Abstract
Background
Although infections are a major cause of morbidity and mortality after total joint arthroplasty (TJA), little is known about nationwide epidemiology and trends of infections after TJA.
Questions/purposes
We therefore determined (1) trends of postoperative pneumonia, urinary tract infection (UTI), surgical site infection (SSI), sepsis, and severe sepsis after TJA; (2) risk factors of these infections; (3) effect of these infections on length of stay (LOS) and hospital charges; and (4) the infection-related mortality rate and its predictors.
Methods
The International Classification of Diseases, 9th Revision codes were used to identify patients who underwent TJA and were diagnosed with aforementioned infections during hospitalization in the Nationwide Inpatient Sample database from 2002 to 2010. Multivariate analysis was performed to identify risk factors of these infections.
Results
Rates of pneumonia, UTI, SSI, sepsis, and severe sepsis were 0.74%, 3.26%, 0.31%, 0.25%, and 0.15%, respectively. Number of comorbidities and type of TJA were independent predictors of infection. Mortality decreased during the study period (odds ratio, 0.87; 95% confidence interval, 0.86–0.89). The median LOS was 3 days without complications but increased in the presence of SSI (median, 7 days), sepsis (median, 12 days), and severe sepsis (median, 15 days). Occurrence of pneumonia, sepsis, and severe sepsis increased risk of mortality 5.2, 8.5, and 66.2 times, respectively.
Conclusions
Rates of UTI, pneumonia, and SSI but not sepsis and severe sepsis are apparently decreasing. The likelihood of infection is increasing with number of comorbidities and revision surgeries. Rate of sepsis-related mortality is also decreasing.
Level of Evidence
Level II, prognostic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
THA and TKA are associated with substantial reductions in pain and restoration of function in patients with advance arthritis [8, 10, 26, 33]. However, postoperative complications may compromise the outcome of these procedures [22]. Postoperative infections and sepsis are major complications after total joint arthroplasty (TJA) because any postoperative infection increases the likelihood of mortality up to 32-fold [48] and, in the case of TJA, results in seeding of the implant and periprosthetic joint infection (PJI) [14, 40, 41]. Revision TJA resulting from PJI is associated with higher costs, increased length of hospital stay, and a 1% to 2.7% mortality rate [23]. It is estimated that the cost of treating PJI in the United States will exceed USD 1.62 billion by 2020 [25]. Moreover, postoperative sepsis and infection complications also increase patients’ morbidity and mortality, prolong hospital stay, and increase healthcare resource use regardless of PJI occurrence [3]. Therefore, any postoperative infection should be diagnosed and treated aggressively.
Postoperative sepsis and infection complications have been investigated widely using administrative databases such as the Nationwide Inpatient Sample (NIS) [4, 22, 48–50]. Bateman et al. [4] indicated postoperative sepsis and severe sepsis occur, respectively, in 0.9% and 0.5% of cases after all types of surgery. They showed an increase in the rate of postoperative severe sepsis from 0.3% to 0.9% from 1997 to 2006 but a parallel decline in the rate of in-hospital mortality after severe sepsis from 44.4% to 34.0% [4]. Vogel et al. [48], in a study not limited to patients undergoing TJA, indicated that age, sex, race, economic status of patients, and size and type of hospital are determinants of postoperative sepsis. Determining the epidemiologic pattern and risk factors of infection complications and sepsis after TJA will help physicians to recognize those patients who are at a greater risk of these complications and who may benefit from special care.
We used the NIS data to determine (1) trends of common postoperative infection complications (pneumonia, urinary tract infection [UTI], surgical site infection [SSI], sepsis, and severe sepsis) after TJA; (2) risk factors of these infection complications; (3) effect of postoperative infection and sepsis on length of stay (LOS) and total hospital charges; and (4) the mortality rate and its predictors resulting from postoperative infections in patients undergoing TJA.
Materials and Methods
We used the NIS data from 2002 to 2010 for this study. The NIS developed as part of the Healthcare Cost and Utilization Project of the Agency for Healthcare Research and Quality. The NIS database is the largest all-payer hospital database in the United States and by their estimate represents approximately 20% of all hospital inpatient stays [49] from approximately 1051 hospitals in 45 states. Because the NIS database has been sufficiently deidentified, this study was exempt from institutional review board review.
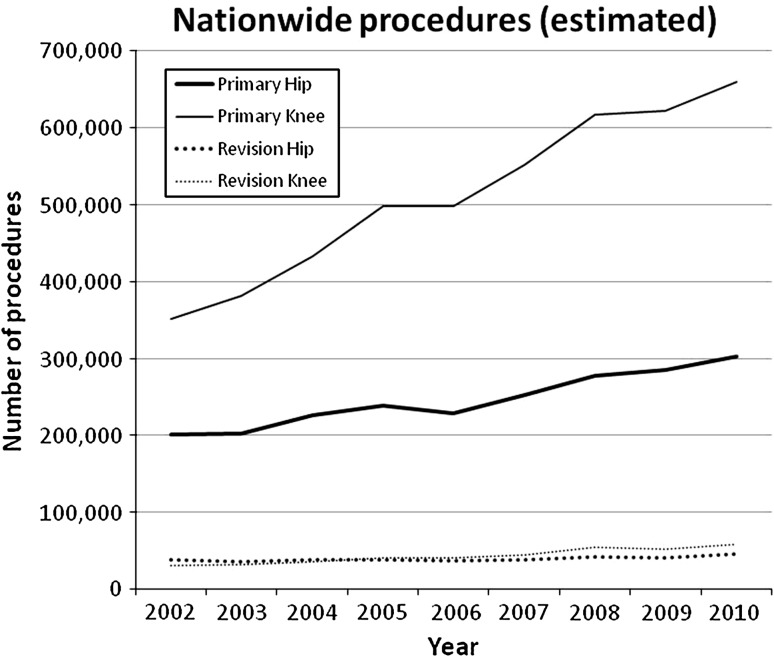
We ran a query based on the International Classification of Disease, 9th Revision, Clinical Modification (ICD-9-CM) codes to identify patients who underwent TJA. The ICD-9-CM codes of 81.51 for primary THA, 81.53 for revision THA, 81.54 for primary TKA, and 81.55 for revision TKA were used. The estimated nationwide total number of procedures increased for all types of TJA during the period from 2002 to 2010; however, the increase is more prominent in primary procedures (Fig. 1). Established ICD-9-CM codes were used to flag sepsis and infection complications and organ dysfunctions (Table 1). Sepsis was defined based on ICD-9 codes and severe sepsis was considered as sepsis with organ dysfunction [4]. Patients’ comorbidities were determined using the ICD-9 codes for the 29 Elixhauser comorbidities, which are tracked in the NIS database from 2002 on [18]. The Elixhauser comorbidity index has been used frequently in previous studies using the NIS data [13, 21, 43]. Based on recent studies, the Elixhauser comorbidity index performs well in predicting the outcome of patients [7, 11, 27] and based on the recent systematic review performed by Sharabiani et al. [42], the Elixhauser comorbidity index seems to be one of the best comorbidity indices for predicting outcome of patients in administrative databases. Therefore, in the present study, we decided to use this comorbidity index in the analyses.
Fig. 1.
The NIS data indicate that all TJAs are being performed in increasing numbers.
Table 1.
ICD-9-CM codes were used to detect postoperative infection complications and sepsis in patients who underwent total joint arthroplasty
| Infection complication | ICD-9-CM codes |
|---|---|
| Pneumonia | 997.3, 482.0–482.2, 482.3x, 482.4x, 482.81–482.83, 482.89, 482.9 |
| Urinary tract infection | 599.0, 996.64 |
| Surgical site infection | 998.31, 998.32, 998.5x |
| Streptococcal septicemia | 038.0 |
| Staphylococcal septicemia | 038.1 |
| Pneumococcal septicemia | 038.2 |
| Anaerobe septicemia | 038.3 |
| Gram-negative septicemia | 038.4 |
| Other specified septicemia | 038.8 |
| Unspecified septicemia | 038.9 |
| Systemic candidiasis | 112.5 |
| Systemic inflammatory response syndrome resulting from infectious process without organ dysfunction | 995.91 |
| Systemic inflammatory response syndrome resulting from infectious process with organ dysfunction | 995.92 |
| Septic shock | 785.52 |
| Organ dysfunction | |
| Cardiovascular | 427.5, 458,458.8, 458.9, 796.3, 785.5 |
| Respiratory | 518.5, 518.81, 418.82, 518.84, 786.09, 799.1 |
| Renal | 584 |
| Central nervous system | 293.0, 348.1, 348.3, 780.01 |
ICD-9-CM = International Classification of Diseases, 9th Revision, Clinical Modification.
Rates of UTI, SSI, pneumonia, sepsis, and severe sepsis were calculated for each year separately using number of TJAs performed in the corresponding year as the denominator. Mortality rates were also calculated in patients without sepsis, with sepsis, and severe sepsis separately. Multivariate logistic regression was performed to identify which factors were significantly associated with the occurrence of each of these infections. For each infection a full model was created using all available patient-level (demographics, comorbidities, surgery type) and hospital-level (region, type, size) variables, and then the model was simplified to remove all parameters not affecting the predictive power of the model. Factors affecting mortality were similarly modeled.
Total hospital charges in various years were adjusted to 2010 US dollars. Because neither total hospital charges nor LOS follow normal (Gaussian) distributions, bivariate comparisons between infected and noninfected cases were analyzed using the nonparametric Wilcoxon test. We used R 2.15.1 (R Foundation for Statistical Computing, Vienna, Austria) for all analyses and the “rms” package within R for the logistic regression.
Results
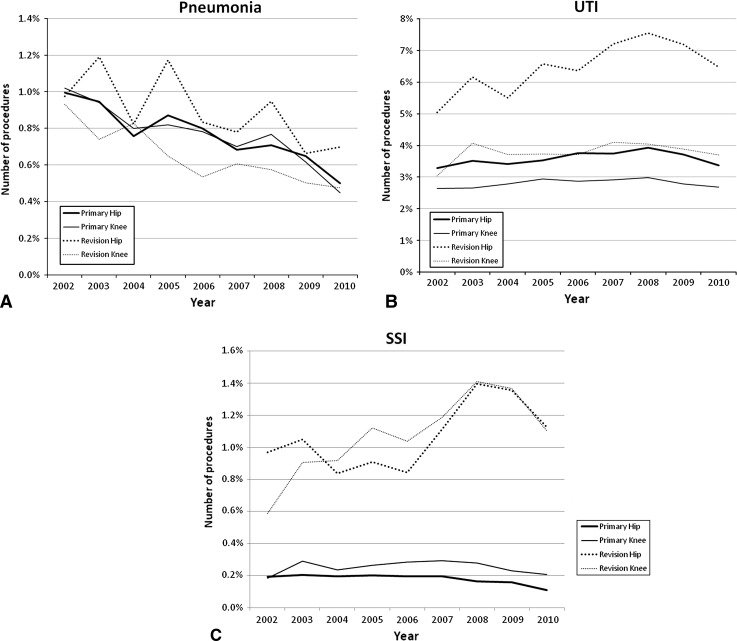
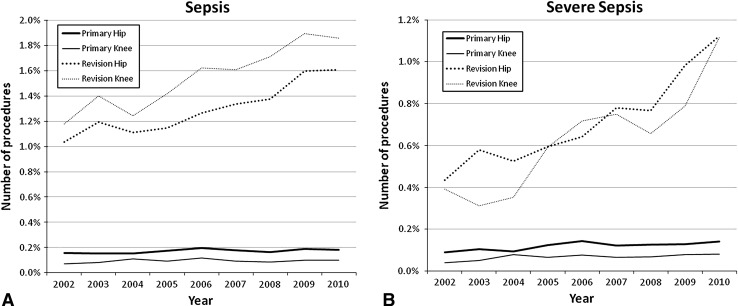
Overall rates of pneumonia, UTI, and SSI were 0.74%, 3.26%, and 0.31%, respectively, for the cases queried. Rates of pneumonia decreased over time (Fig. 2A). The multivariate model (Table 2) indicated that revision TKA had lower rates of pneumonia than each of the other surgeries. UTI (Fig. 2B) and SSI (Fig. 2C) rates were both relatively flat over the period queried, but the multivariate analysis indicates that when other demographic and clinical factors were controlled for, both infection rates would drop over time although not as sharply as pneumonia (odd ratio [OR], 0.98–0.99 per year versus 0.91 per year for pneumonia). Revision hip surgeries had the largest rates of UTI (6.47%), whereas revisions of either joint had higher rates of SSI (1.07% hip; 1.11% knee). Sepsis occurred in a total of 0.25% of cases after TJA; 0.15% of cases were severe sepsis (Fig. 3A–B). Revision surgeries were associated with greater rates of sepsis. Overall sepsis rates were 1.31% within revision hip and 1.60% within revision knee; severe sepsis rates were 0.73% in revision hip and 0.68% within revision knee.
Fig. 2A–C.
Nationwide trends of pneumonia (A), UTI (B), and SSI (C) are plotted by type of procedure. Controlling for demographic and clinical factors, these rates all tended to reduce by year.
Table 2.
Factors associated with infection complications in multivariate analysis
| Factor | Pneumonia | Urinary tract infection | Surgical site infection | ||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p value | OR | 95% CI | p value | OR | 95% CI | p value | |
| Age | 1.01 | 1.01–1.01 | < 0.001 | 1.04 | 1.03–1.04 | < 0.001 | – | – | NS |
| Elixhauser Comorbidity Index | 1.32 | 1.30–1.33 | < 0.001 | 1.31 | 1.30–1.31 | < 0.001 | 1.30 | 1.27–1.32 | < 0.001 |
| Female | 0.83 | 0.79–0.86 | < 0.001 | 2.13 | 12.07–2.19 | < 0.001 | 0.69 | 0.65–0.74 | < 0.001 |
| Hospital size | |||||||||
| Small | REF* | – | – | REF | – | – | REF | – | – |
| Medium | – | – | NS | 1.13 | 1.09–1.18 | < 0.001 | 1.12 | 1.01–1.24 | 0.04 |
| Large | 0.92 | 0.86–0.97 | < 0.001 | 1.18 | 1.14–1.22 | < 0.001 | – | – | NS |
| Hospital type | |||||||||
| Academic | REF | – | – | REF | – | – | REF | – | – |
| Rural | 0.78 | 0.72–0.83 | < 0.001 | 1.15 | 1.11–1.20 | < 0.001 | 0.73 | 0.65–0.81 | < 0.001 |
| Urban private | 0.75 | 0.71–0.80 | < 0.001 | 1.32 | 1.28–1.36 | < 0.001 | 0.84 | 0.77–0.92 | < 0.001 |
| Geographic region | |||||||||
| Northeast | REF | – | – | REF | – | – | REF | – | – |
| Midwest | 0.80 | 0.74–0.85 | < 0.001 | 1.08 | 1.04–1.12 | < 0.001 | 0.89 | 0.80–0.98 | 0.02 |
| South | 1.22 | 1.14–1.30 | < 0.001 | 0.86 | 0.82–0.89 | < 0.001 | – | – | NS |
| West | 0.85 | 0.81–0.89 | < 0.001 | 0.94 | 0.92–0.96 | < 0.001 | 1.11 | 1.04–1.20 | < 0.001 |
| Ethnicity | 1.12 | 0.98–1.28 | 0.07 | ||||||
| White | REF | – | – | REF | – | – | REF | – | – |
| Black | – | – | NS | 1.20 | 1.16–1.26 | < 0.001 | – | – | NS |
| Hispanic | – | – | NS | 1.21 | 1.15–1.28 | < 0.001 | 1.19 | 1.03–1.38 | 0.02 |
| Asian | 1.46 | 1.22–1.76 | < 0.001 | NS | NS | NS | 1.58 | 1.21–2.06 | < 0.001 |
| Native American | – | – | NS | 1.55 | 1.32–1.80 | < 0.001 | – | – | NS |
| Type of arthroplasty | |||||||||
| THA | 1.33 | 1.19–1.49 | < 0.001 | 1.43 | 1.39–1.46 | < 0.001 | 1.34 | 1.13–1.58 | < 0.001 |
| TKA | 1.28 | 1.15–1.43 | < 0.001 | – | – | NS | 0.85 | 0.78–0.93 | < 0.001 |
| Revision THA | 1.44 | 1.25–1.65 | < 0.001 | 2.38 | 2.28–2.47 | < 0.001 | – | – | NS |
| Revision TKA | – | – | NS | 1.41 | 1.34–1.47 | < 0.001 | – | – | NS |
| Insurance | |||||||||
| Medicare | REF | – | – | REF | – | – | REF | – | – |
| Medicaid | – | – | NS | 1.36 | 1.27–1.46 | < 0.001 | – | – | NS |
| Private | – | – | NS | 0.93 | 0.90–0.96 | < 0.001 | 2.29 | 1.77–2.96 | < 0.001 |
| Self–pay | – | – | NS | 1.37 | 1.18–1.59 | < 0.001 | 3.29 | 2.55–4.23 | < 0.001 |
| No charge | – | – | NS | 1.77 | 1.33–2.35 | < 0.001 | 12.18 | 9.45–15.69 | < 0.001 |
| Other | – | – | NS | – | – | NS | 12.79 | 9.96–16.43 | < 0.001 |
| Year | 0.91 | 0.90–0.91 | < 0.001 | 0.99 | 0.99–1.00 | 0.001 | 0.98 | 0.97–0.99 | 0.003 |
* For factors with more than two categories, the reference category is labeled REF; OR = odds ratio; CI = confidence interval; NS = not significant.
Fig. 3A–B.
Trends of sepsis (A) and severe sepsis (B) from 2002 to 2010. Rates of any sepsis (severe or not severe) or severe alone increase annually.
Logistic regression models (Table 2) showed that all three infection (pneumonia, UTI, and SSI) rates declined with year; however, the rate was largest in pneumonia. Revision THA was predicted to have the largest rates of UTI (OR, 2.38; 95% confidence interval [CI], 2.28–2.35). The large OR seen when primary insurance was no charge or other suggested the payer field reflects change in responsibility when an SSI occurs. Recomputing the model excluding primary payer, the ORs for revision THA became 12.39 (95% CI, 9.62–15.95) and for revision TKA 12.90 (95% CI, 10.05–16.57) with a negligible effect on other parameters. Revision surgery was a major risk factor for sepsis or severe sepsis and rates increased over time (Table 3). Patients on Medicaid were likelier to develop any sepsis; however, this effect was not as strong as for severe sepsis (OR, 1.74 versus OR, 1.13).
Table 3.
Factors associated with sepsis and severe sepsis in multivariate analysis
| Factor | Any sepsis | Severe sepsis | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p value | OR | 95% CI | p value | |
| Age | 1.03 | 1.03–1.04 | < 0.001 | 1.03 | 1.02–1.03 | < 0.001 |
| Elixhauser Comorbidity Index | 1.63 | 1.59–1.67 | < 0.001 | 1.64 | 1.63–1.65 | < 0.001 |
| Female | 0.54 | 0.49–0.58 | < 0.001 | 0.69 | 0.68–0.70 | < 0.001 |
| Hospital size | ||||||
| Small | REF* | – | – | REF | – | – |
| Medium | 1.56 | 1.33–1.83 | < 0.001 | 1.13 | 1.10–1.16 | < 0.001 |
| Large | 1.63 | 1.41–1.89 | < 0.001 | 1.15 | 1.12–1.18 | < 0.001 |
| Geographic region | ||||||
| Northeast | REF | – | – | REF | – | – |
| Midwest | 0.85 | 0.74–0.98 | 0.02 | 1.13 | 1.10–1.16 | < 0.001 |
| South | – | – | NS | 1.17 | 1.15–1.20 | < 0.001 |
| West | – | – | NS | – | – | NS |
| Ethnicity | ||||||
| White | REF | – | – | REF | – | – |
| Black | – | – | NS | 1.05 | 1.02–1.09 | < 0.001 |
| Hispanic | – | – | NS | – | – | NS |
| Asian | – | – | NS | 1.20 | 1.11–1.30 | < 0.001 |
| Native American | – | – | NS | – | – | NS |
| Type of arthroplasty | ||||||
| THA | 1.72 | 1.53–1.92 | < 0.001 | 1.78 | 1.54–2.06 | < 0.001 |
| TKA | – | – | NS | 1.27 | 1.10–1.47 | < 0.001 |
| Revision THA | 7.76 | 6.91–8.71 | < 0.001 | 2.50 | 2.16–2.89 | < 0.001 |
| Revision TKA | 8.07 | 7.20–9.06 | < 0.001 | 1.57 | 1.35–1.81 | < 0.001 |
| Insurance | ||||||
| Medicare | REF | – | – | REF | – | – |
| Medicaid | 1.74 | 1.39–2.18 | < 0.001 | 1.13 | 1.07–1.19 | < 0.001 |
| Private | 0.78 | 0.68–0.88 | < 0.001 | 0.96 | 0.94–0.98 | < 0.001 |
| Self-pay | – | – | NS | 1.26 | 1.12–1.41 | 0.22 |
| No charge | – | – | NS | – | – | NS |
| Other | 0.70 | 0.51–0.96 | 0.03 | – | – | NS |
| Year | 1.04 | 1.02–1.05 | < 0.001 | 1.08 | 1.08–1.09 | < 0.0001 |
* For factors with more than two categories, the reference category is labeled REF; OR = odds ratio; CI = confidence interval; NS = not significant.
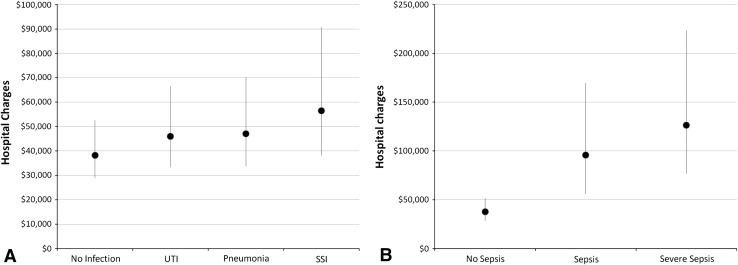
Median LOS was 3 days (interquartile range [IQR], 3–4 days) in patients without infection complications. LOS increased in the presence of SSI (median, 7 days; IQR, 5–11 days; p < 0.001), sepsis (median, 12 days; IQR, 7–20 days; p < 0.001), and severe sepsis (median, 15 days; IQR, 9–24; p < 0.001). Median hospital charges increased with the presence of any infection (pneumonia, UTI, or SSI) but this trend was small compared with the overall variation in charges (Fig. 4A). A more striking increase in total charges is produced by the presence of sepsis (Fig. 4B).
Fig. 4A–B.
Comparison of hospitalization charges between patients without any infection and those with UTI or SSI and pneumonia (A) and a similar comparison between patients without sepsis and those with sepsis of any kind or those with specifically severe sepsis (B). Figures demonstrate infections increase hospital charges in patients having TJA.
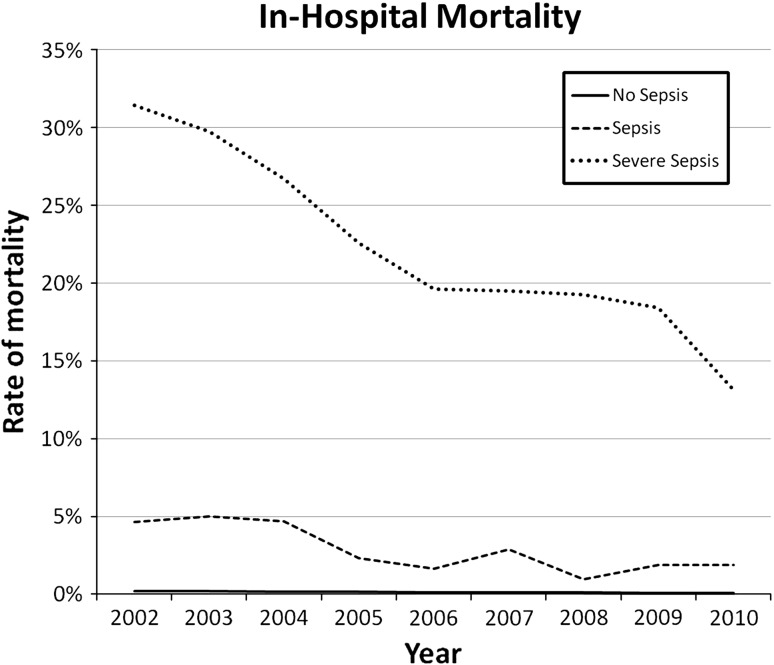
Total rate of mortality in patients was 0.14% but increased to 12.97% and 20.31% in patients with sepsis and severe sepsis, respectively (Fig. 5). Logistic regression analysis confirmed that mortality decreased during the study period (OR, 0.87; 95% CI, 0.86–0.89; p < 0.001). Occurrence of pneumonia, sepsis, and severe sepsis increased risk of mortality 5.23, 8.56, and 66.27 times, respectively (Table 4).
Fig. 5.
Rate of mortality after TJA decreases per year but is sharply increased by the presence of sepsis.
Table 4.
Factors associated with mortality in multivariate analysis
| Factor | OR | 95% CI | p value |
|---|---|---|---|
| Age | 1.08 | 1.03–1.04 | < 0.001 |
| Elixhauser Comorbidity Index | 1.36 | 1.32–1.40 | < 0.001 |
| Female | 0.67 | 0.61–0.74 | < 0.001 |
| Geographic region | |||
| Northeast | REF | – | – |
| Midwest | 0.84 | 0.73–0.98 | 0.03 |
| South | – | – | NS |
| West | 0.71 | 0.61–0.82 | NS |
| Ethnicity | |||
| White | REF | – | – |
| Black | 1.50 | 1.26–1.79 | < 0.001 |
| Hispanic | – | – | NS |
| Asian | – | – | NS |
| Native American | – | – | NS |
| Type of arthroplasty | |||
| THA | 1.84 | 1.66–2.03 | < 0.001 |
| TKA | – | – | NS |
| Revision THA | 2.94 | 2.58–3.37 | < 0.001 |
| Revision TKA | – | – | NS |
| Insurance | |||
| Medicare | REF | – | – |
| Medicaid | 1.92 | 1.40–2.63 | < 0.001 |
| Private | – | – | NS |
| Self-pay | 2.07 | 1.14–3.75 | 0.016 |
| No charge | – | – | NS |
| Other | 0.70 | 0.51–0.96 | 0.03 |
| Year | 0.88 | 0.86–0.89 | < 0.001 |
| UTI | 1.47 | 1.27–1.71 | < 0.001 |
| Pneumonia | 5.23 | 4.35–6.30 | < 0.001 |
| Sepsis | 8.56 | 5.97–12.28 | < 0.001 |
| Severe sepsis | 66.28 | 57.18–76.81 | < 0.001 |
* For factors with more than two categories, the reference category is labeled REF; OR = odds ratio; CI = confidence interval; NS = not significant; UTI = urinary tract infection.
Discussion
Any infection after TJA should be considered as a serious complication and treated aggressively because of the possibility of seeding the prosthesis leading to PJI [14, 40, 41]. However, national epidemiologic pattern, trends, and impact of postoperative infections and sepsis on LOS and hospital charges after TJA have not yet well defined. Using nationally representative data, the present study aims to determine (1) trends of postoperative infections including pneumonia, UTI, SSI, sepsis, and severe sepsis after TJA; (2) risk factors of these infections; (3) effect of postoperative infection and sepsis on LOS and total hospital charges; and (4) the infection-related mortality rate and its predictors.
The present study, similar to previous reports from administrative databases, has some limitations that should be highlighted before discussing our findings. First, we only tried to illustrate epidemiologic patterns and risk factors of infection complications and sepsis after TJA. We were not able to explore the cause of some findings because many factors contribute to development of postoperative infection and sepsis that are not available in the NIS database. Where possible, numerous relevant variables that might affect infection complications were included in the multivariate models. Second, the NIS database provides only in-hospital complications and mortality and patients cannot be followed up after hospital discharge. Therefore, it is expected that the rate of postoperative infection, sepsis, and mortality would be higher than what we found. A relatively lower rate of SSI in this study compared with the reported incidence in the literature [32, 38, 46] can be explained by missing postdischarge SSI episodes in this study. Although the incidence of SSI after TJA varies in different reports, the incidence of SSI after primary TJA in our study was always less than 0.4%, much lower than the incidence of 0.7% to 1.8% in the literature [6]. Third, the ICD-9 codes used in the NIS database are subject to variation in definition of complications and unintentional errors [47] between different hospitals. Administrative coding is reportedly inaccurate for detecting infection complications [20, 44, 45, 51]; however, using administrative databases is the most feasible and cost-effective method to evaluate epidemiologic pattern of infection complications after TJA. Fourth, we did not control for other in-hospital systemic complications such as cardiovascular and renal complications, stroke, venous thromboembolism, and other systemic infections that can affect LOS of hospitalization. Given the relatively low incidence of these systemic complications after TJA, and that our analysis controlled for other variables that can influence development of these complications, we believe the results of the present study are less likely to be affected by this limitation.
Literature reports show considerable variation in the rates of postoperative sepsis and infection complications likely resulting from differences in methodology and definition of complications (Table 5); these differences make comparison of the data and conclusions difficult. Because we took only in-hospital complications into account, the rate of infections may be lower than studies with longer followup. According to our findings, rates of SSI, UTI, and pneumonia but not sepsis and severe sepsis are decreasing. The increasing trends in sepsis and severe sepsis rates are consistent with previous reports [4, 17, 28] but causes of this increase cannot be investigated by the NIS data. The decline in the rate of SSI in recent years is interesting because Kurtz et al. [25], using the NIS data set, had previously described increasing rates of PJI after TJA. Because we did not query for specific ICD-9 codes for PJI, our findings may reflect mainly superficial SSI that can explain this discrepancy. Moreover, reduction in LOS in recent decades results in an underestimation of in-hospital infection complications including SSI after TJA. Some of these patients will be readmitted to the hospital during the first month after the index TJA [12].
Table 5.
Rate of infection complications, sepsis, and severe sepsis in the current study and some previous reports
| Study | Surgery | Database | Followup | Sepsis | Severe sepsis | SSI | PJI | UTI | Pneumonia |
|---|---|---|---|---|---|---|---|---|---|
| Pulido et al. [35] | TJA | Single institute | 43 months | NR | NR | NR | 0.7% | NR | NR |
| Parvizi et al. [31] | TJA | Single institute | 6 weeks | NR | NR | 0.46% (superficial SSI) | NR | 2.09% | 0.16% |
| Pulido et al. [36] | TJA | Single institute | In-hospital | 0.05% | NR | 0.27% | 0.08% | 1.36% | 0.15% |
| Cram et al. [12] | TKA | Medicare | 30 days | 0.1%–0.2% | NR | 0.4%–0.6% | NR | NR | NR |
| Peersman et al. [32] | TKA | Single institute | Up to 156 months | NR | NR | 0.39%–1.06% | – | NR | NR |
| Bozic et al. [9] | THA | Medicare | 2 years | NR | NR | NR | 2.07% | NR | NR |
| Namba et al. [29] | THA | Multiinstitute | 72 days | NR | NR | 0.51% (deep SSI) | NR | NR | NR |
| Bateman et al. [4] | Elective orthopaedic and non-orthopaedic operations | NIS | In-hospital | 0.9% | 0.5% | NR | NR | NR | NR |
| Vogel et al. [48] | Elective non-orthopaedic surgery | NIS | In-hospital | 1.21% | NR | NR | NA | NR | NR |
| Vogel et al. [49] | Vascular surgery | NIS | In-hospital | 0.08%-2.06% | NR | 0.08%–1.38% | NA | 0.77%–2.86% | 0.63%–6.63% |
| Current study | TJA | NIS | In-hospital | 0.25% | 0.15% | 0.31% | NR | 3.26% | 0.74% |
SSI = surgical site infection; PJI = periprosthetic joint infection; UTI = urinary tract infection; NIS = Nationwide Inpatient Sample; TJA = total joint arthroplasty; NR = not reported; NA = not applicable.
Our findings are consistent with previous reports indicating a lower rate of sepsis and severe sepsis as well as sepsis-related mortality in females than males [1, 4, 16, 52]. The sex discrepancy in development and outcome of infection and sepsis can be partly explained by the action of sex hormones on immune system function. Estrogen enhances immune function [2] and may even result in autoimmune disorders, whereas testosterone suppresses immune function [2, 5]. Moreover, variations in societal role and exposures of male and females may also play a role [5]. UTI was the only infection that was observed more frequently in females because it was expected and has been previously reported that women are at greater risk of UTI after TJA [19]. We found race can affect occurrence of some of the infectious complications and sepsis. As has been suggested, race can be an indicator for secondary issues that can affect incidence and outcome of infectious complications and sepsis, whereas they cannot be explored using administrative databases [47]. Race can indirectly indicate preexisting comorbidities and socioeconomic status [47]. Type of insurance that facilitates healthcare access was another factor that came up in multivariate analysis as an independent predictor of some of the infectious complications. Our results are consistent with those of O’Brien et al. [30] that showed patients with Medicaid insurance are at greater risk for development of sepsis and in-hospital mortality. This increased risk might be attributable to higher preexisting comorbidities, which were not considered in the Elixhauser comorbidities as well as access to healthcare facilities.
We found that development of postoperative SSI, sepsis, and severe sepsis prolongs LOS and increases hospital charges consistent with previous reports [24, 34]. It has been found that in surgical patients, development of postoperative complications such as infections will prolong LOS, which consequently may increase hospital charges [15, 49]. Development of postoperative infections delays hospital discharge until appropriate workup and treatment are performed.
Using data from National Hospital Discharge Survey, Martin et al. [28] showed that the incidence of sepsis and the number of sepsis-related deaths increased, whereas the overall in-hospital mortality rate of sepsis declined from 1979 to 2000. Similarly, a later study by Dombrovskiy et al. [17] also indicated the rate of in-hospital sepsis-related mortality increased from 1993 to 2003. These two studies [17, 28] reported any sepsis leading to hospitalization including both medical and surgical cases. In contrary, the study by Bateman et al. [4], which only included postoperative severe sepsis from the NIS data, indicated decline in the rate of in-hospital severe sepsis-related mortality from 1997 to 2006. Similar to this study [4], we also found a decline in the sepsis-related mortality rate. Decline in the mortality rate may be explained by improvement in monitoring of patients and early diagnosis of sepsis during hospitalization (indicated by an increase in the number of sepsis during the study period), early goal-directed therapy [39], and introducing new drugs for treatment of sepsis [37].
Our data and analyses suggest the rates of UTI, pneumonia, and SSI are decreasing after TJA. The likelihood of infection is increasing with number of comorbidities and revision surgeries, whereas female sex is protective against sepsis and the majority of infection complications except UTI. The rates of sepsis and severe sepsis after TJA are increasing, whereas the rate of sepsis-related mortality is decreasing.
Footnotes
One of the authors (JP) certifies that he has or may receive payments or benefits, in any one year, an amount in excess of USD 10,000 from Zimmer (Warsaw, IN, USA), Smith & Nephew (Memphis, TN, USA), and ConvaTec (Princeton, NJ, USA). One of the authors (WJH) certifies that he has or may receive payments or benefits, in any one year, an amount in excess of USD 10,000 from Stryker Orthopaedics (Mahwah, NJ, USA).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
This study was exempt from review by the institutional review board because the Nationwide Inpatient Sample (NIS) database has been sufficiently deidentified.
References
- 1.Adrie C, Azoulay E, Francais A, Clec’h C, Darques L, Schwebel C, Nakache D, Jamali S, Goldgran-Toledano D, Garrouste-Orgeas M, Timsit JF. Influence of gender on the outcome of severe sepsis: a reappraisal. Chest. 2007;132:1786–1793. doi: 10.1378/chest.07-0420. [DOI] [PubMed] [Google Scholar]
- 2.Angele MK, Schwacha MG, Ayala A, Chaudry IH. Effect of gender and sex hormones on immune responses following shock. Shock. 2000;14:81–90. doi: 10.1097/00024382-200014020-00001. [DOI] [PubMed] [Google Scholar]
- 3.Barnes CL. Overview: the health care burden and financial costs of surgical site infections. Am J Orthop (Belle Mead NJ). 2011;40:2–5. [PubMed] [Google Scholar]
- 4.Bateman BT, Schmidt U, Berman MF, Bittner EA. Temporal trends in the epidemiology of severe postoperative sepsis after elective surgery: a large, nationwide sample. Anesthesiology. 2010;112:917–925. doi: 10.1097/ALN.0b013e3181cea3d0. [DOI] [PubMed] [Google Scholar]
- 5.Beery TA. Sex differences in infection and sepsis. Crit Care Nurs Clin North Am. 2003;15:55–62. doi: 10.1016/S0899-5885(02)00028-X. [DOI] [PubMed] [Google Scholar]
- 6.Bolon MK, Hooper D, Stevenson KB, Greenbaum M, Olsen MA, Herwaldt L, Noskin GA, Fraser VJ, Climo M, Khan Y, Vostok J, Yokoe DS, Centers for Disease Control and Prevention Epicenters Program Improved surveillance for surgical site infections after orthopedic implantation procedures: extending applications for automated data. Clin Infect Dis. 2009;48:1223–1229. doi: 10.1086/597584. [DOI] [PubMed] [Google Scholar]
- 7.Bottle A, Aylin P. Comorbidity scores for administrative data benefited from adaptation to local coding and diagnostic practices. J Clin Epidemiol. 2011;64:1426–1433. doi: 10.1016/j.jclinepi.2011.04.004. [DOI] [PubMed] [Google Scholar]
- 8.Bozic KJ, Kurtz SM, Lau E, Ong K, Chiu V, Vail TP, Rubash HE, Berry DJ. The epidemiology of revision total knee arthroplasty in the United States. Clin Orthop Relat Res. 2010;468:45–51. doi: 10.1007/s11999-009-0945-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bozic KJ, Ong K, Lau E, Berry DJ, Vail TP, Kurtz SM, Rubash HE. Estimating risk in Medicare patients with THA: an electronic risk calculator for periprosthetic joint infection and mortality. Clin Orthop Relat Res. 2013;471:574–583. doi: 10.1007/s11999-012-2605-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Carr AJ, Robertsson O, Graves S, Price AJ, Arden NK, Judge A, Beard DJ. Knee replacement. Lancet. 2012;379:1331–1340. doi: 10.1016/S0140-6736(11)60752-6. [DOI] [PubMed] [Google Scholar]
- 11.Chu YT, Ng YY, Wu SC. Comparison of different comorbidity measures for use with administrative data in predicting short- and long-term mortality. BMC Health Serv Res. 2010;10:140. doi: 10.1186/1472-6963-10-140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cram P, Lu X, Kates SL, Singh JA, Li Y, Wolf BR. Total knee arthroplasty volume, utilization, and outcomes among Medicare beneficiaries, 1991–2010. JAMA. 2012;308:1227–1236. doi: 10.1001/2012.jama.11153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Csikesz NG, Nguyen LN, Tseng JF, Shah SA. Nationwide volume and mortality after elective surgery in cirrhotic patients. J Am Coll Surg. 2009;208:96–103. doi: 10.1016/j.jamcollsurg.2008.09.006. [DOI] [PubMed] [Google Scholar]
- 14.David TS, Vrahas MS. Perioperative lower urinary tract infections and deep sepsis in patients undergoing total joint arthroplasty. J Am Acad Orthop Surg. 2000;8:66–74. doi: 10.5435/00124635-200001000-00007. [DOI] [PubMed] [Google Scholar]
- 15.Dimick JB, Chen SL, Taheri PA, Henderson WG, Khuri SF, Campbell DA., Jr Hospital costs associated with surgical complications: a report from the private-sector National Surgical Quality Improvement Program. J Am Coll Surg. 2004;199:531–537. doi: 10.1016/j.jamcollsurg.2004.05.276. [DOI] [PubMed] [Google Scholar]
- 16.Diodato MD, Knoferl MW, Schwacha MG, Bland KI, Chaudry IH. Gender differences in the inflammatory response and survival following haemorrhage and subsequent sepsis. Cytokine. 2001;14:162–169. doi: 10.1006/cyto.2001.0861. [DOI] [PubMed] [Google Scholar]
- 17.Dombrovskiy VY, Martin AA, Sunderram J, Paz HL. Rapid increase in hospitalization and mortality rates for severe sepsis in the United States: a trend analysis from 1993 to 2003. Crit Care Med. 2007;35:1244–1250. doi: 10.1097/01.CCM.0000261890.41311.E9. [DOI] [PubMed] [Google Scholar]
- 18.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 19.Iorio R, Whang W, Healy WL, Patch DA, Najibi S, Appleby D. The utility of bladder catheterization in total hip arthroplasty. Clin Orthop Relat Res. 2005;432:148–152. doi: 10.1097/01.blo.0000149823.57513.00. [DOI] [PubMed] [Google Scholar]
- 20.Jhung MA, Banerjee SN. Administrative coding data and health care-associated infections. Clin Infect Dis. 2009;49:949–955. doi: 10.1086/605086. [DOI] [PubMed] [Google Scholar]
- 21.Kaplan GG, Hubbard J, Panaccione R, Shaheen AA, Quan H, Nguyen GC, Dixon E, Ghosh S, Myers RP. Risk of comorbidities on postoperative outcomes in patients with inflammatory bowel disease. Arch Surg. 2011;146:959–964. doi: 10.1001/archsurg.2011.194. [DOI] [PubMed] [Google Scholar]
- 22.Kirksey M, Chiu YL, Ma Y, Gonzalez Della Valle A, Poultsides L, Gerner P, Memtsoudis SG. Trends in in-hospital major morbidity and mortality after total joint arthroplasty: United States 1998–2008. Anesth Analg. 2012;115:321–327. doi: 10.1213/ANE.0b013e31825b6824. [DOI] [PubMed] [Google Scholar]
- 23.Koulouvaris P, Sculco P, Finerty E, Sculco T, Sharrock NE. Relationship between perioperative urinary tract infection and deep infection after joint arthroplasty. Clin Orthop Relat Res. 2009;467:1859–1867. doi: 10.1007/s11999-008-0614-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kurtz SM, Lau E, Schmier J, Ong KL, Zhao K, Parvizi J. Infection burden for hip and knee arthroplasty in the United States. J Arthroplasty. 2008;23:984–991. doi: 10.1016/j.arth.2007.10.017. [DOI] [PubMed] [Google Scholar]
- 25.Kurtz SM, Lau E, Watson H, Schmier JK, Parvizi J. Economic burden of periprosthetic joint infection in the United States. J Arthroplasty. 2012;27(Suppl):61–65.e1. [DOI] [PubMed]
- 26.Kurtz SM, Ong KL, Schmier J, Zhao K, Mowat F, Lau E. Primary and revision arthroplasty surgery caseloads in the United States from 1990 to 2004. J Arthroplasty. 2009;24:195–203. doi: 10.1016/j.arth.2007.11.015. [DOI] [PubMed] [Google Scholar]
- 27.Li B, Evans D, Faris P, Dean S, Quan H. Risk adjustment performance of Charlson and Elixhauser comorbidities in ICD-9 and ICD-10 administrative databases. BMC Health Serv Res. 2008;8:12. doi: 10.1186/1472-6963-8-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Martin GS, Mannino DM, Eaton S, Moss M. The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med. 2003;348:1546–1554. doi: 10.1056/NEJMoa022139. [DOI] [PubMed] [Google Scholar]
- 29.Namba RS, Inacio MC, Paxton EW. Risk factors associated with surgical site infection in 30,491 primary total hip replacements. J Bone Joint Surg Br. 2012;94:1330–1338. doi: 10.2106/JBJS.K.01363. [DOI] [PubMed] [Google Scholar]
- 30.O’Brien JM, Jr, Lu B, Ali NA, Levine DA, Aberegg SK, Lemeshow S. Insurance type and sepsis-associated hospitalizations and sepsis-associated mortality among US adults: a retrospective cohort study. Crit Care. 2011;15:R130. doi: 10.1186/cc10243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Parvizi J, Mui A, Purtill JJ, Sharkey PF, Hozack WJ, Rothman RH. Total joint arthroplasty: when do fatal or near-fatal complications occur? J Bone Joint Surg Am. 2007;89:27–32. doi: 10.2106/JBJS.E.01443. [DOI] [PubMed] [Google Scholar]
- 32.Peersman G, Laskin R, Davis J, Peterson M. Infection in total knee replacement: a retrospective review of 6489 total knee replacements. Clin Orthop Relat Res. 2001;392:15–23. doi: 10.1097/00003086-200111000-00003. [DOI] [PubMed] [Google Scholar]
- 33.Pivec R, Johnson AJ, Mears SC, Mont MA. Hip arthroplasty. Lancet. 2012;380:1768–1777. doi: 10.1016/S0140-6736(12)60607-2. [DOI] [PubMed] [Google Scholar]
- 34.Poultsides LA, Ma Y, Della Valle AG, Chiu YL, Sculco TP, Memtsoudis SG. In-hospital surgical site infections after primary hip and knee arthroplasty—incidence and risk factors. J Arthroplasty. 2012 Nov 8 [Epub ahead of print]. [DOI] [PubMed]
- 35.Pulido L, Ghanem E, Joshi A, Purtill JJ, Parvizi J. Periprosthetic joint infection: the incidence, timing, and predisposing factors. Clin Orthop Relat Res. 2008;466:1710–1715. doi: 10.1007/s11999-008-0209-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pulido L, Parvizi J, Macgibeny M, Sharkey PF, Purtill JJ, Rothman RH, Hozack WJ. In hospital complications after total joint arthroplasty. J Arthroplasty. 2008;23(Suppl 1):139–145. doi: 10.1016/j.arth.2008.05.011. [DOI] [PubMed] [Google Scholar]
- 37.Rice TW, Bernard GR. Therapeutic intervention and targets for sepsis. Annu Rev Med. 2005;56:225–248. doi: 10.1146/annurev.med.56.082103.104356. [DOI] [PubMed] [Google Scholar]
- 38.Ridgeway S, Wilson J, Charlet A, Kafatos G, Pearson A, Coello R. Infection of the surgical site after arthroplasty of the hip. J Bone Joint Surg Br. 2005;87:844–850. doi: 10.1302/0301-620X.87B6.15121. [DOI] [PubMed] [Google Scholar]
- 39.Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, Peterson E, Tomlanovich M, Early Goal-Directed Therapy Collaborative Group Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345:1368–1377. doi: 10.1056/NEJMoa010307. [DOI] [PubMed] [Google Scholar]
- 40.Rodriguez D, Pigrau C, Euba G, Cobo J, Garcia-Lechuz J, Palomino J, Riera M, Del Toro MD, Granados A, Ariza X. Acute haematogenous prosthetic joint infection: prospective evaluation of medical and surgical management. Clin Microbiol Infect. 2010;16:1789–1795. doi: 10.1111/j.1469-0691.2010.03157.x. [DOI] [PubMed] [Google Scholar]
- 41.Sendi P, Banderet F, Graber P, Zimmerli W. Periprosthetic joint infection following Staphylococcus aureus bacteremia. J Infect. 2011;63:17–22. doi: 10.1016/j.jinf.2011.05.005. [DOI] [PubMed] [Google Scholar]
- 42.Sharabiani MT, Aylin P, Bottle A. Systematic review of comorbidity indices for administrative data. Med Care. 2012;50:1109–1118. doi: 10.1097/MLR.0b013e31825f64d0. [DOI] [PubMed] [Google Scholar]
- 43.Shen Y, Silverstein JC, Roth S. In-hospital complications and mortality after elective spinal fusion surgery in the United States: a study of the Nationwide Inpatient Sample from 2001 to 2005. J Neurosurg Anesthesiol. 2009;21:21–30. doi: 10.1097/ANA.0b013e31818b47e9. [DOI] [PubMed] [Google Scholar]
- 44.Stamm AM, Bettacchi CJ. A comparison of 3 metrics to identify health care-associated infections. Am J Infect Control. 2012;40:688–691. doi: 10.1016/j.ajic.2012.01.033. [DOI] [PubMed] [Google Scholar]
- 45.Stevenson KB, Khan Y, Dickman J, Gillenwater T, Kulich P, Myers C, Taylor D, Santangelo J, Lundy J, Jarjoura D, Li X, Shook J, Mangino JE. Administrative coding data, compared with CDC/NHSN criteria, are poor indicators of health care-associated infections. Am J Infect Control. 2008;36:155–164. doi: 10.1016/j.ajic.2008.01.004. [DOI] [PubMed] [Google Scholar]
- 46.Urquhart DM, Hanna FS, Brennan SL, Wluka AE, Leder K, Cameron PA, Graves SE, Cicuttini FM. Incidence and risk factors for deep surgical site infection after primary total hip arthroplasty: a systematic review. J Arthroplasty. 2010;25:1216-1222.e1211-1213. [DOI] [PubMed]
- 47.Vogel TR. Update and review of racial disparities in sepsis. Surg Infect (Larchmt). 2012;13:203–208. doi: 10.1089/sur.2012.124. [DOI] [PubMed] [Google Scholar]
- 48.Vogel TR, Dombrovskiy VY, Carson JL, Graham AM, Lowry SF. Postoperative sepsis in the United States. Ann Surg. 2010;252:1065–1071. doi: 10.1097/SLA.0b013e3181dcf36e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Vogel TR, Dombrovskiy VY, Carson JL, Haser PB, Lowry SF, Graham AM. Infectious complications after elective vascular surgical procedures. J Vasc Surg. 2010;51:122–129. doi: 10.1016/j.jvs.2009.08.006. [DOI] [PubMed] [Google Scholar]
- 50.Vogel TR, Dombrovskiy VY, Lowry SF. Trends in postoperative sepsis: are we improving outcomes? Surg Infect (Larchmt). 2009;10:71–78. doi: 10.1089/sur.2008.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.West J, Khan Y, Murray DM, Stevenson KB. Assessing specific secondary ICD-9-CM codes as potential predictors of surgical site infections. Am J Infect Control. 2010;38:701–705. doi: 10.1016/j.ajic.2010.03.015. [DOI] [PubMed] [Google Scholar]
- 52.Wichmann MW, Inthorn D, Andress HJ, Schildberg FW. Incidence and mortality of severe sepsis in surgical intensive care patients: the influence of patient gender on disease process and outcome. Intensive Care Med. 2000;26:167–172. doi: 10.1007/s001340050041. [DOI] [PubMed] [Google Scholar]