Abstract
This study explored the influence of an external support at the thoracic and pelvic level of the trunk on the success of reaching, postural stability and reaching kinematics while infants reached for a toy. Seventeen infants (4–6 months) were clustered into two groups according to their trunk control assessed with the Segmental Assessment of Trunk Control (SATCo). Major differences were seen between groups with pelvic support, whereas with thoracic support, all infants showed similar quality reaching behaviours. With the external pelvic support, infants who had acquired trunk control in the lumbar region were more accurate in their reaching movements (less movement time, improved straightness of reach, less movement units and path length per movement unit) and were more stable (decreased trunk and head displacement) during a reach than infants that had only acquired trunk control in the thoracic region. These results support the hypothesis that trunk control influences the quality of reaching behaviour.
Keywords: typically developing infants, segmental trunk control, sitting, reaching
Introduction
Postural control and reaching movements are two remarkable and complex motor milestones that are acquired progressively during the first years of life and are subsequently used throughout life in a variety of tasks (van der Heide et al. 2003). Although the maturational process of these two functions is different and emerges at various developmental stages during infancy, they are closely related to each other. It is widely acknowledged that motor development is not only a result of neural maturation, but is a dynamic process involving interaction between environmental constraints and sensorimotor systems. Reaching for an object is usually accompanied by postural adjustments prior to and during movement to provide mechanical stability and to maintain the body's equilibrium (Assaiante et al. 2005; Van der Fits et al. 1999a).
Research regarding the sequence of development of trunk control is still a matter of controversy. For instance, evidence has shown that intentional reaching with the feet can be developed earlier than with the hands, at the age of 2 months, in a specified context (Galloway and Thelen 2004), implying the possibility of a bottom-up sequence of trunk control. However, there is also evidence supporting the concept that head and trunk control defined as non-perturbance of head and torso during reach (Thelen and Spencer 1998), are developed in a top-down order. For example, infants are able first to maintain their head in relation to the trunk when they are 2 – 3 months old, although head control is not complete at this developmental stage (Touwen 1976; van Wullften Palthe and Hopkins 1993). The more mature head control at 4 months of age is important for environmental exploration (Hadders-Algra 2008) and it has also been suggested to be relevant in successful reaching (Thelen and Spencer 1998). In addition to this evidence, a top-down direction-specific recruitment of cervical, thoracic and lumbar muscles is predominant at 4 months of age, also suggesting functional relevance of a top-down order (van Balen et al. 2012). Subsequently, the ability to sit upright without support occurs approximately at the age of 8–9 months (Harbourne et al. 1993; McGraw 1945; Saavedra et al. 2012). Beginning at that time and continuing up to 18 months there is a gradual replacement by a bottom-up recruitment preference, indicating that the focus of control moves towards the support surface (Assaiante 1998; Hadders-Algra 2008).
The presence of direction–specific activity of postural muscles and the complete top-down pattern of recruitment of postural muscles used in the control of independent sitting is not a prerequisite for the emergence of reaching movements, although the quality and success of reaching is associated with this recruitment (de Graaf-Peters 2007). Postural control development appears to improve reaching kinematics because reaching is associated with self-produced complex and internal postural perturbations which change according to the infant's position and level of stability (de Graaf-Peters et al. 2007, Hopkins and Rönnqvist 2002; Thelen and Spencer 1998). These self-produced perturbations caused by the reach must be compensated by preparatory postural adjustments to allow an accurate reach to occur. Trunk control, which is the foundation of posture, is a critical element for early reaching. Studies have demonstrated this by enabling the emergence of reaching movements in newborn infants when given appropriate support of the entire trunk (Grenier and Amiel-tison 1981; von Hofsten 1982). This interesting fact suggests that arm muscular strength or control of the arm's biomechanics may be a less significant factor in relationship to reaching efficiently once the trunk is supported.
The ability to reach appears when infants are about 3 months old but reaches are characterized by irregular trajectories and are unsuccessful in terms of grasping and holding objects (Van der Fits et al. 1999b). It is not until the age of 4–5 months that the onset of functional reaching occurs (Gessell and Ames 1947; von Hofsten 1991). At this age, full-term infants are able to grasp stationary and moving toys (Grönqvist 2011); infants aged 18 weeks can even grasp non-stationary toys moving at 30cm/s (von Hofsten 1980). At 4–5 months, successful reaches, defined as including object contact, are characterized by large numbers of movement units (MUs) and non-regular trajectories towards the object (Gessell and Ames 1947). After the age of 6 months, the reaching sequence during which infants orient and direct their hand towards a toy becomes straighter and shorter. Also, the movement is composed of fewer MUs (1–2) and the first MU is differentiated by being longer in length and duration than the second (Hopkins and Rönnqvist 2002). At this time the kinematic parameters of a reach start to assume an adult-like form in which straightness and smoothness are correlated; fewer MUs are associated with a straighter trajectory of reaching, and peak velocity is achieved at a greater percent of the reaching path (von Hofsten 1991).
Previous studies on the development of reaching skills have been designed to test muscular strength and control of arm mechanics of infants. These studies concluded that insufficient muscular strength or insufficient control over the unstable arm does not restrict early reaching and that movement becomes smoother as age increases (Out et al. 1998; Konczak et al. 1997). Although this research has given insights into the motor control of reaching, it has not addressed the issue of the infants’ need for trunk control as a foundational element required for accurate reaching.
Though considerable research has been performed independently on both the development of postural control and the development of reaching, the relationship between the maturational transition of reaching kinematics and the progression of trunk control acquired during early infancy has not been thoroughly investigated. Previous studies have dealt with the lack of trunk control in 4 and 6 month old infants, by using supine or semi-reclined seating, which alters the effect of gravity on the trunk and subsequently influences the kinematics of reaching. In addition these studies evaluated the trunk as a single segment, and therefore often designed protocols to observe infants sitting in fully supported or unsupported states (de Graaf-Peters et al. 2007; Hopkins and Rönnqvist 2002; Thelen and Spencer 1998), failing to allow observation of the contribution of individual regions to trunk control and reaching. Addressing the development of postural control from a multi-segment perspective is a novel technique that has yet to be fully explored. We suggest keeping the effect of gravity constant by using vertical alignment with higher versus lower levels of external trunk support to allow more precise analysis of the effect of trunk control on reaching.
In summary, though previous research has given extensive insights into the control of reaching development, it has not specifically addressed the contribution of upper and lower regions of trunk control to reaching. This study will seek to fill this gap through the use of two unique approaches. First we used vertical alignment with two levels of external support (thoracic and pelvic) to test effects of regional support on reaching in typically developing infants between the ages 4 and 6 months. Within this temporal period sitting posture control emerges, and infants master their reaching and grasping skills. Secondly, we classified our sample into two groups according to the infant’s region of intrinsic trunk control as measured by the Segmental Assessment of Trunk Control (SATCo) (Butler et al. 2010). Group 1 infants demonstrated postural control in the thoracic region while Group 2 infants demonstrated control in the thoracic and lumbar region. Kinematic parameters of visually guided reaches towards a toy were examined as well as their success in grasping it. The hypothesis suggested was that with the use of the external thoracic support all infants would have equivalent reaching patterns and success since both groups demonstrated postural control in the thoracic region. In addition, it suggested that when external support was provided at the pelvic level, only the infants who already had developed control of the lumbar region would have better reaching performance and success.
Method
Participants
Seventeen healthy infants born at term were recruited for this cross-sectional study (9 males and 8 females). The infants were aged between 4 and 6 months. The recruitment was carried out by using flyers in different child care centers in Eugene and Springfield (Oregon, USA). This study was reviewed and accepted by the Institutional Review Board for Human Subjects Research at the University of Oregon.
Materials and Procedure
Subjects were asked to come to the laboratory for one session of approximately 90 minutes. During this visit, infants were clinically tested with the SATCo to determine their level of trunk control and the Alberta Infant Motor Scale (AIMS) to identify their level of gross motor function. In addition, the parents were asked to respond to a health questionnaire about their infants, were informed in detail about the experimental procedure and signed the informed consent. All infants were video recorded during the assessment. Table 1 shows the clinical characteristics for each group.
Table 1.
Group Characteristics
| n | Sex Ratio | SATCo | AIMS | Age | Sitting Ability |
|
|---|---|---|---|---|---|---|
| Group | (Male:Female) | M(min-max) | M(min-max) | M(min-max) | ||
| Group 1 | 8 | (5:3) | 4.50 (4 – 5) | 18.25 (15 – 24) | 4.50 (4 – 5) | Non-sitters |
| Group 2 | 9 | (3:6) | 6.56 (6 – 7) | 29.33 (23 – 41) | 6.22 (5 – 6) | Sitters |
Note: M = mean.
SATCo is a new clinical measure that allows a precise examination of balance control of the trunk at various levels of support. It tests the infant’s trunk control as the evaluator manually changes the level of trunk support from a high level of support at the shoulder girdle to assess cervical (head) control, through support at the axillae (upper thoracic control), inferior scapula (mid-thoracic control), lower ribs (lower thoracic control), below ribs (upper lumbar control), pelvis (lower lumbar control), and finally, no support, in order to measure full trunk control. It is designed to assess: 1. static control (maintaining a neutral trunk posture) 2. active or anticipatory control (maintaining a neutral posture during head movement) and 3. reactive control (maintaining or regaining trunk control following a threat to balance, produced by a brisk nudge). The infant’s ability to maintain or quickly regain a vertical position of the free region of the trunk in all planes is assessed during static, active and reactive testing and scored accordingly as present or absent. The score reflects the region where infants lose control of posture in; 1 = head, 2 = upper thoracic, 3 = mid-thoracic, 4 = lower thoracic, 5 = upper lumbar, 6 = lower lumbar, 7 = pelvis, 8 = no loss of trunk control (Butler et al. 2010). Thus, for example, an infant with SATCo score 4, loses control of posture in static, active or reactive tests when the evaluator supports the lower thoracic region of the trunk (lower ribs). However, an infant with SATCo score 6, does not lose control until the evaluator supports the lower lumbar region of the trunk (the pelvis). In this study, we classified our sample into two groups according to their SATCo score: Group 1 = infants with SATCo scores 4 and 5 (demonstrating control in the thoracic region), Group 2 = infants with SATCo scores 6 and 7 (demonstrating control in the thoracic and lumbar region). Other tools such as the AIMS, inform us about the acquisition of infants' developmental gross motor milestones from term age through independent walking (Piper et al. 1992). Both of these tests follow a specific scoring criterion and have been shown to be valid, reliable measures of developmental change in infants (Butler et al. 2010; Piper et al. 1992; van Haastert et al. 2006). They thus can be used as clinical measures of the developmental level of trunk control and motor function.
The reaching test was conducted at pelvic and thoracic levels of support for every infant. The support at the thoracic level was placed below the scapular girdle and the pelvic level of support was around the pelvis, corresponding to middle thoracic level and lower lumbar level of the SATCo, respectively. The design of the study was counterbalanced, with half the infants first being provided with thoracic support, and half first being provided with pelvic support, in order to eliminate fatigue or training effects as confounding variables.
The reaching test was synchronized with the collection of kinematic data using the Flock of Birds miniBIRD electromagnetic tracking sensors (Ascension Technology, Burlington, VT). Four sensors were placed on the infant: one superficial to the styloid process of the radius on each wrist, one on the posterior and prominent part of the cervical vertebra 7 (C7), and one on a headband with the sensor centered on the forehead. These sensors were used to track arm and head movements. Prior to starting the reaching test, position markers were taken of the left and right tragus, the medial/lateral and anterior/posterior points of the external support (pelvic or thoracic). This allowed us to estimate the location of the head center of mass (HCOM) using the center of the distance between the midpoint of the two tragus markers and the head sensor. The center of the base of support (BOS) was defined as the midpoint of the two vectors created between the medial/lateral and anterior/posterior markers of the external level of support.
The reaching test involved the infant being placed in a seated position on a bench. The pelvis of the infant was secured to the bench with specially designed straps and Velcro. Three straps were firmly attached to the underside of the bench: two of them were used to wrap each hip joint and the third surrounded both posterior superior iliac spines (Butler et al. 2010). An adjustable support device located behind the bench provided trunk stability at one of the two levels studied. This device surrounded the trunk, offering strong stability at the level being studied and below (Saavedra et al. 2012). Once posture was stabilized, a colourful object was hung by the tester in front of the infant’s sternum at approximately the arm’s length. The toy was presented 15 times per level of support, but there were occasions in which this number had to be reduced due to fussiness of the infant. If that was the case, the infant’s maximum number of trials was noted and the rest was counted as missing data. In addition, the tester occasionally presented a different toy (coloured rings or blocks) in order to keep the infant engaged in the task of reaching. The entire session was video recorded to ensure differentiation between nondirected arm movements and reaching movements towards the toy during the analysis.
All reaches were visually analyzed by two coders using computerized video-coding software (www.openshapa.org) for further evaluation of the kinematic parameters. This program allowed us to determine the onset and offset of every visually guided intentional reach. A light emitting diode (LED), placed on the corner of the visual field, was used to synchronize video and kinematic data during each reaching trial. With this, we made sure that we were selecting reaches within the reaching test time. We defined the onset of a reach as the moment when the infant initiated a movement of the upper extremity towards the toy while looking at it. The offset of the reach was determined when the infant touched the toy with the intention of grasping it. If an infant initiated a reaching movement towards the toy and lost interest during the trajectory by stopping and looking away, these reaches were not selected. Inter-rater reliability was validated by having both coders evaluate 50% of the data and obtained a coefficient of agreement above 0.85.
Reaches were coded as unimanual or bimanual. We defined bimanual reaches as those in which we visually saw the infant touch the toy with both hands and which also had an onset time difference between both arms of less than 1000 ms. Occasionally, infants would begin unimanually and then switch to the other arm before reaching the toy. In this case, for the kinematic data analysis, only one arm, considered as the predominant arm, was selected. This selection was the same for the case of bimanual reaches. The arm predominance was determined based on the hand that manipulated the object once it was held. If infants used compensatory strategies like reaching with their head or dragging the toy with their forearm, these were not considered.
Data Analysis
Data were filtered with a Butterworth low-pass filter with a cut-off frequency of 6Hz prior to calculating the kinematic variables. All unimanual or bimanual reaches were pooled together and were analyzed at both thoracic and pelvic levels for each group, to output kinematic data. Additionally, the total number of successful and unsuccessful grasps of the toy was also counted. Kinematic data at every level of support were analyzed using custom algorithms with the software Matlab (The MathWorks, Inc., Boston, MA). We examined the following variables for each reach: movement time, straightness score, MUs, reach path divided by the number of MUs, angular head displacement, angular trunk displacement and percentage of successful grasps.
Movement time was calculated in seconds between the onset and the end of the reach. Straightness was determined by first measuring the trajectory of a straight line from the beginning of the trial to the moment when the infant touched the toy, which is the shortest distance to the target; considered as the baseline path length with a value of one. The amount that the arm movements deviated from this trajectory was then determined as the proportional increase in trajectory compared to this baseline path. Using this method, values greater than one meant a more devious arm movement (von Hofsten 1991). A MU was defined according to Grönqvist et al. (2011), as the portion of the arm movement between two velocity minima with a velocity peak that should be greater than 2.3 cm/s. Also, if the difference between the highest minima of one MU and the peak velocity of another MU was less than 8 cm/s they were considered as one MU. Path length per MU was calculated by dividing the total reach path by the number of MUs. In terms of postural control, the angular displacement of the head and trunk were analyzed as two different segments to distinguish their displacement during a reach. Head displacement and trunk displacement were calculated as the angular summation during a reach in the anterior-posterior plane. For the head displacement, the angle between the HCOM with respect to the C7 sensor was applied and for the trunk displacement, the angle between the C7 sensor and the BOS was used. This provided the angle of the trunk segment above the external support.
Statistical Analysis
The data analysis was carried out using SPSS 16.0 for Windows (SPSS Inc., Chicago, IL, USA). The total number of successful/unsuccessful grasps and the kinematic parameters were computed by using the Linear Mixed procedure. This statistical approach is more accurate when data are more unbalanced since it allows for a more adequate modeling of the covariance structure and can deal with incomplete data. Bayesian Criterion-type model was used to select the covariance structure with the best fit; the structure exhibiting the smallest criteria values was considered the most desirable. The model selected was the Scale Identity covariance for the repeated measure. Follow-up pairwise comparisons based on the estimated marginal means were conducted to analyze significant main or interaction effects applying the Bonferroni adjustment. For all tests, the preset alpha level was .05.
Results
Differences in Reaching Accuracy According to Level of Support
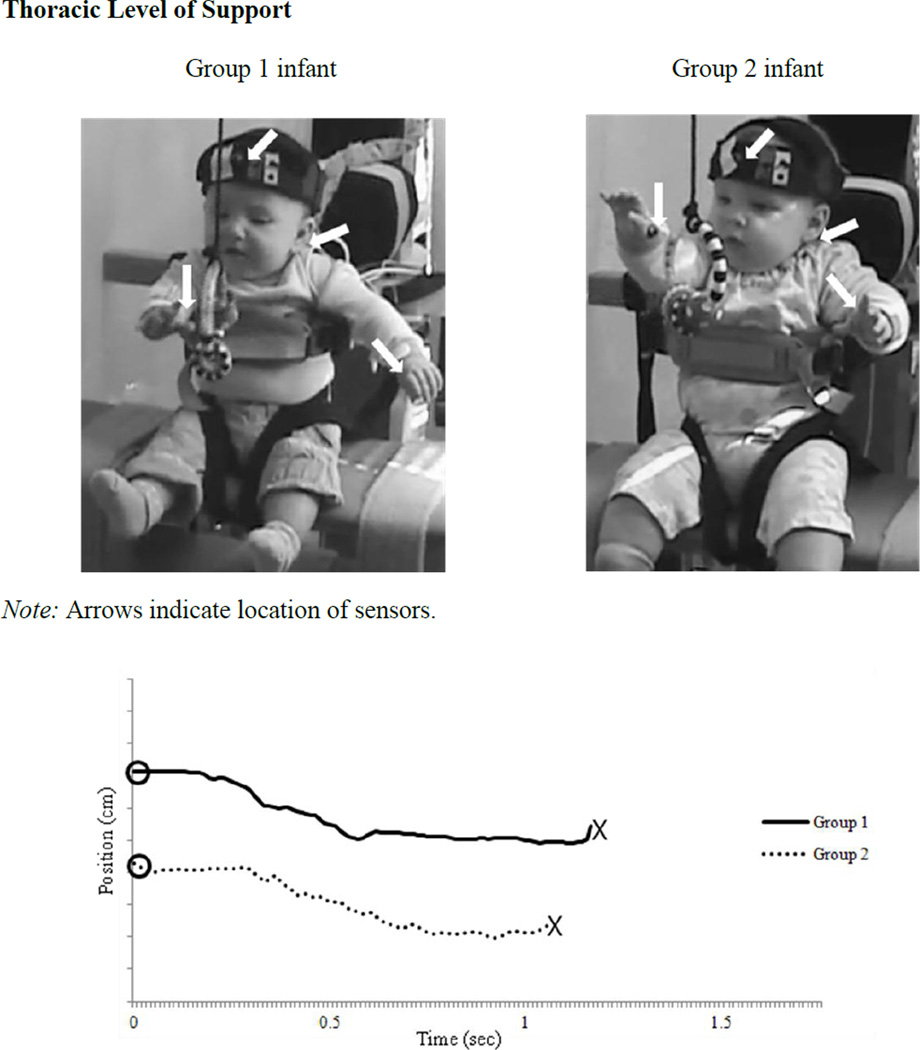
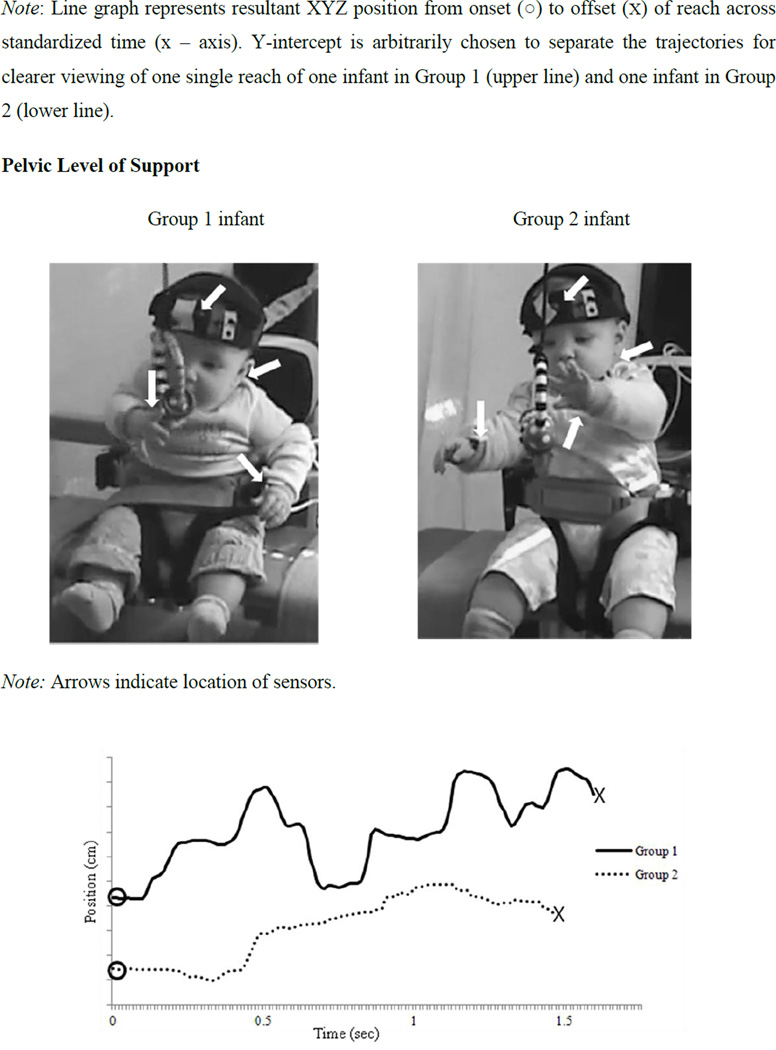
The graphs from Figure 1 are examples of a reach at the thoracic and pelvic level of support of a Group 1 and a Group 2 infant, in addition to the photographic image during the reach. The graphical representation of the arm trajectory shows how the two infants showed a similar reaching position trajectory with thoracic support and both infants seemed to look equally stable during the reach; however, the arm trajectories with pelvic support show that the Group 1 infant had a more jerky reach than the Group 2 infant. A total of number of 293 reaches was analyzed. Figure 2 shows statistical results for group effects at each level of support.
Figure 1.
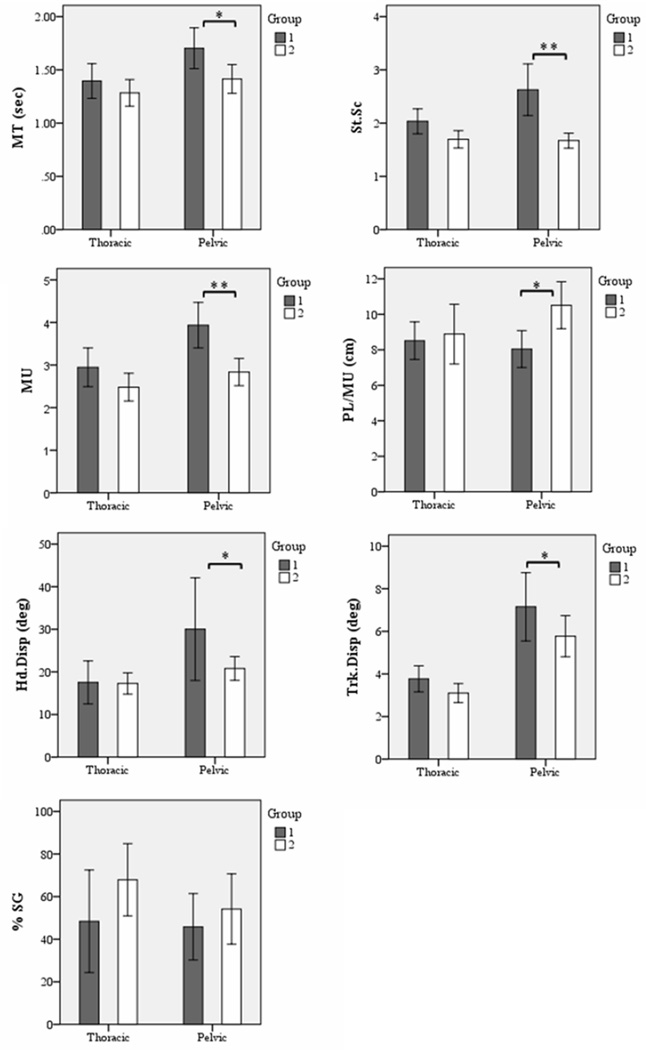
Figure 2.
Estimated group means for: movement time (MT), straightness score (St.Sc.), movement units (MU), path divided by number of MUs (PL/MU), angular head displacement (Hd.Disp.), angular trunk displacement (Trk.Displ.), and percentage of successful grasps (%SG); at both levels of support, Group 1 (dark gray bars) and Group 2 (light gray bars). Error bars, +/− 2 SE. * = p < .05, ** = p < .01.
Thoracic Support
None of the variables analyzed showed significant effects of group for thoracic support. These results suggest that all infants were equally stable with thoracic support and had similar kinematic parameters during the reaching sequence.
Pelvic Support
All variables except for %SG showed a significant effect of group for pelvic support. Group 1 infants compared to Group 2 infants showed: increased movement time, F(1, 289) = 6.82, p < .05, an increase in straightness score, F(1, 289) = 24.90, p < .01, an increase in MUs, F(1, 289) = 13.97, p < .01, a decrease in path length per MU, F(1, 289) = 6.49, p < .05, an increase in head displacement, F (1, 289) = 4.42, p < .05 and an increase in trunk displacement, F(1, 289) = 4.07, p < .05.
Overall, these results show that when providing an external pelvic support, stability, determined by Hd.Displ. and Trk.Displ., is better in infants who had acquired control of their thoracic and lumbar region (SATCo scores 6 and 7); additionally they showed straighter reaches, less MUs and covered greater distance per MU.
Discussion
The primary purpose of this study was to more specifically investigate the contribution of upper and lower regions of trunk control to reaching. We addressed this by using vertical alignment at two levels of support (thoracic and pelvic) and by grouping infants according to their region of intrinsic trunk control. In this manner, we confirm previous studies by showing that the infants’ ability to control the trunk influences the quality of reaching (Spencer et al. 2000; Hopkins and Ronqvist 2002). In addition, our results expand previous findings by providing evidence that depending on the intrinsic control of the trunk region acquired, the level of external support has an impact on the quality of reaching movements. In what follows, we discuss how reaching abilities of two groups of infants who demonstrated control of different regions of the trunk showed significant differences in their reaching patterns depending on whether they were given thoracic vs. pelvic support.
We predicted that if infants were provided with thoracic support, the two groups would demonstrate similar reaching behaviours and show similar patterns of control of their stability, given that both groups had trunk control at the thoracic region, according to their SATCo score. In contrast, we believed that when provided with pelvic support the two groups would behave differently due to the difference of the extent of intrinsic trunk control they had developed. Our prediction was correct when comparing Group 1 and 2 for movement time, straightness score, MUs, path length per MU, head displacement and trunk displacement. However, percentage of successful grasps was the same between Group 1 and 2 at both levels of support.
Previous research showed that 6 month old infants have quicker reaches, straighter reaching trajectories, less MUs and increased path length per MU than 4 month infants (de Graaf-Peters et al. 2007; Fallang et al. 2000; Thelen and Spencer 1998; von Hofsten 1991). We expanded these findings by testing 4 to 6 month old infants in vertical alignment with external support at thoracic and pelvic levels and showed that differences in reaching kinematics depend on the infants’ region of intrinsic control. Both groups had acquired control in the thoracic region and demonstrated similar reaching patterns when given external support at the thoracic level. This is consistent with other studies showing the development of head and upper torso control as precursors for the emergence of successful reaching (Thelen and Spencer 1998; Spencer et al. 2000). In contrast, Group 2 had also acquired control in the lumbar region and demonstrated significantly better quality of reach than Group 1 when provided external support at the pelvic level. Between Groups 1 and 2 there were many differences, such as age, experience and gross motor development. However the fact that differences between groups were only seen with pelvic support and not with thoracic support indicates that region of intrinsic control achieved is the main factor contributing to differences in quality of reaching observed in this study.
The variables related to postural stability during a reach corroborate those from the clinical data from the SATCo and AIMS evaluation of the infants. Group 1 infants had a mean SATCo score of 4.50 and were non-independent sitters, whereas Group 2 infants were independent sitters and had a mean SATCo score of 6.56. These results correspond well with data from the previous literature, which suggest that the motor strategies for independent sitting acquisition do not emerge until approximately 5 months of age (Bayley, 1969; Gessell, 1946), and that until that point, muscle response synergies underlying reaching movements are variable (Hadders-Algra et al. 1996; Hirschfeld and Forssberg 1994). In addition, the SATCo scores for each group show a trend similar to the results found by Saavedra (2009) regarding the segmental development of trunk control, and further expand these results by showing how the region of trunk control affects reaching parameters.
One specific item of the SATCo test is to analyze the active control of posture for each support level, which is assessed by encouraging the infant to actively turn their head to each side. This requires anticipatory postural adjustments to maintain the head and trunk in the midline and this is precisely what is being challenged during a reach. Group 1 infants had increased displacement of the head and trunk with external pelvic support as compared to Group 2, indicating excessive sway and thus loss of balance control. This was expected since Group 1 infants did not have the ability to actively control their trunk when manually supported at the lower lumbar or pelvic region during the SATCo evaluation. On the contrary, all infants showed active trunk control with mid-thoracic support and thus, kinematic parameters related to posture indicate that with external thoracic support, the ability to maintain stability during a reach was the same for both groups.
An unexpected result was the lack of difference in percentage of successful grasps between Group 1 and 2 with pelvic support. However, our findings are consistent with other studies showing that once onset of successful reaches appears, infants are equally successful in a variety of testing positions. For example, the study conducted by Van der Fits et al. (1999a) showed that 4–5 month old infants, when placed in three positions; supine, semi-reclined and in an infant chair, were equally able to produce successful reaches in all three testing positions. This suggests that once infants learn to successfully reach for a toy, their further improvement of intrinsic trunk control contributes primarily to increased quality of reaching.
Conclusion
Previous studies have shown that infants start reaching at 4 months of age before acquiring full trunk control (Fallang et al. 2003; Out et al. 1998; Van der Fits et al. 1999a). It has also been shown that when given support both newborns and other young infants initiate reaching movements towards objects (Grenier and Amiel-tison 1981; von Hofsten 1982). Studies that have investigated the effects of trunk support in infants have not quantified either the amount of support provided or the infant’s intrinsic level of trunk control. This study expands previous results by showing for the first time that the specific region of trunk control influences reaching ability. More precisely, the data suggest that reaching performance is tightly correlated with the progressive segmental acquisition of trunk control. This raises important questions regarding whether this correlation of reaching performance with trunk control is comparable to that seen in infants with developmental delays and neurological disorders. Similar information on children with neurological disorders could be used to implement more efficient therapeutic strategies to enable reaching in daily life activities.
Acknowledgements
This work was supported by the National Institutes of Health grant 1R01HD062745, Marjorie Woollacott, principal investigator, and by the McNair Scholars Program for Francine Porter. The authors would like to thank Wayne Manselle for his valuable help with computer programming and technical assistance.
Contributor Information
Jaya Rachwani, Human Physiology and Institute of Neuroscience, University of Oregon, rachwani@uoregon.edu.
Victor Santamaria, Human Physiology and Institute of Neuroscience, University of Oregon, vsantama@uoregon.edu.
Sandra L. Saavedra, Human Physiology and Institute of Neuroscience, University of Oregon, ssaavedr@umich.edu
Stacy Wood, Human Physiology and Institute of Neuroscience, University of Oregon, staci@uoregon.edu.
Francine Porter, Human Physiology and Institute of Neuroscience, University of Oregon, francine.porter@gmail.com.
Marjorie H. Woollacott, Human Physiology and Institute of Neuroscience, University of Oregon, mwool@uoregon.edu
References
- Assaiante C, Mallau S, Viel S, Marianne J, Schmitz C. Development of posture control in healthy children: A functional approach. Neural Plast. 2005;12:109–118. doi: 10.1155/NP.2005.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Assaiante C. Development of locomotor balance control in healthy children. Neurosci Biobehav Rev. 1998;22(4):527–532. doi: 10.1016/s0149-7634(97)00040-7. [DOI] [PubMed] [Google Scholar]
- Bayley N. Bayley Scales of Infant Development. New York: Oxford University Press; 1969. [Google Scholar]
- Butler PB, Saavedra S, Sofranac M, Jarvis SE, Woollacott MH. Refinement, reliability, and validity of the segmental assessment of trunk control. Pediatr Phys Ther. 2010;22:246–257. doi: 10.1097/PEP.0b013e3181e69490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Graaf-Peters VB, Bakker H, van Eykern LA, Otten B, Hadders-Algra M. Postural adjustments and reaching in 4- and 6- months-old infants: an EMG and kinematical study. Exp Brain Res. 2007;181:647–656. doi: 10.1007/s00221-007-0964-6. [DOI] [PubMed] [Google Scholar]
- Fallang B, Saugstad OD, Hadders-Algra M. Goal directed reaching and postural control in supine position in healthy infants. Behav Brain Res. 2000;115:9–18. doi: 10.1016/s0166-4328(00)00231-x. [DOI] [PubMed] [Google Scholar]
- Fallang B, Didrik S, Hadders-Algra M. Postural Adjustments in Preterm Infants at 4 and 6 Months Post-Term During Voluntary Reaching in Supine Position. Pediatr Res. 2003;54:826–833. doi: 10.1203/01.PDR.0000088072.64794.F3. [DOI] [PubMed] [Google Scholar]
- Galloway JC, Thelen E. Feet first: object exploration. Infant Behav & Dev. 2004;27:107–112. [Google Scholar]
- Gessell A. Manual of child psychology. New York: Wiley; 1946. The ontogenesis of infant behavior. [Google Scholar]
- Gessell A, Ames LB. The development of handedness. J Genet Psychol. 1947;70:155–175. doi: 10.1080/08856559.1947.10533403. [DOI] [PubMed] [Google Scholar]
- Grenier A, Amiel-tison C. Liberated-Motricity by Holding The Head During The 1st Weeks of Life. Arch Fr Pediatr. 1981;8:557–561. [PubMed] [Google Scholar]
- Grönqvist H, Brodd SK, Von Hofsten C. Reaching strategies of very preterm infants at 8 months corrected age. Exp Brain Res. 2011;209:225–233. doi: 10.1007/s00221-011-2538-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hadders-Algra M. Development of postural control. In: Hadders-Algra M, Brogren Carlberg E, editors. Postural Control: a key issue in developmental disorders. London: Mac Keith Press; 2008. pp. 22–73. [Google Scholar]
- Hadders-Algra M, Brogren E, Forssberg H. Ontogeny of postural adjustments during sitting in infancy: variation, selection and modulation. J Physiol. 1996;493:273–288. doi: 10.1113/jphysiol.1996.sp021382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harbourne RT, Giuliani C, Neela JM. A kinematic and electromyographic analysis of the development of sitting posture in infants. Dev Psychobiol. 1993;26:51–64. doi: 10.1002/dev.420260105. [DOI] [PubMed] [Google Scholar]
- Hirschfeld H, Forssberg H. Epigenetic Development of Postural Responses for Sitting during Infancy. Exp Brain Res. 1994;97:528–540. doi: 10.1007/BF00241546. [DOI] [PubMed] [Google Scholar]
- Hopkins B, Rönnqvist L. Facilitating postural control: effects on the reaching behavior of 6-month-old infants. Dev Psychobiol. 2002;40:168–182. doi: 10.1002/dev.10021. [DOI] [PubMed] [Google Scholar]
- Konczak J, Borutta M, Dichgans J. The development of goal-directed reaching in infants II. Learning to produce task-adequate patterns of joint torque. Exp Brain Res. 1997;113:465–474. doi: 10.1007/pl00005599. [DOI] [PubMed] [Google Scholar]
- van Balen LC, Dijkstra LJ, Hadders-Algra M. Development of postural adjustments during reaching in typically developing infants from 4 to 18 months. Exp Brain Res. 2012;220(2):109–119. doi: 10.1007/s00221-012-3121-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGraw MB. The neuromuscular maturation of the human infant. London: McKeith; 1945. [Google Scholar]
- Out L, van Soest AJ, Savelsberg GJP, Hopkins B. The effects of posture on early movements. J Mot Behav. 1998;3:260–272. doi: 10.1080/00222899809601341. [DOI] [PubMed] [Google Scholar]
- Piper MC, Pinnell LE, Darrah J, Maguire T, Byrne PJ. Construction and validation of the Alberta Infant Motor Scale (AIMS) Can J Public Health. 1992;83:46–50. [PubMed] [Google Scholar]
- Saavedra S. Contribution of Spinal Segments to Control of Posture in Typical and Atypical Development. University of Oregon: Doctoral Dissertation; 2009. [Google Scholar]
- Saavedra SL, Van Donkeelar P, Woollacott MH. Learning about gravity: Segmental assessment of upright control as infants develop independent sitting. J Neurophysiol. 2012;108(8):2215–2229. doi: 10.1152/jn.01193.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spencer JP, Vereijken B, Diedrich FJ, Thelen E. Posture and the emergence of manual skills. Dev Sci. 2000;3(2):216–233. [Google Scholar]
- Thelen E, Spencer JP. Postural control during reaching in young infants: a dynamic systems approach. Neurosci Biobehav Rev. 1998;22:507–514. doi: 10.1016/s0149-7634(97)00037-7. [DOI] [PubMed] [Google Scholar]
- Touwen BCL. Neurological development in infancy. Philadelphia: JB Lippincott; 1976. [Google Scholar]
- Van der Fits IBM, Klip AWJ, Van Eykern LA, Hadders-Algra M. Postural adjustments during spontaneous and goal directed arm movements in the first half year of life. Behav Brain Res. 1999a;106:75–90. doi: 10.1016/s0166-4328(99)00093-5. [DOI] [PubMed] [Google Scholar]
- Van der Fits IBM, Otten E, Klip AWJ. The development of postural adjustments during reaching in 6- to 8-month-old infants. Exp Brain Res. 1999b;126:517–528. doi: 10.1007/s002210050760. [DOI] [PubMed] [Google Scholar]
- van der Heide JC, Otten B, van Eykern LA, Hadders-Algra M. Development of postural adjustments during reaching in sitting children. Exp Brain Res. 2003;151:32–45. doi: 10.1007/s00221-003-1451-3. [DOI] [PubMed] [Google Scholar]
- van Balen LC, Dijkstra Linze J, Hadders-Algra M. Development of postural adjustments during reaching in typically developing infants from 4 to 18 months. Exp Brain Res. 2012;220:109–119. doi: 10.1007/s00221-012-3121-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Haastert IC, de Vries LS, Helders PJM, Jongmans MJ. Early gross motor development of preterm infants according to the Alberta infant motor scale. J Pediatr. 2006;149:617–622. doi: 10.1016/j.jpeds.2006.07.025. [DOI] [PubMed] [Google Scholar]
- von Hofsten C. Eye-Hand coordination in the newborn. Dev Psychol. 1982;18:450–461. [Google Scholar]
- von Hofsten C. Predictive reaching for moving objects by human infants. J Exp Child Psychol. 1980;30(3):369–382. doi: 10.1016/0022-0965(80)90043-0. [DOI] [PubMed] [Google Scholar]
- von Hofsten C. Structuring of early reaching movements: A longitudinal study. J Mot Behav. 1991;23:280–292. doi: 10.1080/00222895.1991.9942039. [DOI] [PubMed] [Google Scholar]
- van Wullften Palthe T, Hopkins B. A longitudinal study of neural maturation and early mother-infant interaction. J Child Psychol Psychiatry. 1993;34:1031–1041. doi: 10.1111/j.1469-7610.1993.tb01106.x. [DOI] [PubMed] [Google Scholar]