Abstract
Importance
While many persons at advanced ages live independently and are free of disability, we know little about how likely older people are to be disabled in the basic activities of daily that are necessary for independent living as they enter the last years of life.
Objective
To determine national estimates of disability during the last two years of life.
Design
Prospective cohort study.
Setting
A nationally representative study of older adults
Participants
Participants ages 50+ who died in the Health and Retirement Study between 1995 and 2010. Each participant was interviewed once at a varying time point in the last 24 months of life. We used these interviews to calculate national estimates of the prevalence of disability across the two years prior to death. We modeled the prevalence of disability in the two years prior to death for groups defined by age at death and gender.
Main Outcome Measure
Disability was defined as need for help with one of following activities of daily living: dressing, bathing, eating, transferring, walking across the room, and toileting.
Results
There were 8,232 decedents (mean age at death 79, 52% women). The prevalence of disability rose from 28% (95% CI, 24-31%) 2 years before death to 56% (52-60%) in the last month of life. Those who died at the oldest ages were much more likely to have disability 2 years before death (ages 50-69, 15%; 70-79, 21%; 80-89, 31%; 90+, 50%; p for trend <.0001). Disability was more common in women 2 years before death (32%, 28-36%) then men (21%, 18-24%,p<.0001), even after adjustment for higher age at death.
Conclusions
Those who live to an older age are likely to be disabled, and thus in need of caregiving assistance, many months or years prior to death. Women have a substantially longer period of end-of-life disability than men.
Introduction
The population of US adults over age 85 is expected to triple, from 5.4 million to 19 million between 2008 and 2050.1 This explosion of our nations' older adult population will occur in the context of a health care system that is primarily focused on disease management, and is unprepared to manage the patient and caregiver needs imposed by disability.2 It also occurs in the context of a culture where many persons live in both fear and denial of the disablement that occurs with aging.3 The public is bombarded with messages that frailty and disability are not inevitable, and the most popular medical personalities assail the public with health messages that healthy living will lead to a long life free of disability to the end of life.4
Many people do live into their eighth and ninth decades free of disability and able to live independently. However, it is also the case that with increasing age, the end of life course is increasingly likely to be marked by disability.5-8 Thus, it is likely that most well-functioning older adults and their families will need to be prepared for a period of disability as they continue to age and approach the last years of life. Preparation for this period of disability may be particularly important for older women who are much more likely to be widowed and lack a spousal caregiver.9 However, there is surprisingly little national data on a person's likelihood of being disabled over the last months of life. Further, we lack national estimates of how end of life disability varies according to age at death, gender, and socio-economic status. These knowledge gaps limit our ability to plan for supportive services for disabled older adults in their last years of life and target services to the most vulnerable groups.
We therefore conducted a study of the nationally representative Health and Retirement Study, to describe the prevalence of disability and functional problems during the last two years of life. To help target services to the most vulnerable to disability, we present findings for key groups, including the oldest adults and women.
Methods
Subjects
The HRS is an ongoing nationally representative longitudinal study of changes in health and wealth in persons over age 50, funded by the National Institute on Aging. The HRS uses a national area probability sample of U.S. households. Subjects are interviewed every two years. Enrollment began in 1992 and additional subjects are added every 6 years so that the study remains representative of the U.S. population over age 50. Follow up rates are very high (85-93%), and date of death is determined for nearly all subjects (99%).10 Each subject is interviewed once every two years. Thus, generally, each HRS subject is interviewed once in the last 2 years of life, and the timing of this end of life interview is random, based on the time between the last interview of life and date of death. The 1-hour HRS interviews are conducted primarily by phone, but face-to-face interviews are conducted for most participants who are 80 years or older, too ill to participate in the telephone interview, or unable to access a phone. For subjects who are too ill or cognitively impaired to conduct an interview, proxy interviews are conducted with subjects' next-of-kin.
In total, 28,390 subjects were interviewed between January 1995 and December 2010; of these, 10,250 died.. We excluded 1,989 subjects who had their last interview prior to the last two years of life (720 days of life, one month was defined as a 30 day increment), and 29 subjects who had implausible interview dates relative to their date of death. Our final sample consisted of 8,232 decedents. We compared the 1,989 subjects with interviews prior to the last 2 years of life to subjects in our final sample as described below.
This study was approved by the Committee on Human Subjects Research at the University of California, San Francisco.
Measures
Our primary analysis described the prevalence of older adults who have disability in activities of daily living (ADL) during the last two years of life. The need for help with these measures generally means the person will need assistance from a family member, friend, or formal long term care services.11,12 Measures included 6 ADL: dressing, bathing, eating, transferring in or out of bed, walking across the room, and toileting. Subjects were first asked if they have difficulty with each ADL. Subjects reporting difficulty were then asked if they required assistance for that ADL; those who responded “yes” were considered to have disability. Subjects who reported the need for assistance with 3 or more ADL were considered severely disabled.6 We additionally report the prevalence of selected higher order mobility and functional problems,11 defined as difficulty or inability to: walk several blocks, walk one block, walk up several flights of stairs, walk up one flight of stairs, take medications, and manage finances.
We evaluated predictors of disability that had been shown to correlate with disability in previous studies, including: sociodemographic factors (age, gender, race/ethnicity, educational attainment, household net worth); chronic conditions (high blood pressure, heart disease, diabetes, cancer, cognitive impairment, stroke, lung disease, arthritis); and health events (hospitalizations or falls within the last two years).5-7 We used household net worth at enrollment because we were concerned that household net worth at the last interview prior to death might be confounded – as individuals become disabled and consider nursing home placement, they often “spend down” their assets to qualify for Medicaid's long term care benefit.13
Analysis
HRS subjects reported disability at a range of time points during the last two years of life. We first use these reports to present the unadjusted monthly prevalence of disability during the last two years of life. We then used these reports to model the probability that a subject would be disabled across the last two years of life. We used HRS survey weights to calculate national estimates of the prevalence of disability during the last two years of life. To construct these estimates we modeled the prevalence of disability using a restricted cubic spline with four knots placed at standard cutpoints (Harrell's recommended cutpoints14), in this case 23, 17, 10, and 2 months prior to death. To assess the robustness of our results to the number and location of the knots, a variety of alternative locations and numbers of knots were also examined. Results were extremely similar for a wide variety of knot choices. We found that the restricted cubic spline models were superior to the linear model in all cases using Wald tests. Goodness of fit for the logistic regression models was verified by a modified Hosmer-Lemeshow approach.15,16 Nonsignificant values suggested a good fit for all models. The c-statistic ranged from 0.71-0.77 across models, suggesting very good model discrimination.
We used the spline model in a multivariable regression to estimate the probability of disability during the last two years of life for relevant subgroups. Model covariates included age at death, gender, race/ethnicity, educational attainment, and household net worth. Probabilities were determined for subgroups holding other covariates fixed at their population means. Because differences by age and gender were of central interest, we additionally present model results stratified by age at death and gender.
We conducted several additional analyses to place our findings in context and test the robustness of our findings. First, we examined time trends in disability for the most recent 10 year period, 2000-2010. Second, to contrast disability among patients who are dying with disability rates in the general living population of older adults, we report rates of disability by age among the entire 2010 HRS cohort (14,436 subjects). Third, we were concerned that the 1,989 subjects with no interview during the last 2 years of life may have differed systematically from interviewed subjects in our sample. Therefore we compare these groups by age, gender, race/ethnicity, and disability during the last 3 months of life as described by next of kin in after-death interviews.
All analyses used survey weights provided by the HRS to account for the complex survey design and unequal probability of subject selection.17 All analyses were conducted in Stata 12 (College Station, Texas).
Results
Characteristics of the subjects are described in Table 1. The mean age at the time of death was 81 for women (SD 11) and 77 for men (SD 11). Overall, 52% were female. Twenty-two percent of decedent women were 90 and older, 11% of decedent men were 90 and older. Differences between subjects interviewed in the last year of life and subjects interviewed one to two years prior to death were not significant for gender, race/ethnicity, educational attainment or net worth; subjects interviewed one to two years prior to death were one year younger at death than those interviewed in the last year of life (p<.001).
Table 1. Characteristics of Subjects*.
| Characteristics | Overall (N=8232) | Men (n=3877) | Women (n=4355) |
|---|---|---|---|
| Demographics | |||
|
| |||
| Age at death, yr | |||
| mean (SD) | 79 (11) | 77 (11) | 81 (11) |
| 50 – 69 yr, % | 22 | 27 | 17 |
| 70 – 79 yr, % | 27 | 30 | 24 |
| 80 – 89 yr, % | 35 | 32 | 37 |
| ≥ 90 yr, % | 16 | 11 | 22 |
|
| |||
| Race/Ethnicity, % | |||
| Non-Hispanic White | 83 | 84 | 83 |
| Non-Hispanic Black | 11 | 10 | 11 |
| Hispanic | 5 | 5 | 4 |
| Other | 1 | 1 | 1 |
|
| |||
| Married/Partnered, % | 43 | 63 | 26 |
|
| |||
| Social Factors | |||
|
| |||
| Education < high school, % | 42 | 41 | 43 |
|
| |||
| Household net worth, $ | |||
| Median (IQR) | 78000 | 93711 | 66000 |
| (17010,192600) | (25640, 231000) | (10005, 159500) | |
| < $17010, % | 25 | 21 | 28 |
| $17010 – <78000, % | 25 | 24 | 26 |
| $78000 – <192600, % | 25 | 25 | 25 |
| ≥ $192600, % | 25 | 30 | 20 |
|
| |||
| The last interview was a proxy, % | 27 | 24 | 29 |
|
| |||
| Nursing home resident at the last interview, % | 16 | 10 | 22 |
|
| |||
| Recent hospitalization, % | 55 | 54 | 56 |
|
| |||
| Recent fall, %+ | 48 | 46 | 49 |
|
| |||
| Chronic conditions | |||
| High blood pressure | 64 | 59 | 68 |
| Heart disease | 48 | 50 | 46 |
| Diabetes | 27 | 29 | 24 |
| Cancer | 26 | 27 | 25 |
| Cognitive impairment | 26 | 21 | 30 |
| Stroke | 23 | 22 | 25 |
| Lung disease | 22 | 23 | 21 |
| Arthritis | 65 | 58 | 71 |
Reported values incorporate survey weights to account for the complex survey design.
Questions about falling in last two years were asked for respondents 65 years or older in some survey years, but not all. Among the 8232 decedents in the study, 958 decedents were not asked the falls question in the interview prior to death.
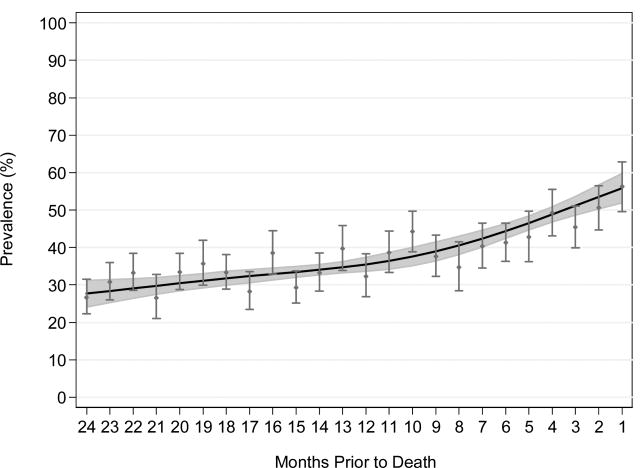
Unadjusted and modeled adjusted findings were similar (Figure 1). Because of slight differences between subjects interviewed across the two years before death, and to leverage the power of modeling, we focus on the adjusted findings for the remainder of the results.
Figure 1. Prevalence of Unadjusted and Adjusted ADL Disability during the Last Two Years of Life.
Circles represent the mean monthly prevalence of disability in an activity of daily living (ADL) (bathing, getting out of bed, dressing, eating, walking across a room, and using the toilet). Bars represent 95% confidence intervals. The black line represents ADL disability modeled as a spline with knots at 23, 17, 10, and 2 months prior to death, adjusted for age at death, gender, race/ethnicity, educational attainment, and household net worth. Grey shading above and below the line represents modeled 95% confidence intervals.
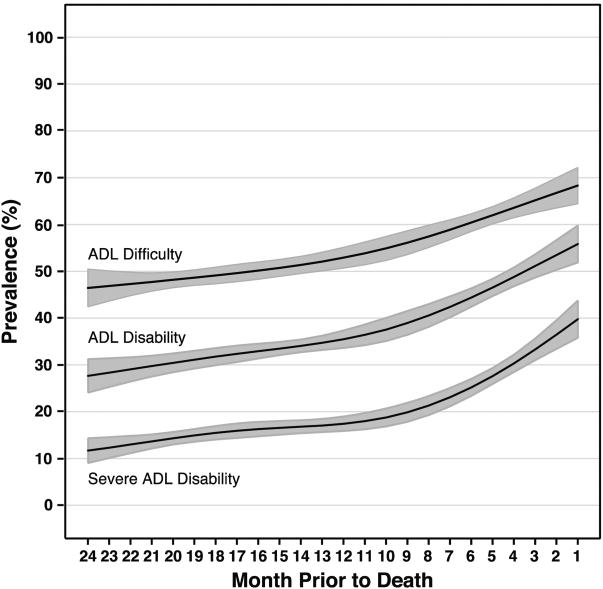
The prevalence of disability (requiring assistance with ADL) rose during the last 2 years of life (Figures 1-3, Table 2). Twenty four months prior to death, 46% (95% CI, 42-50%) had an ADL difficulty, 28% (95% CI, 24-31%) had ADL disability, and 12% had severe ADL disability (95% CI, 9-14%), rising to 68% (95% CI, 64-72%), 56% (95% CI, 52-60%), and 40% (95% CI, 36-44%) in the last month of life (Figure 2). The rise in prevalence was steeper for severe ADL disability than for ADL difficulty, with the steepest increase in prevalence of severe disability occuring in the last 6 months of life. Examining the prevalence of disability by individual ADL revealed a similar pattern of increasing prevalence during the months before death, with highest rates for bathing disability and dressing disability (eFigure 1).
Figure 3. Prevalence of ADL Disability by Age and Gender during the Last Two Years of Life.
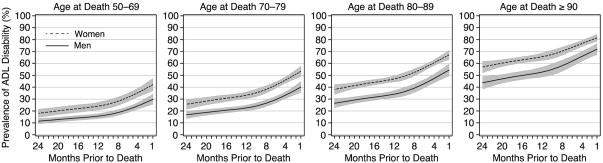
Prevalence of disability modeled as a spline with knots at 23, 17, 10, and 2 months prior to death, stratified by age at death and gender, adjusted for race/ethnicity, educational attainment, and household net worth.
Table 2. Prevalence of ADL Disability during the Last Two Years of Life across Subgroups*.
| Predictors | Predicted Prevalence: 24 Months prior to Death | Predicted Prevalence: 12 Months prior to Death | Predicted Prevalence: 6 Months prior to Death | Predicted Prevalence: 1 Month prior to Death | p Value+ |
|---|---|---|---|---|---|
| % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | ||
| 28 (24 - 31) | 36 (34 - 37) | 44 (42 - 46) | 56 (52 - 60) | ||
| Demographics/Social Factors | |||||
| Age at death, yr | |||||
| 50 – 69 | 14 (12 - 17) | 19 (17 - 22) | 26 (23 - 28) | 35 (31 - 40) | Ref. |
| 70 – 79 | 21 (17 - 24) | 27 (25 - 30) | 35 (33 - 38) | 46 (42 - 51) | <0.001 |
| 80 – 89 | 32 (28 - 35) | 40 (38 - 42) | 49 (47 - 52) | 61 (56 - 65) | <0.001 |
| ≥ 90 | 50 (45 - 55) | 59 (56 - 62) | 68 (64 - 71) | 77 (73 - 80) | <0.001 |
| Gender | |||||
| Men | 21 (18 - 25) | 28 (26 - 30) | 36 (34 - 39) | 47 (43 - 52) | Ref. |
| Women | 32 (28 - 36) | 40 (38 - 42) | 49 (47 - 51) | 61 (57 - 64) | <0.001 |
| Race/Ethnicity | |||||
| Non-Hispanic White | 26 (23 - 29) | 34 (32 - 36) | 42 (40 - 44) | 54 (50 - 58) | Ref. |
| Non-Hispanic Black | 29 (24 - 34) | 37 (33 - 41) | 46 (42 - 51) | 58 (53 - 63) | 0.07 |
| Hispanic | 30 (23 - 36) | 38 (32 - 43) | 47 (41 - 52) | 58 (52 - 65) | 0.13 |
| Education | |||||
| ≥ High school | 25 (21 - 29) | 32 (30 - 34) | 41 (38 - 43) | 52 (48 - 56) | Ref. |
| < High school | 29 (26 - 32) | 37 (34 - 40) | 46 (43 - 49) | 58 (53 - 62) | 0.001 |
| Net worth at enrollment | |||||
| <$17010 | 32 (28 - 35) | 40 (37 - 43) | 49 (46 - 52) | 60 (56 - 65) | <0.001 |
| $17010 – <78000 | 27 (22 - 32) | 35 (32 - 38) | 44 (41 - 47) | 55 (50 - 60) | 0.03 |
| $78000 – <192600 | 25 (21 - 28) | 32 (29 - 35) | 40 (38 - 43) | 52 (47 - 56) | 0.36 |
| ≥ $192600 | 23 (19 - 27) | 30 (27 - 33) | 39 (35 - 42) | 50 (46 - 54) | Ref. |
| Married/Partnered | |||||
| Yes | 29 (25 - 32) | 37 (34 - 40) | 46 (43 - 49) | 58 (53 - 62) | Ref. |
| No | 25 (21 - 28) | 32 (30 - 34) | 41 (38 - 43) | 52 (48 - 56) | 0.003 |
| Chronic Conditions | |||||
| High blood pressure | |||||
| Yes | 28 (25 - 32) | 36 (34 - 39) | 45 (43 - 48) | 57 (53 - 61) | <0.001 |
| No | 23 (20 - 27) | 30 (28 - 33) | 39 (36 - 41) | 50 (46 - 55) | Ref. |
| Heart disease | |||||
| Yes | 31 (27 - 35) | 39 (37 - 42) | 48 (46 - 51) | 59 (55 - 64) | <0.001 |
| No | 23 (19 - 26) | 30 (27 - 32) | 38 (35 - 40) | 49 (45 - 53) | Ref. |
| Diabetes | |||||
| Yes | 34 (29 - 38) | 42 (39 - 45) | 51 (48 - 54) | 63 (58 - 67) | <0.001 |
| No | 24 (21 - 27) | 31 (29 - 33) | 40 (38 - 42) | 51 (47 - 55) | Ref. |
| Cancer | |||||
| Yes | 23 (20 - 27) | 31 (28 - 34) | 39 (36 - 43) | 51 (46 - 56) | 0.007 |
| No | 27 (24 - 31) | 35 (33 - 37) | 44 (42 - 46) | 56 (52 - 60) | Ref. |
| Cognitive impairment | |||||
| Yes | 59 (54 - 65) | 67 (64 - 70) | 74 (71 - 76) | 81 (78 - 83) | <0.001 |
| No | 19 (16 - 22) | 25 (24 - 27) | 32 (30 - 33) | 41 (36 - 45) | Ref. |
| Stroke | |||||
| Yes | 49 (43 - 54) | 58 (55 - 61) | 67 (64 - 69) | 76 (72 - 80) | <0.001 |
| No | 20 (17 - 23) | 27 (25 - 29) | 35 (33 - 37) | 46 (42 - 50) | Ref. |
| Lung disease | |||||
| Yes | 31 (27 - 36) | 40 (37 - 43) | 49 (46 - 52) | 60 (56 - 65) | <0.001 |
| No | 25 (22 - 28) | 33 (31 - 35) | 41 (39 - 43) | 52 (48 - 56) | Ref. |
| Arthritis | |||||
| Yes | 29 (26 - 33) | 38 (36 - 40) | 47 (44 - 49) | 58 (54 - 62) | <0.001 |
| No | 21 (18 - 24) | 28 (25 - 30) | 35 (33 - 38) | 46 (42 - 50) | Ref. |
| Recent hospitalization | |||||
| Yes | 35 (31 - 40) | 44 (42 - 47) | 52 (50 - 55) | 62 (59 - 66) | <0.001 |
| No | 17 (14 - 20) | 23 (21 - 25) | 29 (27 - 32) | 38 (34 - 42) | Ref. |
| Recent fall± | |||||
| Yes | 36 (31 - 41) | 45 (43 - 48) | 56 (54 - 59) | 69 (64 - 73) | <0.001 |
| No | 22 (19 - 26) | 30 (28 - 32) | 39 (37 - 42) | 53 (48 - 58) | Ref. |
Reported values incorporate survey weights to account for the complex survey design. Disability prevalence modeled as a spline with knots at 23, 17, 10, and 2 months prior to death, adjusted for age at death, gender, race/ethnicity, educational attainment, and household net worth. Probabilities were determined for subgroups holding other covariates fixed at their population means.
p-values are calculated for the association between predictors and disability during the last two years of life. The predictor labeled “ref” is the reference.
Questions about falling in last two years were asked for respondents 65 years or older in some survey years, but not all. Among the 8232 decedents in the study, 958 decedents were not asked the falls question in the interview prior to death.
Figure 2. Prevalence of ADL Difficulty, Disability, and Severe Disability during the Last Two Years of Life.
Prevalence of difficulty or disability, defined as the need for assistance, with any of 6 activities of daily living (ADL). Outcomes modeled as a spline with knots at 23, 17, 10, and 2 months prior to death, adjusted for age at death, gender, race/ethnicity, educational attainment, and household net worth. Severe disability is a report of 3 or more activity of daily living disabilities.
The vast majority of older adults had difficulty with walking and stair climbing during the last two years of life (eFigure 2). Two years prior to death, 69% of older adults had difficulty with walking several blocks, 45% walking one block, 82% climbing several flights of stairs, 53% climbing one flight of stairs, 22% managing finances, and 14% taking medications. In the last month of life, these rates rose to 85% for walking several blocks, 68% for walking one block, 91% for several flights of stairs, 72% for one flight of stairs, 45% for managing finances, and 32% for taking medications.
Those who died at advanced old age were much more likely to be disabled during the two years prior to death than those who died at younger ages (Figure 3, Table 2). Fifty percent (95% CI, 45-55%) of subjects who died in their 90's were disabled 24 months prior to death, 59% (95% CI, 56-62%) 12 months prior to death, and 77% (95% CI, 73-80%) in the last month of life. In contrast, the prevalence of disability for individuals who died before the age of 70 was at least 35% lower at any time point during the last two years of life.
Even after adjustment for age of death and other socio-demographic factors, women were more likely to experience disability during the two years before death than men (Table 2). At any given age at death, women were more likely to be disabled than men during the two years prior to death (Figure 3). Among social factors, net worth was a major predictor of disability in the two years prior to death (Table 2). The highest burden of ADL disability was experienced by those in the lowest quartile of net worth (32% two years prior to death, 95% CI 28-35%), and the lowest burden among those with the greatest wealth (23% two year prior to death, 95% CI, 19-27%). Subjects with lower educational attainment were more likely to experience disability. In unadjusted analysis married or partnered subjects were less likely to become disabled during the two years before death (31% vs. 42%, p<0.001), but this relationship reversed after adjustment for sociodemographic factors (Table 2). Differences by race/ethnicity were not found after adjustment for socioeconomic factors. All examined chronic conditions and health events were associated with end-of-life disability (Table 2).
To place our findings in context and to test the robustness of our findings we conducted several additional analyses. First, no time trend for disability was present for the years 2000-2010 (p for trend=0.42). Second, we examined rates of disability among all living subjects in the 2010 HRS for comparison, and these were lower for all subgroups when compared with disability at the end of life (see eTable 1). Third, we compared the 1,989 decedent subjects who were not interviewed during the last 2 years of life with the 8,232 decedent subjects in our sample, and found them to be similar in terms of age, gender, and race/ethnicity (all p > 0.4). However, when we compared after-death reports by next-of-kin about disability during the last 3 months of life, disability was 4% more common among the 1,989 excluded decedents than the 8,232 subjects in our sample (78% vs. 74%, P=0.02).
Comment
Those who live to an older age are much more likely than those who die at younger ages to be disabled in basic activities of daily living, and thus dependent on caregiver assistance months or years prior to death. Over one third of all older adults can expect to experience need assistance with ADL disability a year prior to death, and over a quarter two years prior to death. Nearly all older adults will have difficulty walking or climbing stairs two years before death. Half of all older adults who live to their tenth decade will be disabled in activities of daily living two years prior to death, and over two-thirds six months prior to death, and thus be dependent on the help of family or paid caregivers for a protracted period of time. Among women and men who live to the same age, women will be disabled substantially longer before death. The poor bear a greater burden of functional impairment and disability in the two years prior to death than the wealthy.
Many persons are now living independently into their 9th and 10th decades. While we often can not exactly predict when these individuals are entering their last two years of life, we know with certainty that all will have an end of life experience, and in most cases, will need assistance with basic activities a protracted period of time before death. From a societal perspective, the number of persons living with disability prior to death will balloon as the population ages.
Our data do not directly address the compression of morbidity hypothesis which suggests that as life expectancy increases on a societal level, the amount of time spent in disabled states will decrease, although we found no time trend in rates of disability over the most recent 10 years.18 Our data do question whether it is currently reasonable to sell the public a view of aging that purports that it is reasonable to expect to both live a long life and remain free of disability throughout life.4 Our findings add to the evidence that those who live to advanced ages will spend greater periods of time in states of disability prior to death than those who die at younger ages.6,7
One response to the information we present is to increase resources directed at the prevention of disability prior to death. Many people fear living in a state of disability prior to death, and some fear living in a prolonged state of disability prior to death more than death itself.19 Yet previous research suggests that once older adults become disabled, they often report that they maintain a good quality of life.20 Younger, non-disabled persons underestimate their ability to adapt to disability in advanced age. Efforts directed at prevention of disability are important. For many older adults, however, disability is part and parcel of life. Our findings suggest that many older adults have a prolonged period of time to learn to adapt and cope with disability prior to death.
Another response to this information is an acknowledgement of the inevitability of disability at the end of life, and support for formal and informal care systems that promote a high quality of life for disabled persons nearing the end of life.20 Our current system is too focused on disease-specific outcomes, such as gycoslyated hemoglobin levels for patients with diabetes, or survival in patients with heart failure.21 But these outcomes do a poor job of capturing the goals of older adults, who often live with disability, multiple chronic conditions, and cognitive impairment for months or years prior to death. Our health care system needs to be redirected toward the meeting goals of the many older adults whose priority is maintaining physical function and a high quality of life in their last years.21
The needs for ADL assistance in the last years of life we describe are often provided by unpaid family caregivers, resulting in a considerable savings to our society.22 Our current health system does an inadequate job of supporting family caregivers, many of whom, untrained and unprepared, struggle for months and years providing in-home care for disabled older adults with little support from our health or social systems.2,23,24 Caregiving is a duty for some and a gift for others. But caregiving also places a significant physical, psychological, and financial strain on families.25,26 Successful healthcare innovations that incorporate family caregivers have been developed,27-30 but in comparison to drug and device innovations designed for older adults, these healthcare innovations have not been widely implemented and disseminated.
While previous research demonstrated that women are more likely to become disabled then men,5,31 to our knowledge, this is the first national study to demonstrate that women are at risk for increased disability at all time points during the last two years of life, independent of age of death. The combination of higher life expectancy and higher rates of disability at any given age at death makes end of life disability a crucial yet generally unrecognized women's health issue. As with many issues in geriatrics, the etiology of this gender gap is likely multifactorial, attributable to some mix of gender differences in rates of disabling conditions (e.g. depression, osteoarthritis), geriatric syndromes (e.g. falls), and predisposing physiologic factors (e.g. body fat composition and sarcopenia).31 Furthermore, women disproportionately bear the burden of providing care for disabled older adults. Whereas disabled older men are likely to be cared for by a spouse, disabled older women are more likely to be living alone, with few financial resources, cared for by a daughter.31 Policy makers need to account for these gender disparities when designing interventions to support women in their last years of life.
Our estimates of disability during the last two years of life are likely conservative, for two reasons. First, according to next-of-kin after the subject's death, the 1,989 excluded subjects without an interview in the last two years had 4% higher rates of disability than subjects included in our sample. Second, next-of-kin of subjects included in our sample report higher rates of any disability during the last 3 months of life (74%) than subjects reported themselves in the last month of life (56%). This is likely because disability continues to increase during the final month, and next-of-kin report their last recollections of their loved ones from the final days of life, when rates of disability are highest.
Older age disability is known to be a dynamic process and older persons have episodes of recurrence and remission of disability before becoming permanently disabled.11,12 Our study design is not able to capture individual trajectories of function. While our analyses do not provide data about the disability trajectories individuals may experience in the last months of life,6 they do provide detailed estimates of the proportion of persons who will have ADL disability, and thus need caregiving assistance at some point during the last two years of life. It also provides national estimates of the disability burden in men and women, and how the risk of disability varies by wealth. These detailed estimates, which did not previously exist, provide essential data that provide insights into population health and caregiving needs in the last two years of life.
Conclusion
Regardless of whether compression of morbidity is occurring, it is important for health system and society to plan better for the epidemic of end-of-life disability that is inevitable in an aging population. Preventive efforts are important, yet so too are funding, research, and policy initiatives that address quality of life concerns of adults living with disability in their last years. Our health systems are designed to pay for disease management, and are sorely unprepared to meet the needs that stem from disability. Policy changes might first target the most vulnerable groups, particularly women who live to advanced age and the families that care for them.
Supplementary Material
Acknowledgments
Dr. Smith had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Funding: Dr. Smith was supported by the National Center for Research Resources UCSF-CTSI (UL1 RR024131) and a Paul Beeson Career Development Award in Aging 1K23AG040772-01A1. Drs. Walter and Covinsky were supported by K-24 grants from the National Institute on Aging (K24AG029812 and 1K24AG041180-01, respectively).
Footnotes
The authors have no conflicts of interest.
The NIH had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
References
- 1.2008 National Population Projections. [Accessed 10/29/12];2008 http://www.census.gov/population/projections/
- 2.Levine C. The loneliness of the long-term care giver. N Engl J Med. 1999 May 20;340(20):1587. doi: 10.1056/NEJM199905203402013. [DOI] [PubMed] [Google Scholar]
- 3.Gillick MR. The Denial of Aging: Perpetual Youth, Eternal Life, and Other Dangerous Fantasies. Boston, MA: Harvard University Press; 2007. [Google Scholar]
- 4.Roizen MF, Oz MC. You Staying Young: The Owner's Manual for Extending Your Warranty. New York: Free Press; 2007. [Google Scholar]
- 5.Katz S, Branch LG, Branson MH, Papsidero JA, Beck JC, Greer DS. Active life expectancy. N Engl J Med. 1983 Nov 17;309(20):1218–1224. doi: 10.1056/NEJM198311173092005. [DOI] [PubMed] [Google Scholar]
- 6.Gill TM, Gahbauer EA, Han L, Allore HG. Trajectories of disability in the last year of life. N Engl J Med. 2010 Apr 1;362(13):1173–1180. doi: 10.1056/NEJMoa0909087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhao J, Barclay S, Farquhar M, Kinmonth AL, Brayne C, Fleming J. The oldest old in the last year of life: population-based findings from Cambridge city over-75s cohort study participants aged 85 and older at death. J Am Geriatr Soc. Jan;58(1):1–11. doi: 10.1111/j.1532-5415.2009.02622.x. [DOI] [PubMed] [Google Scholar]
- 8.Kulminski A, Ukraintseva SV, Akushevich I, Arbeev KG, Land K, Yashin AI. Accelerated accumulation of health deficits as a characteristic of aging. Experimental gerontology. 2007 Oct;42(10):963–970. doi: 10.1016/j.exger.2007.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stone R, Cafferata GL, Sangl J. Caregivers of the frail elderly: a national profile. Gerontologist. 1987 Oct;27(5):616–626. doi: 10.1093/geront/27.5.616. [DOI] [PubMed] [Google Scholar]
- 10. [Accessed 10/29/2012];Health and Retirement Study: Sample Sizes and Response Rates. 2011 http://hrsonline.isr.umich.edu/sitedocs/sampleresponse.pdf.
- 11.Verbrugge LM, Jette AM. The disablement process. Soc Sci Med. 1994 Jan;38(1):1–14. doi: 10.1016/0277-9536(94)90294-1. [DOI] [PubMed] [Google Scholar]
- 12.Covinsky KE, Pierluissi E, Johnston CB. Hospitalization-associated disability: “She was probably able to ambulate, but I'm not sure”. JAMA. 2011 Oct 26;306(16):1782–1793. doi: 10.1001/jama.2011.1556. [DOI] [PubMed] [Google Scholar]
- 13.Feder J, Komisar HL, Niefeld M. Long-term care in the United States: an overview. Health Aff (Millwood) 2000 May-Jun;19(3):40–56. doi: 10.1377/hlthaff.19.3.40. [DOI] [PubMed] [Google Scholar]
- 14.Harrell FEJ. With Applications to Linear Models, Logistic Regression, and Survival Analysis. New York: Springer; 2001. Regression Modeling Strategies. [Google Scholar]
- 15.Archer KJ, Lemeshow S. Goodness-of-fit test for a logistic regression model fitted using survey sample data. Stata J. 2006;6:97–105. [Google Scholar]
- 16.Prabasaj P, Pennell ML, Lemeshow S. Standardizing the power of the Hosmer-Lemeshow goodness of fit test in large data sets. Statistics in Medicine. 2012;32:67–80. doi: 10.1002/sim.5525. [DOI] [PubMed] [Google Scholar]
- 17.Health and Retirement Study: Sampling Weights. http://hrsonline.isr.umich.edu/sitedocs/wghtdoc.pdf.
- 18.Fries JF. Aging, natural death, and the compression of morbidity. N Engl J Med. 1980 Jul 17;303(3):130–135. doi: 10.1056/NEJM198007173030304. [DOI] [PubMed] [Google Scholar]
- 19.Sutherland HJ, Llewellyn-Thomas H, Boyd NF, Till JE. Attitudes toward quality of survival. The concept of “maximal endurable time”. Med Decis Making. 1982;2(3):299–309. doi: 10.1177/0272989X8200200306. [DOI] [PubMed] [Google Scholar]
- 20.King J, Yourman L, Ahalt C, et al. Quality of Life in Late Life Disability: “I don't feel bitter because I am in a wheelchair.”. Journal of the American Geriatrics Society. 2011 doi: 10.1111/j.1532-5415.2011.03844.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Reuben DB, Tinetti ME. Goal-oriented patient care--an alternative health outcomes paradigm. N Engl J Med. 2012 Mar 1;366(9):777–779. doi: 10.1056/NEJMp1113631. [DOI] [PubMed] [Google Scholar]
- 22.Arno PS, Levine C, Memmott MM. The economic value of informal caregiving. Health Aff (Millwood) 1999 Mar-Apr;18(2):182–188. doi: 10.1377/hlthaff.18.2.182. [DOI] [PubMed] [Google Scholar]
- 23.Levine C, Halper D, Peist A, Gould DA. Bridging troubled waters: family caregivers, transitions, and long-term care. Health Aff (Millwood) 2010 Jan-Feb;29(1):116–124. doi: 10.1377/hlthaff.2009.0520. [DOI] [PubMed] [Google Scholar]
- 24.Katz SJ, Kabeto M, Langa KM. Gender disparities in the receipt of home care for elderly people with disability in the United States. JAMA. 2000 Dec 20;284(23):3022–3027. doi: 10.1001/jama.284.23.3022. [DOI] [PubMed] [Google Scholar]
- 25.Rabow MW, Hauser JM, Adams J. Supporting family caregivers at the end of life: “they don't know what they don't know”. JAMA. 2004 Jan 28;291(4):483–491. doi: 10.1001/jama.291.4.483. [DOI] [PubMed] [Google Scholar]
- 26.Covinsky KE, Goldman L, Cook EF, et al. The impact of serious illness on patients' families. SUPPORT Investigators. Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatment. JAMA. 1994 Dec 21;272(23):1839–1844. doi: 10.1001/jama.272.23.1839. [DOI] [PubMed] [Google Scholar]
- 27.Boyd CM, Reider L, Frey K, et al. The effects of guided care on the perceived quality of health care for multi-morbid older persons: 18-month outcomes from a cluster-randomized controlled trial. J Gen Intern Med. 2010 Mar;25(3):235–242. doi: 10.1007/s11606-009-1192-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wolff JL, Giovannetti ER, Boyd CM, et al. Effects of guided care on family caregivers. Gerontologist. 2010 Aug;50(4):459–470. doi: 10.1093/geront/gnp124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Naylor MD, Brooten DA, Campbell RL, Maislin G, McCauley KM, Schwartz JS. Transitional care of older adults hospitalized with heart failure: a randomized, controlled trial. J Am Geriatr Soc. 2004 May;52(5):675–684. doi: 10.1111/j.1532-5415.2004.52202.x. [DOI] [PubMed] [Google Scholar]
- 30.Coleman EA, Parry C, Chalmers S, Min SJ. The care transitions intervention: results of a randomized controlled trial. Arch Intern Med. 2006 Sep 25;166(17):1822–1828. doi: 10.1001/archinte.166.17.1822. [DOI] [PubMed] [Google Scholar]
- 31.Newman AB, Brach JS. Gender gap in longevity and disability in older persons. Epidemiol Rev. 2001;23(2):343–350. doi: 10.1093/oxfordjournals.epirev.a000810. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.