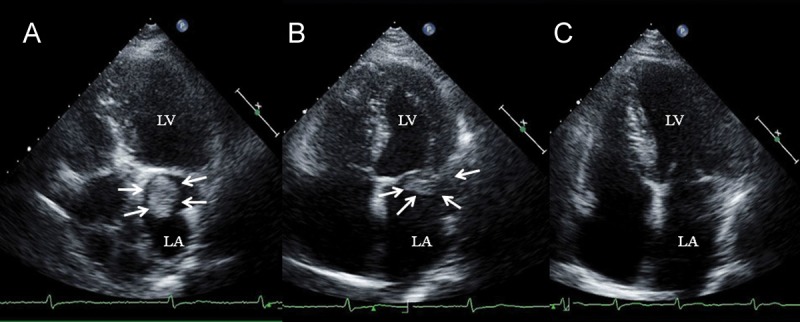
A 72-year-old woman was admitted to our hospital with acute exacerbation of chronic heart failure. Her medical history included chronic heart failure, permanent atrial fibrillation, and psychiatric disease. Despite a CHA2DS2-VASc score of 5, poor drug compliance compelled her to warfarin administration. Coarse crackles were evident over both lungs and a chest X-ray showed pulmonary congestion. Electrocardiography showed atrial fibrillation with a ventricular heart rate of 98. Blood tests revealed BNP 775.7 pg/mL and D-dimer 4.0 μg/mL. The heart failure was promptly compensated by intravenous furosemide. However, transthoracic echocardiography (TTE) demonstrated a mobile high echoic mass of 2.6 × 3.0 cm in the left atrium (LA) (Panel A, white arrows; LA, left atrium; LV, left ventricle). We administered heparin and warfarin, and TTE after 1 month showed that the LA mass had shrunk to 1.7 × 1.0 cm, confirming that it was thrombus (Panel B, white arrows). Warfarin was changed to dabigatran 300 mg/day because she had a delusional disorder. She has remained on dabigatran for 4 months without any serious bleeding complications, and TTE confirmed that the thrombus had disappeared (Panel C).
Dabigatran is a direct thrombin inhibitor that exerts anticoagulant effects by binding to the active site of thrombin. Since it acts independently of antithrombin, it can inhibit thrombin bound to fibrin and fibrin degradation products, implying that it also has thrombolytic properties. In fact, dabigatran possibly induced thrombolysis in this patient, indicating that this drug could be a therapeutic option for patients with intracardiac thrombus.