Abstract
Background
Tardy ulnar nerve palsy is a common late complication of traumatic cubitus valgus deformity. Whether both problems can be corrected together, safely and effectively, in a single surgical procedure remains unknown.
Questions/purposes
We therefore reviewed a patient cohort having this combined surgery and compared preoperatively and at a minimum of 24 months postoperatively (1) active elbow ROM; (2) radiographic correction of the cubitus valgus deformity of the preoperative and postoperative humerus-elbow-wrist angles and the medial prominence index; (3) ulnar nerve function through grip strength and static two-point discrimination; and (4) overall upper limb disability by the DASH score.
Methods
Between 2004 and 2009, 13 patients who had traumatic cubitus valgus deformities and tardy ulnar nerve palsy (Dellon’s Grade III) were treated with simultaneous supracondylar dome osteotomy and anterior transposition of the ulnar nerve and were reviewed retrospectively. The minimum followup was 24 months (mean, 33 months; range, 24–52 months).
Results
The mean preoperative ROM was 16° to 124° and mean postoperative ROM was 10° to 126°. All osteotomies healed uneventfully. The mean postoperative humerus-elbow-wrist angle was 11° and the average correction was 24°. None of the patients had recurrence of the deformity or residual prominence of the medial condyle at the last followup. The mean grip strength and static two-point discrimination improved from 20 kg of force and 6.9 mm to 27 kg of force and 4.0 mm (p = 0.002 and p = 0.004, respectively). Subjective ulnar nerve symptoms improved in all but one patient. The mean DASH score improved from 29 points to 16 points (p = 0.001).
Conclusion
A combined supracondylar dome osteotomy and anterior transposition of the ulnar nerve is effective in correcting posttraumatic cubitus valgus deformity and its associated ulnar nerve palsy.
Level of Evidence
Level IV, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Tardy ulnar nerve palsy is a common late complication of traumatic cubitus valgus deformity resulting from nonunion or malunion of fractures of the lateral condyle of the distal humerus in childhood [5, 12, 18]. Although various surgical techniques have been proposed to manage ulnar nerve symptoms associated with posttraumatic cubitus valgus, anterior transposition of the ulnar nerve remains the most common [7, 13]. The success of ulnar nerve recovery after transposition likely depends not only on the severity of the preoperative ulnar nerve involvement but also on whether the cubitus valgus deformity is corrected [1, 3, 14]. There is general support for addressing isolated (those without associated ulnar nerve symptoms) severe cubitus valgus deformities with a carrying angle greater than 20° [11, 17] with a supracondylar correctional osteotomy of the distal humerus. Not correcting the angular deformity at the elbow may lead to pain and apprehension (fear of instability) when using the elbow as a result of lateral instability and limited ROM [11, 17, 18]. However, there is little information regarding the use of a combined approach of a correctional supracondylar osteotomy with an anterior transposition of the ulnar nerve in patients with severe cubitus valgus and ulnar nerve palsy.
We therefore reviewed a patient cohort having this combined surgery to determine the change in their status at a minimum of 24 months after the procedure with respect to (1) active elbow ROM; (2) radiographic correction of the cubitus valgus deformity by comparing preoperative and postoperative humerus-elbow-wrist (HEW) angles and the medial prominence index; (3) ulnar nerve function through grip strength and static two-point discrimination; and (4) overall upper limb disability by the DASH.
Patients and Methods
After institutional review board approval, we retrospectively reviewed the medical records of 32 patients (32 elbows) who underwent anterior transposition of the ulnar nerve between 2004 and 2009 for tardy ulnar nerve palsy secondary to traumatic cubitus valgus deformity. Inclusion criteria included simultaneous anterior transposition of the ulnar nerve and supracondylar corrective osteotomy of the distal humerus to correct a cubitus valgus deformity at the elbow greater than 20°, and postoperative followup greater than 24 months. The combined procedures were conducted only for patients who wanted to correct their deformities while undergoing anterior transposition of the ulnar nerve. Nineteen of the 32 patients were excluded from the study (no osteotomy [n = 18] and followup less than 24 months [n = 1]). Indications for supracondylar corrective osteotomy in patients with traumatic cubitus valgus deformity were (1) cubitus valgus deformity at the elbow greater than 20°, and (2) pain and apprehension (fear of instability) when using the elbow as a result of lateral instability. We presented treatment options, anterior transposition alone or the combination of corrective osteotomy and anterior transposition to all patients with tardy ulnar nerve palsy with severe cubitus valgus deformity. The combined procedures were done only for patients who wanted to correct their deformities while undergoing anterior transposition of the ulnar nerve. One patient was excluded from the study because of inadequate followup (< 24 months).
The remaining 13 patients with a mean age at the time of surgery of 41 ±11 years (range, 22–56 years) were included in the study (Table 1). There were 11 male and two female patients. Cubitus valgus deformity was secondary to lateral condylar nonunion in nine patients and lateral condyle malunion in four patients.
Table 1.
Patient details and clinical data
| Patient number | Age (years) | Sex | Followup (months) | HEW angle (°) | ROM (°) | |||
|---|---|---|---|---|---|---|---|---|
| Normal | Preoperative | Postoperative | Preoperative | Postoperative | ||||
| 1 | 40 | M | 52 | 8 | 47 | 10 | 70 | 90 |
| 2 | 55 | M | 41 | 13 | 20 | 10 | 100 | 110 |
| 3 | 34 | F | 41 | 11 | 29 | 9 | 127 | 120 |
| 4 | 40 | M | 31 | 16 | 38 | 14 | 120 | 120 |
| 5 | 45 | M | 26 | 15 | 34 | 15 | 90 | 97 |
| 6 | 23 | M | 36 | 10 | 37 | 12 | 125 | 130 |
| 7 | 22 | M | 26 | 11 | 46 | 16 | 100 | 115 |
| 8 | 43 | M | 38 | 13 | 43 | 10 | 90 | 108 |
| 9 | 51 | M | 36 | 8 | 24 | 9 | 110 | 107 |
| 10 | 37 | F | 34 | 11 | 35 | 9 | 130 | 130 |
| 11 | 41 | M | 28 | 16 | 38 | 13 | 115 | 125 |
| 12 | 39 | M | 24 | 15 | 34 | 14 | 115 | 120 |
| 13 | 56 | F | 24 | 10 | 37 | 13 | 115 | 125 |
| Patient number | Grip strength (kg force) | 2-PD | DASH | Result for deformity correction | |||
|---|---|---|---|---|---|---|---|
| Preoperative | Postoperative | Preoperative | Postoperative | Preoperative | Postoperative | ||
| 1 | 19 | 20 | 5 | 3 | 22 | 18 | Excellent |
| 2 | 16 | 23 | 14 | 6 | 32 | 19 | Excellent |
| 3 | 20 | 30 | 6 | 5 | 20 | 13 | Excellent |
| 4 | 20 | 25 | 8 | 3 | 18 | 17 | Excellent |
| 5 | 11 | 16 | 6 | 3 | 43 | 18 | Excellent |
| 6 | 14 | 14 | 10 | 4 | 43 | 16 | Excellent |
| 7 | 18 | 24 | 6 | 7 | 18 | 11 | Good |
| 8 | 19 | 20 | 5 | 3 | 23 | 18 | Excellent |
| 9 | 9 | 16 | 9 | 4 | 33 | 21 | Excellent |
| 10 | 24 | 41 | 8 | 5 | 20 | 13 | Excellent |
| 11 | 36 | 44 | 3 | 3 | 18 | 17 | Excellent |
| 12 | 19 | 27 | 7 | 4 | 44 | 18 | Excellent |
| 13 | 36 | 48 | 3 | 2 | 43 | 10 | Excellent |
HEW = humerus-elbow-wrist; 2-PD = two-point discrimination; M = male; F = female.
Among the nine patients with nonunion, five were classified according to the system of Toh et al. [18] as having a Group I nonunion resulting from a Milch Type I injury, and four were classified as having a Group II nonunion resulting from a Milch Type II injury [18]. All patients had ulnar nerve innervating intrinsic muscle wasting at the time of initial presentation that was classified as Dellon Grade III [4]. Patients with intermittent paresthesia and subjective weakness were classified as having Grade I criteria, patients with intermittent paresthesia and measurable weakness in pinch and grip strength were classified as having Grade II criteria, and patients with persistent paresthesia, abnormal two-point discrimination, and measurable weakness in pinch and grip strength with intrinsic atrophy were classified as having Grade III criteria. Electrodiagnostic tests were performed in all of our patients to confirm the diagnosis of ulnar neuropathy around the elbow. The minimum followup after surgery was 24 months (mean, 34 months; range, 24–52 months). The dominant elbow was involved in six of the 13 patients.
Clinical and radiographic assessments of the upper extremities were performed before surgery. AP radiographs of both extremities were obtained with the elbow extended and the forearm supinated. The radiographic carrying angle was measured using the HEW angle on the AP radiographs [16]. Patients with a flexion contracture of the affected elbow were instructed how to maintain their medial and lateral condyles in the same horizontal plane while AP radiographs were taken to prevent overestimating the HEW angles. To measure the HEW angle, two transverse lines (one proximal and one distal) across the humerus that connected the medial and lateral cortices and two lines (one proximal and one distal) across the forearm that connected the medial cortex of the ulna and the lateral cortex of the radius were drawn. Then, a line connecting the midpoints of the two cross-humeral lines and another connecting the midpoints of the two lines across the forearm were drawn. The angle of intersection by these two lines was measured as the HEW angle (Fig. 1). To enhance the reliability of radiographic measurements, intraobserver or interobserver variability was adjusted for the mean of two values assessed by different observers (YRC, YCJ). The active ROM of the affected elbow was assessed and compared with that of the normal side. A flexion contracture of the elbow was measured with the medial and lateral condyles held in the same horizontal plane with two fingers because, in patients with cubitus valgus, as the elbow is extended the shoulder tends to rotate externally and mask the true flexion contracture of the elbow. The medial prominence index was measured on the preoperative and postoperative radiographs. The index represents the difference between the medial and lateral widths of the distal part of the humerus, as measured from the longitudinal midhumeral axis, and is expressed as a percentage of the total width of the distal part of the humerus (Fig. 2). The necessary corrective angle was estimated between the HEW angles of the normal and deformed elbows.
Fig. 1.

The humerus-elbow-wrist (HEW) angle is measured by connecting the midpoints of the two cross-humeral lines and another connecting the midpoints of the two lines across the forearm. The angle of intersection by these two lines is the HEW angle.
Fig. 2.
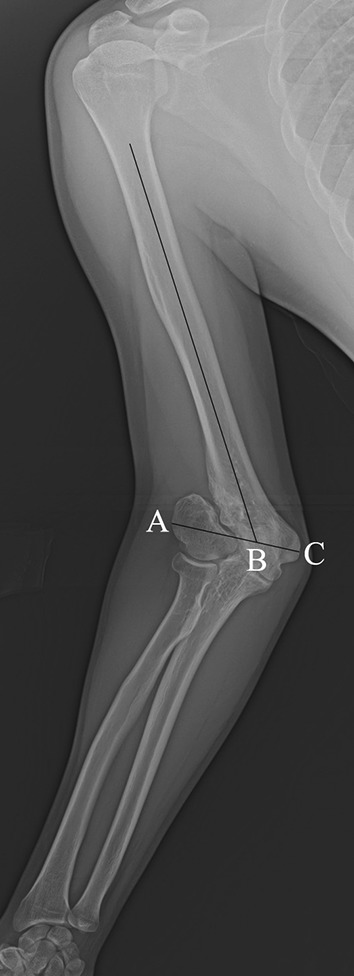
The medial prominence index (%) was calculated by (BC-AB)/AC × 100. Point B refers to a crosslink between the line connecting the medial epicondyle (C) and the lateral epicondyle (A) and the longitudinal midhumeral axis.
Under general anesthesia, the patient was placed in a lateral decubitus position with the affected arm supported by an armrest. After applying a sterile tourniquet, a posterior longitudinal skin incision was made from the distal upper arm to the olecranon. The ulnar nerve was exposed and protected with a Penrose drain throughout the operation. The triceps muscle was split along the midline to expose the distal humerus and olecranon. The periosteum was incised longitudinally in the midline, and subperiosteal dissection was performed to expose the metaphysis and diaphysis of the distal humerus. Osteophytes located at the tip of the olecranon were excised to improve elbow extension. A semicircle with a radius of approximately 3-cm from the intersection point of the midline axis of the humerus and the upper margin of the olecranon fossa was drawn on the surface of the distal humeral metaphysis (Fig. 3) [17]. The apex of the semicircle was proximal for engagement of the medial condyle after osteotomy. A line then was drawn from the center of the semicircle along the surface of the humerus to the end point of the semicircle for a guide to estimate the angle of correction. Multiple interrupted drill holes were made along the circle using a 1.8-mm K-wire. The dome-shaped osteotomy was completed with a 0.25-inch osteotome, and the distal fragment was rotated coronally to correct the cubitus valgus deformity (Fig. 3). The osteotomy was temporarily fixed with one K-wire or a Locking Compression Plate (LCP) 2.0 (Synthes®, Oberdorf, Switzerland). The osteotomy site was secured with two conventional or LCP reconstruction plates (Synthes®) in all cases. None of our nine patients with established lateral condylar nonunion of the humerus underwent osteosynthesis at surgery.
Fig. 3A–C.
(A) A semicircle from the intersection point of the midline axis of the humerus and the upper margin of the olecranon fossa was drawn and the necessary correction angle (*) was marked. (B) The dome-shaped osteotomy was completed and the distal fragment was rotated coronally to correct the cubitus valgus deformity. (C) A photograph shows the dome-shaped osteotomy of the distal humerus after completion of the osteotomy.
Anterior transposition of the ulnar nerve was performed after correction of the angular deformity in the elbow. The shoulder was internally rotated with the elbow in 90° flexion. A medial skin flap was retracted to thoroughly expose the ulnar nerve. All nerve-compressing structures (ie, arcade of Struthers, brachial fascia, Osborne’s ligament, Osborne’s fascia, and the flexor-pronator aponeurosis) were released. The medial intermuscular septum was excised as part of the procedure. The ulnar nerve then was carefully lifted from its bed with its accompanying longitudinal vascular supply intact by using a small Penrose drain. Neurolysis was performed if necessary to separate the posterior motor branches from the main ulnar nerve for transposition of the nerve without tension. The ulnar nerve then was moved anteriorly to a subcutaneous position and a fascial sling raised from the underlying muscle fascia was created to prevent slippage of the nerve after transposition [2]. After skin closure, a long arm splint was applied with 90° elbow flexion for 2 weeks followed by gentle passive and active ROM exercises.
Postoperatively, patients underwent regular followups at an outpatient clinic at 2 weeks, 6 weeks, 3 months, 6 months, 1 year, and annually thereafter; standard AP and lateral radiographs were obtained at each visit. Each patient was assessed for HEW angle, elbow ROM, medial prominence, grip strength, and static 2-point discrimination at 3 months, 6 months, 1 year, and annually thereafter, postoperatively. The DASH survey also was completed by each patient at each followup after 3 months postoperatively [8]. Grip strength was measured using a Baseline Hydraulic Hand Dynamometer (Fabrication Enterprises Inc, Irvington, NY, USA). We checked longitudinal static 2-point discrimination in the little finger using a Baseline Two Point Discriminator (Fabrication Enterprises Inc). The DASH questionnaire, a self-report questionnaire introduced by Hudak et al. [8], was given to each patient preoperatively and at each followup. The questionnaire contains 30 items: 21 questions that assess difficulties with specific tasks, five that evaluate symptoms, and four more questions that evaluate social function, work function, sleep, and confidence (one for each). The DASH scores are scaled between 0 and 100 with higher scores representing greater upper extremity disability. The clinical outcome after correction of the cubitus valgus deformity was evaluated using the modified criteria of Oppenheim et al., based on measurement of the correction of the HEW angle, active elbow ROM, and the presence of complications [10, 16]. An excellent result indicated correction of the HEW angle to within 5° of the contralateral elbow, loss of less than 5° ROM, and no complications. A good result indicated correction of the HEW angle to within 6° to 10° of the contralateral elbow, loss of 6° to 10° ROM, and/or a lazy-s deformity. A poor result was assigned whenever there was residual (uncorrected) valgus differing greater than 10° from the contralateral side or loss greater than 10° in any plane of motion compared with the preoperative examination.
SPSS Version 18.0 (SPSS, Inc, Chicago, IL, USA) was used for statistical analyses. HEW angles, elbow ROM, medial prominence index, grip strength, 2-point discrimination, and DASH score before surgery were compared with the corresponding values at the last followup using the Wilcoxon signed-rank test. A p value less than 0.05 was considered significant.
Results
Before surgery, the mean active extension in these patients was −16° (95% CI, −11° to −21°); after surgery, the mean active extension was −10° (95% CI, −7° to −14°) (p = 0.007). Before surgery, the mean active flexion in these patients was 124° (95% CI, 117°–131°); after surgery, the mean active flexion was 126° (95% CI, 120°–131°) (p = 0.506). However, one patient lost 7° ROM. Deformity correction was rated as excellent for 12 patients and good for one patient based on the modified criteria of Oppenheim et al. (Table 1).
All osteotomies of the distal humerus showed union on radiographs taken 3 months after surgery. The mean HEW angle was corrected from 36° (95% CI, 31°–40°) to 12° (95% CI, 10°–14°) (p = 0.001) (Fig. 4). The average improvement in the medial prominence index was 17%, from a mean of −8% (95% CI, −14% to −2%) to 9% (95% CI, 0%–18%) (p = 0.007).
Fig. 4A–C.
(A) A 22-year-old male patient (Patient 6) presented with severe tardy ulnar nerve palsy resulting from a traumatic cubitus valgus deformity from malunion of the right distal humerus (HEW angle, 37° valgus). (B) A supracondylar dome-shaped osteotomy in combination with anterior transposition of the ulnar nerve was performed. (C) Three years postoperatively the HEW angle was corrected to 12° valgus. Excellent results were obtained for deformity correction and improvement in the ulnar nerve palsy.
At last followup, the grip strength increased from a mean of 20 kg of force (95% CI, 15–25 kg of force) to 27 kg of force (95% CI, 20–33 kg of force) (p = 0.002). The mean 2-point discrimination improved from 7 mm (95% CI, 5–9 mm) to 4 mm (95% CI, 3–4 mm) (p = 0.004).
The mean DASH score improved from 29 points (95% CI, 22–36 points) to 16 points (95% CI, 14–18 points) (p = 0.001). All but one patient reported subjective improvement in their symptoms.
Discussion
It remains controversial whether supracondylar humeral osteotomy should be done at the same time as anterior transposition of the ulnar nerve for patients presenting with tardy ulnar nerve palsy from cubitus valgus. We evaluated a group of patients in whom the procedures were done concurrently, rather than in a staged fashion, and assessed radiographic and clinical results at a minimum of 2 years. We found that the deformity was well corrected with a supracondylar dome osteotomy and ulnar nerve symptoms and signs improved without decreased elbow ROM.
This study has several limitations. Information was collected retrospectively and included only a small number of patients. Additionally, there was no control group of patients treated with anterior transposition of the ulnar nerve alone. All of our patients had a cubitus valgus deformity greater than 20° and underwent correction of the deformity concurrent with nerve transposition if they wanted. However, there are few cases for which corrective osteotomy and nerve transposition would be indicated. Patients with flexion contracture of the elbow tend to rotate their shoulder externally to mask their flexion contracture while radiographs are being taken. The HEW angle can be overestimated with this compensatory movement of the shoulder. We instructed our patients how to maintain their medial and lateral condyles in the same horizontal plane while radiographs were being taken to get proper projection of their elbows.
Furthermore, there is no reliable, reproducible, and valid outcome measure for patients who underwent supracondylar correctional osteotomy and anterior transposition of the ulnar nerve simultaneously for ulnar nerve palsy from a traumatic cubitus valgus deformity. The DASH score, which is more of a general upper-extremity instrument, was used in our study to evaluate the disabilities from ulnar nerve palsy from traumatic cubitus valgus deformity. Although retrospective studies generally involve selection bias, our study did not have this issue because we performed correction of the deformity concurrent with nerve transposition in all patients, if they intended to correct their deformity at the same time. One of our patients was excluded from this study owing to inadequate followup (less than 2 years). This patient’s last visit was at 6 months postoperative. At that time, the osteotomy site had healed completely; however, the assessment at that time seemed to be inadequate to judge the end results from the surgery. Therefore, we analyzed data from the last 13 patients who had more than 2 years of followup.
In our study, the dome-shaped osteotomy was performed to correct a traumatic cubitus valgus deformity. No patients experienced significant loss of elbow ROM at 2 or more years of followup. Fixation with two conventional reconstruction or LCP reconstruction plates (Synthes®) achieved stable fixation, which permitted early ROM exercises for the elbow and maintained elbow ROM. We believe that excision of any osteophytes at the tip of the olecranon through a posterior capsulotomy was another reason why our patients showed little improvement of active elbow extension. None of our nine patients with established lateral condylar nonunion of the humerus underwent osteosynthesis at surgery. This seems to be another reason why our patients with lateral condylar nonunion maintained their elbow ROM postoperatively. Treatment of old, established nonunions of the lateral condyle of the humerus remains controversial. However, osteosynthesis of the lateral condyle has been associated with complications, including loss of elbow ROM [9–11, 18], necrosis of the lateral condylar fragment [9], and persistent nonunion [10, 11, 18]. Therefore, osteosynthesis of the lateral condyle should be considered only in patients with severe elbow pain and apprehension with use secondary to lateral instability [11]. None of our patients with lateral condylar nonunion experienced those symptoms preoperatively.
All patients achieved nearly normal HEW angles without recurrence of deformity or a residual prominence of the medial condyle. Although there is no consensus, a supracondylar osteotomy of the distal humerus generally is indicated if the carrying angle exceeds 20° [11, 17]. A medial closing-wedge osteotomy traditionally has been used to correct the cubitus valgus deformity resulting from its simplicity and ease; however, loss of the deformity correction and decreased elbow ROM from a large valgus moment after correction have been reported [9, 11]. Prominence of the medial condyle of the distal humerus also can occur as a result of a medial shift in the humerus-ulna axis. Because the center of rotation of the distal humeral fragment is located at the lateral end of the osteotomy plane [10], the valgus moment is much larger after the medial closing-wedge osteotomy. This valgus moment can hinder the fixation necessary to maintain the achieved correction [17]. A simple step-cut translation osteotomy was described with excellent clinical results [10]. This technique modified the simple step-cut osteotomy by resecting a triangular wedge-shaped fragment from the proximal fragment and translating the distal fragment to prevent condylar prominence after correction. The three cuts required at the distal humerus in this procedure make it difficult to control the angle of correction once the osteotomy is complete [6]. In contrast, a dome-shaped osteotomy maintains the center of rotation of the distal humeral fragment in the midline of the humerus such that a much smaller valgus moment is needed to correct the valgus deformity [17]. Therefore, with the dome-shaped osteotomy, loss of correction or the presence of a medial prominence after correction of the deformity is unlikely to occur [6, 17].
Traumatic cubitus valgus deformity can result in tardy ulnar nerve palsy [5, 12, 18]. Although decompression and anterior transposition of the ulnar nerve is a common procedure for ulnar nerve symptoms [7, 13], there is little information regarding the use of a combined approach of deformity correction with an anterior transposition of the ulnar nerve in patients with severe cubitus valgus and ulnar nerve palsy. Some authors reported that angular deformity at the elbow correlates with poor prognosis and recurrence of ulnar nerve symptoms after operative treatment for cubital tunnel syndrome [1, 3]. In a prospective cohort study of anterior transposition of the ulnar nerve in 10 patients with severe ulnar nerve palsy caused by traumatic cubitus valgus deformity, all 10 patients reported subjective improvement [13]. Among them, however, only four patients had greater than 20° cubitus valgus deformity. Furthermore, one of them had a fair result according to the modified Bishop scoring system. In 2005, Kim et al. reported on 13 patients with cubitus valgus who underwent a step-cut translation osteotomy [10]. Among them, five patients had tardy ulnar nerve palsy preoperatively and underwent subcutaneous anterior transposition of the ulnar nerve combined with the corrective osteotomy. They reported complete relief of nerve symptoms after surgery. In the current study, the DASH score significantly improved (p = 0.001) from a mean of 29 points to 16 points 2 years after surgery. All but one patient showed symptomatic improvement. Relieving the pathologic traction on the ulnar nerve at the elbow by performing deformity correction, having the rotation center of the distal humeral fragment at the midline of the humerus, in combination with anterior transposition of the ulnar nerve seems to offer a promising clinical outcome.
Based on the results of this small, retrospective study, we are cautiously optimistic about the supracondylar dome-shaped osteotomy in combination with anterior transposition of the ulnar nerve for patients with severe traumatic cubitus valgus deformity and tardy ulnar nerve palsy. A comparative study of anterior transposition of the ulnar nerve alone and the concomitant corrective osteotomy is warranted to prove the advantages of combined osteotomy over ulnar nerve transposition alone in patients with severe traumatic cubitus valgus deformity and tardy ulnar nerve palsy.
Acknowledgments
We thank Bo Ram Kim RN (specializing in orthopaedics), for assessing clinical outcomes and collecting data and Dong Soo Jang (medical illustrator), for the schematic drawings of operative procedure.
Footnotes
Each author certifies that he or she, or a member of their immediate family, has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Barrios C, Ganoza C, de Pablos J, Canadell J. Posttraumatic ulnar neuropathy versus non-traumatic cubital tunnel syndrome: clinical features and response to surgery. Acta Neurochir (Wien). 1991;110:44–48. doi: 10.1007/BF01402047. [DOI] [PubMed] [Google Scholar]
- 2.Caputo AE, Watson HK. Subcutaneous anterior transposition of the ulnar nerve for failed decompression of cubital tunnel syndrome. J Hand Surg Am. 2000;25:544–551. doi: 10.1053/jhsu.2000.6005. [DOI] [PubMed] [Google Scholar]
- 3.Dellon AL. Review of treatment results for ulnar nerve entrapment at the elbow. J Hand Surg Am. 1989;14:688–700. doi: 10.1016/0363-5023(89)90192-5. [DOI] [PubMed] [Google Scholar]
- 4.Dellon AL. Techniques for successful management of ulnar nerve entrapment at the elbow. Neurosurg Clin N Am. 1991;2:57–73. [PubMed] [Google Scholar]
- 5.Gay JR, Love JG. Diagnosis and treatment of tardy paralysis of the ulnar nerve; based on a study of 100 cases. J Bone Joint Surg Am. 1947;29:1087–1097. [PubMed] [Google Scholar]
- 6.Hahn SB, Choi YR, Kang HJ. Corrective dome osteotomy for cubitus varus and valgus in adults. J Shoulder Elbow Surg. 2009;18:38–43. doi: 10.1016/j.jse.2008.07.013. [DOI] [PubMed] [Google Scholar]
- 7.Helfet DL, Kloen P, Anand N, Rosen HS. Open reduction and internal fixation of delayed unions and nonunions of fractures of the distal part of the humerus. J Bone Joint Surg Am. 2003;85:33–40. doi: 10.2106/00004623-200301000-00006. [DOI] [PubMed] [Google Scholar]
- 8.Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: the DASH (Disabilities of the Arm, Shoulder and Hand) [corrected]. The Upper Extremity Collaborative Group (UECG) Am J Ind Med. 1996;29:602–608. doi: 10.1002/(SICI)1097-0274(199606)29:6<602::AID-AJIM4>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 9.Jakob R, Fowles JV, Rang M, Kassab MT. Observations concerning fractures of the lateral humeral condyle in children. J Bone Joint Surg Br. 1975;57:430–436. [PubMed] [Google Scholar]
- 10.Kim HT, Lee JS, Yoo CI. Management of cubitus varus and valgus. J Bone Joint Surg Am. 2005;87:771–780. doi: 10.2106/JBJS.D.01870. [DOI] [PubMed] [Google Scholar]
- 11.Masada K, Kawai H, Kawabata H, Masatomi T, Tsuyuguchi Y, Yamamoto K. Osteosynthesis for old, established non-union of the lateral condyle of the humerus. J Bone Joint Surg Am. 1990;72:32–40. [PubMed] [Google Scholar]
- 12.Mc Gowan AJ. The results of transposition of the ulnar nerve for traumatic ulnar neuritis. J Bone Joint Surg Br. 1950;32:293–301. [DOI] [PubMed]
- 13.Mortazavi SM, Heidari P, Asadollahi S, Farzan M. Severe tardy ulnar nerve palsy caused by traumatic cubitus valgus deformity: functional outcome of subcutaneous anterior transposition. J Hand Surg Eur Vol. 2008;33:575–580. doi: 10.1177/1753193408092252. [DOI] [PubMed] [Google Scholar]
- 14.Mowlavi A, Andrews K, Lille S, Verhulst S, Zook EG, Milner S. The management of cubital tunnel syndrome: a meta-analysis of clinical studies. Plast Reconstr Surg. 2000;106:327–334. doi: 10.1097/00006534-200008000-00014. [DOI] [PubMed] [Google Scholar]
- 15.Nouhan R, Kleinert JM. Ulnar nerve decompression by transposing the nerve and Z-lengthening the flexor-pronator mass: clinical outcome. J Hand Surg Am. 1997;22:127–131. doi: 10.1016/S0363-5023(05)80192-3. [DOI] [PubMed] [Google Scholar]
- 16.Oppenheim WL, Clader TJ, Smith C, Bayer M. Supracondylar humeral osteotomy for traumatic childhood cubitus varus deformity. Clin Orthop Relat Res. 1984;188:34–39. [PubMed] [Google Scholar]
- 17.Tien YC, Chen JC, Fu YC, Chih TT, Hunag PJ, Wang GJ. Supracondylar dome osteotomy for cubitus valgus deformity associated with a lateral condylar nonunion in children. J Bone Joint Surg Am. 2005;87:1456–1463. doi: 10.2106/JBJS.C.01545. [DOI] [PubMed] [Google Scholar]
- 18.Toh S, Tsubo K, Nishikawa S, Inoue S, Nakamura R, Harata S. Long-standing nonunion of fractures of the lateral humeral condyle. J Bone Joint Surg Am. 2002;84:593–598. doi: 10.1302/0301-620X.84B2.12131. [DOI] [PubMed] [Google Scholar]




