surgical intervention [2–5, 9, 10, 19, 21, 26, 28, 31, 32, 34, 36–39, 45, 46, 50]. The medical treatment usually was continued during a 6- to 18-month period. The treatment of TB of the pubic symphysis generally is medical without surgical intervention [5, 6]. In patients with relapse of the TB or recurrence of a new lesion, 50% of these patients had antitubercular treatment for less than 12 months [51]. This is a strong indication against short-term antitubercular treatment regimens, particularly in countries where malnutrition, lack of education, poverty, and large population act as precipitating factors. Longer-term treatment for 12 to 18 months usually resolves the problems of recurrence and relapse [51]. Use of antitubercular drugs must be continued for approximately 18 months and must include isoniazid. The fourth edition of the WHO guidelines for treatment of TB suggests longer treatment for TB meningitis and for bone or joint TB [53].
Before the advent of antituberculosis treatment, most of the patients were treated with surgery. Curettage [2, 7, 31, 34, 36–38, 44] and sequestrectomy [1, 7, 10, 16, 25, 37] were the most commonly used procedures. The other surgical procedures such as abscess exploration, aspiration, fistula incision, abscess excision, pus drainage, pubic bone excision, and removal of the symphysis pubis, have been reported by many authors [5, 6, 13, 16, 25, 29, 34, 35, 37, 42] to control the infection. Arthrodesis of the symphysis joint was recommended by some authors to prevent mechanical instability of the symphysis and sacroiliac joint [6, 7, 36]. In one case, fusion of the sacroiliac joint was performed to prevent this late complication [11]. Autogenous cancellous bone graft was used in three cases and a reconstruction plate was used for fixation in two cases. We do not favor bone grafting and fixation for such cases owing to infective process. Additionally the use of implants should be limited in this area owing to questionable implant purchase in the cancellous bone and risk of recurrence.
We suggest that initial antitubercular chemotherapy alone should be tried for every patient under supervision. Surgery should be limited for specific indications such as biopsy, abscesses and sinuses that show no regression after 3 to 6 months of antitubercular treatment, recurrent abscess, tense abscess with pressure symptoms, and for patients who show no response after 6 to 8 weeks of antituberculosis treatment. Our case series shows that a complete course of antitubercular chemotherapy remains the keystone of successful treatment. Healing of the symphysis takes place by the defects being encapsulated with calcium but not being filled in [43].
Although the prognosis for control of infection is good, there is a danger of extension to other organs, especially the urinary bladder [2, 49]. Two patients had recurrences and one patient had partial healing and persistence of sinus, but eventually these patients achieved healing with treatment [36, 37]. Despite infection control in most of the patients, four patients whose cases were reported in the English literature died [21, 25, 43].
TB of the pubic symphysis is a rare condition. A high index of suspicion is required to establish the correct diagnosis at an early stage and to properly treat the patient. A large review of previously reported cases provides insight about this uncommon but treatable disease.
Electronic supplementary material
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the reporting of this case report, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Alpert L. Tuberculosis of the symphysis pubis. N Engl J Med. 1939;220:786–792. doi: 10.1056/NEJM193905112201904. [DOI] [Google Scholar]
- 2.Aswathaman K, Devasia A. Osteuria. Urology. 2008;71(546):e13. doi: 10.1016/j.urology.2007.11.023. [DOI] [PubMed] [Google Scholar]
- 3.Bali K, Kumar V, Patel S, Mootha AK. Tuberculosis of symphysis pubis in a 17 year old male: a rare case presentation and review of literature. J Orthop Surg Res. 2010;5:63. doi: 10.1186/1749-799X-5-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Balsarkar DJ, Joshi MA. Tuberculosis of pubic symphysis presenting with hypogastric mass. J Postgrad Med. 2001;47:54. [PubMed] [Google Scholar]
- 5.Barnett E. Tuberculous osteitis pubis. Br J Radiol. 1957;30:125–128. doi: 10.1259/0007-1285-30-351-125. [DOI] [PubMed] [Google Scholar]
- 6.Bayrakci K, Daglar B, Tasbas BA, Agar M, Gunel U. Tuberculosis osteomyelitis of symphysis pubis. Orthopedics. 2006;29:948–950. doi: 10.3928/01477447-20061001-15. [DOI] [PubMed] [Google Scholar]
- 7.Bean HC. Tuberculosis of pubic symphysis. J Bone Joint Surg Am. 1930;12:345–352. [Google Scholar]
- 8.Becker I, Woodley SJ, Stringer MD. The adult human pubic symphysis: a systematic review. J Anat. 2010;217:475–487. doi: 10.1111/j.1469-7580.2010.01300.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Benbouazza K, Allali F, Bezza A, el Hassani S, el Maghraoui A, Lazrak N, Hassouni F, Hajjaj-Hassouni N. [Pubic tuberculous osteo-arthritis: apropos of 2 cases][in French] Rev Chir Orthop Reparatrice Appar Mot. 1997;83:670–672. [PubMed] [Google Scholar]
- 10.Bevan PG. Tuberculosis of pubis presenting as a cold abscess of the thigh. Br Med J. 1955;2:832–833. doi: 10.1136/bmj.2.4943.832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Blair HC. Tuberculosis of symphysis pubis. J Bone Joint Surg Am. 1929;11:401–402. [Google Scholar]
- 12.Bronner U, Lindquist L, Svanbom M. [Tuberculous infection of the symphysis][in Swedish] Lakartidningen. 1990;87:388–389. [PubMed] [Google Scholar]
- 13.Büngner. Sobre la Tuberculosis de la Sinfisis pubiana [Tuberculosis of the symphysis of the pubis]. Clin mod Zaragoza. 1914;XIII:143–160.
- 14.Cadili G. [Tuberculosis of the pubic symphysis][in Italian] Sicil Sanit. 1964;33:21–26. [PubMed] [Google Scholar]
- 15.Chaaveau M, Contribution B. l’etude des Osteite tuberculeuses juxta coxales d’apres 20 observations recu B l’H6pital. Paris, France: Maritime de Berc; 1922. [Google Scholar]
- 16.Chauvel. Osteite tuberculeuse du pubis: ablation de la moitié gauche de la symphyse. guérison. Bull et mém Soc de Chir de Paris. 1890;XVI:430.
- 17.Clairmont PJ. Tuberculous osteitis of symphysis pubis, with sinus formation and mixed infection with the staphylococcus aureus. Br J Surg. 1925;12:606. [Google Scholar]
- 18.Coventry MB, Mitchell WC. Osteitis pubis: observations based on a study of 45 patients. JAMA. 1961;178:898–905. doi: 10.1001/jama.1961.03040480028006. [DOI] [PubMed] [Google Scholar]
- 19.Devarajan R, Ojha H, Desai KM, Chen K. Tubercular osteomyelitis of the pubic symphysis caseating into the bladder with concurrent tubercular pyonephrosis and epididymitis. BJU Int. 2000;86:144. [Google Scholar]
- 20.Dybowski WR, Makuchowa K. [Tuberculosis of the pubic symphysis][in Polish] Chir Narzadow Ruchu Ortop Pol. 1974;39:633–639. [PubMed] [Google Scholar]
- 21.Ellis W. Multiple bone lesions caused by Avian-Battey mycobacteria: report of a case. J Bone Joint Surg Br. 1974;56:323–326. [PubMed] [Google Scholar]
- 22.Fairbank HA. Tuberculosis of the pubis. Br Med J. 1955;2:1028. doi: 10.1136/bmj.2.4946.1028. [DOI] [Google Scholar]
- 23.Fares G, Pagani A. [Tubercular osteitis of the pubis][in Italian] Minerva Ortop. 1966;17:459–469. [PubMed] [Google Scholar]
- 24.Gamble JG, Simmons SC, Freedman M. The symphysis pubis: anatomic and pathologic considerations. Clin Orthop Relat Res. 1986;203:261–272. [PubMed] [Google Scholar]
- 25.Greger E. Five cases of tuberculosis of the symphysis pubis. Acta Orthop Scand. 1938;9:43. doi: 10.3109/17453673808988892. [DOI] [Google Scholar]
- 26.Gulia J, Kim P, Kortepeter MG, Nguewou A, Waga M, Lai L. Multiple fractures of the symphysis pubis due to tuberculous osteomyelitis. Southeast Asian J Trop Med Public Health. 2009;40:1279–1283. [PubMed] [Google Scholar]
- 27.Harris NH, Murray RO. Lesions of the symphysis in athletes. Br Med J. 1974;4:211–214. doi: 10.1136/bmj.4.5938.211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hunter DC, Sim D. Pelvic tuberculosis: a case of delayed diagnosis. Acta Obstet Gynecol Scand. 2001;80:281–282. doi: 10.1034/j.1600-0412.2001.080003281.x. [DOI] [PubMed] [Google Scholar]
- 29.Jackson JB., Jr A case of tuberculosis of the symphysis pubis. Am J Roentgenol. 1923;10:806. [Google Scholar]
- 30.Joachimouits R. Uber die differential diagnose der schambein tuberkulose beim weibe und uber die wege der abzzebwanderung bei dieser Erkrankung. Deutsche Zeitschrift für Chirurgie. 1929;219:257–277. doi: 10.1007/BF02819495. [DOI] [Google Scholar]
- 31.Ker NB. Tuberculosis of the pubic symphysis. J R Soc Med. 1986;79:429–430. doi: 10.1177/014107688607900716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Khazov PD. [Congestive abscess masking a soft tissue tumor][in Russian] Probl Tuberk. 1992;5–6:55–56. [PubMed] [Google Scholar]
- 33.Kirker JR. Tuberculous osteitis pubis. J Bone Joint Surg Br. 1956;38:602. [Google Scholar]
- 34.Manzaneque L, Marin I, García-Bragado F, Beiztegui A, Dastis C, Sánchez-Matas P. Osteoarticular tuberculosis of the symphysis pubis presenting as a hypogastric cystic mass in a woman with primary Sjögren’s syndrome. Br J Rheumatol. 1992;31:495–496. doi: 10.1093/rheumatology/31.7.495. [DOI] [PubMed] [Google Scholar]
- 35.Mario C. Considerazioni anatomo-pathologiche e note cliniche sulla tuberculosi primitiva della sinfisi pubica [Primary tuberculosis of the symphosis of the pubis]. Atti d r Accad fisiocrit in Siena. 1913;V:487.
- 36.Moon MS, Ok IY, Ha KY, Sihn JC. Tuberculosis of the ischiopubic ramus: a report of five cases. Int Orthop. 1990;14:175–177. doi: 10.1007/BF00180124. [DOI] [PubMed] [Google Scholar]
- 37.Nicholson OR. Tuberculosis of the pubis: report of eleven cases. J Bone Joint Surg Br. 1958;40:6–15. doi: 10.1302/0301-620X.40B1.6. [DOI] [PubMed] [Google Scholar]
- 38.Ohkouchi M, Inase N, Yasui M, Miura H. [Case of pubic tuberculous osteomyelitis and pericarditis during anti-tuberculosis chemotherapy][in Japanese] Kekkaku. 2004;79:531–535. [PubMed] [Google Scholar]
- 39.Qassemyar Q, Smail A, Perignon D, Robbe M, Sinna R. [Cold abscess and Bazin’s indurated erythema associated to pubic symphysis tuberculosis][in French] Med Mal Infect. 2010;40:552–554. doi: 10.1016/j.medmal.2010.02.008. [DOI] [PubMed] [Google Scholar]
- 40.Quaini P. [Tuberculosis of the pubic symphysis in pregnancy][in undetermined language]. Minerva Ginecol. 1953;5:Atti, 57–61. [PubMed]
- 41.Rajasekaran S, Dheenadhyalan J. Tuberculosis of bone and joints. In: Bulstrode C, Buckwalter J, Carr A, Marsh L, Fairbank J, Wilson-MacDonald J, Bowden G, editors. Oxford Textbook of Orthopaedics and Trauma. 1. Oxford, UK: Oxford University Press; 2002. pp. 1532–1560. [Google Scholar]
- 42.Ramakrishnaiah VP, Jain V, Choon AT, Rao BH. Retroperitoneal cold abscess with tuberculosis of sacro-iliac joint and pubic bone: a case report of unusual presentation of osteo-articular tuberculosis. J Indian Med Assoc. 2000;98:128–129. [PubMed] [Google Scholar]
- 43.Reich L. Ein Fall von Karies der Symphyse als Osteosarkom diagnostiziert. Fortschr. auf dem Gebiete der Röntgenstrahlen. 1923;XXXI:621.
- 44.Rendu A, Wertheimer P. Sur un cas de tuberculose du pubis et de la symphyse pubienne. Rev d’Orthop. 1922;IX:363–366.
- 45.Rozadilla A, Nolla JM, Rodriguez J, Del Blanco J, Roig Escofet D. Tuberculosis of the pubis symphysis. J Rheumatol. 1991;18:1271–1272. [PubMed] [Google Scholar]
- 46.Singh S, Arora S, Sural S, Dhal A. Tuberculosis of the pubic symphysis masquerading as osteitis pubis: a case report. Acta Orthop Traumatol Turc. 2012;46:223–227. doi: 10.3944/AOTT.2012.2696. [DOI] [PubMed] [Google Scholar]
- 47.Sorrel E, Sorrel-Déjerine Y. Tuberculose osseuse et ostéo-articulaire. Paris, France: Masson et Cie; 1932. [Google Scholar]
-
48.Swynghedauw ET, Druon. La tuberculose de l’angle du pubis et de la symphyse pubienne (osteoarthrite tuberculeuse de la symphyse).
 . 1923;XCVI:413.
. 1923;XCVI:413.
- 49.Thilesen. Tilfzelde av necrose i belrkenbenene, stendannelse om et i blzeren indtrzengt necrotisert benstykke etc. Norsk Magasin for Lagevidenskapen; 1855.
- 50.Tsay MH, Chen MC, Jaung GY, Pang KK, Chen BF. Atypical skeletal tuberculosis mimicking tumor metastases: report of a case. J Formos Med Assoc. 1995;94:428–431. [PubMed] [Google Scholar]
- 51.Tuli SM. Clinical features. In: Tuli SM, ed. Tuberculosis of Skeletal System (bones, joints, spine and bursal sheaths). 4th ed. New Delhi, India: Jaypee Brothers; 2010:54–55, 62–64.
- 52.Wheeler WK. Periostitis pubes following suprapubic cystostomy. J Urol. 1941;45:467. [Google Scholar]
- 53.World Health Organization. Treatment of Tuberculosis Guidelines. 4th ed.. Available at: http://whqlibdoc.who.int/publications/2010/9789241547833_eng.pdf. Accessed February 26, 2013.
- 54.Usandizaga M. [Tuberculosis of the pubic symphysis and labor][in Spanish] Acta Obstet Ginecol Hisp Lusit. 1969;17:302–309. [PubMed] [Google Scholar]
- 55.Vogelzang RL, Hendrix RW, Neiman HL. Computed tomography of tuberculous osteomyelitis of the pubis. J Comput Assist Tomogr. 1983;7:914–915. doi: 10.1097/00004728-198310000-00035. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.