Over the past 25 years, epidemiologic studies of outcomes of sleep disordered breathing (SDB) have focused primarily on cardiovascular diseases, injuries and traffic crashes, and diminished quality of life, mental health, and cognition. In 2012, two observational studies—one from Spain1 and one from Wisconsin2—added cancer to the list of conditions found to be associated with SDB. These studies were inspired by recent proof-of-concept evidence from animal models demonstrating accelerated tumor progression in mice exposed to intermittent hypoxia,3,4 and basic science research relating experimentally induced intermittent hypoxia to processes (e.g., pro-angiogenic, pro-metastatic) that may promote cancer progression.5–9 The Spanish study followed cohorts of adult patients initially referred for clinical SDB evaluations for subsequent cases of incident cancer. The Wisconsin-based study followed a cohort of employed adults with polysomnographically determined SDB status at baseline for cancer mortality. Both studies found positive associations between SDB and cancer outcomes, especially when SDB was characterized by severity of nocturnal hypoxia. Thus, limited evidence linking SDB and cancer now exists. However, we are in nascent stages of the scientific process that should eventually delineate relationships between these two conditions. We expect there will soon be an acceleration of epidemiologic investigations of SDB and cancer that, along with parallel work in the basic sciences, will begin to clarify associations of SDB phenotypes and severity levels with specific cancers as well as the roles (if any) of SDB in carcinogenesis, tumor progression, metastasis, and mortality.
As with the two 2012 investigations,1,2 most early epidemiologic studies of SDB and cancer will likely build on data collected in existing datasets and studies already in-progress—studies not specifically designed at the outset to address SDB-cancer hypotheses. In this issue of SLEEP, Christensen and colleagues provide another example of this approach in which they investigated the association of symptoms of SDB (assessed in the early 1990s) and subsequent cancer diagnoses in Copenhagen City Heart Study subjects.10 Participant-reported SDB symptoms queried included sleepiness, snoring, and breathing pauses. Cancer incidence data were accumulated from Denmark-wide hospital discharge and mortality registries, and over an average of 13 years of follow-up, 1,985 subjects were identified as being diagnosed with cancer from a total 8,783 baseline subjects. Results were essentially “negative”— the authors found no evidence that baseline SDB symptoms were strongly associated, in a dose-response fashion, with incident cancer. Thus, the Christensen findings raise a question: do their results refute previous limited evidence in favor of a SDB-cancer association?
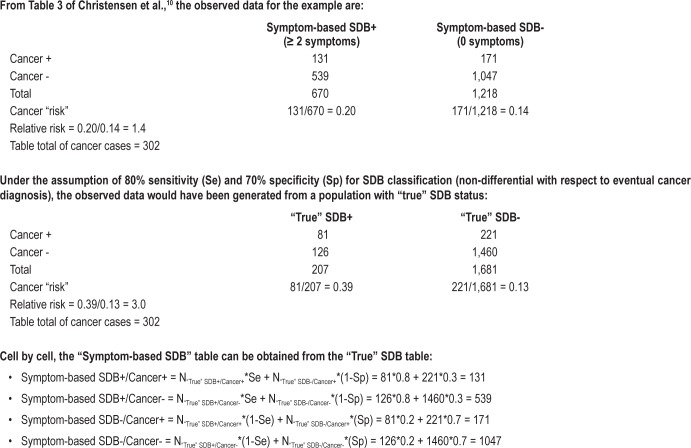
In our view, the answer—for the time being—is no. While the Christensen study had important strengths—a large population-based sample, prospective design with lengthy follow-up, and careful control for several confounding variables—it must also be interpreted in light of its limitations. Most salient was the characterization of SDB by symptom-based self-report. Classification of SDB by symptom-based report has been used in many previous studies, and there have been many evaluations of the validity of symptom-based report relative to objective SDB assessments. In a systematic review, Abrishami and coauthors11 summarized validation studies examining the sensitivity and specificity of a variety of symptom-based instruments for SDB prediction. Generally, symptom-based instruments had sensitivities and specificities of 65% to 80% and 45% to 60%, respectively, for identifying SDB when referenced to standards such as polysomnography. If there truly is a positive association between SDB and cancer, and if SDB misclassification is unrelated to cancer risk, then SDB-cancer associations measured in a study that used symptom-based SDB assessment would likely underestimate SDB-cancer associations.12 As a simplified illustration using data from the Christensen paper,10 consider the last rows of their Table 3, in which the number of incident cancer cases is provided for subsets of subjects stratified by number of SDB symptoms. Of the 670 subjects who reported ≥ 2 SDB symptoms, 131 developed cancer (131/670 ≈ a 20% observed “risk” of developing cancer); and, of the 1,218 subjects reporting no symptoms, 171 developed cancer (171/1,218 ≈ 14% “risk”). The approximate unadjusted relative risk is then 20%/14% = 1.4, indicating that subjects with ≥ 2 SDB symptoms had a 40% higher risk of developing cancer compared to those without symptoms. For given sensitivity and specificity values, the degree of underestimation of the SDB-cancer association due to SDB misclassification can be estimated. If we optimistically assume that SDB was classified with sensitivity = 80% and specificity = 70%, then the most likely “actual” (but unobserved) unadjusted relative risk in the sample would be 3.0 (see Figure 1). That is, SDB so-classified would produce an estimate only 20% ([1.4-1]/[3.0-1] = 0.2) of the magnitude of SDB-associated risk elevation that would be expected to be measured if SDB had been polysomnographically assessed. The sought-after SDB-cancer association “signal” may be almost completely obscured by the “noise” resulting from (in particular) nonspecific SDB assessment. Thus, negative studies that employ symptom-based SDB assessment cannot be taken as strongly refuting important SDB-cancer associations.
Figure 1.
Calculations for the simplified illustrative example.
As with the new Christensen study10 and the Spanish and Wisconsin SDB-cancer studies of 2012,1,2 there will be continued examinations of SDB-cancer associations in currently existing datasets and study populations. These will likely share some of the substantial limitations of the (now at least three) previous studies that were not designed from the outset to examine SDB-cancer associations. Ideal future epidemiologic investigations specifically established to assess SDB-cancer outcomes would include: sufficiently large population-based samples to examine common cancer subtypes; long-term follow-up to encompass extended cancer preclinical periods and allow for distinguishing carcinogenic from cancer-prognostic effects of SDB; objective measures of SDB; robust assessment of important potential confounding factors (e.g., high-quality nutrition and physical activity data); and accurate measurement of SDB treatments undertaken by study subjects. While these approaches are unlikely to co-occur in any one study, future studies may more closely approach this ideal than might be achieved by interrogation of existing cohorts and datasets. Still, we expect investigators will continue to take advantage of relatively inexpensive opportunities to examine SDB-cancer associations in databases from extant cohorts. Indeed, we hope that, like Christensen and colleagues, other investigative teams will explore SDB-cancer associations in existing study populations and publish findings regardless of whether they are “positive” or “negative” to prevent publication bias. Even more, we encourage the undertaking of investigations specifically designed to examine SDB-cancer associations—including, perhaps most promisingly, the relationship of SDB, or SDB treatment, with cancer progression and prognosis in patients newly diagnosed with specific cancers. Such investigations will likely be logistically challenging, expensive, and will not produce quick results, but the need for the research is paramount. A strong causal association between highly and increasingly13 prevalent SDB and carcinogenesis would have clear implications for preventing and managing SDB in persons without cancer, and a causal relationship between SDB and survival in patients with cancer would suggest the need for rapid diagnosis and treatment of SDB in such patients.
CITATION
Peppard PE; Nieto FJ. Here come the sleep apnea-cancer studies. SLEEP 2013;36(10):1409-1411.
DISCLOSURE STATEMENT
The authors have indicated no financial conflicts of interest.
REFERENCES
- 1.Campos-Rodriguez F, Martinez-Garcia MA, Martinez M, et al. Spanish Sleep Network. Association between obstructive sleep apnea and cancer incidence in a large multicenter Spanish cohort. Am J Respir Crit Care Med. 2013;187:99–105. doi: 10.1164/rccm.201209-1671OC. [DOI] [PubMed] [Google Scholar]
- 2.Nieto FJ, Peppard PE, Young T, Finn LA, Hla KM, Farre R. Sleep-disordered breathing and cancer mortality: results from the Wisconsin Sleep Cohort Study. Am J Respir Crit Care Med. 2012;186:190–4. doi: 10.1164/rccm.201201-0130OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Almendros I, Montserrat JM, Ramirez J, et al. Intermittent hypoxia enhances cancer progression in a mouse model of sleep apnoea. Eur Respir J. 2012;39:215–7. doi: 10.1183/09031936.00185110. [DOI] [PubMed] [Google Scholar]
- 4.Almendros I, Montserrat JM, Torres M, et al. Obesity and intermittent hypoxia increase tumor growth in a mouse model of sleep apnea. Sleep Med. 2012;13:1254–60. doi: 10.1016/j.sleep.2012.08.012. [DOI] [PubMed] [Google Scholar]
- 5.Liu Y, Song X, Wang X, et al. Effect of chronic intermittent hypoxia on biological behavior and hypoxia-associated gene expression in lung cancer cells. J Cell Biochem. 2010;111:554–63. doi: 10.1002/jcb.22739. [DOI] [PubMed] [Google Scholar]
- 6.Toffoli S, Michiels C. Intermittent hypoxia is a key regulator of cancer cell and endothelial cell interplay in tumours. FEBS J. 2008;275:2991–3002. doi: 10.1111/j.1742-4658.2008.06454.x. [DOI] [PubMed] [Google Scholar]
- 7.Rofstad EK, Gaustad JV, Egeland TA, Mathiesen B, Galappathi K. Tumors exposed to acute cyclic hypoxic stress show enhanced angiogenesis, perfusion and metastatic dissemination. Int J Cancer. 2010;127:1535–46. doi: 10.1002/ijc.25176. [DOI] [PubMed] [Google Scholar]
- 8.Cairns RA, Kalliomaki T, Hill RP. Acute (cyclic) hypoxia enhances spontaneous metastasis of KHT murine tumors. Cancer Res. 2001;61:8903–8. [PubMed] [Google Scholar]
- 9.Almendros I, Montserrat JM, Torres M, et al. Intermittent hypoxia increases melanoma metastasis to the lung in a mouse model of sleep apnea. Respir Physiol Neurobiol. 2013;186:303–7. doi: 10.1016/j.resp.2013.03.001. [DOI] [PubMed] [Google Scholar]
- 10.Christensen AS, Clark A, Salo P, et al. Symptoms of sleep disordered breathing and risk of cancer: A prospective cohort study. Sleep. 2013;36:1429–35. doi: 10.5665/sleep.3030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Abrishami A, Khajehdehi A, Chung F. A systematic review of screening questionnaires for obstructive sleep apnea. Can J Anesth. 2010;57:423–38. doi: 10.1007/s12630-010-9280-x. [DOI] [PubMed] [Google Scholar]
- 12.Rothman KJ, Greenland S, Lash TL. Modern epidemiology. 3rd ed. Philadelphia: Lippincott Williams & Wilkins; 2008. pp. 201–2. [Google Scholar]
- 13.Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM. Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol. 2013 Apr 14; doi: 10.1093/aje/kws342. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]