Abstract
Study Objective:
To examine the effects of obesity and frequent mental distress (FMD) on the relationship of sleep duration with coronary heart disease (CHD), stroke, and diabetes.
Design:
Cross-sectional study.
Setting:
Population-based surveillance.
Participants:
There were 54,269 adults age 45 y or older who completed the 2010 Behavioral Risk Factor Surveillance System survey in 14 states.
Results:
Nearly one third (31.1% or an estimated 11.1 million) of respondents age 45 y and older reported being short sleepers (≤ 6 h), 64.8% being optimal sleepers (7-9 h), and 4.1% being long sleepers (≥ 10 h) in a 24-h period. Compared with the optimal sleep duration, both short and long sleep durations were significantly associated with obesity, FMD (mental health was not good ≥ 14 days during the past 30 days), CHD, stroke, and diabetes after controlling for sex, age, race/ethnicity, and education. The U-shaped relationships of sleep duration with CHD, stroke, and diabetes were moderately attenuated by FMD. The relationship between sleep duration and diabetes was slightly attenuated by obesity.
Conclusions:
Sleep duration had U-shaped relationships with leading chronic diseases. Further prospective studies are needed to determine how mental health and maintenance of a normal weight may interact with sleep duration to prevent chronic diseases.
Citation:
Liu Y; Wheaton AG; Chapman DP; Croft JB. Sleep duration and chronic diseases among US adults age 45 years and older: evidence from the 2010 Behavioral Risk Factor Surveillance System. SLEEP 2013;36(10):1421-1427.
Keywords: Chronic disease, mental health, population-based survey, sleep duration
INTRODUCTION
There is a perception that the proportion of US adults who report short sleep duration (≤ 6 h per 24-h period) is greater than that of decades ago; however, survey trends are not consistent.1–3 It has been suggested that short sleep duration may be explained by longer working hours; lifestyle changes, such as increased family time; use of electronics such as television or computers; and shift work.3,4 Research has demonstrated that both short and long sleep duration are associated with obesity, depression, anxiety, diabetes mellitus, and cardiovascular disease,5–14 although definitions of short and long sleep duration vary across studies.1 However, underlying mechanisms for relationships between sleep duration and chronic diseases are understudied.
Evidence-based studies suggest that there are at least two potential pathways that may explain why short sleep duration is associated with chronic diseases. First, short sleep duration may result in greater insulin resistance, as well as decreased leptin and increased ghrelin through regulation of the hypothalamic-pituitary-adrenal axis. This may lead to metabolic abnormalities and weight gain.15,16 Chronic metabolic impairments such as obesity may subsequently lead to the development of diabetes, heart disease, and stroke.8,9,17–19 This is corroborated by results from a prospective study with 10-y follow-up among women that body mass index (BMI) may significantly attenuate the association of short and long sleep duration with diabetes.17 Therefore, obesity may play an intermediate or mediating role on relationships between sleep duration and chronic diseases. Evidence also demonstrates that sleep duration is associated with depression and anxiety.20,21 Depression and/or anxiety, whether present separately or simultaneously, are independent risk factors for type 2 diabetes, hypertension, and cardiovascular disease.17,22–24 Therefore, mental disorders also may mediate relationships between sleep duration and chronic diseases.
This study assesses relationships between sleep duration and selected chronic diseases among US adults age 45 y or older in 14 states using data from the 2010 Behavioral Risk Factor Surveillance System (BRFSS) and examines whether those relationships were attenuated by frequent mental distress (FMD) and/or obesity. Because of the variety of public health information collected from the nation's largest annual number of adult respondents, the BRFSS sleep data have been utilized to examine socioeconomic determinants, state and regional differences, and correlations with chronic diseases and health risk behaviors.14,25–40
METHODS
Data Source
The BRFSS is a random-digital-dialing telephone survey of more than 450,000 annual respondents that is conducted by the state health departments in collaboration with the Centers for Disease Control and Prevention in all 50 states, the District of Columbia, and US territories. The BRFSS collected data on health-related behaviors that are linked to chronic diseases and other conditions among the adult population (age 18 y or older) living in households with landline telephones in 2010. Disproportional sampling of respondents defined by race/ethnicity, sex, or age may vary between states and each sample is weighted to the respondent's probability of selection in order to obtain a study population representative of a given state. Trained interviewers administered standardized questionnaires to all adult respondents. In addition to the core questionnaire about chronic diseases and mental health, 14 states (Arkansas, California, Connecticut, Delaware, District of Columbia, Hawaii, Kansas, Maryland, Michigan, Minnesota, Missouri, Nebraska, Nevada, and Oregon) administered the optional sleep module in 2010. All respondents had given oral informed consent to participate in the interview. The response rate (complete and partial interview relative to total eligible households) varied by state among the 14 states and ranged from 39.0% to 68.8% (median = 52.7%) in 2010.41 A detailed description of the BRFSS survey design, data collection, and full-text questionnaires as well as the public access electronic data files with no personal identifiers can be found at http://www.cdc.gov/brfss.
Measures
Awareness of having chronic diseases was defined through subjects' affirmative responses to the question of whether they had ever been told by a doctor or other health professional that they had diabetes mellitus; coronary heart disease (CHD), which included a heart attack, angina pectoris, and/or CHD; or stroke. Persons who reported “don't know/not sure” were defined as not having the condition. Those who reported having borderline diabetes or prediabetes or having diabetes only during pregnancy were defined as not having diabetes mellitus. Including the small number of persons with borderline diabetes or prediabetes in the nondiabetes group biases the results toward the null finding (a conservative approach) if these persons are also more likely to have a short sleep duration while excluding these persons from the analyses would have led to an overestimate of the actual relationship.
Sleep duration was based on the response to the question, “On average, how many hours of sleep do you get in a 24-h period? Think about the time you actually spend sleeping or napping, not just the amount of sleep you think you should get.” As in all other CDC surveillance systems, duration of sleep was reported as whole numbers rounded to the nearest hour. The National Sleep Foundation suggests that most adults need 7-9 h of sleep per night (www.sleepfoundation.org) whereas the National Heart, Lung, and Blood Institute recommends 7-8 h a day for adults (www.nhlbi.nih.gov/health/health-topics/topics/sdd/howmuch.html/). The Institute of Medicine report on sleep disorders refers to an average basal need of 7-8 h per night for adults.42 However, preliminary data analyses for this study showed that the number of sleep hours was not linearly associated with chronic diseases, and another study had observed that the strength of the associations with chronic disease was quite similar for 7, 8, and 9 h of sleep.11 Therefore, sleep duration for these analyses was defined as short (≤ 6 h), optimal (7-9 h), and long (≥ 10 h).
Sociodemographic characteristics that were examined as covariates in the association between sleep duration and chronic diseases included sex, age in y (45-54, 55-64, and 65 y or older), race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, and other non-Hispanic), and education (less than high school graduate, high school diploma or general equivalency diploma recipient, and some college or college graduate).
FMD was defined if respondents indicated ≥ 14 days to the question “about your mental health, which includes stress, depression and problems with emotions, for how many days during the past 30 days was your mental health not good?” Because a lengthy telephone survey such as the BRFSS is limited to a single-item mental health question, FMD was developed as an indicator of the perceived mental distress burden of common mental disorders and had been utilized previously to examine correlations with a sleep indicator, depression, anxiety, physical impairments, and sociodemographic characteristics, as well as to examine geographic variations between states.25,43,44 FMD was derived based on the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR).45 Receiver operating characteristic (ROC) analyses of the number of days of the BRFSS FMD measure with other measures of clinically relevant psychiatric symptomatology (the Patient Health Questionnaire-8 in a US population sample of 170,814 adults, and the Kessler-6 in a US population sample of 141,560 adults) demonstrated 0.87 and 0.84 of the respective areas under the curve, which suggest good accuracy for FMD.46
Assessment of obesity was based on the BMI (kg/m2) calculated from self-reported height in inches and weight in pounds and was dichotomized into nonobese (BMI < 30.0 kg/m2) and obese (BMI ≥ 30 kg/m2). The BMI-based weight classification has been used often in epidemiological surveys.47,48 It has been widely recognized from validation studies that the prevalence of obesity calculated from self-reported height and weight are underestimated.49–51 However, it is a cost-effective approach to obtain BMI information from respondents in such a large-scale population-based study.
Study Population
Because of the low prevalence of chronic diseases among adults aged 18-44 y (1.2% with CHD, 0.7% with stroke, and 2.8% with diabetes), only data for respondents aged 45-99 y were analyzed in this study, as analyses incorporating the younger age groups were assumed to provide unstable estimates of mediation effects. Restricting the population sample did not affect the sampling weight because of the BRFSS study design. In 2010, 56,640 adults age 45 y or older in the 14 states answered BRFSS questions about sociodemographic characteristics, self-reported height and weight, chronic disease, and sleep duration. Those respondents who had missing information on sleep duration (n = 2,352) and chronic diseases (n = 19) were excluded. The remaining 54,269 respondents (95.8%) were included in the current study. The excluded population who were missing information for sleep duration were more likely to report having diabetes (16.3% versus 13.2%, P < 0.05) and stroke (6.4% versus 4.3%, P < 0.001) than in the included population. The prevalence of obesity, FMD, and CHD was similar in excluded and included populations. However, due to the relatively small sample size of the excluded population, the influence of the missing data on our results is likely limited.
Statistical Analyses
First, the distributions of selected characteristics and sleep duration among study respondents were examined. Then, weighted prevalence estimates of obesity, FMD, and selected chronic diseases were obtained for groups defined by selected sociodemographic characteristics and sleep duration. Logistic regression analyses were performed to examine associations of short and long sleep duration with FMD, obesity, and selected chronic diseases and were adjusted for sex, age, race/ethnicity, and education. The magnitude of a potential mediation effect was assessed by measuring the percentage of change in effect between models with and without the specific proposed mediator = [(OR no mediator − OR with mediator) / (OR no mediator − 1)] × 100.52,53 A significant mediation effect was defined only if sleep duration also was significantly associated with both the potential mediator and chronic disease and the potential mediator was significantly associated with chronic disease.54 A modified Sobel test, which is tailored for a dichotomized outcome variable, was conducted to assess whether there was a significant effect for the potential mediator in the relationship between sleep duration and each of the three chronic diseases.55 A partial mediating effect was determined to be present if the relationship between sleep duration and chronic disease still remained significant when the potential mediator was added to the model. A complete mediating effect was defined if the relationship between sleep duration and chronic disease was no longer significant with the potential mediator included in the model. All analyses were conducted using SAS-callable SUDAAN to account for the complex sampling design.56 The statistical significance level was denoted as P < 0.05.
RESULTS
Among 54,269 respondents age 45 y and older, 33.1% were age 65 y and older; 52.8% were women; 76.5% were non-Hispanic white; 5.7% were non-Hispanic black; 10.2% were Hispanic; and 64.5% had more than a high school education (Table 1). Sleeping on average ≤ 6 h was reported by 31.1% of respondents (an estimated 11.1 million adults age 45 y or older), and only 4.1% (an estimated 1.4 million adults age 45 y or older) reported usually sleeping ≥ 10 h in a 24-h period. In addition, 28.8% of respondents were obese and 9.7% had FMD. Respondents reported having CHD (10.9%), stroke (4.3%), or diabetes (13.2%). Of all study respondents, only a small percentage reported having all three diseases (0.6%), whereas 4.1% reported having any two, 9.6% reported diabetes only, 6.8% reported CHD only, and 2.2% reported stroke only.
Table 1.
Distributions of selected characteristics among adults age 45 years and older, 14 states,a Behavioral Risk Factor Surveillance System, 2010
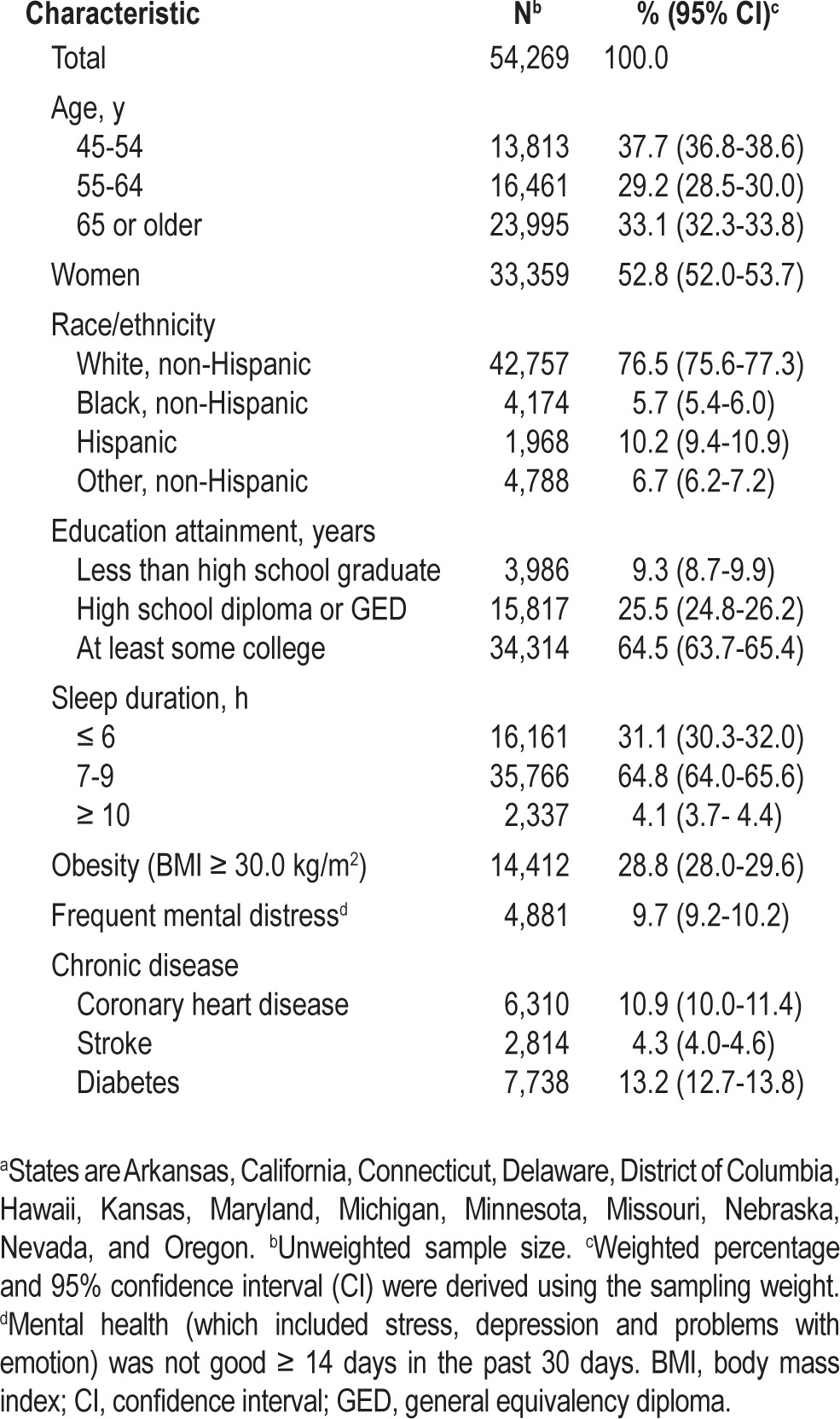
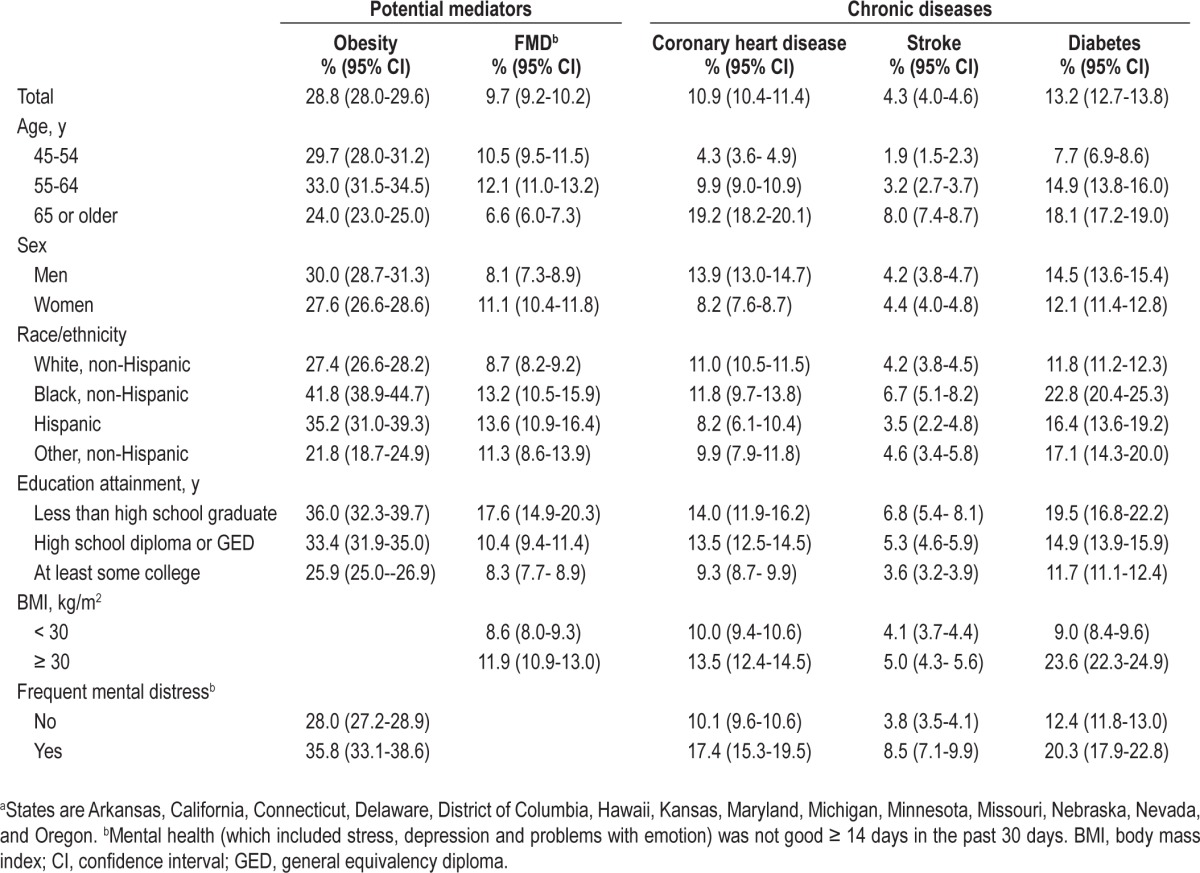
Table 2 presents the weighted percentages of obesity, FMD, and chronic diseases by selected characteristics. Compared to respondents age 65 y and older, those age 45-54 y and 55-64 y had higher percentages of obesity and FMD but had a lower prevalence of CHD, stroke, and diabetes (P < 0.05). Men reported a higher percentage of obesity, CHD, and diabetes but reported a lower percentage of FMD than women (P < 0.05). Non-Hispanic blacks and Hispanics had a higher prevalence of obesity, FMD, and diabetes than non-Hispanic whites (P < 0.05). There was an inverse relationship between education and each of the five conditions (P < 0.05). Obese respondents were more likely to report having FMD, CHD, and diabetes than did nonobese respondents (P < 0.05). Persons reporting FMD were more likely than those without FMD to report being obese (P < 0.05) or to report having one or more of the three chronic diseases (P < 0.05).
Table 2.
Weighted percentages of potential mediators and chronic diseases by selected characteristics among adults age 45 years and older, 14 states,a Behavioral Risk Factor Surveillance System, 2010
Associations Between Sleep Duration, Obesity, FMD, and Chronic Disease
Compared to respondents reporting the optimal 7-9 h, short sleepers reported a higher prevalence of obesity, FMD, CHD, stroke, and diabetes (P < 0.05; Table 3). Long sleepers also reported a higher prevalence of obesity, FMD, and the three chronic diseases than did the optimal sleepers. Odds ratios were obtained to examine the association of sleep duration with obesity, FMD, and chronic diseases using logistic regression models. Without controlling for any covariates, the likelihood for reporting obesity, FMD, CHD, stroke, and diabetes were significantly greater among both short and long sleepers compared to optimal sleepers (Model 1). These associations persisted after controlling for sex, age, race/ethnicity, and education (Model 2; P < 0.05).
Table 3.
The association of sleep duration with potential mediators and chronic diseases among adults age 45 years or older, 14 states,a Behavioral Risk Factor Surveillance System, 2010
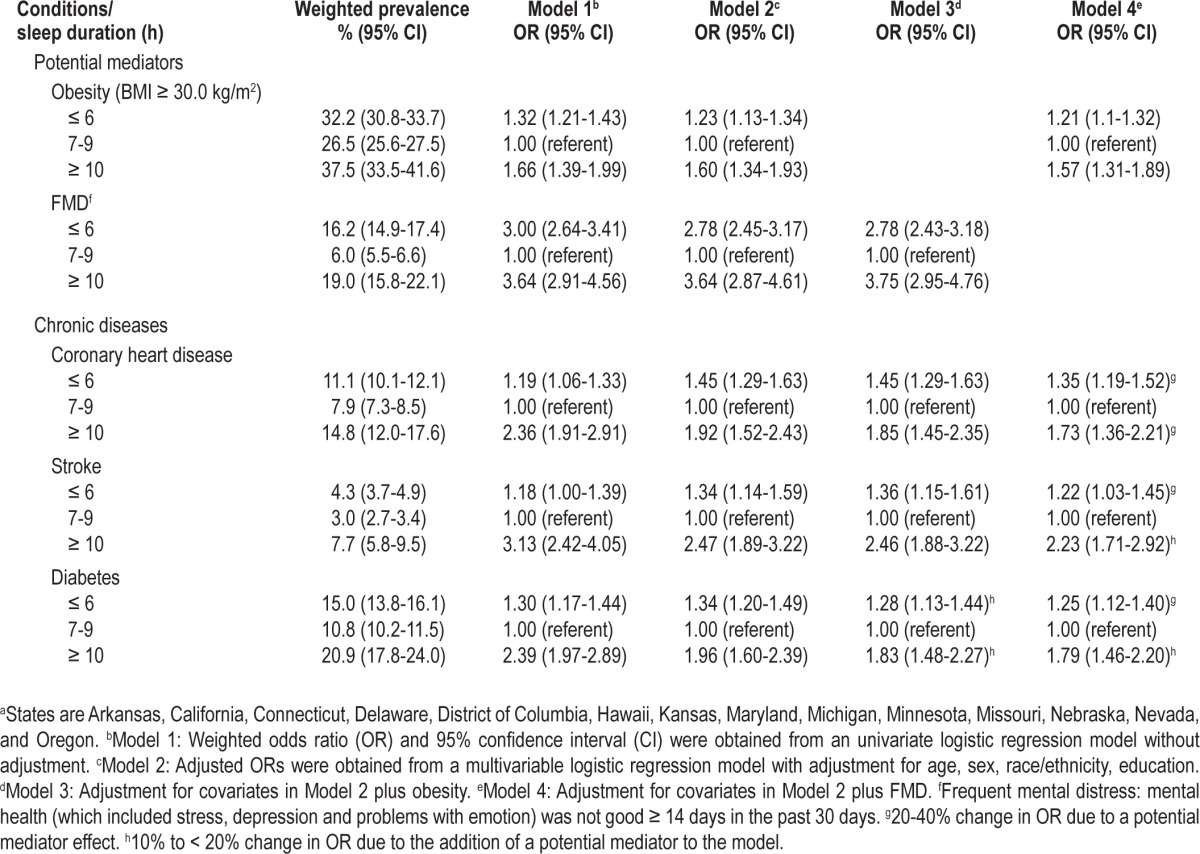
Mediation Effects
The increased likelihoods of CHD and stroke among short and long sleepers in comparison with optimal sleepers were not affected by adding obesity to the previous multivariable regression models and remained statistically significant (Model 3). However, the likelihood of diabetes was slightly attenuated after further controlling for obesity (Model 3). When adjusting for FMD in addition to age, sex, race/ethnicity, and education, a moderate reduction in the likelihood of CHD (Model 4) was observed for both short and long sleep duration, whereas moderate reductions in the odds of stroke and diabetes were observed for short sleep duration. In contrast, FMD only slightly attenuated the association of long sleep duration with stroke and diabetes (Model 4). In addition, the significant U-shaped association between sleep duration and obesity persisted after controlling for the sociodemographic covariates and FMD (Model 4), as did the significant U-shaped association between sleep duration and FMD after the adjustment for sociodemographics and obesity (Model 3). The results from the Sobel test for mediation supported these findings (data not shown).
DISCUSSION
This study demonstrated that compared with optimal sleep duration (7-9 h per day), both short (≤ 6 h per day) and long (≥ 10 h per day) sleep duration were significantly associated with CHD, stroke, and diabetes among adults age 45 y or older. These associations were more pronounced with long sleep duration than with short sleep duration. Furthermore, these relationships were moderately attenuated but not completely explained by either FMD or obesity. Therefore, our findings add some insights into the possible underlying mechanism of the association between sleep duration and chronic disease.
Previous findings have indicated that both short and long sleep duration are associated with increased risk for obesity. Obesity, in turn, has been shown as a robust risk factor for diabetes and cardiovascular diseases.9,12,18,57,58 For example, the results observed among 70,026 women age 30-55 y in the Nurse's Health Study suggested that compared to optimal sleep (defined as 8 h per day in the study), the significant relationship of diabetes with short sleep (defined as ≤ 5 sleep h) did not persist after adjustment for categorical BMI but still remained with long sleep (defined as ≥ 9 sleep h).9 Another prospective study indicated that significant relationships between short and long sleep duration and diabetes were attenuated by obesity among 1,139 men aged 40-70 y in the Massachusetts Male Aging Study.12 The consistency of these and previous findings might be explained by obesity playing a potential mediator between short sleep and diabetes. However, the association between long sleep duration and chronic disease is less clearly understood. One possible explanation is that the longer sleep duration could also be linked to obesity or impaired mental health.5,6 Additionally, associations of CHD and stroke with sleep duration were not attenuated by obesity. One possible explanation was that sleep duration might be associated with CHD or stroke through other mediators such as mental distress or hypertension.
Depression and anxiety often coexist with sleep loss and many chronic diseases.5,6,20,21 Previously observed relationships between frequent insufficient sleep (defined as ≥ 14 days of inadequate sleep or rest in the past 30 days) and FMD indicated that perceived sleep loss was highly associated with mental health.44 Results regarding significant relationships between FMD and chronic diseases from prospective studies were also consistent with our findings.59 Prior research among 60,028 women age 25-46 y in a prospective Nurse's Health Study suggested that depression might confound or mediate the association between long sleep duration and mortality.60 The current investigation appears to be the first to assess FMD as a potential mediator in the relationship between sleep duration and chronic disease. However, well-designed prospective studies are needed to assess whether psychological distress or depression are causal intermediates or confounders of this association. In addition, experimental studies with sleep deprivation suggest that prolonged sleep loss reduces human natural immune function,61,62 exacerbates inflammation,63,64 and could lead to metabolic syndrome disease and other chronic diseases.65 Therefore, future research is warranted to explore other potential pathways.
Although this is the largest study to date to address the potential mediation effect in the relationship between sleep duration and chronic diseases, several limitations should be noted. First, because the BRFSS is a cross-sectional study, it is not possible to make causal inferences and determine whether short or long sleep duration result in obesity, FMD, and chronic conditions, or vice versa. Second, sample selection bias due to the low response rate may also have occurred because institutionalized persons, persons residing in households without landline telephones, younger adults who only have cellular telephones, and persons with severely impaired physical or mental health might not have been reached or have had the means to complete the BRFSS survey and thus were not included in the survey. However, the effect of potential systematic bias is likely limited as the moderately positive relationship between sleep duration and chronic disease revealed in our study is consistent with results from prior research.7–9 Third, self-reported sleep duration on national surveillance systems has not been validated by polysomnography or actigraphy and may not be as accurate as these objective measures and may have underestimated a true association with chronic diseases association if poor sleep duration is overreported. In addition, due to the self-reported nature of all examined variables, an underreporting of chronic diseases (not confirmed by medical records or self-reported medication usage), FMD, and obesity (calculated from respondents' self-reported height and weight) may have occurred,66,67 potentially resulting in a stronger relationship of short and long sleep duration with the outcomes in this study. Finally, our results were derived from a sample of the population that was restricted to adult respondents in 14 states and may not represent findings for the entire US. However, the overall percentage of short sleep duration and the distribution of sleep duration in the BRFSS study population are comparable to findings for sleep duration in study populations for the National Health and Nutrition Examination Survey68 and the National Health Interview Survey.69
Sleep duration may not reflect quality of sleep because persons with long sleep durations also may have poor sleep quality.70 Thus, sleep duration tends to have a U-shaped relationship with health outcomes, with at least one study suggesting a significant relationship for sleep durations < 5 h with diabetes, myocardial infarction, and stroke compared to 7 h of sleep but no significant differences for persons reporting 5-6 h.14 Another sleep indicator, perceived insufficient sleep (number of days without enough rest or sleep in the past 30 days), may be a good alternative to address the quality of sleep and tends to have a direct linear relationship with health outcomes. Several studies of BRFSS sleep data demonstrate that both perceived insufficient sleep and sleep duration are correlated with obesity, diabetes, cardiovascular disease, high blood pressure, arthritis, and asthma.14,28,30,31,39 One study demonstrated that when both sleep indicators are evaluated together, each demonstrates unique effects with different cardiometabolic health outcomes.14 This is the first study to examine potential mediators for the association of sleep duration with chronic diseases. These findings are consistent with previous findings that the significant associations of the number of days of frequent insufficient sleep with various chronic disease outcomes are mediated significantly but not fully by frequent mental distress and/or obesity.39
CONCLUSION
The current study suggests that short and particularly long sleep durations (≤ 6 h and ≥ 10 h, respectively) are significantly associated with CHD, stroke, and diabetes among adults age 45 y or older, even after controlling for age, sex, race/ethnicity, education, obesity, or FMD. These results suggest that physicians should monitor mental well-being and body weight in addition to sleep health for patients with chronic disease.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention. This paper was presented in part at the National Sleep Foundation's Sleep Health & Safety 2013 conference on March 1-2, 2013 in Washington, DC.
REFERENCES
- 1.Bin YS, Marshall NS, Glozier N. Secular trends in adult sleep duration: a systematic review. Sleep Med Rev. 2012;16:223–30. doi: 10.1016/j.smrv.2011.07.003. [DOI] [PubMed] [Google Scholar]
- 2.Knutson KL, Cauter EV, Rathouz PJ, Deleire T, Lauderdale DS. Trends in the prevalence of short sleepers in the USA: 1975-2006. Sleep. 2010;33:37–45. doi: 10.1093/sleep/33.1.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Luckhaupt SE, Tak S, Calvert GM. The prevalence of short sleep duration by industry and occupation in the National Health Interview Survey. Sleep. 2010;33:149–59. doi: 10.1093/sleep/33.2.149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Basner M, Fomberstein KM, Razavi FM, et al. American time use survey: sleep time and its relationship to waking activities. Sleep. 2007;30:1085–95. doi: 10.1093/sleep/30.9.1085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Van den Berg JF, Luijendijk HJ, Tulen JH, Hofman A, Neven AK, Tiemeier H. Sleep in depression and anxiety disorders: a population-based study of elderly persons. J Clin Psychiatry. 2009;70:1105–13. doi: 10.4088/JCP.08m04448. [DOI] [PubMed] [Google Scholar]
- 6.Van Mill JG, Hoogendijk WJ, Vogelzangs N, van Dyck R, Peninx BW. Insomnia and sleep duration in a large cohort of patients with major depressive disorders and anxiety disorders. J Clin Psychiatry. 2010;71:239–46. doi: 10.4088/JCP.09m05218gry. [DOI] [PubMed] [Google Scholar]
- 7.Gangwisch JE, Malaspina D, Boden-Albala B, Heymsfield SB. Inadequate sleep as a risk factor for obesity: analyses of the NHANES I. Sleep. 2005;28:1289–96. doi: 10.1093/sleep/28.10.1289. [DOI] [PubMed] [Google Scholar]
- 8.Gottlieb DJ, Punjabi NM, Newman AB, et al. Association of sleep time with diabetes mellitus and impaired glucose tolerance. Arch Intern Med. 2005;165:863–7. doi: 10.1001/archinte.165.8.863. [DOI] [PubMed] [Google Scholar]
- 9.Ayas NT, White DP, Manson JE, et al. A prospective study of sleep duration and coronary heart disease in women. Arch Intern Med. 2003;163:205–9. doi: 10.1001/archinte.163.2.205. [DOI] [PubMed] [Google Scholar]
- 10.Magee CA, Kritharides L, Attia J, McElduff P, Banks E. Short and long sleep duration are associated with prevalent cardiovascular disease in Australian adults. J Sleep Res. 2012;21:441–7. doi: 10.1111/j.1365-2869.2011.00993.x. [DOI] [PubMed] [Google Scholar]
- 11.Sabanayagam C, Shankar A. Sleep duration and cardiovascular diseases: results from the National Health Interview Survey. Sleep. 2010;33:1037–42. doi: 10.1093/sleep/33.8.1037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yaggi HK, Araujo AB, McKinlay JB. Sleep duration as a risk factor for the development of type 2 diabetes. Diabetes Care. 2006;29:657–61. doi: 10.2337/diacare.29.03.06.dc05-0879. [DOI] [PubMed] [Google Scholar]
- 13.Magee L, Hale L. Longitudinal association between sleep duration and subsequent weight gain: a systematic review. Sleep Med Rev. 2012;16:231–41. doi: 10.1016/j.smrv.2011.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Altman NG, Izci-Balserak B, Schopfer E, et al. Sleep duration versus sleep insufficiency as predictors of cardiometabolic health outcomes. Sleep Med. 2012;13:1261–70. doi: 10.1016/j.sleep.2012.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Spiegel K, Leproult R, Cauter EV. Impact of sleep debt on metabolic and endocrine function. Lancet. 1999;354:1435–9. doi: 10.1016/S0140-6736(99)01376-8. [DOI] [PubMed] [Google Scholar]
- 16.Patel SR, Malhotra A, White DP, Gottlieb DJ, Hu FB. Association between reduced sleep and weight gain in women. Am J Epidemiol. 2006;164:846–50. doi: 10.1093/aje/kwj280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ayas NT, White DP, Al-Delaimy WK, et al. A prospective study of self-reported sleep duration and incident diabetes in women. Diabetes Care. 2003;26:380–4. doi: 10.2337/diacare.26.2.380. [DOI] [PubMed] [Google Scholar]
- 18.Buxton OM, Marcelli E. Short and long sleep are positively associated with obesity, diabetes, hypertension, and cardiovascular disease among adults in the United States. Soc Sci Med. 2010;71:1027–36. doi: 10.1016/j.socscimed.2010.05.041. [DOI] [PubMed] [Google Scholar]
- 19.Cappuccio FP, Cooper D, D'Elia L, Strazzullo P, Miller MA. Quantity and quality of sleep and incidence of type 2 diabetes. Diabetes Care. 2010;33:414–20. doi: 10.2337/dc09-1124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mezick EJ, Hall M, Matthews KA. Are sleep and depression independent or overlapping risk factors for cardiovascular disease? Sleep Med Rev. 2010;15:51–63. doi: 10.1016/j.smrv.2010.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mallon L, Broman JE, Hetta J. High incidence of diabetes in men with sleep complaints or short sleep duration: a 12-year follow-up study of a middle-aged population. Diabetes Care. 2005;28:2762–7. doi: 10.2337/diacare.28.11.2762. [DOI] [PubMed] [Google Scholar]
- 22.Engum A. The role of depression and anxiety in onset of diabetes in a large population-based study. Psychsom Res. 2007;62:31–8. doi: 10.1016/j.jpsychores.2006.07.009. [DOI] [PubMed] [Google Scholar]
- 23.Shen BJ, Avivi YE, Todaro JF, et al. Anxiety characteristics independently and prospectively predict myocardial infarction in men. J Am Coll Cardiol. 2008;51:113–9. doi: 10.1016/j.jacc.2007.09.033. [DOI] [PubMed] [Google Scholar]
- 24.Roest AM, Martens EJ, de jonge P, Denollet J. Anxiety and risk of incidence coronary heart disease: a meta-analysis. J Am Coll Cardiol. 2010;56:38–46. doi: 10.1016/j.jacc.2010.03.034. [DOI] [PubMed] [Google Scholar]
- 25.Strine TW, Chapman DP. Associations of frequent sleep insufficiency with health-related quality of life and health behaviors. Sleep Med. 2005;6:23–7. doi: 10.1016/j.sleep.2004.06.003. [DOI] [PubMed] [Google Scholar]
- 26.Centers for Disease Control and Prevention. Perceived insufficient rest or sleep among adults—United States, 2008. MMWR. 2009;58:1175–9. [PubMed] [Google Scholar]
- 27.Grandner MA, Patel NP, Gehrman PR, et al. Who gets the best sleep? Ethnic and socioeconomic factors related to sleep complaints. Sleep Med. 2010;11:470–8. doi: 10.1016/j.sleep.2009.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shankar A, Syamala S, Kalidindi S. Insufficient rest or sleep and its relation to cardiovascular disease, diabetes and obesity in a national multiethnic sample. PLoS One. 2010;5:e14189. doi: 10.1371/journal.pone.0014189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Centers for Disease Control and Prevention. Unhealthy sleep behaviors—12 states, 2009. MMWR. 2011;60:233–8. [PubMed] [Google Scholar]
- 30.Vishnu A, Shankar A, Kalidindi S. Examination of the association between insufficient sleep and cardiovascular disease and diabetes by race/ethnicity. Int J Endocrinol. 2011:789358. doi: 10.1155/2011/789358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wheaton AG, Perry GS, Chapman DP, McKnight-Eily LR, Presley-Cantrell LR, Croft JB. Relationship between body mass index and perceived insufficient sleep among U.S. adults: an analysis of 2008 BRFSS data. BMC Public Health. 2011;11:295. doi: 10.1186/1471-2458-11-295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sabanayagam C, Shankar A. The association between active smoking, smokeless tobacco, second-hand smoke exposure and insufficient sleep. Sleep Med. 2011;12:7–11. doi: 10.1016/j.sleep.2010.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chapman DP, Wheaton AG, Perry GS, Sturgis SL, Strine TW, Croft JB. Household demographics and perceived insufficient sleep among US adults. J Community Health. 2012;37:344–9. doi: 10.1007/s10900-011-9451-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Grandner MA, Martin JL, Patel NP, et al. Age and sleep disturbances among American men and women: data from the U.S. Behavioral Risk Factor Surveillance System. Sleep. 2012;35:395–406. doi: 10.5665/sleep.1704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Grandner MA, Hale L, Jackson N, Patel NP, Gooneratne NS, Troxel WM. Perceived racial discrimination as an independent predictor of sleep disturbance and daytime fatigue. Behav Sleep Med. 2012;10:235–49. doi: 10.1080/15402002.2012.654548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Grandner MA, Jackson NJ, Pigeon WR, Gooneratne NS, Patel NP. State and regional prevalence of sleep disturbance and daytime fatigue. J Clin Sleep Med. 2012;8:77–86. doi: 10.5664/jcsm.1668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Centers for Disease Control and Prevention. Drowsy driving—19 states and the District of Columbia, 2009-2010. MMWR. 2013;61:1033–7. [PubMed] [Google Scholar]
- 38.Chapman DP, Liu Y, Presley-Cantrell LR, et al. Adverse childhood experiences and frequent insufficient sleep in 5 U.S. states, 2009: a retrospective cohort. BMC Public Health. 2013;13:3. doi: 10.1186/1471-2458-13-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Liu Y, Croft JB, Wheaton AG, et al. Association between perceived insufficient sleep, frequent mental distress, obesity and chronic diseases among US adults, 2009 Behavioral Risk Factor Surveillance System. BMC Public Health. 2013;13:84. doi: 10.1186/1471-2458-13-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chapman DP, Croft JB, Liu Y, Perry GS, Presley-Cantrell LR, Ford ES. Excess frequent insufficient sleep in American Indians/Alaska Natives. J Environ Public Health. 2013:259645. doi: 10.1155/2013/259645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Centers for Disease Control and Prevention. BRFSS 2010 Summary Data Quality Report. Version # 1, revised 05/02/2011. ftp://ftp.cdc.gov/pub/Data/Brfss/2010_Summary_Data_Quality_Report.pdf.
- 42.Institute of Medicine. Washington, DC: National Academies Press; 2006. Sleep disorders and sleep deprivation: an unmet public health problem. [PubMed] [Google Scholar]
- 43.Moriarty DG, Zack MM, Holt JB, Chapman DP, Safran MA. Geographic patterns of frequent mental distress: U.S. adults, 1993-2001 and 2003-2006. Am J Prev Med. 2009;36:497–505. doi: 10.1016/j.amepre.2009.01.038. [DOI] [PubMed] [Google Scholar]
- 44.Strine TW, Chapman DP, Kobau R, Balluz L, Mokdad AH. Depression, anxiety, and physical impairments and quality of life in the U.S. noninstitutionalized population. Psychiatr Serv. 2004;55:1408–13. doi: 10.1176/appi.ps.55.12.1408. [DOI] [PubMed] [Google Scholar]
- 45.Washington DC: American Psychiatric Association; 2000. Diagnostic and statistical manual of mental disorders, fourth edition, text revision (DSM-IV-TR) [Google Scholar]
- 46.Bossarte RM, He H, Claassen CA, Knox K, Tu X. Development and validation of a 6-day standard for the identification of frequent mental distress. Soc Psychiatry Psychiatr Epidemiol. 2011;46:403–11. doi: 10.1007/s00127-010-0204-4. [DOI] [PubMed] [Google Scholar]
- 47.Mokdad AH, Serdula MK, Dietz WH, Bowman BA, Marks JS, Koplan JP. The spread of the obesity epidemic in the United States, 1991-1998. JAMA. 1999;282:1519–22. doi: 10.1001/jama.282.16.1519. [DOI] [PubMed] [Google Scholar]
- 48.Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999-2010. JAMA. 2012;307:491–7. doi: 10.1001/jama.2012.39. [DOI] [PubMed] [Google Scholar]
- 49.Rowland ML. Self-reported weight and height. Am J Clin Nutr. 1990;52:1125–33. doi: 10.1093/ajcn/52.6.1125. [DOI] [PubMed] [Google Scholar]
- 50.Palta M, Prineas RJ, Berman R, Hannan P. Comparison of self-reported and measured height and weight. Am J Epidemiol. 1982;115:223–30. doi: 10.1093/oxfordjournals.aje.a113294. [DOI] [PubMed] [Google Scholar]
- 51.Stommel M, Schoenborn CA. Accuracy and usefulness of BMI measures based on self-reported weight and height: findings from the NHANES & NHIS 2001-2006. BMC Public Health. 2009;9:421430. doi: 10.1186/1471-2458-9-421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Rothman KJ, Greenland S, Lash TL. Modern epidemiology. Philadelphia: Lippincott Williams & Wilkins; 2008. Measures of effect and measures of association. [Google Scholar]
- 53.Van de Mheen HD, Stronks K, Mackenbach JP. A life course perspective on socio-economic inequalities in health: the influence of childhood socio-economic conditions as selection process. Sociology Health Illness. 1998;20:754–77. [Google Scholar]
- 54.Baron RM, Kenny DA. The moderator-mediator distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51:1173–82. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 55.Jasti S, Dudley WN, Goldwater E. SAS macros for testing statistical mediation in data with binary mediators or outcomes. Nurs Res. 2008;57:118–22. doi: 10.1097/01.NNR.0000313479.55002.74. [DOI] [PubMed] [Google Scholar]
- 56.Research Triangle Institute. SUDAAN, Release 10.0. North Carolina: Research Triangle Park; 2008. [Google Scholar]
- 57.Cappuccio FP, Cooper D, D'Elia L, Strazzullo P, Miller MA. Sleep duration predicts cardiovascular outcomes: a systematic review and meta-analysis of prospective studies. Euro Heart. 2011;32:1484–92. doi: 10.1093/eurheartj/ehr007. [DOI] [PubMed] [Google Scholar]
- 58.Malhotra A, Loscalzo J. Sleep and cardiovascular disease: an overview. Prog Cardiovasc Dis. 2009;51:279–84. doi: 10.1016/j.pcad.2008.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Hamer M, Molloy GJ, Stamatakis E. Psychological distress as a risk factor for cardiovascular events: pathophysiological and behavioral mechanisms. J Am Coll Cardiol. 2008;52:2156–62. doi: 10.1016/j.jacc.2008.08.057. [DOI] [PubMed] [Google Scholar]
- 60.Patel SR, Malhotra A, Gotttlieb DJ, White DP, Hu FB. Correlates of long sleep duration. Sleep. 2006;29:881–9. doi: 10.1093/sleep/29.7.881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Irwin M, Mcclintick J, Costlow C, Fortner M, White J, Gillin JC. Partial night sleep deprivation reduces natural killer and cellular immune responses in humans. FASEB J. 1996;10:643–53. doi: 10.1096/fasebj.10.5.8621064. [DOI] [PubMed] [Google Scholar]
- 62.Dinges DF, Douglas SD, Zaugg L, et al. Leukocytosis and natural killer cell function parallel neurobehavioral fatigue induced by 64 hours of sleep deprivation. J Clin Invest. 1994;93:1930–9. doi: 10.1172/JCI117184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Irwin MR, Wang M, Campomayor CO, Collado-Hidalgo A, Cole S. Sleep deprivation and activation of morning levels of cellular and genomic markers of inflammation. Arch Intern Med. 2006;166:1756–62. doi: 10.1001/archinte.166.16.1756. [DOI] [PubMed] [Google Scholar]
- 64.Mullington JM, Simpson NS, Meier-Ewert HK, Haack M. Sleep loss and inflammation. Best Pract Res Clin Endocrinol Metab. 2010;24:775–84. doi: 10.1016/j.beem.2010.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Simpson N, Dinges DF. Sleep and inflammation. Nutrition Rev. 2007;65:S224–52. doi: 10.1111/j.1753-4887.2007.tb00371.x. [DOI] [PubMed] [Google Scholar]
- 66.Jackson C, Jatulis DE, Fortmann SP. The Behavioral Risk Factor Survey and the Stanford Five-City Project Survey: a comparison of cardiovascular risk behavior estimates. Am J Public Health. 1992;82:412–6. doi: 10.2105/ajph.82.3.412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Bowlin SJ, Morrill BD, Nafziger AN, Jenkins PL, Lewis C, Pearson TA. Validity of cardiovascular disease risk factors assessed by telephone survey: the Behavioral Risk Factor Survey. J Clin Epidemiol. 1993;46:561–71. doi: 10.1016/0895-4356(93)90129-o. [DOI] [PubMed] [Google Scholar]
- 68.Centers for Disease Control and Prevention. Effect of short sleep duration on daily activities—United States, 2005-2008. MMWR. 2011;60:239–42. [PubMed] [Google Scholar]
- 69.Fang J, Wheaton AG, Keenan NL, Greenlund KJ, Perry GS, Croft JB. Association of sleep duration and hypertension among US adults varies by age and sex. Am J Hypertens. 2012;25:335–41. doi: 10.1038/ajh.2011.201. [DOI] [PubMed] [Google Scholar]
- 70.Lauderdale DS, Knutson KL, Yan LL, Liu K, Rathouz PJ. Sleep duration: how well do self-reports reflect objective measures? The CARDIA Sleep Study. Epidemiology. 2008;19:838–45. doi: 10.1097/EDE.0b013e318187a7b0. [DOI] [PMC free article] [PubMed] [Google Scholar]


