Abstract
Background
Selective bundle anterior cruciate ligament (ACL) reconstruction and/or remnant ACL preservation may be reasonable options for some patients. However, the frequency of isolated anteromedial (AM) or posterolateral (PL) bundle injuries in patients undergoing ACL reconstruction is unknown, and the value of MRI for prediction of this injury pattern is likewise unknown.
Questions/purposes
We sought to determine (1) the proportion of knees with an intact AM or PL bundle in patients undergoing ACL reconstruction; (2) whether MRI predicted the bundle conditions seen at the time of surgery; and (3) whether the accuracy of the MRI prediction was affected by the timing of MRI after injury.
Methods
During primary ACL reconstructions of 156 knees, conditions of AM and PL bundles were separately examined and classified into three categories: (1) completely torn; (2) attenuated; and (3) intact. Then, the bundles were assessed by blinded observers on MRI and classified into the corresponding three categories for 77 patients who had an MRI at our institution using a standard protocol. Diagnostic accuracy of MRI was computed, and the early MRI group (≤ 6 weeks from injury to MRI acquisition) was compared with the late MRI group (> 6 weeks).
Results
Only 11 (7%) of the 156 knees we treated had an intact AM (one knee) or PL bundle (10 knees). Another 55 knees (35%) had a structurally continuous but attenuated AM or PL bundle. The overall diagnostic accuracy of MRI was 83%; accuracy was better for the AM bundle than the PL bundle (91% versus 78%; p = 0.026). MR prediction was less accurate in the early MRI group, particularly for PL bundle injury.
Conclusions
An isolated bundle tear is uncommon in patients with ACL tears undergoing reconstruction. MRI can help surgeons predict bundle injury pattern with satisfactory precision, but caution should be used in predicting PL bundle injury using MRI with early acquisition time from injury.
Level of Evidence
Level III, diagnostic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Attributable in part to an improved understanding of the anatomy of anterior cruciate ligament (ACL) and theoretical benefit of preserving remnant tissue of ACL, the remnant preservation technique and/or selective bundle reconstruction have received increased attention [3, 12, 14, 15, 24]. Because the two functional ACL bundles, the anteromedial (AM) and the posterolateral (PL) bundles [6, 22, 31], have different tension patterns according to the flexion angle of the knee [19, 30], each bundle of the ACL may show a different rupture pattern according to the injury mechanism [34]. Accordingly, there may be isolated ACL bundle injuries that can be candidates for selective bundle reconstruction [1, 22] while preserving the uninjured bundle [3, 9, 15, 32].
Theoretically, selective bundle and/or remnant-preserving ACL reconstruction may have advantages such as preservation of mechanoreceptor and vascularity and increased stability by sparing intact bundle. To date, a few studies partly supported these advantages in terms of stability and joint position sense [1, 3, 33]. Nevertheless, these techniques may be technically demanding and limit graft selection and fixation method. Moreover, preservation of useless remnants may adversely affect outcomes and result in impingement or a Cyclops lesion [16]. Given the potential advantages and disadvantages of the technique, precise preoperative prediction of each ACL bundle condition would help surgeons establish proper surgical plans when considering selective bundle reconstruction. In this respect, although patients’ subjective instability and physical findings are the most important for decision of ACL reconstruction, MRI may have a valuable role because it is the best noninvasive modality to assess ACL structural integrity [28]. Nevertheless, information on the diagnostic accuracy of MRI to detect individual bundle injuries is lacking. One potential difficulty is assessing PL bundle injury on MRI resulting from the fact that the PL bundle is shorter than the AM bundle making it potentially harder to evaluate [17, 22]. Another potential problem with the diagnostic accuracy of MRI is related to the time elapsed from injury to acquisition of MRI. An acute ACL tear may be accompanied by edema of surrounding tissues, which can obscure the discrimination of individual bundles. Furthermore, a torn ACL can heal, especially if it is partially torn [2]. Therefore, the time interval between injury and acquisition of MRI may be important when assessing the diagnostic accuracy of MRI to detect individual bundle injuries.
The purposes of our study were to determine (1) the proportion of knees with an intact AM or PL bundle in patients undergoing ACL reconstruction; (2) whether MRI predicted the bundle conditions seen at the time of surgery; and (3) whether the accuracy of the MRI prediction was affected by the timing of MRI after injury.
Patients and Methods
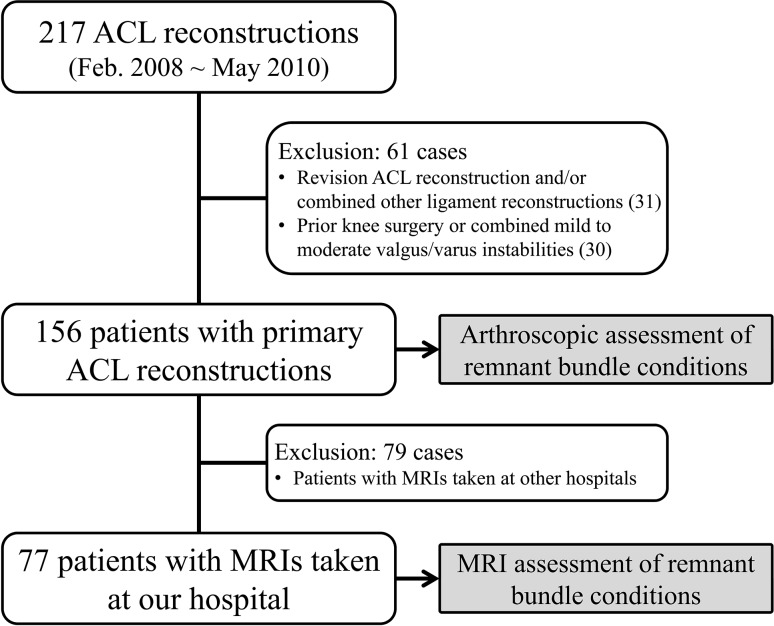
This retrospective study was conducted using a prospectively collected database of 156 primary ACL reconstructions of 156 patients (Fig. 1). For this study, we reviewed a total of 217 cases of ACL reconstructions by a single surgeon (CBC) between February 2008 and May 2010. Our general indication for ACL reconstruction involved subjective instability symptoms with high grade instability on physical examinations (≥ grade 2 in pivot shift test and/or ≥ grade 2 in Lachman test). In addition, if a patient showed pivot shift grade 1 and ≥ grade 1 in Lachman test but had persistent subjective instability recalcitrant to conservative measures, we performed ACL reconstruction when the patient had a near-complete/complete tear of ACL on MRI. Among 217 cases, 31 cases were initially excluded for having revision ACL reconstruction and/or other combined ligament reconstructions. We excluded a further 30 patients who were inappropriate for this study such as a patient with a prior knee surgery or combined mild to moderate valgus/varus instabilities for which combined reconstruction was not needed but may have affected the assessment of the ACL remnant condition. Finally, 156 knees (156 patients) were included in this study for evaluations of arthroscopic findings. There were 127 (81%) males and 29 (19%) females with a mean age of 30 ± 10.4 years (range, 14–64 years). The preoperative physical findings of the 156 patients were grade I in four (3%), grade II in 108 (69%), grade III in 44 (28%) in terms of the Lachman test, and grade I in 16 (10%), grade II in 132 (85%), and grade III in eight (5%) in terms of the pivot shift test.
Fig. 1.
Patient enrollment flowchart is shown.
For purposes of the MRI analysis, we included only those patients whose MRI was performed at our hospital; there were 77 knees meeting this criterion, which was chosen to avoid potential errors resulting from heterogeneity of the MRI protocol. The outside MRIs of the 79 knees were excluded from the imaging analyses in this study. There was no difference in the sex proportion, age, body mass index, and the timing of MRI from injury between the 77 patients with MRIs at our institution and the other 79 patients (p = 0.076–0.402, chi-square test for sex proportion and Student’s t-tests for the other variables). All the study protocols were approved by the institutional review board of the authors’ hospital.
Arthroscopic Evaluation (156 Knees)
All arthroscopic examinations were performed by one experienced orthopaedic knee surgeon (CBC), who had more than 10 years’ experience as a knee specialist. During arthroscopy, the condition of each bundle was assessed by observation through AM and anterolateral portals. When a continuous bundle was found, particular attention was given to the tension of the bundle at various flexion angles between 10° and 90° and during the internal and external rotation of the tibia. We believe that these procedures are particularly crucial in examining the PL bundle, which, even in the normal condition, can be lax in a flexed (> 60°) knee. Then, we classified the condition of the each bundle into three categories (Figs. 2–4): (1) completely torn (bundle was not continuous, not visible, or completely detached from its original attachments) (Fig. 2); (2) attenuated (bundle remained in continuity between femoral and tibial insertions on direct arthroscopic visualization but did not have proper resistance to deformation on probing during knee motions and tibial rotations and thus could not be preserved as a functional bundle) (Fig. 3); and (3) intact (bundle was continuous and had proper resistance during the functional range of knee motion and tibial rotation) (Fig. 4).
Fig. 2.
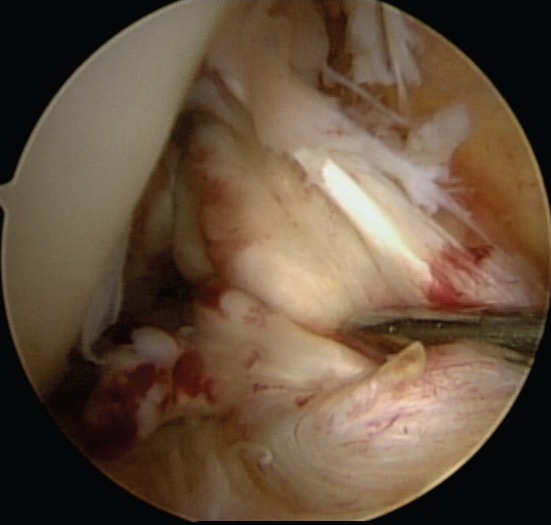
Arthroscopic photograph showing the completely torn AM and PL bundles.
Fig. 4A–B.
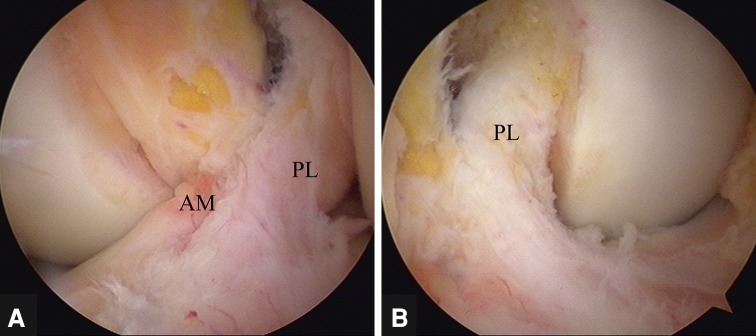
Arthroscopic photographs showing the completely torn AM bundle and the intact PL bundle. (A) The arthroscopic view through an anterolateral portal showing the normal-looking PL bundle and discontinuity of the AM bundle. (B) The arthroscopic view through an AM portal more clearly showed the intact PL bundle.
Fig. 3A–B.
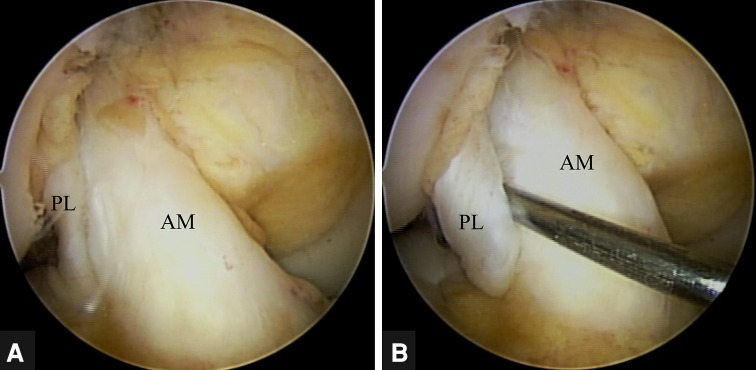
Arthroscopic photographs showing the intact AM bundle and the attenuated PL bundle. (A) The arthroscopic view through an anterolateral portal showing the normal-looking AM bundle and continuous but thin PL bundle. (B) Attenuation of the PL bundle was confirmed by probing.
MRI Protocol and Interpretation (77 Knees)
All the MRIs were taken using a 1.5-T scanner (Intera; Philips, Best, The Netherlands) and reviewed on a picture archiving and communication system (Infinite, Seoul, Korea). The used sequences for evaluation were as follows: sagittal fat-suppressed (FS) T2-weighted (TR/TE 2000–2500/50–65 ms), sagittal proton density (PD)-weighted (TR/TE 2200–3900/12–20 ms), coronal T2- and PD-weighted (TR/TE 3000–3500/120 and 13 ms), oblique coronal PD-weighted (TR/TE 3300–6000/12–30 ms), and axial FS PD-weighted (TR/TE 2300–5600/12–20 ms) images with a 16- to 20-cm field of view, 90° flip angle, a 2- to 4-mm thickness, and 512 × 512 matrix.
Image assessments were subsequently performed by one musculoskeletal radiologist (JYC) who was blinded to arthroscopic results. The conditions of the AM and PL bundles were separately assessed and classified into three categories: (1) completely torn; (2) attenuated; and (3) intact. These three categories were determined based on previously reported MRI criteria of ACL injury (Figs. 5–7) [18, 27–29]. Completely torn was defined as a failure to visualize the ACL. Obvious discontinuity was also considered a sign of a complete injury (Fig. 5) [28, 29]. Increased signal intensity within the ligament substance, distortion of fibers, and significant thinning of the bundles without obvious discontinuity were all defined as attenuated (Fig. 6) [17, 27–29]. In contrast, an ACL bundle that could be followed continuously with homogeneous low signal intensity from the tibial and to the femoral insertions was defined as intact (Fig. 7) [28, 29].
Fig. 5A–B.
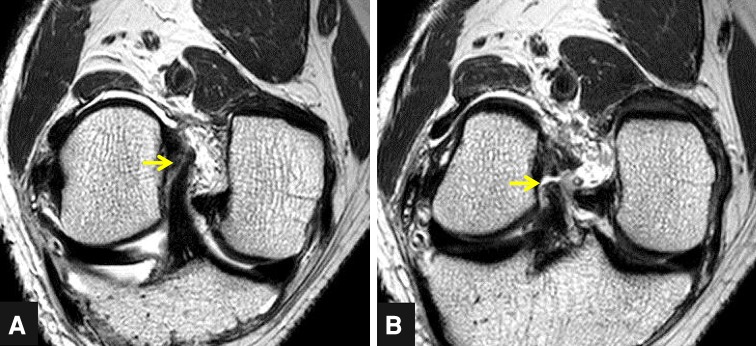
MR images showing the completely torn AM and PL bundles. (A) The oblique coronal MR image showed a complete tear of the AM bundle near the femoral attachment (arrow). (B) The oblique coronal MR image showed a complete tear of the PL bundle near the femoral attachment (arrow).
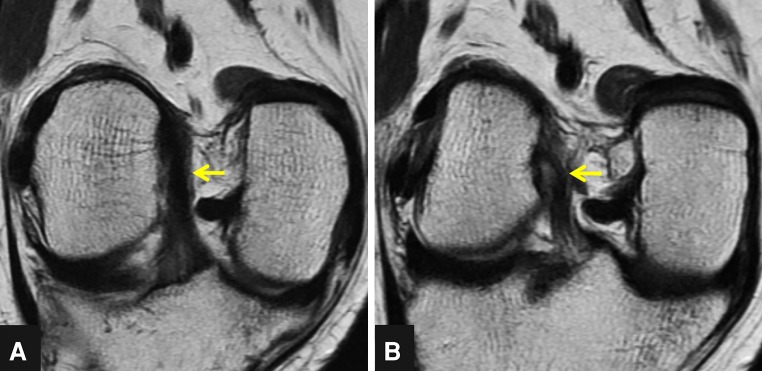
Fig. 7A–B.
MR images showing the attenuated AM and the intact PL bundle. (A) The oblique coronal MR image showed the thin AM bundle with a wavy course (arrow). (B) The oblique coronal MR image showed the intact PL bundle (arrow).
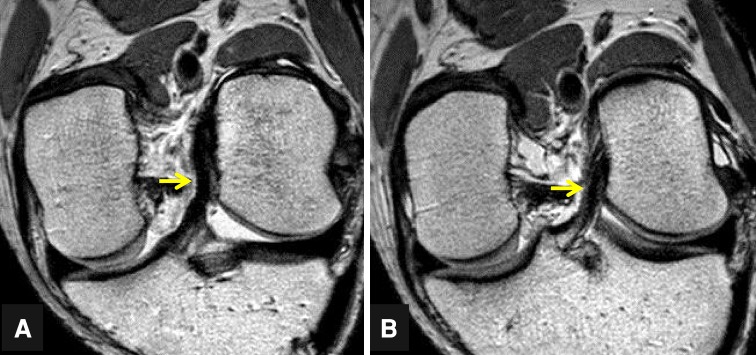
Fig. 6A–B.
MR images showing the intact AM and the attenuated PL bundle. (A) The oblique coronal MR image showed the continuous AM bundle with normal signal intensity (arrow). (B) The oblique coronal MR image showed the thin PL bundle with a wavy course (arrow).
To determine the intra- and interobserver reliabilities of measurements, 20 subjects were chosen and measured twice (3 weeks apart) by three observers (one radiologist and two orthopaedic surgeons; JYC, MJC, HHW). The reliabilities of measurements were confirmed using kappa coefficient. The kappa coefficients for the intraobserver reliability were from 0.643 to 1.000 and for the interobserver reliability were from 0.444 to 0.828. The kappa coefficients had wide ranges from moderate to excellent. However, in this study, the various and relatively low kappa coefficients were not caused by low agreements but rather by a high prevalence index (0.8 in kappa coefficient of 0.444), which can increase chance agreement and decrease kappa coefficient [23].
In addition, to determine whether the diagnostic accuracy of MRI can be influenced by the time elapsed from injury to acquisition of MRI, 77 knees were allocated into two groups: the early MRI group (≤ 6 weeks from injury to MRI acquisition) and the late MRI group (> 6 weeks from injury to MRI acquisition). There were 45 knees in the early MRI group and 32 knees in the late MRI group.
Statistical Analysis
Statistical analysis was conducted with the SPSS for Windows statistical package (Version 18.0; SPSS, Chicago, IL, USA). The proportion of isolated bundle tears and continuous remnant ACL bundles were calculated and documented. Accuracies and error patterns in MRI assessments of injury severities between AM and PL bundles were calculated and analyzed using a chi-square test or a Fisher’s exact test. In addition, accuracies and error patterns in MRI assessments of injury severities of the bundles were separately assessed between the early MRI group and the late MRI group and analyzed using a chi-square test or a Fisher’s exact test.
Results
Isolated bundle injury was infrequent in our patients requiring ACL reconstruction. In the arthroscopic assessments of 156 patients, only 11 patients (7%) had an intact AM or PL bundle. Among them, 10 (6.4%) had an intact PL bundle and only one (0.6%) had an intact AM bundle. In addition, there were 55 patients (35%; 58 bundles) who had structurally continuous but attenuated bundles, which would not be suitable for isolated bundle reconstruction (AM bundles: 18 and PL bundles: 40) (Table 1).
Table 1.
Conditions of anteromedial (AM) and posterolateral (PL) bundles that were assessed on the basis of arthroscopic findings in 156 patients undergoing anterior cruciate ligament reconstruction
| Bundle condition | AM bundle | PL bundle |
|---|---|---|
| Completely torn | 137 (87.8%) | 106 (68.0%) |
| Attenuated | 18 (11.6%) | 40 (25.6%) |
| Intact | 1 (0.6%) | 10 (6.4%) |
Data are presented as number of patients with proportions in parentheses.
The diagnostic accuracy of MRI was 83% in predicting bundle injury pattern and was better for the AM bundle than the PL bundle, particularly in the early MRI group. The accuracy of MRI prediction was 91% (70 of 77) for AM bundles and 78% (60 of 77) for PL bundles (p = 0.026; Table 2). Overall, injury severity of the AM bundle was more likely to be underrated on MRI, whereas that of the PL bundle was likely to be overrated on MRI (p = 0.001; Table 2).
Table 2.
Accuracies of MRI assessments on injury severities of anteromedial (AM) and posterolateral (PL) bundles in 77 patients undergoing anterior cruciate ligament reconstruction
| Assessment result | AM bundle (N = 77) | PL bundle (N = 77) | p value |
|---|---|---|---|
| Accurate | 70 (91%) | 60 (78%) | 0.026* |
| Inaccurate | 7 (9%) | 17 (22%) | |
| Overrated | 0 | 13 (17%) | 0.001† |
| Underrated | 7 (9%) | 4 (5%) |
Data are presented as number of patients with proportions in parentheses; * statistical analysis was performed using a chi-square test; †statistical analysis was performed using Fisher’s exact test.
In the comparison between the early MRI group and the late MRI group, injury severity of the PL bundle was overrated in the early MRI group, whereas injury severity of the PL bundle was not overrated in the late MRI group (10 of 11; p = 0.004 and three of six; p = 0.464, respectively; Table 3).
Table 3.
Comparative results of accuracies of MRI assessments on injury severity of anteromedial (AM) and posterolateral (PL) bundles between early and late MRI groups
| Assessment result | Early MRI group (N = 45) | p value | Late MRI group (N = 32) | p value | ||
|---|---|---|---|---|---|---|
| AM bundle | PL bundle | AM bundle | PL bundle | |||
| Accurate | 41 (91%) | 34 (76%) | 0.048* | 29 (91%) | 26 (82%) | 0.474† |
| Inaccurate | 4 (9%) | 11 (24%) | 3 (9%) | 6 (18%) | ||
| Overrated | 0 | 10 (22%) | 0.004† | 0 | 3 (9%) | 0.464† |
| Underrated | 4 (9%) | 1 (2%) | 3 (9%) | 3 (9%) | ||
Data are presented as number of patients with proportions in parentheses; * statistical analysis was performed using a chi-square test; †statistical analyses were performed using Fisher’s exact tests.
Discussion
Despite recent enthusiasm for selective bundle reconstruction and the remnant ACL preservation technique, there has been only limited information on the prevalence of isolated bundle tears and functional remnant bundles and diagnostic values of preoperative MRI for the condition of each bundle. In this study, we sought to determine the proportion of the examined knees with an intact AM or PL bundle in patients undergoing ACL reconstruction. We also wanted to determine how well MRI predicts the condition of individual bundles and whether the accuracy of MRI in predicting the bundle injury pattern is affected by the timing of MRI after injury.
The present study has several limitations that should be noted. First, only 77 (49%) of 156 knees were included in the analysis to determine the diagnostic accuracy of MRI; we included only patients who had MRIs at our institution, and we did this to keep the MRI protocol identical. Nevertheless, we noted no difference of characteristics between the patients who were included in the analysis and those who were not. We believe that the selection bias regarding the result of MRI assessment would be minimal. Second, we did not provide the result of relationship between physical findings and MRI or arthroscopic findings, which would be an important issue. However, we intended to study only the patients requiring ACL reconstruction mostly with high-grade instability on physical examinations. Consequently, patients who had partial ACL injury but did not undergo ACL reconstruction as a result of low-grade subjective/objective instability were not included in the study. Therefore, results of the physical examinations of our study cohort are skewed, and the cohort may not be suitable to generally represent the patients with isolated bundle injury. Regarding this issue, further study would be required to draw a conclusion. Third, as mentioned, we included the patient requiring ACL reconstruction in this study based on our surgical indication. Thus, the prevalence of an intact bundle can be changed when using other criteria for ACL reconstruction. Fourth, estimating the integrity of each bundle during arthroscopy can be limited, and intrasubstance injury may not be detected. However, we made every effort to perform accurate arthroscopic assessment; besides the precise observation of the insertion area of the remnant bundle, we believe that evaluation of the tension of the remnant bundle during various angles of knee flexion and rotation would be the best optimal method to assess the condition of the bundle. Finally, our MRI protocol may not be perfect, and other advanced MRI protocol may provide better accuracy for prediction of the bundle condition. However, our routine protocol includes an additional oblique coronal view, which is known to be useful to assess each bundle condition. Thus, we believe that our MRI protocol has satisfactory accuracy to assess each bundle in current practice.
The proportion of isolated bundle tears in the knees undergoing ACL reconstruction was only 7% in this study, and an isolated PL bundle tear was detected in only one (0.6 %) of 156 knees. Surgical reconstruction might be required in symptomatic patients with partial ACL tears [13, 21, 33], and some surgeons prefer an ACL augmentation technique when treating the patients with partial ACL tears [4, 5, 33]. However, our study found that most remnant bundles are often loose and nonfunctional, even if the ACL remnant bridges the femur and the tibia [3]. This finding suggests that candidates for selective bundle reconstruction are uncommon in patients with instability warranting ACL reconstruction, although an isolated bundle tear can occur as a result of different anatomy and tension patterns of each bundle. Thus, it is important to make a comprehensive decision as to whether the remnant bundle is preserved using clinical and arthroscopic assessments. As mentioned, there were few isolated PL bundle tears in this study. A previous study with a similar purpose found that AM bundles were graded as tears in all cases, although the PL was elongated or intact in 12% of patients [34]. Along with the previous study, the performing selective bundle reconstruction in either the AM or PL bundle according to MRI findings should be decided with caution based on the following results, especially for selective PL bundle reconstruction: (1) all but one with isolated bundle injuries had AM bundle injury in this study (that is, isolated PL bundle injury is very rare, and so we believe few surgeons will develop sufficient experience with this procedure to be able to recommend it); (2) diagnostic accuracy of MRI was lower for the PL bundle than the AM bundle; and (3) injury severity of the PL bundle tended to be overrated, especially in the early MRI group.
To some extent, our findings support the hypotheses that MRI can accurately predict conditions of ACL bundles, although accuracy of MRI appears to be influenced by which bundle is injured and when the MRI examination was performed. Although some studies have reported that MRI is sensitive and specific for diagnosing complete ACL rupture [7, 20, 26, 28], other studies reported limited diagnostic value of MRI for distinguishing between partial and complete ACL tears [10, 27–29]. Furthermore, clear discrimination of the two bundles of ACL can sometimes be difficult [22]. In particular, PL bundle injuries are difficult to diagnose using a standard MRI protocol because the PL bundle has a more oblique course [17]; our data tended to confirm this. We found that diagnosis of PL bundle injuries indeed is more difficult, especially within 6 weeks of injury. Nevertheless, a previous study suggested that oblique coronal images can improve the ability of MRI to detect PL bundle injuries [25]. In that study, diagnostic accuracy of MRI to detect PL bundle injuries was between 67% and 80% with use of oblique coronal images [25]. However, it was still lower by 10% than that of the AM bundle. Consistent with the previous study, the accuracy of MRI diagnosis was less accurate (78%) for the PL bundle condition, although additional oblique coronal images were used.
We also found that the prediction of the condition of each bundle by MRI would be affected by time elapsed from injury to acquisition of MRI. Particularly, the injury severity of PL bundles tended to be overrated in the early MRI group. In the acute stage of ACL injury, a torn ACL can appear as a cloud-like mass accompanied by swelling of surrounding soft tissues. Furthermore, the morphology of the torn ACL fibers is obscured by the initial hemorrhage [28], making it more difficult to distinguish AM and PL bundles in an acute tear than in a chronic tear. Another possible explanation for the difference in PL bundle is that healing of a PL bundle with time may contribute to the more accurate rating of PL bundle integrity in the late MRI group. In fact, spontaneous healing of a torn ACL was demonstrated in several studies [2, 8, 11]. Nevertheless, further studies should be warranted to prove our speculation about the healing potential of the PL bundle.
In conclusion, our findings suggest that an isolated bundle tear is uncommon in patients with a symptomatic ACL tear warranting reconstruction. Coupled with the thorough clinical examinations, MRI can help surgeons predict a bundle injury pattern with satisfactory precision but caution should be used in predicting PL bundle injury using MRI, particularly MRI with early acquisition time from injury.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution has approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent was obtained.
This work was performed at the Joint Reconstruction Center, Seoul National University Bundang Hospital, Seoul, Korea.
References
- 1.Adachi N, Ochi M, Uchio Y, Sumen Y. Anterior cruciate ligament augmentation under arthroscopy. A minimum 2-year follow-up in 40 patients. Arch Orthop Trauma Surg. 2000;120:128–133. doi: 10.1007/s004020050028. [DOI] [PubMed] [Google Scholar]
- 2.Ahn JH, Chang MJ, Lee YS, Koh KH, Park YS, Eun SS. Non-operative treatment of ACL rupture with mild instability. Arch Orthop Trauma Surg. 2010;130:1001–1006. doi: 10.1007/s00402-010-1077-4. [DOI] [PubMed] [Google Scholar]
- 3.Ahn JH, Wang JH, Lee YS, Kim JG, Kang JH, Koh KH. Anterior cruciate ligament reconstruction using remnant preservation and a femoral tensioning technique: clinical and magnetic resonance imaging results. Arthroscopy. 2011;27:1079–1089. doi: 10.1016/j.arthro.2011.03.002. [DOI] [PubMed] [Google Scholar]
- 4.Borbon CA, Mouzopoulos G, Siebold R. Why perform an ACL augmentation? Knee Surg Sports Traumatol Arthrosc. 2012;20:245–251. doi: 10.1007/s00167-011-1565-2. [DOI] [PubMed] [Google Scholar]
- 5.Buda R, Di Caprio F, Giuriati L, Luciani D, Busacca M, Giannini S. Partial ACL tears augmented with distally inserted hamstring tendons and over-the-top fixation: an MRI evaluation. Knee. 2008;15:111–116. doi: 10.1016/j.knee.2007.12.002. [DOI] [PubMed] [Google Scholar]
- 6.Chhabra A, Starman JS, Ferretti M, Vidal AF, Zantop T, Fu FH. Anatomic, radiographic, biomechanical, and kinematic evaluation of the anterior cruciate ligament and its two functional bundles. J Bone Joint Surg Am. 2006;88(Suppl 4):2–10. doi: 10.2106/JBJS.F.00616. [DOI] [PubMed] [Google Scholar]
- 7.Collins MS, Unruh KP, Bond JR, Mandrekar JN. Magnetic resonance imaging of surgically confirmed anterior cruciate ligament graft disruption. Skeletal Radiol. 2008;37:233–243. doi: 10.1007/s00256-007-0423-2. [DOI] [PubMed] [Google Scholar]
- 8.Costa-Paz M, Ayerza MA, Tanoira I, Astoul J, Muscolo DL. Spontaneous healing in complete ACL ruptures: a clinical and MRI study. Clin Orthop Relat Res. 2012;470:979–985. doi: 10.1007/s11999-011-1933-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Crain EH, Fithian DC, Paxton EW, Luetzow WF. Variation in anterior cruciate ligament scar pattern: does the scar pattern affect anterior laxity in anterior cruciate ligament-deficient knees? Arthroscopy. 2005;21:19–24. doi: 10.1016/j.arthro.2004.09.015. [DOI] [PubMed] [Google Scholar]
- 10.Dejour D, Ntagiopoulos PG, Saggin PR, Panisset JC. The diagnostic value of clinical tests, magnetic resonance imaging, and instrumented laxity in the differentiation of complete versus partial anterior cruciate ligament tears. Arthroscopy. 2013;29:491–499. doi: 10.1016/j.arthro.2012.10.013. [DOI] [PubMed] [Google Scholar]
- 11.Fujimoto E, Sumen Y, Ochi M, Ikuta Y. Spontaneous healing of acute anterior cruciate ligament (ACL) injuries - conservative treatment using an extension block soft brace without anterior stabilization. Arch Orthop Trauma Surg. 2002;122:212–216. doi: 10.1007/s00402-001-0387-y. [DOI] [PubMed] [Google Scholar]
- 12.Hong L, Li X, Zhang H, Liu X, Zhang J, Shen JW, Feng H. Anterior cruciate ligament reconstruction with remnant preservation: a prospective, randomized controlled study. Am J Sports Med. 2012;40:2747–2755. doi: 10.1177/0363546512461481. [DOI] [PubMed] [Google Scholar]
- 13.Noyes FR, Mooar LA, Moorman CT, 3rd, McGinniss GH. Partial tears of the anterior cruciate ligament. Progression to complete ligament deficiency. J Bone Joint Surg Br. 1989;71:825–833. doi: 10.1302/0301-620X.71B5.2584255. [DOI] [PubMed] [Google Scholar]
- 14.Ochi M, Adachi N, Uchio Y, Deie M, Kumahashi N, Ishikawa M, Sera S. A minimum 2-year follow-up after selective anteromedial or posterolateral bundle anterior cruciate ligament reconstruction. Arthroscopy. 2009;25:117–122. doi: 10.1016/j.arthro.2008.10.011. [DOI] [PubMed] [Google Scholar]
- 15.Ohsawa T, Kimura M, Kobayashi Y, Hagiwara K, Yorifuji H, Takagishi K. Arthroscopic evaluation of preserved ligament remnant after selective anteromedial or posterolateral bundle anterior cruciate ligament reconstruction. Arthroscopy. 2012;28:807–817. doi: 10.1016/j.arthro.2011.11.033. [DOI] [PubMed] [Google Scholar]
- 16.Papalia R, Franceschi F, Vasta S, Di Martino A, Maffulli N, Denaro V. Sparing the anterior cruciate ligament remnant: is it worth the hassle? Br Med Bull. 2012;104:91–111. doi: 10.1093/bmb/ldr053. [DOI] [PubMed] [Google Scholar]
- 17.Petersen W, Zantop T. Partial rupture of the anterior cruciate ligament. Arthroscopy. 2006;22:1143–1145. doi: 10.1016/j.arthro.2006.08.017. [DOI] [PubMed] [Google Scholar]
- 18.Roberts CC, Towers JD, Spangehl MJ, Carrino JA, Morrison WB. Advanced MR imaging of the cruciate ligaments. Radiol Clin North Am. 2007;45:1003–1016, vi–vii. [DOI] [PubMed]
- 19.Sakane M, Fox RJ, Woo SL, Livesay GA, Li G, Fu FH. In situ forces in the anterior cruciate ligament and its bundles in response to anterior tibial loads. J Orthop Res. 1997;15:285–293. doi: 10.1002/jor.1100150219. [DOI] [PubMed] [Google Scholar]
- 20.Sampson MJ, Jackson MP, Moran CJ, Shine S, Moran R, Eustace SJ. Three Tesla MRI for the diagnosis of meniscal and anterior cruciate ligament pathology: a comparison to arthroscopic findings. Clin Radiol. 2008;63:1106–1111. doi: 10.1016/j.crad.2008.04.008. [DOI] [PubMed] [Google Scholar]
- 21.Serrano-Fernandez JM, Espejo-Baena A, Martin-Castilla B, De La Torre-Solis F, Mariscal-Lara J, Merino-Ruiz ML. Augmentation technique for partial ACL ruptures using semitendinosus tendon in the over-the-top position. Knee Surg Sports Traumatol Arthrosc. 2010;18:1214–1218. doi: 10.1007/s00167-010-1068-6. [DOI] [PubMed] [Google Scholar]
- 22.Siebold R, Fu FH. Assessment and augmentation of symptomatic anteromedial or posterolateral bundle tears of the anterior cruciate ligament. Arthroscopy. 2008;24:1289–1298. doi: 10.1016/j.arthro.2008.06.016. [DOI] [PubMed] [Google Scholar]
- 23.Sim J, Wright CC. The kappa statistic in reliability studies: use, interpretation, and sample size requirements. Phys Ther. 2005;85:257–268. [PubMed] [Google Scholar]
- 24.Sonnery-Cottet B, Lavoie F, Ogassawara R, Scussiato RG, Kidder JF, Chambat P. Selective anteromedial bundle reconstruction in partial ACL tears: a series of 36 patients with mean 24 months follow-up. Knee Surg Sports Traumatol Arthrosc. 2010;18:47–51. doi: 10.1007/s00167-009-0855-4. [DOI] [PubMed] [Google Scholar]
- 25.Steckel H, Vadala G, Davis D, Musahl V, Fu FH. 3-T MR imaging of partial ACL tears: a cadaver study. Knee Surg Sports Traumatol Arthrosc. 2007;15:1066–1071. doi: 10.1007/s00167-007-0337-5. [DOI] [PubMed] [Google Scholar]
- 26.Thomas S, Pullagura M, Robinson E, Cohen A, Banaszkiewicz P. The value of magnetic resonance imaging in our current management of ACL and meniscal injuries. Knee Surg Sports Traumatol Arthrosc. 2007;15:533–536. doi: 10.1007/s00167-006-0259-7. [DOI] [PubMed] [Google Scholar]
- 27.Umans H, Wimpfheimer O, Haramati N, Applbaum YH, Adler M, Bosco J. Diagnosis of partial tears of the anterior cruciate ligament of the knee: value of MR imaging. AJR Am J Roentgenol. 1995;165:893–897. doi: 10.2214/ajr.165.4.7676988. [DOI] [PubMed] [Google Scholar]
- 28.Van Dyck P, De Smet E, Veryser J, Lambrecht V, Gielen JL, Vanhoenacker FM, Dossche L, Parizel PM. Partial tear of the anterior cruciate ligament of the knee: injury patterns on MR imaging. Knee Surg Sports Traumatol Arthrosc. 2012;20:256–261. doi: 10.1007/s00167-011-1617-7. [DOI] [PubMed] [Google Scholar]
- 29.Van Dyck P, Vanhoenacker FM, Gielen JL, Dossche L, Van Gestel J, Wouters K, Parizel PM. Three tesla magnetic resonance imaging of the anterior cruciate ligament of the knee: can we differentiate complete from partial tears? Skeletal Radiol. 2011;40:701–707. doi: 10.1007/s00256-010-1044-8. [DOI] [PubMed] [Google Scholar]
- 30.Yagi M, Wong EK, Kanamori A, Debski RE, Fu FH, Woo SL. Biomechanical analysis of an anatomic anterior cruciate ligament reconstruction. Am J Sports Med. 2002;30:660–666. doi: 10.1177/03635465020300050501. [DOI] [PubMed] [Google Scholar]
- 31.Yasuda K, Kondo E, Ichiyama H, Kitamura N, Tanabe Y, Tohyama H, Minami A. Anatomic reconstruction of the anteromedial and posterolateral bundles of the anterior cruciate ligament using hamstring tendon grafts. Arthroscopy. 2004;20:1015–1025. doi: 10.1016/j.arthro.2004.08.010. [DOI] [PubMed] [Google Scholar]
- 32.Yasuda K, Kondo E, Kitamura N, Kawaguchi Y, Kai S, Tanabe Y. A pilot study of anatomic double-bundle anterior cruciate ligament reconstruction with ligament remnant tissue preservation. Arthroscopy. 2012;28:343–353. doi: 10.1016/j.arthro.2011.08.305. [DOI] [PubMed] [Google Scholar]
- 33.Yoon KH, Bae DK, Cho SM, Park SY, Lee JH. Standard anterior cruciate ligament reconstruction versus isolated single-bundle augmentation with hamstring autograft. Arthroscopy. 2009;25:1265–1274. doi: 10.1016/j.arthro.2009.05.020. [DOI] [PubMed] [Google Scholar]
- 34.Zantop T, Brucker PU, Vidal A, Zelle BA, Fu FH. Intraarticular rupture pattern of the ACL. Clin Orthop Relat Res. 2007;454:48–53. doi: 10.1097/BLO.0b013e31802ca45b. [DOI] [PubMed] [Google Scholar]