Abstract
Study Objectives:
To investigate the associations of specific neighborhood features (disorder, safety, social cohesion, physical environment, and socioeconomic status) with sleep duration and quality.
Design:
Cross-sectional. One wave of a population-based study (Multi-Ethnic Study of Atherosclerosis).
Setting:
Community-dwelling participants in New York, NY and Los Angeles, CA.
Participants:
There were 1,406 participants (636 males, 770 females).
Interventions:
NA.
Measurements and Results:
Sleep was assessed using reported hours of sleep, the Epworth Sleepiness Scale, and insomnia symptoms. Neighborhood characteristics were assessed via questionnaires administered to neighbors of study participants and were aggregated to the neighborhood (census tract) level using empirical Bayes estimation. An adverse social environment (characterized by high disorder, and low safety and social cohesion) was associated with shorter sleep duration after adjustment for the physical environment, neighborhood and individual-level socioeconomic status (SES), and other short sleep risk factors (mean difference per standard deviation increase in summary social environment scale 0.24 h 95% confidence interval 0.08, 0.43). Adverse neighborhood social and physical environments, and neighborhood SES were associated with greater sleepiness, but associations with physical environments were no longer statistically significant after adjustment for sociodemographic characteristics. Neighborhood SES was a weaker and less consistent predictor of specific measures of neighborhood social and physical environments. Neighborhood characteristics were not associated with insomnia.
Conclusions:
Shortened sleep related to adverse social environments represents one potential pathway through which neighborhoods may influence health.
Citation:
DeSantis AS; Diez Roux AV; Moore K; Baron KG; Mujahid MS; Nieto FJ. Associations of neighborhood characteristics with sleep timing and quality: the multi-ethnic study of atherosclerosis. SLEEP 2013;36(10):1543-1551.
Keywords: Neighborhoods, sleep duration, daytime sleepiness
INTRODUCTION
A number of studies have linked neighborhood characteristics to cardiovascular risk factors and outcomes, including body mass index (BMI), diabetes, hypertension, and cardiovascular events.1–6 Important questions remain regarding whether these associations reflect causal processes, and if so, what the mediating mechanisms might be. In many studies, associations of neighborhood factors with cardiovascular-related outcomes persist after adjustment for standard risk factors,2,4–7 suggesting that other mediators could be involved.
Alterations of sleep have emerged as important risk factors for hypertension, diabetes, obesity, and cardiovascular events.8–11 Recently, sleep quality and quantity have been proposed as potential contributors to the links between neighborhood disadvantage and poorer health in general.11–14 Alterations of sleep could also be one of the mechanisms through which neighborhood contexts affect cardiovascular risk.
Several studies have analyzed the associations of physical environmental factors (e.g., noise and traffic) with sleep, finding that increased noise and traffic are associated with poorer sleep.15–18 A few studies have investigated associations between neighborhood social environments and sleep.12,13,16,19 Most of these studies have included only one measure of social environments. For example, one study focused on neighborhood disorder (as assessed by a combined index of self-reported perceptions of neighborhood crime, noise, and cleanliness)12 and another focused on neighborhood violence and perceptions of safety.16 A few studies have examined neighborhood socioeconomic status (SES) and sleep but most have focused on associations with sleep apnea in children, rather than normative sleep patterns and quality in adults.19,20
Although it has been hypothesized that neighborhood physical and social environments may contribute to neighborhood differences in cardiovascular disease (CVD) and other outcomes, few studies have investigated associations of multiple measures of neighborhood social and physical environments with sleep in large population studies. Using data from a multiethnic, population-based sample, we investigated associations of neighborhood social environments (disorder, safety, and social cohesion) and physical environments (noise and traffic) with total hours of sleep, daytime sleepiness, and insomnia. We hypothesized that higher levels of neighborhood disorder, lower levels of neighborhood social cohesion, safety, and SES and higher levels of noise/traffic would be associated with decreased sleep quantity and increased daytime sleepiness and insomnia symptoms after adjustment for confounders. Neighborhood disorder, safety, and cohesion are hypothesized to influence sleep as a result of increased psychological stress,12 which could lead to states of vigilance or increased arousal, making it difficult to sleep. Physical environmental factors (e.g., noise and street traffic) may influence sleep, sleep disturbances, and, consequently, daytime sleepiness, more directly by disrupting one's ability to sleep due to disturbances in the immediate proximity.15,17,18
METHODS
The data utilized in these analyses come from the Multi-Ethnic Study of Atherosclerosis (MESA), a longitudinal study of adults between 45 and 84 years old from six US cities. The study was designed to prospectively examine risk factors for subclinical cardiovascular disease and its progression to clinical disease. All participants were free of clinical cardiovascular disease at baseline. Various population-based approaches (e.g., sampling from lists of area residents, Medicare and Medicaid Services lists, and random digit dialing) were utilized to recruit participants. Twenty-two participants with a history of clinical cardiovascular disease at baseline (2000-2002) were excluded from participation. After the baseline examination, three follow-up examinations were conducted at intervals of 1.5-2 years. The current analyses utilize data on neighborhood characteristics from an ancillary study conducted in two of the sites, New York and Los Angeles.
Sleep Measures
A sleep questionnaire was included as part of the 2005-2007 follow-up (MESA Exam 4). We examined three separate indicators of sleep quality and duration: average sleep duration in hours, daytime sleepiness, and insomnia symptoms. Sleep duration in hours was assessed using a single question: “How much sleep do you usually get at night (or your main sleep period) on weekdays or workdays?” (This was an open-ended question, without precoded categories, and respondents were requested to respond in hours). Daytime sleepiness was assessed using the eight-item Epworth Sleepiness Scale (ESS).21 The scale asks respondents, “How likely are you to doze off or fall asleep in the following situations, in contrast to feeling just tired?” Situations include activities such as: watching television, sitting and talking to someone, as a passenger in a car for 1 h without a break; in a car, while stopped for a few min in traffic, etc. Responses include: 0 = no chance of dozing; 1 = slight chance of dozing; 2 = moderate chance of dozing; 3 = high chance of dozing. Scores may range from 0 to 24.
Level of insomnia symptoms was determined based on questionnaire responses or diagnosis of insomnia by a physician. To assess insomnia symptoms, participants reported on the frequency of sleep disturbances and interruptions (e.g., trouble falling asleep; waking up during the night and having difficulty getting back to sleep; waking up too early in the morning and unable to get back to sleep) over the past mo. Responses ranged from one (never) to five (frequently, i.e., five or more nights/week). Response options included never, rarely (once or twice/month), sometimes (two to four times/month), often (five to 15 times/month), and almost always (16 to 30 times/ month). Those who reported frequently experiencing at least one of these sleep disturbances 5 or more nights/week, as well as those who reported a physician diagnosis of insomnia, were considered to have insomnia.
Neighborhood Measures
Neighborhood characteristics were assessed as part of the MESA Neighborhood Study, an ancillary study to MESA. Between 2006 and 2008, the MESA Neighborhood Study conducted a Community Survey (CS II) at two of the six MESA sites (New York and Los Angeles) to assess various features of neighborhoods, with census tracts used to proxy neighborhoods. The CS II collected information from residents of MESA neighborhoods, who themselves were not MESA participants, using random digit dialing and listed household sampling frames to target areas where MESA participants reside. In total, there were 5,178 respondents in 628 census tracts in New York and Los Angeles. The timing of data collection for CS II (2006-2008) largely overlaps with the timing of the Sleep History questionnaires in Exam 4 (2005-2007). The fact that reports of neighborhood characteristics were collected from residents of census tracts in which MESA study participants resided, rather than from MESA participants themselves, allowed us to improve the precision of estimates of neighborhood characteristics by increasing the number of informants per neighborhood, and by avoiding same-source bias that could arise if a common factor relates to both adverse reports of neighborhood environments and sleep, or if poor sleep causes participants to report more adverse neighborhood environments.
Four individual neighborhood domains were investigated: neighborhood disorder (12 items),22 safety (three items),23 social cohesion (four items),24 and physical environment (two items). Each score was transformed into standard deviation (SD) units to facilitate comparisons. We also combined the standardized scores for safety, disorder, and social cohesion to create a summary index representing all neighborhood social factors. Neighborhood disorder was reverse-coded before averaging such that higher scores for the summary index indicate better neighborhood quality (i.e., lower disorder).
Census tract measures for each neighborhood domain were estimated using empirical Bayes estimates conditioned on respondent's age and sex and study site to calculate levels of each characteristic within the census tracts in which MESA study participants resided.25 Empirical Bayes estimates take into account the nested nature of the data (item responses within individuals within neighborhoods) and use all available data from across neighborhoods to improve estimates. Detailed information on the psychometric and ecometric properties of neighborhood scales, as well as the procedures for calculating empirical Bayes estimates, are available elsewhere.25 There was an average of 6.9 MESA study participants (median = 5; inter-quartile [IQ] range 3 to 8) and 14.9 CS II respondents (median = 18; IQ range 3 to 22) per census tract.
In addition to the measures of social and physical environments, for comparison purposes, we also investigated a summary measure of neighborhood SES as a proxy for a range of environmental influences. Neighborhood SES was characterized based on a factor score derived from principal components analysis of US census tract-level data.7 The factor score includes data on median household income, percentage of homes with interest and dividends, median value of owner-occupied housing, percentage of residents with at least a high school diploma, percentage of residents with at least a BA degree, and percentage of residents employed in managerial professions. It was also transformed into SD units.
Sociodemographic Factors
Participants self-identified their race/ethnicity as non-Hispanic white, non-Hispanic Black/African-American, Chinese, and Hispanic/Latino. SES was assessed using educational attainment and an income-wealth index. Education was based on a nine-point scale ranging from 0 to 8 (no schooling; less than 8th grade; less than high school, high school/GED diploma; some college, completed vocational/technical degree; associates degree; bachelors degree; and graduate or professional school). Participants were grouped into three educational categories (less than high school, high school, or at least some college) for analysis. Wealth was determined based on reported assets from the following list: owning one or more cars, owning or paying a mortgage on a home, owning land, or owning investments (e.g., stocks or bonds). Participants received one point for ownership of each of these assets, resulting in a five-point wealth index (range = 0 to 4). Income (originally reported on a 13-category scale), was divided into quintiles, and coded from 0 to 4 before being summed with the assets variable to create an income-wealth index.26
Covariates
Analyses were also adjusted for medical risk factors for sleep disturbances (diabetes, hypertension, BMI, and depression), which may confound and/or mediate the neighborhood-sleep associations. Participants with a fasting glucose ≥ 126 mg/dL or taking insulin or oral diabetes medication were considered diabetic. Participants with elevated systolic or diastolic blood pressure (≥ 130/85 mmHg or antihypertensive treatment) were classified as hypertensive. BMI was calculated based on weight and height measured at the MESA examination. Depressive symptomology was based on scores on the Center for Epidemiologic Studies of Depression (CES-D).27
Exclusion Criteria
Participants were required to provide valid data for their sleep questionnaires for at least one of the sleep outcomes examined and to have at least one CS II participant residing in their census tract. There were 1,999 participants in the MESA study in the New York and Los Angeles sites at Exam 4, and 1,463 of these participants resided in census tracts with CS II respondents. Of these 1,463 participants, 41 failed to provide complete data for the sleep variables and covariates, resulting in a final analytic sample of 1,412. The final analytical sample did not differ significantly from the full MESA sample at the New York and Los Angeles sites, with respect to sociodemographic composition, cardiovascular risk factors, or sleep duration or quality.
Analyses
We first examined the distribution of selected individual and neighborhood characteristics across categories of sleep outcomes. Descriptive statistics for hours of sleep and daytime sleepiness were investigated in tertiles, and insomnia was investigated as present/absent. Analysis of variance and chi-square tests were used to compare continuous and categorical covariates, respectively, across categories of sleep outcomes for the continuous sleep outcomes. Differences between persons with and without insomnia were investigated using t-tests for the continuous covariates and chi-square tests for the categorical variables.
We next analyzed whether there were differences in mean sleep duration, mean daytime sleepiness score, and prevalence of insomnia symptoms across neighborhood characteristics, after adjustment for age and sex. In order to determine whether there was an approximate dose-response trend, neighborhood characteristics were categorized into tertiles for these analyses. The models used to estimate age- and sex-adjusted means for hours of sleep and daytime sleepiness accounted for within-census tract clustering using a random intercept for each tract.28 Models for insomnia used Generalized Estimating Equations29 to account for clustering by census tract.
Finally, we estimated mean differences in hours of sleep and in daytime sleepiness score as well as odds ratios of insomnia associated with a standard deviation increase in neighborhood characteristics before and after adjustment for sets of covariates. Neighborhood characteristics were included as continuous variables because descriptive analyses did not provide strong evidence of a threshold effect. Variables were transformed into SD units to allow comparison across the different measures. Each neighborhood characteristic was investigated separately in multilevel models that accounted for within neighborhood clustering using a random intercept for each cluster.
For each sleep outcome and each neighborhood predictor (including the summary social environment score) we fit a series of sequential models: model 1 adjusted for age and sex, model 2 adjusted for social and demographic factors including race/ethnicity, education, income-wealth, and model 3 adjusted for other factors that may serve as potential confounds (or alternatively mediators) of the neighborhood-sleep associations (e.g., depressive symptoms, BMI, diabetes, hypertension).
In order to investigate the independent effects of the social environment, the physical environment, and neighborhood SES, we fit the same sequence of models including the three factors (social environment summary score, the physical environment, and neighborhood SES) simultaneously in the same model.
Finally, we examined whether associations of neighborhood characteristics with sleep were modified by sex, SES, age, or site. Each of these characteristics was interacted with neighborhood characteristics in separate models. To do this, we included interaction terms between each neighborhood characteristic (e.g., disorder) and each of the following socio-demographic characteristics, with the interactions entered into models one at a time: sex, race, age, site, and SES, controlling for all the others. All analyses were conducted using SAS software (SAS Institute, Cary, NC).
RESULTS
Table 1 shows the distribution of selected demographic, socioeconomic, and neighborhood characteristics across categories of sleep outcomes. Mean hours of sleep ranged from 5.46 h in the lowest tertile to 8.32 h in the highest tertile. Persons reporting more hours of sleep had lower daytime sleepiness scores and lower prevalence of insomnia. Persons reporting the most hours of sleep tended to be older and were more likely to be white than those reporting the least hours of sleep. Those in the middle tertile of sleep duration were more likely to have at least some college education and also had lower BMIs and lower levels of depressive symptoms than those in the highest and lowest tertiles. Persons in the middle tertile of sleep duration had the most favorable neighborhood scores (i.e., lower scores of disorder and higher scores of safety, social cohesion, overall social environment quality, and SES).
Table 1.
Distribution of selected demographic, socioeconomic, and neighborhood characteristics across categories of sleep outcomes (N = 1,406)
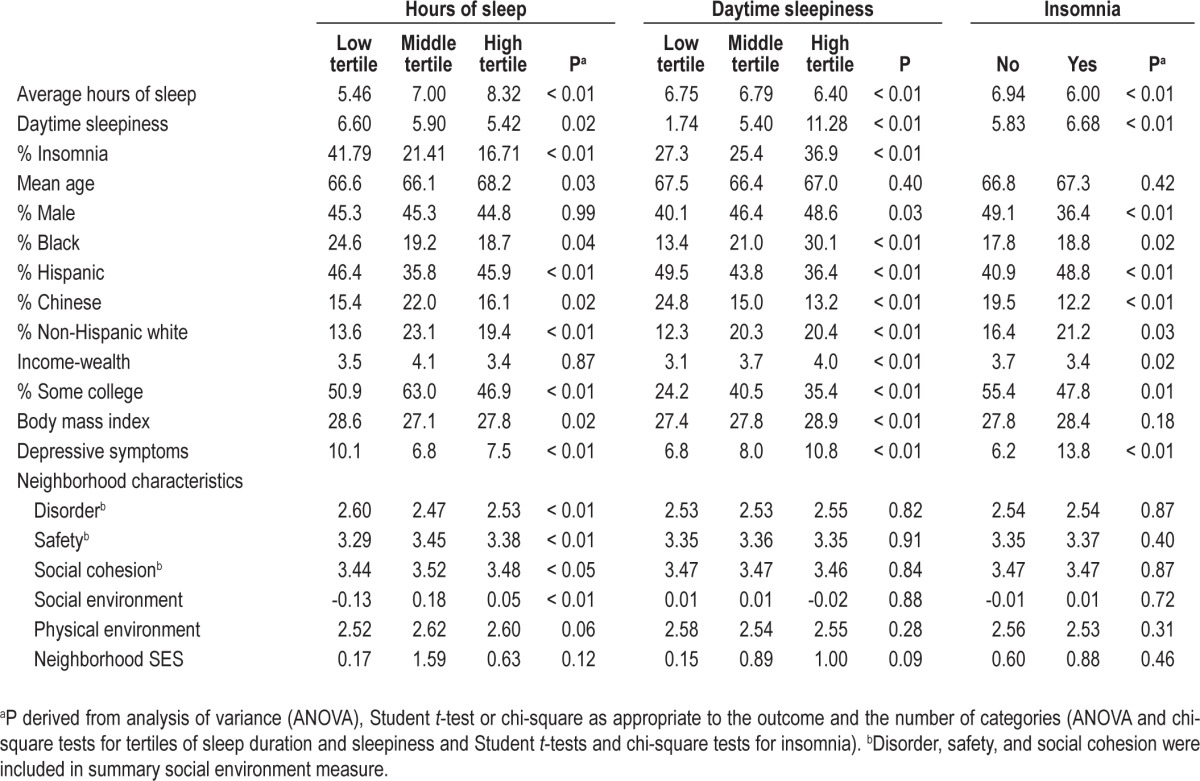
Daytime sleepiness scores ranged from 1.74 in the lowest tertile to 11.28 in the highest tertile. Higher levels of daytime sleepiness were associated with higher levels of insomnia, male sex, and white race/ethnicity. Persons reporting more sleepiness tended to have higher incomes, more education, higher BMI, and higher levels of depressive symptoms than those reporting less sleepiness. More daytime sleepiness was also associated with poorer physical environments.
Overall, 29% of the sample had insomnia. Having insomnia was significantly associated with female sex and with Hispanic or white race/ethnicity. Those with insomnia had higher levels of depressive symptoms and lower levels of education and income-wealth. Insomnia was not associated with neighborhood characteristics.
Table 2 shows mean hours of sleep, mean daytime sleepiness score, and the prevalence of insomnia across tertiles of neighborhood characteristics after adjustment for age and sex. For each of the neighborhood characteristics, higher scores reflect better neighborhood quality, with the exception of disorder, in which case higher scores indicate greater disorder. Correlations between neighborhood factors ranged from a low of r = 0.41 for safety and physical environment to a high of r = -0.92 for safety and disorder.
Table 2.
Age- and sex-adjusted sleep outcomes by levels of neighborhood characteristics (N = 1,406)
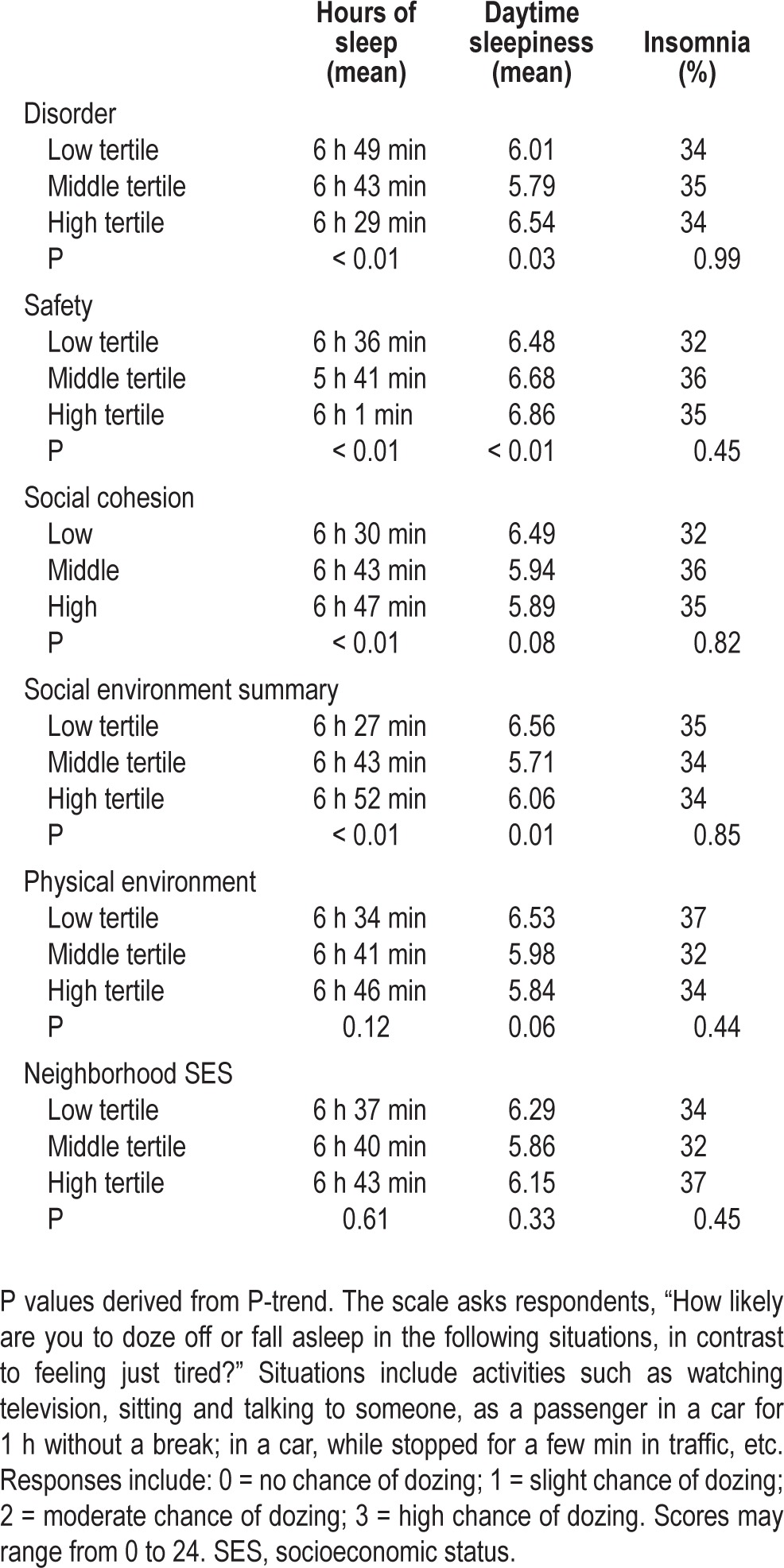
In general, improving neighborhood quality (lower disorder, higher safety, higher social cohesion, and better physical environment) was associated with longer sleep duration in a linear fashion (except associations with safety which were not clearly linear across the tertiles). Associations of neighborhoods with daytime sleepiness were not as consistent: greater neighborhood safety was associated with greater sleepiness, and higher cohesion was associated with less sleepiness. A better physical environment was associated with less sleepiness. Other associations did not show a clear linear pattern. There were no significant associations of neighborhood characteristics with presence of insomnia.
Table 3 shows mean differences in hours of sleep and daytime sleepiness scores associated with neighborhood characteristics before and after adjusting for covariates. Better neighborhood environments were associated with longer sleep duration. In general, associations with the social environment were stronger than associations with the physical environment or SES. Associations with disorder, safety, and the summary social environment score were slightly reduced but remained statistically significant after adjustment for race/ethnicity and socioeconomic position (mean differences: -0.10 h [95% confidence interval (CI): -0.20, -0.00], 0.11 h [95% CI: 0.02, 0.20] and 0.10 h [95% CI: 0.01, 0.20] for SD increases in neighborhood disorder, safety, and the social environment summary score, respectively). Further adjustment for medical risk factors for sleep (hypertension, BMI, diabetes, and depressive symptoms) did not substantially modify these associations.
Table 3.
Adjusted mean differences in hours of sleep and daytime sleepiness associated with a 1-standard deviation increase in neighborhood characteristics (N = 1,406)
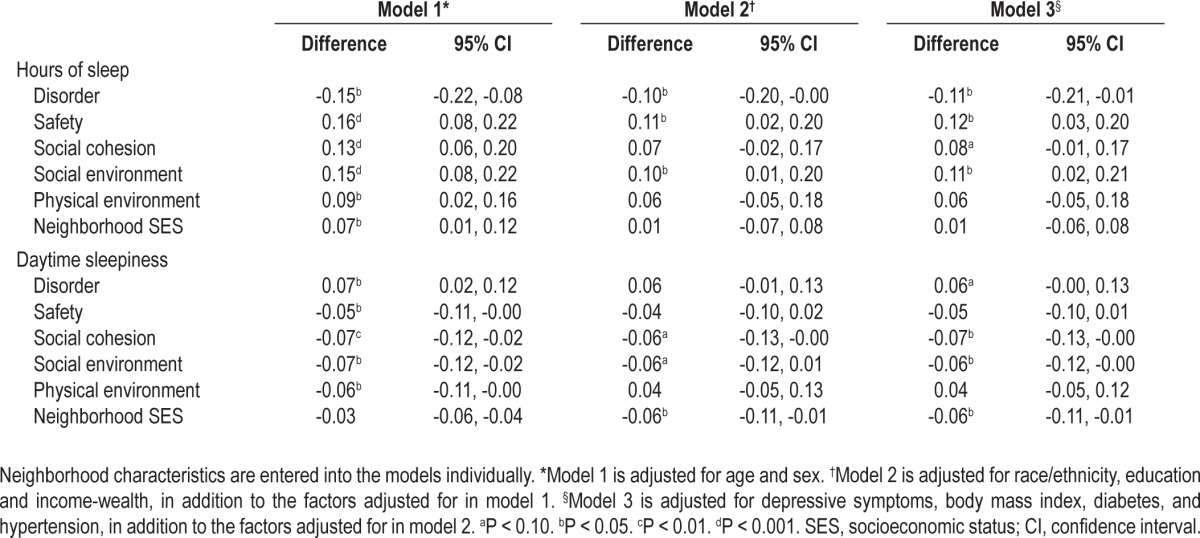
Daytime Sleepiness
Each of the neighborhood characteristics, with the exception of neighborhood SES, was also associated with daytime sleepiness in models controlling for age and sex (Table 3). The magnitude of the associations was generally similar across social and physical environment measures (mean differences = 0.07 [95% CI: 0.02, 0.12], -0.05 [95% CI: -0.11, 0.0], -0.07 [95% CI: -0.12, 0.00] and -0.06 [95% CI: -0.11, 0.0]) for disorder, safety, social cohesion, and physical environment, respectively. Although point estimates were not substantially altered, CIs became wider and associations were no longer statistically significant after adjustment for socio-demographic factors. The association of higher neighborhood SES with less daytime sleepiness became statistically significant after adjustment for individual-level sociodemographic characteristics (mean difference = -0.06 [95% CI: -0.11, -0.01]). Associations of neighborhood characteristics with daytime sleepiness were virtually identical after controlling for CVD risk factors (hyper-tension, BMI, diabetes, and depressive symptoms).
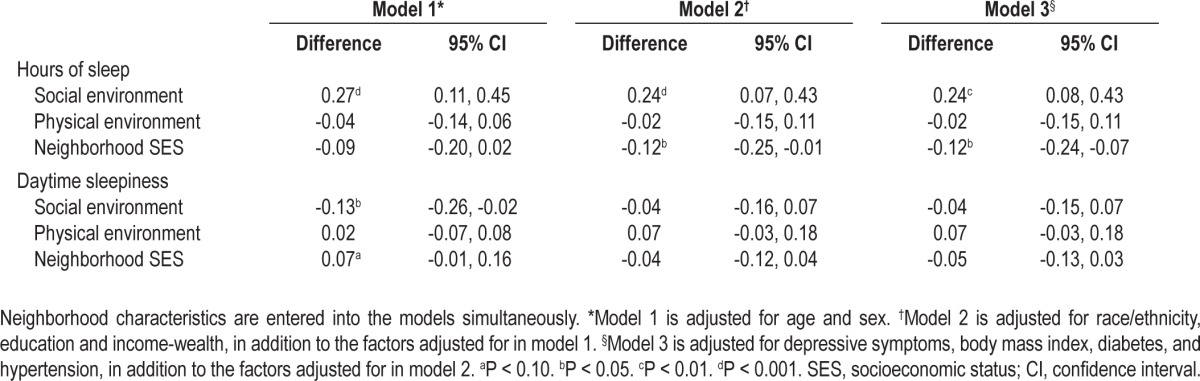
When social environment summary scores, physical environment scores, and neighborhood SES were analyzed simultaneously in relation to sleep duration, each SD increase in neighborhood social environment summary score was associated with 0.24 h (95% CI: 0.10, 0.37) more sleep, but physical environment and neighborhood SES were not associated with sleep duration (Table 4). These associations changed little after additional adjustment for individual-level sociodemographic characteristics except that the association of higher neighborhood SES with shorter duration became slightly stronger and statistically significant. All associations remained virtually identical after adjustment for individual CVD risk factors (Table 4, last column). When the three neighborhood indicators were examined simultaneously in relation to daytime sleepiness, only a better social environment was associated with less sleepiness (mean difference in daytime sleepiness per SD increase in social environment summary score -0.13 SD [95% CI: -0.26, -0.02]). This association was weakened and was no longer statistically significant after adjustment for sociodemographic factors.
Table 4.
Adjusted mean differences in hours of sleep and daytime sleepiness associated with a 1-standard deviation increase in neighborhood characteristics (N = 1,406)
We found no evidence of effect modification of associations of neighborhood factors with sleep duration or daytime sleepiness according to sex, SES, and age (not shown). Of the 15 interactions tested (five neighborhood factors interacted with three demographic characteristics), none were significant. Interactions by age, sex, and race were also tested in the model with summary measures, and were not significant. Results were generally robust to separate adjustment for income and wealth.
Tests of effect modification according to site revealed no statistically significant differences in associations of neighborhood characteristics with sleep duration. However, in age, sex-, race- and SES-adjusted models associations of a more adverse neighborhood social environment with greater daytime sleepiness appeared to be present in New York but not Los Angeles (mean difference per SD unit increase -0.12 in NY and 0.03 in LA, [P-value for interaction < 0.01]). A similar pattern was observed for neighborhood SES.
Insomnia was not associated with any of the neighborhood factors before or after adjustment for race/ethnicity, SES, or CVD risk factors (not shown).
DISCUSSION
Both neighborhood social and physical environments were associated with self-reported sleep duration and daytime sleepiness after adjustment for age and sex. An adverse social environment (characterized by high disorder and low safety and social cohesion) remained associated with shorter sleep duration after adjustment for the physical environment, neighborhood SES, and individual level sociodemographic characteristics and other short sleep risk factors. Associations of neighborhood social and physical environments with sleepiness were no longer statistically significant after adjustment for sociodemographic characteristics. Neighborhood SES was a weaker and less consistent predictor than the more specific measures of neighborhood social and physical environments. We observed no associations of neighborhood characteristics with insomnia.
To date, much of the literature on associations of neighborhood characteristics with sleep has focused on either the physical environment (i.e., noise and traffic) or a single measure of the social environment, rather than examining multiple indicators social and physical environments within a single study. For example, social factors such as neighborhood disorder and exposure to neighborhood violence have been linked to poorer sleep quality in a small number of studies.12,16 One study found that sleep quality both partially mediated and amplified associations of neighborhood disorder with psychological distress.12 Another study found that personal exposure to neighborhood violence, but not perceptions of neighborhood safety, was associated with increased sleep disturbances.16 In the current study, we investigated a more comprehensive set of social environment measures as well as the extent to which the social environment was associated with sleep independently of the physical environment and neighborhood SES. We found that an adverse social environment was associated with shorter sleep duration after adjustment for the physical environment, neighborhood SES, sociodemographic factors, and other risk factors for short sleep.
A few studies have investigated associations of the physical environment with sleep. Noise levels in decibels measured empirically using sound level meters have been associated with increased levels of daytime sleepiness17 and sleep disturbances,15,18 although these studies generally did not control for social environment features. Noise exposure in laboratory settings has been found to increase levels of arousal and sleep disturbances30 as well as increase activation of the body's stress systems, as assessed by levels of catecholamines and glucocorticoids,31 leading to speculation that noise exposure at night in naturalistic settings may lead to activation of the body's stress systems, thereby increasing risk of CVD.15 We found that an adverse physical environment was associated with shorter sleep duration and more sleepiness in age- and sex-adjusted models but these associations were no longer statistically significant after adjustment for sociodemographic factors. Limitations of our measure of the physical environment, which was based solely on self-reports of noise and traffic, may have affected our ability to estimate the effect of the physical environment.
There are a number of pathways through which neighborhood factors may influence sleep. The neighborhood social environment likely indirectly influences sleep via arousal of the body's stress systems, as stressful environments may lead to a heightened state of vigilance, thereby making it more difficult for residents to “shut down” their physiologic stress response systems at night.15 In contrast, physical environmental factors may influence sleep directly, as a result of noise disturbances, as well as indirectly, by activating the sympathetic nervous system and potentially exacerbating levels of physiologic stress system activity.15 These findings are consistent with research indicating that persons in urban areas also tend to sleep fewer hours.32 We found stronger and more consistent associations of sleep with neighborhood social environments than with neighborhood physical environments. Physical environment measures were limited and differential validity of our measures in both domains could have influenced these results.
We investigated neighborhood SES as an alternative indicator of neighborhood environmental features potentially related to sleep. The few studies that have investigated associations of neighborhood SES have largely focused on associations with sleep apnea in children. Two studies identified associations of neighborhood disadvantage and pediatric sleep apnea in 8- to 11-year-olds the United States.19 and 2- to 8-year-olds in Canada.20 An important limitation of neighborhood SES measures is the fact that the measure is only an imperfect proxy for the more specific environmental features that may be relevant. In addition, it may be difficult to analytically separate the effect of neighborhood SES from that of individual level SES factors. Consistent with the hypothesis that neighborhood social and environmental features are more directly related to sleep, our study showed that associations of neighborhood SES with sleep duration were less consistent than those observed with other neighborhood measures.
Of the three sleep-related outcomes we investigated, sleep duration was the one most strongly and consistently associated with neighborhood characteristics. Daytime sleepiness showed weaker associations that were no longer statistically significant after adjusting for socio-demographic characteristics. Insomnia was not related to neighborhood factors. It is plausible that the etiology and hence causes of these three outcomes differ. Variable measurement validity across the three outcomes for self-reported items could also have influenced our results.
The clinical implications of reduced sleep and daytime sleepiness are not negligible. Reduced sleep has been related to a number of adverse physical health outcomes, including development of diabetes and impaired glucose regulation, hypertension, hypercholesterolemia, higher BMI, and reduced immunocompetence, as well as increases in depressed mood and daytime sleepiness.33,34 Daytime sleepiness has been related to impaired cognitive functioning, and increased likelihood of experiencing various types of accidents, including occupational and automobile accidents.35 Although the magnitude of the associations we report is small, they could have important implications. A meta-analysis of 36 population samples found that each additional hour of sleep was associated with a 0.35 unit lower BMI in adults.36 In addition to associations with health, as little as 20 min of additional sleep in adolescents has been linked to improved academic performance (substantially higher grades),37 and a 45-min increase in sleep among adolescents has predicted reductions in sleepiness, fatigue, and depressed mood.38 Measurement error in both neighborhood characteristics and sleep outcomes could have led to an underestimation of the associations of neighborhood characteristics with sleep. In addition, even small associations may have an effect on shifting the distribution of sleep at the population level and contributing to differences in sleep across various social groups.
One important limitation to this study is the use of self-reported measures of sleep duration. Prior research indicates that people tend to underreport their sleep duration, and that this differs by demographic and medical risk factors.39 Specifically, one study found that although the sample as a whole tended to underreport sleep, results for blacks, overweight individuals, and those with hypertension were more accurate than those of whites, individuals of normal weight, and normotensive persons, respectively. Although we include controls for these factors, systematic biases in self-reported sleep by these factors could result in incomplete adjustment for these potential confounders. In addition, participants reported only on estimates of sleep on weekdays and workdays, but not weekends and nonwork days, and variability across days, and drastically reduced weekend sleep or dependence on “catch-up” sleep on weekends may also be related to neighborhood characteristics and health. A second limitation is that we did not include objective measures of noise or traffic, as has been done in some prior studies.15 Objective measures of noise and traffic in the immediate vicinity of a participant's home would likely provide a more accurate estimate of the association of these factors with sleep. Regardless, it is conceivable that certain persons are more sensitive to noise disturbances than others and/or that individuals exposed to noise regularly may adapt to disturbances over time. Thus, self-reported noise perceptions may be a more relevant method of assessing how naturally occurring noise around the home may influence sleep. In addition, we did not specifically question participants regarding the reasons for decreased sleep hours, and it is possible that other household factors, as well as work schedules, could confound the associations of neighborhood factors with sleep.3 In order to minimize heterogeneity, the questionnaire focused on sleep during the week. Thus, we were unable to examine the associations of neighborhood factors with sleep during weekends.
An additional limitation is that cross-sectional data prevent us from ruling out systematic self-selection into neighborhoods by participants with different sleep habits and quality. Because persons of lower SES may reside in neighborhoods of poorer quality and experience decreased sleep duration and poorer sleep quality, individual SES represents a key potential confounding variable. However, individual SES was not strongly associated with sleep outcomes in this study and associations were generally robust to SES adjustment. We included several CVD risk factors (BMI, hypertension, etc.) as covariates in our final models. These conditions may be the result of neighborhood exposures and could thus mediate rather than confound the links between neighborhood and sleep. However, our results were generally robust to adjustment for these risks factors.
It is plausible that individual-level factors modify the effect of neighborhood environments on sleep. We found no evidence of effect modification by age, sex, SES, or race/ethnicity but power to investigate interactions was limited. We found no evidence that indicated modification of the association of neighborhoods with sleep duration. In the case of sleepiness, there was some evidence that associations were stronger in New York than Los Angeles; however, limited power precludes us from drawing firm conclusions regarding the modifying effect of site.
A strength of our study is that the use of reports of neighborhood characteristics from persons other than those reporting on their sleep habits thus eliminating the possibility of same-source bias. Moreover, the dense sampling design of CS II informants, in combination with the use of empirical Bayes estimates of neighborhood characteristics, likely increased the validity of measures of neighborhood characteristics. In addition, the MESA study includes an ethnically and socioeconomically diverse population, and the neighborhoods in the CS II have substantial variation in each of the neighborhood characteristics analyzed.
Additional research is necessary to clarify the nature of any potentially causal pathways linking neighborhood characteristics, sleep, and health outcomes, but these results are consistent with the possibility that neighborhood factors may contribute to differences in sleep duration. Given the growing body of evidence linking sleep duration and quality to health, sleep represents one potential pathway through which neighborhoods may influence a multiplicity of health outcomes.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
This study was conducted with the approval of and in compliance with the ethical guidelines of the University of Michigan and in accordance with the regulations of the Health Insurance Portability and Accountability Act (HIPAA) of 1996.
REFERENCES
- 1.Diez Roux AV, Mair C. Neighborhoods and health. Ann NYAS. 2010;1186:125–45. doi: 10.1111/j.1749-6632.2009.05333.x. [DOI] [PubMed] [Google Scholar]
- 2.Fish JS, Ettner S, Ang A, Brown AF. Association of perceived neighborhood safety on body mass index. Am J Public Health. 2010;100:2296–303. doi: 10.2105/AJPH.2009.183293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Adam EK, Snell EK, Pendry P. Sleep timing and quantity in ecological and family context: a nationally representative time-diary study. J Fam Psychol. 2007;21:4–19. doi: 10.1037/0893-3200.21.1.4. [DOI] [PubMed] [Google Scholar]
- 4.Burdette HL, Wadden TA, Whitaker RC. Neighborhood safety, collective efficacy, and obesity in women with young children. Obesity. 2006;14:518–25. doi: 10.1038/oby.2006.67. [DOI] [PubMed] [Google Scholar]
- 5.Augustin T, Glass TA, James BD, Schwartz BS. Neighborhood psychosocial hazards and cardiovascular disease: the Baltimore Memory Study. Am J Public Health. 2008;98:1664–70. doi: 10.2105/AJPH.2007.125138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gallicchio L, Kalesan B. Sleep duration and mortality: a systematic review and meta-analysis. J Sleep Res. 2009;18:148–58. doi: 10.1111/j.1365-2869.2008.00732.x. [DOI] [PubMed] [Google Scholar]
- 7.Diez Roux AV, Merkin SS, Arnett D, et al. Neighborhood of residence and incidence of coronary heart disease. NEJM. 2001;345:99–106. doi: 10.1056/NEJM200107123450205. [DOI] [PubMed] [Google Scholar]
- 8.Chaput JP, Després JP, Bouchard C, Tremblay A. The association between sleep duration and weight gain in adults: a 6-year prospective study from the Quebec Family Study. Sleep. 2008;31:517–23. doi: 10.1093/sleep/31.4.517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gangwisch JE, Heymsfield SB, Boden-Albala B, et al. Short sleep duration as a risk factor for hypertension: analyses of the first National Health and Nutrition Examination Survey. Hypertension. 2006;47:833–9. doi: 10.1161/01.HYP.0000217362.34748.e0. [DOI] [PubMed] [Google Scholar]
- 10.Snell EK, Adam EK, Duncan GJ. Sleep and the body mass index and overweight status of children and adolescents. Child Dev. 2007;78:309–23. doi: 10.1111/j.1467-8624.2007.00999.x. [DOI] [PubMed] [Google Scholar]
- 11.Taheri S. The link between short sleep duration and obesity: we should recommend more sleep to prevent obesity. Arch Dis Child. 2006;91:881–4. doi: 10.1136/adc.2005.093013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hale L, Hill TD, Burdette AM. Does sleep quality mediate the association between neighborhood disorder and self-rated physical health? Prev Med. 2010;51:275–8. doi: 10.1016/j.ypmed.2010.06.017. [DOI] [PubMed] [Google Scholar]
- 13.Hill TD, Burdette AM, Hale L. Neighborhood disorder, sleep quality, and psychological distress: testing a model of structural amplification. Health Place. 2009;15:1006–13. doi: 10.1016/j.healthplace.2009.04.001. [DOI] [PubMed] [Google Scholar]
- 14.Marcus CL. The toll of poverty: no respite even in sleep. J Pediatr. 2006;149:293–4. doi: 10.1016/j.jpeds.2006.07.017. [DOI] [PubMed] [Google Scholar]
- 15.Pirrera S, De Valck E, Cluydts R. Nocturnal road traffic noise: a review on its assessment and consequences on sleep. Environ Int. 2010;36:492–8. doi: 10.1016/j.envint.2010.03.007. [DOI] [PubMed] [Google Scholar]
- 16.Johnson SL, Solomon BS, Shields WC, McDonald EM, McKenzie LB, Gielen AC. Neighborhood violence and its association with mothers' health: assessing the relative importance of perceived safety and exposure to violence. J Urban Health. 2009;86:538–50. doi: 10.1007/s11524-009-9345-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.deKluizenaar Y, Janssen SA, van Lenthe FJ, Miedema HM, Mackenbach JP. Long-term road traffic noise exposure is associated with an increase in morning tiredness. J Acoust Soc Am. 2009;126:626–33. doi: 10.1121/1.3158834. [DOI] [PubMed] [Google Scholar]
- 18.Muzet A. Environmental noise, sleep and health. Sleep Med Rev. 2007;11:135–42. doi: 10.1016/j.smrv.2006.09.001. [DOI] [PubMed] [Google Scholar]
- 19.Spilsbury JC, Storfer-Isser A, Kirchner HL, et al. Neighborhood disadvantage as a risk factor for pediatric obstructive sleep apnea. J Pediatr. 2006;149:342–7. doi: 10.1016/j.jpeds.2006.04.061. [DOI] [PubMed] [Google Scholar]
- 20.Brouillette RT, Horwood L, Constantin E, Brown K, Ross NA. Childhood sleep apnea and neighborhood disadvantage. J Pediatr. 2011;158:789–95. doi: 10.1016/j.jpeds.2010.10.036. [DOI] [PubMed] [Google Scholar]
- 21.Johns MW. A new method for measuring daytime sleepiness: The Epworth Sleepiness Scale. Sleep. 1991;14:540–5. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 22.Ross CE, Mirowsky J. Neighborhood disadvantage, disorder, and health. J Health Soc Behav. 2001;42:258–76. [PubMed] [Google Scholar]
- 23.Mujahid MS, Diez Roux AV, Morenoff JD, Raghunathan T. Assessing the measurement properties of neighborhood scales: from psychometrics to ecometrics. Am J Epidemiol. 2007;165:858–67. doi: 10.1093/aje/kwm040. [DOI] [PubMed] [Google Scholar]
- 24.Sampson RJ, Raudenbush SW, Earls FE. Neighborhoods and violent crime: a multilevel study of collective efficacy. Science. 1997;277:918–24. doi: 10.1126/science.277.5328.918. [DOI] [PubMed] [Google Scholar]
- 25.Mujahid MS, Diez Roux AV, Morenoff J, et al. Neighborhood characteristics and hypertension. Epidemiology. 2008;19:590–8. doi: 10.1097/EDE.0b013e3181772cb2. [DOI] [PubMed] [Google Scholar]
- 26.Hajat A, Diez Roux AV, Franklin TG, et al. Socioeconomic and race/ ethnic differences in daily salivary cortisol profiles: the Multiethnic Study of Atherosclerosis. PNEC. 2010;35:932–43. doi: 10.1016/j.psyneuen.2009.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Radloff LS. The CES-D scale. A self-report depression scale for research in the general population. Applied Psychol Meas. 1977;1:385–401. [Google Scholar]
- 28.Raudenbush SW, Bryk AS. New York: Sage Publications; 2002. Hierarchical linear models: applications and data analysis methods. [Google Scholar]
- 29.Liang K-Y, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73:13–22. [Google Scholar]
- 30.Basner M, Müller U, Elmenhorst EM. Single and combined effects of air, road, and rail traffic noise on sleep and recuperation. Sleep. 2011;34:11–23. doi: 10.1093/sleep/34.1.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Babish W. Stress hormones in the research on cardiovascular effects of noise. Noise Health. 2003;5:1–11. [PubMed] [Google Scholar]
- 32.Hale L, Do DP. Racial differences in self-reports of sleep duration in a population-based study. Sleep. 2007;30:1096–103. doi: 10.1093/sleep/30.9.1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Touma C, Painnan S. Does lack of sleep cause diabetes? Cleveland Clinic J Med. 2011;78:549–58. doi: 10.3949/ccjm.78a.10165. [DOI] [PubMed] [Google Scholar]
- 34.Patel SR, Hu FB. Short sleep duration and weight gain: a systematic review. Obesity. 2012;16:643–53. doi: 10.1038/oby.2007.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Durmer JS, Dinges DF. Neurocognitive consequences of sleep deprivation. Semin Neurol. 2005;25:117–29. doi: 10.1055/s-2005-867080. [DOI] [PubMed] [Google Scholar]
- 36.Cappuccio FP, Taggart FM, Kandala NB, Currie A. Meta-analysis of short sleep duration and obesity in children and adults. Sleep. 2008;31:619. doi: 10.1093/sleep/31.5.619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wolfson AR, Carskadon MA. Sleep schedules and daytime functioning in adolescents. Child Dev. 2008;69:875–87. [PubMed] [Google Scholar]
- 38.Owens JA, Belon B, Moss P. Impact of delaying school start time on adolescent sleep, mood, and behavior. Arch Pediatr Adolesc Med. 2010;164:608. doi: 10.1001/archpediatrics.2010.96. [DOI] [PubMed] [Google Scholar]
- 39.Lauderdale DS, Knutson KL, Yan LL, Liu K, Rathouz PJ. Self-reported and measured sleep duration: how similar are they? Epidemiology. 2008;19:838–45. doi: 10.1097/EDE.0b013e318187a7b0. [DOI] [PMC free article] [PubMed] [Google Scholar]


