Abstract
Program implementers and qualitative researchers have described how increasing availability of HIV antiretroviral therapy (ART) is associated with improvements in psychosocial health and internalized stigma. To determine whether, and through what channels, ART reduces internalized stigma, we analyzed data from 262 HIV-infected, treatment-naïve persons in rural Uganda followed from ART initiation over a median of 3.4 years. We fitted Poisson regression models with cluster-correlated robust estimates of variance, specifying internalized stigma as the dependent variable, adjusting for time on treatment as well as socio-demographic, clinical, and psychosocial variables. Over time on treatment, internalized stigma declined steadily, with the largest decline observed during the first two years of treatment. This trend remained statistically significant after multivariable adjustment (χ2=28.3; p=0.03), and appeared to be driven by ART-induced improvements in HIV symptom burden, physical and psychological wellbeing, and depression symptom severity.
Keywords: social stigma, depression, antiretroviral therapy, highly active, HIV, Uganda
INTRODUCTION
Effective HIV antiretroviral therapy (ART) has been shown to have beneficial impacts on quality of life and mental wellbeing [1–6]. Its increasing availability in resource-limited settings may detach HIV infection from its perceived inevitable terminal medical consequences and concomitant household economic devastation [2, 7], attenuate people’s fears about the illness, and thereby reduce the stigma attached to it [8, 9]. Pervasive HIV-related stigma is an important public health and mental health issue in sub-Saharan Africa [10]. HIV stigma-related events have been shown to be associated with poorer mental health [11]. Internalized stigma, which results when persons with a stigmatized attribute (such as HIV) accept prevailing discriminatory attitudes as valid [12], has also been associated with poorer mental health [13, 14], as well as inhibition of serostatus disclosure [15] and non-adherence to HIV treatment [16].
Early experiences with HIV treatment scale-up in rural Haiti have been consistent with the hypothesis that treatment reduces the stigma of HIV, as program implementers have reported increased demand for HIV testing and counseling [17], fewer HIV-related discriminatory events [18], and increased social integration [19]. These observations have also been borne out in qualitative studies showing that treatment was associated with improved self-image among HIV-infected persons in South Africa and Zimbabwe [20–23]. Large sample studies have yielded conflicting findings about the extent to which treatment reduces the stigma of HIV [24–27]. These studies were restricted to relatively brief periods of data collection, however, and were unable to ascertain the robustness of any observed trends. Therefore we used data from an ongoing cohort of HIV-infected persons in rural Uganda, a region of the country where depression has been found to be relatively pervasive [28, 29] and associated with the HIV epidemic [30], to determine whether participants’ time on treatment was associated with reductions in stigma. A secondary aim of this study was to understand the potential channels through which these changes occurred.
MATERIAL AND METHODS
Study Design
Data for this analysis were drawn from the Uganda AIDS Rural Treatment Outcomes (UARTO) study, an ongoing cohort of treatment-naïve HIV-infected persons initiated in 2005. The primary study site is the Mbarara Immune Suppression Syndrome (ISS) Clinic, an HIV clinic prototypical of scale-up HIV clinics in the region that receive funding from bilateral and multilateral programs such as the U.S. President’s Emergency Plan for AIDS Relief (PEPFAR) and the Global Fund to Fight AIDS, Tuberculosis, and Malaria [31]. More than 100 patients are initiated on ART each month. The ISS Clinic is located in Mbarara, a rural region of southwestern Uganda, reachable by a five-hour automobile drive from the capital city, Kampala.
Persons who tested positive for HIV infection and who met medical criteria for ART were required to have two sessions of pre-treatment counseling before they were permitted to initiate ART [32]. On occasion, if a patient was thought to require immediate treatment, the counseling was either provided on the day of initiation or suspended altogether. These sessions, which were conducted by one of three trained counselors employed as clinic staff, generally lasted 20 minutes and focused on dosing schedule, drug toxicity, drug resistance resulting from missed doses, and management of missed doses. At subsequent visits, patients generally did not receive adherence counseling unless their provider had initiated an inquiry; in practice, virtually no patients received additional adherence counseling subsequent to treatment initiation. The same three counselors also provided supportive counseling for patients experiencing psychosocial difficulties on an as-needed basis. Ready-to-use therapeutic food supplements were given to patients who met stringent criteria for extreme malnutrition. Once patients were on a stable ART regimen, they generally returned to clinic and had contact with a medical officer, clinical officer, or nurse 2–5 times annually.
Patients at the ISS Clinic were eligible for participation in the UARTO study if they were newly initiating ART, were 18 years of age or older, and lived within 20 kilometers of the clinic. They were seen every three months, in a private research office near the ISS Clinic, for data collection that consisted of structured interviews (conducted by a research assistant in the local language, Runyankole) and blood draws. Beginning in August 2007, while recruitment of new treatment-naïve participants was still ongoing, a new scale for measuring internalized HIV-related stigma was added to the study questionnaire; all participants enrolled after that time were included in our analysis.
Written consent was obtained from all study participants. In the event that there were cultural literacy reasons why a signature was not appropriate, participants were allowed to sign consent forms with a thumbprint. Ethical approval for all study procedures was obtained from the Committee on Human Research, University of California at San Francisco; the Partners Human Research Committee, Massachusetts General Hospital; and the Institutional Ethical Review Committee, Mbarara University of Science and Technology.
Measures
The primary variable of interest in this analysis was the Internalized AIDS-Related Stigma Scale (IARSS) (Table 1) [33]. The IARSS is a six-item scale designed to measure the construct of internalized stigma and its attendant self-defacing internal representations of the self [12]. Each item has only two response options (“Yes” or “No”). The IARSS was originally developed using three independent samples of HIV-infected persons in South Africa, Swaziland, and the U.S. [33] and has demonstrated a coherent internal structure and good reliability and construct validity among HIV-infected persons in Uganda [34, 35]. At baseline, the estimated scale reliability coefficient for the internalized stigma scale was 0.73.
Table 1.
The Internalized AIDS-Related Stigma Scale
| 1. | It is difficult to tell people about my HIV infection. |
| 2. | Being HIV positive makes me feel dirty. |
| 3. | I feel guilty that I am HIV positive. |
| 4. | I am ashamed that I am HIV positive. |
| 5. | I sometimes feel worthless because I am HIV positive. |
| 6. | I hide my HIV status from others. |
We measured four constructs related to quality of life that we hypothesized to be associated with the degree of internalized stigma: HIV symptom burden, physical and psychological wellbeing, and depression symptom severity. HIV symptom burden was measured by inquiring about 29 different potential HIV-related symptoms (e.g., “problems with weight loss or wasting,” or “skin problems, such as rash, dryness, or itching”). Participants who endorsed a particular symptom were asked to score the extent to which they found it bothersome on a four-point Likert-type scale ranging from 0 to 4. These variables were used to create an equally weighted average of the z-scores [36], with the sign of the aggregate measure oriented so that greater values of the symptom index were associated with a greater symptom burden. At baseline, the estimated scale reliability coefficient for the symptom index was 0.83. Physical and psychological wellbeing were measured using the Medical Outcomes Study-HIV Health Survey (MOS-HIV) mental health summary (MHS) and physical health summary (PHS) scores [37]. At baseline, the estimated scale reliability coefficients for the Cognitive Functioning subscale of the MOS-HIV was 0.62, while the estimated scale reliability coefficients for the other seven multi-item subscales ranged from 0.78 to 0.89. Depression symptom severity was measured with the 15-item depression subscale of the Hopkins Symptom Checklist (HSCL) [38], modified for the local context with the addition of a 16th item (“feeling like I don’t care about my health”) [14, 39]. We removed the four somatic items (“feeling low in energy, slowed down,” “feeling fidgety,” “poor appetite,” and “having difficulty falling or staying asleep”) and averaged across the remaining 12 cognitive-affective items to avoid possible overlap between symptoms of depression and symptoms of HIV infection [40]. At baseline, the estimated scale reliability coefficient for the HSCL was 0.80.
Statistical Analysis
To characterize changes in internalized stigma over time on treatment, we fitted a Poisson regression model to the data, with the total IARSS score (i.e., count of items out of six) as the dependent variable and a series of binary variables indicating each three-month period of treatment. The estimates were adjusted for baseline socio-demographic and clinical variables, including age, sex, educational attainment (none, primary, or secondary), marital status (legally married or cohabiting with a primary partner vs. other), household asset wealth [41], and CD4+ T-cell count (cells/μL). We adjusted for year of cohort entry to account for potential secular trends in HIV stigmatizing attitudes. We also adjusted for time since diagnosis as a time-varying variable. Cluster-correlated robust estimates of variance were employed to correct standard errors for clustering of observations within study participants over time and for any extra-Poisson variation. A Wald-type chi-squared test was employed to test for the joint statistical significance of the time on treatment indicators. We used a non-parametric equality-of-medians test to assess for differences in baseline characteristics between participants subsequently lost to follow-up (defined as having had no contact with study trackers for a six-month period) vs. those who were not.
To test the hypothesis that the effects of ART on stigma could potentially be accounted for by changes in physical or psychological wellbeing induced by ART, we conducted ancillary analyses to investigate four putative mediators (HIV symptom burden, PHS, MHS, and HSCL) in turn. First, we fitted a linear regression model to assess for trends in the putative mediator subsequent to the initiation of ART. These four regression models adjusted for the covariates listed above, along with the time on treatment indicators. A Wald-type chi-squared test was employed to test for the joint statistical significance of the time on treatment indicators. Second, we fitted a Poisson regression model to estimate the relationship between internalized stigma and three-month lagged values of the putative mediator. These four regression models adjusted for the covariates listed above but excluded the time on treatment indicators. Third, we fitted a Poisson regression model to estimate the relationship between internalized stigma and the time on treatment indicators, adjusting for lagged values of the putative mediator. We then used a Wald-type chi-squared test to assess the degree of attenuation in the joint statistical significance of the time on treatment indicators, relative to the initial regression model that did not include the time on treatment indicators. These steps required the fitting of three regression models per putative mediator, or 12 regression models in total. Cluster-correlated robust estimates of variance were employed throughout. All analyses were conducted using the Stata/MP software package (version 12.0, StataCorp LP, College Station, Tex.).
RESULTS
The analytic sample consisted of 262 men and women who were followed for a median of 3.4 years (interquartile range [IQR], 2.5–4.1) from May 2007 through December 2011 (Table 2). The median time since diagnosis was 0.7 years (IQR, 0.3–1.8). Most were at an advanced stage of illness on presentation, with a median CD4+ T-cell count of 143 cells/μL (IQR, 93–211). The mean IARSS score was 1.7 at baseline (standard deviation, 1.8; median, 1; IQR, 0–3). Twenty-one (8.0%) participants were lost to follow-up.
Table 2.
Baseline sample characteristics (N=262)
| Variable | Median (interquartile range) or Number (percent) |
|---|---|
| Internalized AIDS-Related Stigma score | 1 (0–3) |
| Age (years) | 34 (28–40) |
| Women | 173 (66%) |
| Educational attainment | |
| None | 46 (18%) |
| Primary | 155 (59%) |
| Secondary or greater | 61 (23%) |
| Married or cohabiting with a primary partner | 120 (46%) |
| Household asset wealth score | −0.7 (−1.7 to 0.8) |
| CD4+ T-cell count (cells/μL) | 143 (93–211) |
| Time since HIV diagnosis (years) | 0.7 (0.3–1.8) |
| HIV symptom burden | 0.4 (−0.02 to 0.8) |
| Physical Health Summary score | 44 (35–52) |
| Mental Health Summary score | 43 (35–50) |
| Hopkins Symptom Checklist score | 1.3 (1.1–1.7) |
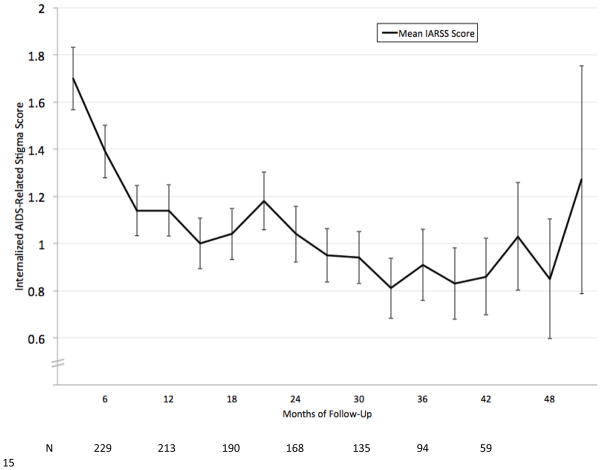
Over time on treatment, IARSS scores declined steadily, with the largest decline observed immediately after treatment initiation (Figure 1). The decline in internalized stigma over time on treatment was confirmed by Poisson regression with adjustment for baseline socio-demographic variables, baseline CD4+ T-cell count, year of cohort entry, and time since diagnosis: a Wald-type chi-squared test rejected the joint hypothesis that the time on treatment indicators were all equal to zero (χ2=28.3; p=0.03). A slight upward trend in internalized stigma was observed towards the end of follow up. Equality-of-medians tests showed that participants lost to follow-up tended to be younger (median age 30 vs. 35 years; χ2=5.6, p=0.02), but other differences in baseline characteristics were not statistically significant.
Figure 1.
Unadjusted mean change in stigma intensity over cumulative duration on HIV antiretroviral therapy
* Bars represent standard errors
We then investigated the extent to which the changes in internalized stigma were driven by changes in HIV symptom burden, physical and psychological wellbeing, and depression symptom severity. All of these variables improved over the course of follow-up: physical and psychological wellbeing improved, while HIV symptom burden and depression symptom severity declined (Table 3). The largest improvement, relative to the baseline median value, was observed for HIV symptom burden. In lagged regression models, each putative mediator had a statistically significant association with internalized stigma that was oriented in the hypothesized direction: greater PHS and MHS scores were associated with lower internalized stigma, while greater HIV symptom burden and depression symptom severity scores were associated with greater internalized stigma. When each putative mediator was added, one by one, to the regression model explaining the decline in internalized stigma over time on treatment, the joint statistical significance of the time on treatment indicators was no longer statistically significant (p-values ranged from 0.23 to 0.73).
Table 3.
Potential channels through which antiretroviral therapy may reduce the stigma of HIV †
| HIV symptom burden | Physical Health Summary score | Mental Health Summary score | |
|---|---|---|---|
| Effect of cumulative treatment duration on the putative mediator, χ2 value (P-value) | 11.9 (<0.001) | 6.4 (<0.001) | 7.2 (<0.001) |
| Association between internalized stigma and lagged values of the putative mediator, adjusted incidence rate ratio (95% confidence interval) | 1.53 (1.30–1.80) | 0.87 (0.79–0.97) ‡ | 0.79 (0.73–0.85) |
| Effect of cumulative treatment duration on internalized stigma, after adjusting for lagged values of the putative mediator, χ2 value (P-value) | 12.0 (0.68) | 18.7 (0.23) | 12.1 (0.67) |
Each cell represents an estimate derived from a separate regression model. All regression models included statistical adjustment for baseline age, sex, educational attainment, marital status, household asset wealth, CD4+ T-cell count, year of cohort entry, and time since HIV diagnosis.
Estimate rate ratio reflects a 10-point change in the value of the putative mediator.
DISCUSSION
In this analysis of data from a cohort HIV-infected persons in rural Uganda, we observed a decline in internalized stigma over time subsequent to the initiation of ART. The observed effects were markedly reduced after adjusting for factors broadly related to quality of life, including HIV symptom burden, physical and psychological wellbeing, and depression symptom severity. These results support the hypothesis that ART may reduce the stigma of HIV by improving quality of life.
Our primary finding, that there was a trend towards decreasing internalized stigma scores over time on ART, is consistent with both qualitative [20–23] and large-sample [24, 25] studies. The effect on stigma was substantive in magnitude and sustained over at least two years of treatment. The statistical significance of the observed trend in stigma scores was substantively reduced after adjusting for HIV symptom burden, physical and psychological wellbeing, and depression symptom severity. This attenuation suggests that ART may reduce stigma by improving quality of life [1–6]. Our analysis was able to exclude the possibility that the observed declines in stigma were driven by differential loss to follow-up of more stigmatized participants.
We offer several caveats to guide interpretation of our results. First, regression to the mean could potentially explain our findings if study participants initiated ART when they were feeling most stigmatized. We find this possibility unlikely given that HIV-related stigma is known to impede uptake of HIV testing [42–46], ART initiation [47–49], and regular engagement in HIV care [50]. Second, face-to-face contact with clinic providers, as well as other services that participants may have received during study follow-up, could have accounted for our findings. In general, however, patients had minimal contact with providers at the ISS Clinic, as visits were 5–10 minutes long and resource limitations prevented the three counselors on staff from providing sustained, intensive psychosocial counseling to any of the 500–800 patients who were seen at the clinic on a weekly basis. Third, our analyses of the putative mediators assumed that we have accounted for all variables that confound the relationship between the putative mediator and internalized stigma [51–53]. Fourth, the study period overlapped with a period of rapid expansion in ART scale-up efforts. The increasing availability of effective treatment could have allayed fears about HIV and diminished stigmatizing attitudes towards HIV-infected persons within the general population [8, 9], which in turn could have reduced internalized stigma among HIV-infected persons. We adjusted for year of cohort entry, however, and did not observe a secular trend in internalized stigma scores among participants at cohort entry. Fifth, a slight upward trend in IARSS scores was observed towards the end of follow-up. We have limited confidence in these estimates given the large standard errors and small sample sizes, but the long-term effects of ART on HIV-related stigma in resource-limited settings are unknown and may be a fruitful area for future research.
Although our study demonstrated that internalized stigma declined over time on treatment, the mean IARSS scores did not trend to zero. Most approaches to stigma reduction have emphasized psycho-educational interventions such as information provision and counseling, which have had limited success [54]. That treatment did not completely eliminate internalized stigma among our study participants suggests there was a floor effect. This may be due to the inability of ART alone to fully reverse the economic and physical decline, and concomitant household asset depletion [55], that have typically occurred by the time people enter treatment [56, 57]. While scale-up of HIV treatment programs can and should be thought of as making an important contribution to reducing HIV-related stigma by targeting the physical decline brought about by the illness, we hypothesize that directly addressing other people’s underlying resource-based fears and directly targeting the economic decline brought about by HIV may play a critical role in reducing the stigma of HIV/AIDS [19, 58–60].
Acknowledgments
We thank the Uganda AIDS Rural Treatment Outcomes (UARTO) study participants who made this study possible by sharing their experiences; Nozmo F.B. Mukiibi for his contributions to study design and implementation; and Annet Kembabazi and Annet Kawuma for providing study coordination and administrative support. While these individuals are acknowledged for their assistance, no endorsement of manuscript contents or conclusions should be inferred. A preliminary version of this analysis was presented in part at the 20th Conference on Retroviruses and Opportunistic Infections, Atlanta, Georgia, USA, March 4, 2013.
SOURCE OF FUNDING: This study was funded by U.S. National Institutes of Health R01 MH-054907, K23 MH-079713, K23 MH-079713-03S1, and P30 AI-027763. Additionally, the authors acknowledge the following sources of salary support: K23 MH-096620 (Tsai), K24 MH-087227 (Bangsberg), K23 MH-087228 (Haberer), and the Burke Family Foundation (Weiser).
References
- 1.Weiser SD, Gupta R, Tsai AC, Frongillo EA, Grede N, Kumbakumba E, et al. Changes in food insecurity, nutritional status, and physical health status after antiretroviral therapy initiation in rural Uganda. J Acquir Immune Defic Syndr. 2012;61(2):179–86. doi: 10.1097/QAI.0b013e318261f064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Palar K, Wagner G, Ghosh-Dastidar B, Mugyenyi P. Role of antiretroviral therapy in improving food security among patients initiating HIV treatment and care in Uganda. AIDS. 2012;26(18):2375–81. doi: 10.1097/QAD.0b013e328359b809. [DOI] [PubMed] [Google Scholar]
- 3.Wagner GJ, Ghosh-Dastidar B, Garnett J, Kityo C, Mugyenyi P. Impact of HIV antiretroviral therapy on depression and mental health among clients With HIV in Uganda. Psychosom Med. 2012;74(9):883–90. doi: 10.1097/PSY.0b013e31826629db. [DOI] [PubMed] [Google Scholar]
- 4.Rabkin JG, Ferrando SJ, Lin SH, Sewell M, McElhiney M. Psychological effects of HAART: a 2-year study. Psychosom Med. 2000;62(3):413–22. doi: 10.1097/00006842-200005000-00015. [DOI] [PubMed] [Google Scholar]
- 5.Brent RJ. The effects of HIV medications on the quality of life of older adults in New York City. Health Econ. 2012;21(8):967–76. doi: 10.1002/hec.1774. [DOI] [PubMed] [Google Scholar]
- 6.Low-Beer S, Chan K, Yip B, Wood E, Montaner JS, O’Shaughnessy MV, et al. Depressive symptoms decline among persons on HIV protease inhibitors. J Acquir Immune Defic Syndr. 2000;23(4):295–301. doi: 10.1097/00126334-200004010-00003. [DOI] [PubMed] [Google Scholar]
- 7.Thirumurthy H, Zivin JG, Goldstein M. The economic impact of AIDS treatment: labor supply in western Kenya. J Hum Resources. 2008;43(3):511–52. [PMC free article] [PubMed] [Google Scholar]
- 8.Wolfe WR, Weiser SD, Leiter K, Steward WT, Percy-de Korte F, Phaladze N, et al. The impact of universal access to antiretroviral therapy on HIV stigma in Botswana. Am J Public Health. 2008;98(10):1865–71. doi: 10.2105/AJPH.2007.122044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Baranov V, Bennett D, Kohler H-P. Population Studies Center Working Paper Series, PSC 12-08. Philadelphia: University of Pennsylvania; 2012. The indirect impact of antiretroviral therapy. [Google Scholar]
- 10.Khandelwal S, Avode G, Baingana F, Conde B, Cruz M, Deva P, et al. Mental and neurological health research priorities setting in developing countries. Soc Psychiatry Psychiatr Epidemiol. 2010;45(4):487–95. doi: 10.1007/s00127-009-0089-2. [DOI] [PubMed] [Google Scholar]
- 11.Adewuya AO, Afolabi MO, Ola BA, Ogundele OA, Ajibare AO, Oladipo BF, et al. Post-traumatic stress disorder (PTSD) after stigma related events in HIV infected individuals in Nigeria. Soc Psychiatry Psychiatr Epidemiol. 2009;44(9):761–6. doi: 10.1007/s00127-009-0493-7. [DOI] [PubMed] [Google Scholar]
- 12.Jones EE, Farina A, Hastorf AH, Markus H, Miller DT, Scott RA. Social stigma: the psychology of marked relationships. New York: W.H. Freeman & Company; 1984. [Google Scholar]
- 13.Simbayi LC, Kalichman S, Strebel A, Cloete A, Henda N, Mqeketo A. Internalized stigma, discrimination, and depression among men and women living with HIV/AIDS in Cape Town, South Africa. Soc Sci Med. 2007;64(9):1823–31. doi: 10.1016/j.socscimed.2007.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tsai AC, Bangsberg DR, Frongillo EA, Hunt PW, Muzoora C, Martin JN, et al. Food insecurity, depression and the modifying role of social support among people living with HIV/AIDS in rural Uganda. Soc Sci Med. 2012;74(12):2012–9. doi: 10.1016/j.socscimed.2012.02.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Norman A, Chopra M, Kadiyala S. Factors related to HIV disclosure in 2 South African communities. Am J Public Health. 2007;97(10):1775–81. doi: 10.2105/AJPH.2005.082511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Boyer S, Clerc I, Bonono C-R, Marcellin F, Bile P-C, Ventelou B. Non-adherence to antiretroviral treatment and unplanned treatment interruption among people living with HIV/AIDS in Cameroon: individual and healthcare supply-related factors. Soc Sci Med. 2011;72(8):1383–92. doi: 10.1016/j.socscimed.2011.02.030. [DOI] [PubMed] [Google Scholar]
- 17.Farmer P, Leandre F, Mukherjee JS, Claude M, Nevil P, Smith-Fawzi MC, et al. Community-based approaches to HIV treatment in resource-poor settings. Lancet. 2001;358(9279):404–9. doi: 10.1016/s0140-6736(01)05550-7. [DOI] [PubMed] [Google Scholar]
- 18.Farmer P, Leandre F, Mukherjee J, Gupta R, Tarter L, Kim JY. Community-based treatment of advanced HIV disease: introducing DOT-HAART (directly observed therapy with highly active antiretroviral therapy) Bull World Health Organ. 2001;79(12):1145–51. [PMC free article] [PubMed] [Google Scholar]
- 19.Castro A, Farmer P. Understanding and addressing AIDS-related stigma: from anthropological theory to clinical practice in Haiti. Am J Public Health. 2005;95(1):53–9. doi: 10.2105/AJPH.2003.028563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gilbert L, Walker L. ‘My biggest fear was that people would reject me once they knew my status...’: stigma as experienced by patients in an HIV/AIDS clinic in Johannesburg, South Africa. Health Soc Care Community. 2010;18(2):139–46. doi: 10.1111/j.1365-2524.2009.00881.x. [DOI] [PubMed] [Google Scholar]
- 21.Zuch M, Lurie M. ‘A virus and nothing else’: the effect of ART on HIV-related stigma in rural South Africa. AIDS Behav. 2012;16(3):564–70. doi: 10.1007/s10461-011-0089-6. [DOI] [PubMed] [Google Scholar]
- 22.Gilbert L, Walker L. “They (ARVs) are my life, without them I’m nothing”--experiences of patients attending a HIV/AIDS clinic in Johannesburg, South Africa. Health Place. 2009;15(4):1123–9. doi: 10.1016/j.healthplace.2009.06.006. [DOI] [PubMed] [Google Scholar]
- 23.Campbell C, Skovdal M, Madanhire C, Mugurungi O, Gregson S, Nyamukapa C. “We, the AIDS people. . .”: how antiretroviral therapy enables Zimbabweans living with HIV/AIDS to cope with stigma. Am J Public Health. 2011;101(6):1004–10. doi: 10.2105/AJPH.2010.202838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kaai S, Bullock S, Sarna A, Chersich M, Luchters S, Geibel S, et al. Perceived stigma among patients receiving antiretroviral treatment: a prospective randomised trial comparing an m-DOT strategy with standard-of-care in Kenya. J Soc Aspects HIV/AIDS. 2010;7(2):62–70. doi: 10.1080/17290376.2010.9724958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Makoae LN, Portillo CJ, Uys LR, Dlamini PS, Greeff M, Chirwa M, et al. The impact of taking or not taking ARVs on HIV stigma as reported by persons living with HIV infection in five African countries. AIDS Care. 2009;21(11):1357–62. doi: 10.1080/09540120902862576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Munoz M, Finnegan K, Zeladita J, Caldas A, Sanchez E, Callacna M, et al. Community-based DOT-HAART accompaniment in an urban resource-poor setting. AIDS Behav. 2010;14(3):721–30. doi: 10.1007/s10461-009-9559-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pearson CR, Micek MA, Pfeiffer J, Montoya P, Matediane E, Jonasse T, et al. One year after ART initiation: psychosocial factors associated with stigma among HIV-positive Mozambicans. AIDS Behav. 2009;13(6):1189–96. doi: 10.1007/s10461-009-9596-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kinyanda E, Woodburn P, Tugumisirize J, Kagugube J, Ndyanabangi S, Patel V. Poverty, life events and the risk for depression in Uganda. Soc Psychiatry Psychiatr Epidemiol. 2011;46(1):35–44. doi: 10.1007/s00127-009-0164-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ovuga E, Boardman J, Wasserman D. The prevalence of depression in two districts of Uganda. Soc Psychiatry Psychiatr Epidemiol. 2005;40(6):439–45. doi: 10.1007/s00127-005-0915-0. [DOI] [PubMed] [Google Scholar]
- 30.Wilk CM, Bolton P. Local perceptions of the mental health effects of the Uganda acquired immunodeficiency syndrome epidemic. J Nerv Ment Dis. 2002;190(6):394–7. doi: 10.1097/00005053-200206000-00008. [DOI] [PubMed] [Google Scholar]
- 31.Geng EH, Bwana MB, Kabakyenga J, Muyindike W, Emenyonu NI, Musinguzi N, et al. Diminishing availability of publicly funded slots for antiretroviral initiation among HIV-infected ART-eligible patients in Uganda. PLoS One. 2010;5(11):e14098. doi: 10.1371/journal.pone.0014098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Siedner MJ, Lankowski A, Haberer JE, Kembabazi A, Emenyonu N, Tsai AC, et al. Rethinking the “pre” in pre-therapy counseling: no benefit of additional visits prior to therapy on adherence or viremia in Ugandans initiating ARVs. PLoS One. 2012;7(6):e39894. doi: 10.1371/journal.pone.0039894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kalichman SC, Simbayi LC, Cloete A, Mthembu PP, Mkhonta RN, Ginindza T. Measuring AIDS stigmas in people living with HIV/AIDS: the Internalized AIDS-Related Stigma Scale. AIDS Care. 2009;21(1):87–93. doi: 10.1080/09540120802032627. [DOI] [PubMed] [Google Scholar]
- 34.Tsai AC, Weiser SD, Steward WT, Mukiibi NF, Kawuma A, Kembabazi A, et al. Evidence for the reliability and validity of the internalized AIDS-related stigma scale in rural Uganda. AIDS Behav. 2013;17(1):427–33. doi: 10.1007/s10461-012-0281-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tsai AC, Bangsberg DR, Kegeles SM, Katz IT, Haberer JE, Muzoora C, et al. Internalized stigma, social distance, and disclosure of HIV seropositivity in rural Uganda. Ann Behav Med. 2013 doi: 10.1007/s12160-013-9514-6. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kling JR, Liebman JB, Katz LF. Experimental analysis of neighborhood effects. Econometrica. 2007;75(1):83–119. [Google Scholar]
- 37.Wu AW, Rubin HR, Mathews WC, Ware JE, Jr, Brysk LT, Hardy WD, et al. A health status questionnaire using 30 items from the Medical Outcomes Study. Preliminary validation in persons with early HIV infection. Med Care. 1991;29(8):786–98. doi: 10.1097/00005650-199108000-00011. [DOI] [PubMed] [Google Scholar]
- 38.Derogatis LR, Lipman RS, Rickels K, Uhlenhuth EH, Covi L. The Hopkins Symptom Checklist (HSCL): a self-report symptom inventory. Behav Sci. 1974;19(1):1–15. doi: 10.1002/bs.3830190102. [DOI] [PubMed] [Google Scholar]
- 39.Bolton P. Cross-cultural validity and reliability testing of a standard psychiatric assessment instrument without a gold standard. J Nerv Ment Dis. 2001;189(4):238–42. doi: 10.1097/00005053-200104000-00005. [DOI] [PubMed] [Google Scholar]
- 40.Kalichman SC, Rompa D, Cage M. Distinguishing between overlapping somatic symptoms of depression and HIV disease in people living with HIV-AIDS. J Nerv Ment Dis. 2000;188(10):662–70. doi: 10.1097/00005053-200010000-00004. [DOI] [PubMed] [Google Scholar]
- 41.Filmer D, Pritchett LH. Estimating wealth effects without expenditure data -- or tears: an application to educational enrollments in states of India. Demography. 2001;38(1):115–32. doi: 10.1353/dem.2001.0003. [DOI] [PubMed] [Google Scholar]
- 42.Young SD, Hlavka Z, Modiba P, Gray G, Van Rooyen H, Richter L, et al. HIV-related stigma, social norms, and HIV testing in Soweto and Vulindlela, South Africa: National Institutes of Mental Health Project Accept (HPTN 043) J Acquir Immune Defic Syndr. 2010;55(5):620–4. doi: 10.1097/QAI.0b013e3181fc6429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Weiser SD, Heisler M, Leiter K, Percy-de Korte F, Tlou S, DeMonner S, et al. Routine HIV testing in Botswana: a population-based study on attitudes, practices, and human rights concerns. PLoS Med. 2006;3(7):e261. doi: 10.1371/journal.pmed.0030261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Musheke M, Ntalasha H, Gari S, McKenzie O, Bond V, Martin-Hilber A, et al. A systematic review of qualitative findings on factors enabling and deterring uptake of HIV testing in sub-Saharan Africa. BMC Pub Health. 2013;13:220. doi: 10.1186/1471-2458-13-220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Musheke M, Bond V, Merten S. Deterrents to HIV-patient initiation of antiretroviral therapy in urban Lusaka, Zambia: a qualitative study. AIDS Patient Care STDs. 2013;27(4):231–41. doi: 10.1089/apc.2012.0341. [DOI] [PubMed] [Google Scholar]
- 46.Turan JM, Bukusi EA, Onono M, Holzemer WL, Miller S, Cohen CR. HIV/AIDS stigma and refusal of HIV testing among pregnant women in rural Kenya: results from the MAMAS Study. AIDS Behav. 2011;15(6):1111–20. doi: 10.1007/s10461-010-9798-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Pollini RA, Blanco E, Crump C, Zuniga ML. A community-based study of barriers to HIV care initiation. AIDS Patient Care STDS. 2011;25(10):601–9. doi: 10.1089/apc.2010.0390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kigozi IM, Dobkin LM, Martin JN, Geng EH, Muyindike W, Emenyonu NI, et al. Late-disease stage at presentation to an HIV clinic in the era of free antiretroviral therapy in Sub-Saharan Africa. J Acquir Immune Defic Syndr. 2009;52(2):280–9. doi: 10.1097/QAI.0b013e3181ab6eab. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Muhamadi L, Nsabagasani X, Tumwesigye MN, Wabwire-Mangen F, Ekstrom AM, Peterson S, et al. Inadequate pre-antiretroviral care, stock-out of antiretroviral drugs and stigma: policy challenges/bottlenecks to the new WHO recommendations for earlier initiation of antiretroviral therapy (CD<350 cells/microL) in eastern Uganda. Health Policy. 2010;97(2–3):187–94. doi: 10.1016/j.healthpol.2010.06.003. [DOI] [PubMed] [Google Scholar]
- 50.Sayles JN, Wong MD, Kinsler JJ, Martins D, Cunningham WE. The association of stigma with self-reported access to medical care and antiretroviral therapy adherence in persons living with HIV/AIDS. J Gen Intern Med. 2009;24(10):1101–8. doi: 10.1007/s11606-009-1068-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Judd CM, Kenny DA. Process analysis: estimating mediation in treatment evaluations. Eval Rev. 1981;5(5):602–19. [Google Scholar]
- 52.James LR, Brett JM. Mediators, moderators, and tests for mediation. J Appl Psychol. 1984;69(2):307–21. [Google Scholar]
- 53.Valeri L, VanderWeele TJ. Mediation analysis allowing for exposure-mediator interactions and causal interpretation: theoretical assumptions and implementation with SAS and SPSS macros. Psychol Methods. 2013 doi: 10.1037/a0031034. in press. Epub 2013 Feb 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sengupta S, Banks B, Jonas D, Miles MS, Smith GC. HIV interventions to reduce HIV/AIDS stigma: a systematic review. AIDS Behav. 2011;15(6):1075–87. doi: 10.1007/s10461-010-9847-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Yamano T, Jayne TS. Measuring the impact of working-age adult mortality on small-scale farm households in Kenya. World Dev. 2004;32(1):91–119. [Google Scholar]
- 56.Wagner G, Ryan G, Huynh A, Kityo C, Mugyenyi P. A qualitative analysis of the economic impact of HIV and antiretroviral therapy on individuals and households in Uganda. AIDS Patient Care STDS. 2009;23(9):793–8. doi: 10.1089/apc.2009.0028. [DOI] [PubMed] [Google Scholar]
- 57.Samuels FA, Rutenberg N. “Health regains but livelihoods lag”: findings from a study with people on ART in Zambia and Kenya. AIDS Care. 2011;23(6):748–54. doi: 10.1080/09540121.2010.532535. [DOI] [PubMed] [Google Scholar]
- 58.Heijnders M, Van Der Meij S. The fight against stigma: an overview of stigma-reduction strategies and interventions. Psychol Health Med. 2006;11(3):353–63. doi: 10.1080/13548500600595327. [DOI] [PubMed] [Google Scholar]
- 59.Goudge J, Ngoma B, Manderson L, Schneider H. Stigma, identity and resistance among people living with HIV in South Africa. SAHARA J. 2009;6(3):94–104. doi: 10.1080/17290376.2009.9724937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Reidpath DD, Chan KY, Gifford SM, Allotey P. ‘He hath the French pox’: stigma, social value and social exclusion. Sociol Health Illn. 2005;27(4):468–89. doi: 10.1111/j.1467-9566.2005.00452.x. [DOI] [PubMed] [Google Scholar]