Abstract
Background and Objectives
Aging, HIV, and social isolation may affect acute care utilization and outcomes. Our objectives were to compare levels of social isolation in aging Veterans with and without HIV and determine associations with hospital admission and mortality.
Study Design, Participants, and Setting
The Veterans Aging Cohort Study (VACS) is a longitudinal study of HIV+ and uninfected Veterans at eight VA Medical Centers nationally. We analyzed data for 1,836 Veterans age ≥55 enrolled in VACS from 2002–2008.
Measurements
We created a Social Isolation Score (SIS) using baseline survey responses about: relationship status, number of friends/family and frequency of visits, and involvement in volunteer work, religious or self-help groups, or other community activities. We compared scores by age and HIV status and used multivariable regression to assess effects of social isolation scores on hospital admission and all-cause mortality.
Results
Mean SIS was higher for HIV+ patients with increasing difference by age (p=.01 for trend). Social isolation was also more prevalent for HIV+ (59%) compared to uninfected patients (51%; p<.001). In multivariable regression analysis of HIV+ and uninfected groups combined, adjusted for demographic and clinical features, isolation was independently associated with increased risk of incident hospitalization (HR=1.25, 95% CI=1.09–1.42) as well as risk of all-cause mortality (HR=1.28, 95% CI=1.06–1.54). Risk estimates calculated for HIV+ and uninfected groups separately were not significantly different.
Conclusions
Social isolation is associated with increased risk of hospitalization and death among both HIV+ and uninfected older Veterans. Despite similar effects in both groups, the population level impact of social isolation may be greater in those who are HIV+ because of the higher prevalence of social isolation, particularly among the oldest patients.
Keywords: Social isolation, aging, HIV/AIDS, hospitalization, mortality, outcomes of care
Background
Social isolation is common among aging adults and has important effects on healthcare and health outcomes.1,2 Numerous studies have demonstrated increased overall risk for mortality3,4 and geriatric morbidity such falls,5 cognitive and functional decline,6,7 especially among those with chronic conditions such as coronary artery disease,8,9 cancer,10 and diabetes.11 Currently, there is less information about isolation among adults aging with Human Immunodeficiency Virus (HIV), yet recent advances in anti-retroviral therapy have transformed HIV to a chronic condition with increased life expectancies and “graying” of the infected population.12,13 Additionally, the incidence of new HIV infections in older adults has increased dramatically in the last decade.14 These trends suggest a need for more information not only about effects of isolation on mortality for the growing number of older adults living with chronic HIV infection but also a need to understand possible effects on acute care utilization given longer life expectancies in this population.
Compared to the aging population with other chronic conditions, adults living with HIV/AIDS may be at particularly high risk for social isolation as they age. Many have lost friends or partners who were also infected but did not survive the early years of the epidemic.15,16 Social networks and support may also be inhibited by the stigma attached to HIV. This stigma is especially strong for populations who are disproportionately infected such as African-Americans and Hispanics,17,18 as well as men who have sex with men (MSM).19 Furthermore, HIV infection itself intensifies many normal aging processes and increases the incidence and severity of frailty.20,21,22 Thus, HIV+ individuals may be at higher risk for isolation and frailty leading to increased overall risk for hospitalization and death when compared to an uninfected cohort. Currently, comparisons on the prevalence and effects of social isolation between HIV+ and uninfected aging patients are lacking. Specifically, current studies have yet to examine how components of social isolation, such as limited engagement with friends, family, or community, may differentially affect acute care utilization and mortality among HIV+ and uninfected older adults.
The Veterans Aging Cohort Study (VACS) dataset presents a unique opportunity to study the prevalence and effects of social isolation on inpatient admission and outcomes of care in an aging population in a multi-site, longitudinal cohort of Veterans and to compare these effects for HIV+ patients with uninfected patients. Our objectives were to compare levels of social isolation in aging Veterans with and without HIV and determine associations with incident hospital admission and all-cause mortality.
Methods
Study design and sample
VACS is an observational cohort of HIV+ and un-infected patients designed to examine the role of social, medical, and psychiatric factors on aging and clinical outcomes. Participants are enrolled prospectively from infectious disease and general medicine clinics at eight VA Medical Centers (Atlanta, GA, Baltimore, MD, Bronx, NY, New York City, NY, Houston, TX, Los Angeles, CA, Pittsburg, PA, Washington, DC). Uninfected patients are matched to the infected group by age, race, and site. A full description of VACS recruitment, enrollment rates, study instruments, study measures collected, and quality control is described elsewhere.23 Briefly, VACS collects socio-demographics, comorbidities, and measures of health behaviors and beliefs from patient surveys, administrative and clinical data sources through the VA national electronic medical record. Institutional review boards at all sites approved the study, and all Veterans provided written informed consent. For the present study, we analyzed a sample of patients from VACS 8 with full data available who were 55 years of age or older when they completed the VACS baseline survey between June 1, 2002 and September 30, 2008 (Table 1).
Table 1.
Patient Characteristics
| N=1836 | Overall | HIV + | Uninfected | p-value | |||
|---|---|---|---|---|---|---|---|
| No. | % | No. | % | No. | % | ||
| Demographics | |||||||
|
| |||||||
| Age | <0.01 | ||||||
| 55–59 | 977 | 53 | 497 | 59 | 480 | 49 | |
| 60–64 | 316 | 17 | 150 | 18 | 166 | 17 | |
| 65–69 | 252 | 14 | 103 | 12 | 149 | 15 | |
| 70–74 | 134 | 7 | 47 | 6 | 87 | 9 | |
| ≥75 | 90 | 5 | 24 | 3 | 66 | 7 | |
| Race / ethnicity | |||||||
| Non-White and/or Hispanic | 1244 | 68 | 599 | 71 | 645 | 65 | 0.01 |
| White / non-Hispanic | 592 | 32 | 248 | 29 | 344 | 35 | |
| Reported household income* | |||||||
| <$25,000 | 1304 | 71 | 654 | 77 | 650 | 66 | <0.01 |
| ≥$25, 000 | 438 | 24 | 160 | 19 | 278 | 19 | |
|
| |||||||
| Clinical Characteristics | |||||||
|
| |||||||
| Beck Depression Inventory | 0.05 | ||||||
| Negative screen | 1401 | 76 | 628 | 74 | 773 | 78 | |
| Positive screen | 435 | 24 | 219 | 26 | 216 | 22 | |
| Alcohol Abuse | 0.33 | ||||||
| Negative screen | 462 | 25 | 643 | 76 | 731 | 74 | |
| Positive screen | 1374 | 75 | 204 | 24 | 258 | 26 | |
| Comorbidities** | |||||||
| Hypertension | 999 | 54 | 330 | 38 | 669 | 67 | <0.01 |
| Dyslipidemia | 572 | 31 | 179 | 21 | 393 | 39 | <0.01 |
| Diabetes | 570 | 25 | 149 | 17 | 321 | 32 | <0.01 |
| Hepatitis C | 327 | 18 | 231 | 27 | 96 | 10 | <0.01 |
| Coronary Artery Disease | 237 | 13 | 73 | 8 | 164 | 16 | <0.01 |
| Number of Comorbidities | <0.01 | ||||||
| 0 | 523 | 28 | 317 | 37 | 206 | 21 | |
| 1 | 696 | 37 | 318 | 37 | 378 | 38 | |
| 2 | 485 | 26 | 183 | 21 | 302 | 30 | |
| 3–5 | 155 | 8 | 42 | 5 | 113 | 11 | |
| Hospitalizations | <0.01 | ||||||
| 0 | 1031 | 56 | 422 | 50 | 609 | 62 | |
| 1 | 341 | 19 | 177 | 21 | 164 | 17 | |
| 2–4 | 327 | 18 | 177 | 21 | 150 | 15 | |
| 5–7 | 76 | 4 | 43 | 5 | 33 | 3 | |
| >7 | 54 | 3 | 28 | 3 | 26 | 3 | |
missing data for 94 (5%)
most frequent comorbidities by ICD-9 codes at time of VACS 8 enrollment
Measurements
Social Isolation
Social isolation has been defined as a state of lacking social engagement, belonging, and contact with others.24 Given the lack of consensus in prior literature on how best to measure social isolation in different populations, we created a Social Isolation Score (SIS) that would be well-suited to study both HIV+ and uninfected older adults by leveraging strengths of the VACS dataset designed to study these populations. First, we identified domains for this score from the VACS 8 baseline survey that captured key concepts of isolation from our review of the existing literature: frequency of visits by close friends,1,2 frequency of visits by family, 1,2 number of close friends and family combined,1,2,25 use of self-help groups in the past year,19 volunteer work or involvement with a community organization,26 attendance of religious events,27 relationship status,28 and living alone.29 Next, for each domain, we chose one question from the VACS 8 baseline survey that best represented the concept and assigned one point for each response indicating isolation and zero points for each response indicating lack of isolation. For questions with multiple responses, we assigned 1 point for the most-isolated response, 0 points to the least-isolated response, and 0.5 points for any response in-between. The final Social Isolation Score contains 8 variables with a range of possible scores from 0–8 in 0.5 increments (Table 2). Finally, we used the Spearman test to assess construct validity and found significant correlation between SIS components (p<0.05 for 23 out of 28 unique combinations).
Table 2.
Components for Social Isolation Scale
| Total N=1836 | All | HIV+ | Uninfected | Social Isolation Score (p-value) | ||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| No. | % | No. | % | No. | % | |||
| Visits from Close Family | ||||||||
| Less than once a month | 324 | 17 | 155 | 18 | 169 | 17 | 1 | |
| A few times a week to monthly | 1037 | 56 | 587 | 58 | 550 | 66 | 0.5 | |
| Daily | 475 | 26 | 205 | 24 | 270 | 27 | 0 | |
| Mean Score | 0.46 | 0.47 | 0.45 | (0.16) | ||||
|
| ||||||||
| Visits from Close Friends | ||||||||
| Less than once a month | 393 | 21 | 166 | 20 | 227 | 23 | 1 | |
| A few times a week to monthly | 951 | 52 | 426 | 50 | 525 | 53 | 0.5 | |
| Daily | 492 | 27 | 255 | 30 | 237 | 24 | 0 | |
| Mean Score | 0.47 | 0.45 | 0.49 | (<0.01) | ||||
|
| ||||||||
| Number of Close Family or Friends | ||||||||
| None | 183 | 10 | 100 | 12 | 83 | 8 | 1 | |
| One | 200 | 11 | 104 | 12 | 96 | 10 | 0.5 | |
| More than one | 1453 | 79 | 643 | 76 | 810 | 82 | 0 | |
| Mean Score | 0.15 | 0.18 | 0.13 | (<0.01) | ||||
|
| ||||||||
| Use of Self-help or Support Group in last year | ||||||||
| No | 1430 | 78 | 640 | 76 | 790 | 80 | 1 | |
| Yes | 406 | 22 | 207 | 24 | 199 | 20 | 0 | |
| Mean Score | 0.78 | 0.76 | 0.80 | (0.03) | ||||
|
| ||||||||
| Volunteer Work or Involvement with a Community Organization | ||||||||
| Little or none of the time | 1181 | 64 | 515 | 61 | 666 | 67 | 1 | |
| Some or a good bit of the time | 387 | 21 | 197 | 23 | 190 | 19 | 0.5 | |
| Most or all of the time | 268 | 15 | 135 | 16 | 133 | 14 | 0 | |
| Mean Score | 0.75 | 0.72 | 0.77 | (<0.01) | ||||
|
| ||||||||
| Frequency of Attendance to Religious Events | ||||||||
| Never | 477 | 26 | 231 | 27 | 246 | 25 | 1 | |
| < twice yearly to 2–3 times a month | 969 | 53 | 443 | 52 | 526 | 53 | 0.5 | |
| Every week to every day | 390 | 21 | 173 | 20 | 217 | 22 | 0 | |
| Mean Score | 0.52 | 0.53 | 0.51 | 0.22 | ||||
|
| ||||||||
| Relationship Status | ||||||||
| Single (incl. separated, divorced, etc) | 1257 | 68 | 683 | 81 | 574 | 58 | 1 | |
| Married or living with partner | 579 | 32 | 164 | 19 | 415 | 42 | 0 | |
| Mean Score | 0.68 | 0.81 | 0.58 | (<0.01) | ||||
|
| ||||||||
| Living Alone | ||||||||
| Yes | 115 | 6 | 60 | 7 | 55 | 6 | 1 | |
| No | 1721 | 94 | 787 | 93 | 934 | 94 | 0 | |
| Mean Score | 0.06 | 0.07 | 0.06 | 0.18 | ||||
| Mean Social Isolation Scores | 3.88 | 3.99 | 3.80 | <0.001 | ||||
Clinical outcomes
Our primary outcomes of interest were: (1) incident admission for acute inpatient care at any VA medical center and (2) all-cause mortality between study enrollment on June 1, 2002 and September 30, 2010 to allow at least 2-year follow-up after the last enrollment date. To account for variations in length of follow up time, we used time-to-event analyses for both outcomes. Since data for the social isolation score were derived from the baseline survey, we abstracted information on the first hospitalization to occur any time after enrollment in VACS 8. Dates of death were used to determine time-to-death within the study and to conduct survival analyses.
Potential confounders
Covariates included age (continuous), race and ethnicity (white/non-Hispanic vs. non-white and/or Hispanic), and income (<$25,000/year vs. ≥$25,000/year) (Table 1). We identified the 5 most-frequent comorbidities from participant ICD-9 codes at the time of enrollment (Hypertension, Dyslipidemia, Diabetes, Hepatitis C, and Coronary Artery Disease) and calculated a sum total of comorbidities for each participant. Alcohol abuse was assessed using the Alcohol Use Disorders Identification Test (AUDIT-C)30,31 and we used the Beck Depression Inventory (BDI) to assess for depressive symptoms. Finally, we calculated a sum total of hospitalizations to any VA medical center during the study dates for each participant.
Analyses
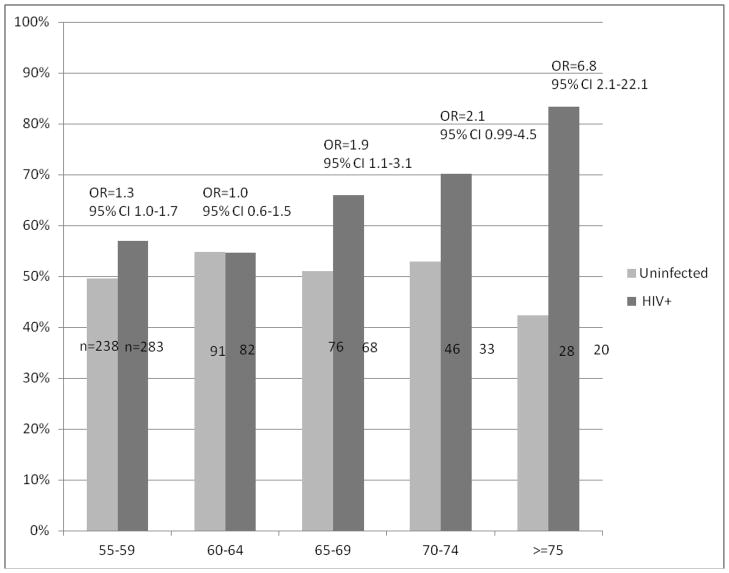
We suspected social isolation would be higher in HIV+ participants a priori based on previous evidence of lower levels of social support in this population. We therefore stratified our descriptive analysis of baseline characteristics and incidence rates for outcomes by HIV status. We then calculated SIS for each patient in the dataset, mean SIS score for all patients, as well as prevalence of social isolation by HIV status. To further explore differences in SIS prevalence and mean scores by HIV status, we graphed unadjusted odds ratios for isolation (SIS≥4) for HIV+ vs. uninfected participants by age in 5 year brackets from 55–75 and over 75 (Figure 1).
Figure 1. Percent of Veterans Isolated (SIS≥4) by Age and HIV Status.
* Odds ratios are unadjusted and demonstrate the likelihood of isolation (SIS≥4) for HIV+ vs. uninfected patientsin each age bracket
We then examined relationships between SIS and time-to-outcomes using Cox multivariable regression models. Initially, we stratified Cox regressions by HIV status; however, we noted that point estimates and effect sizes for HIV+ and uninfected groups in these analyses were very similar. We therefore created a single combined multivariable model with all subjects using the same independent variables from the stratified analysis and an HIV interaction term. The interaction tests for HIV*SIS were non-significant in all combined analyses (for hospital admission HR=0.82, 95% CI= 0.63–1.06; for mortality HR=0.77, 95% CI= 0.55–1.09). We therefore concluded that the effects of SIS on each group (HIV+ and uninfected) were not significantly different and present results of the combined Cox regressions. Finally, we used the variance of inflation test to ensure there was no collinearity between predictor variables. All regressions were performed with age, race, income, HIV status, number of comorbidities, depression, and alcohol abuse as covariates. All analyses were performed using SAS version 9.2.
Results
Complete data were available for 1,836 Veterans aged 55 or older. Ages ranged from 55–91 years (mean=61); 54% were uninfected and 46% were HIV+; 99% were male; 68% were non-white and/or Hispanic; 76% reported an annual income of less than $25,000 (Table 1). Most patients (72%) had 1 or more comorbid condition and most patients screened negative for depression (76%) and alcohol abuse (75%).
Social Isolation Scores (SIS) for the entire sample ranged from 0–8 with a mean of 3.88 (Std dev 1.22). We also calculated SIS for HIV+ and uninfected patients separately (Table 2). As shown in Table 2, mean scores for 5 out of 8 SIS components were higher for HIV+ patients; however, only 2 of these (number of friends and family and relationship status) were significantly different. The overall mean SIS for HIV+ patients (3.99) was significantly higher than for uninfected patients (3.80; p<0.001) and the odds of being isolated were significantly higher for HIV+ patients in all age brackets (except 60–64) with a trend towards increasing odds of isolation with increasing age (Figure 1). The overall prevalence of isolation (SIS≥4) was also greater for HIV+ patients (59%) than uninfected patients (51%; p<.001).
With respect to incident hospitalization, 805 Veterans (43%) had at least one admission to a VA Medical Center between 2002 and 2008 (Table 1). Overall, incidence of hospitalization was higher in HIV+ patients (113 per 1000 person-years) compared to uninfected patients (70 per 1000 person-years; p<.001) and mean time-to-admission was shorter in HIV+ patients compared to uninfected patients (1.8 years vs. 2.2 years; p=.001). After adjusting for age, race/ethnicity, income, number of comorbidities, depression, substance abuse, and HIV status, isolation was independently associated with increased risk of incident hospitalization (HR=1.25, 95% CI=1.09–1.42) in combined analyses of HIV+ and uninfected patients (Table 3).
Table 3.
Effects of Social Isolation Score (SIS) on Inpatient Admission and All-cause Mortality
| Effects of Social Isolation Score (SIS) on: | N=1836 | |
|---|---|---|
| Hazard Ratio | (95% CI) | |
| Inpatient admission during study period | ||
| SIS ≥4 | 1.25 | 1.09 – 1.42 |
| HIV + | 1.67 | 1.46 – 1.91 |
| Age (continuous, per year increase) | 1.01 | 1.00 – 1.02 |
| Number of Table 1 comorbidities (continuous, per unit increase) | 1.33 | 1.24 – 1.42 |
| Non-white race/ethnicity | 1.44 | 1.24 – 1.67 |
| Income <$25,000 / year | 1.57 | 1.34 – 1.86 |
| Depression screen + | 1.13 | 0.97 – 1.32 |
| Alcohol abuse screen + | 0.98 | 0.84 – 1.14 |
|
| ||
| Risk of death during study period | ||
| SIS ≥4 | 1.28 | 1.06 – 1.54 |
| HIV + | 2.02 | 1.67 – 2.46 |
| Age (continuous, per year increase) | 1.05 | 1.04 – 1.07 |
| Number of Table 1 comorbidities (continuous, per unit increase) | 1.13 | 1.03 – 1.25 |
| Non-white race/ethnicity | 1.25 | 1.02 – 1.53 |
| Income <$25,000 / year | 1.38 | 1.08 – 1.77 |
| Depression screen + | 1.18 | 0.95 – 1.46 |
| Alcohol abuse screen + | 1.17 | 0.94 – 1.46 |
Hazard Ratios are adjusted for all variables listed above
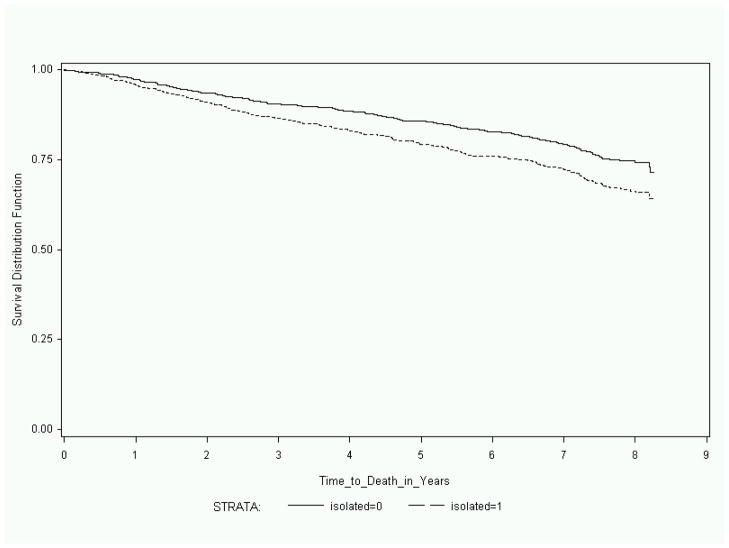
Similar to incident hospitalization, we found that incidence of mortality was higher for HIV+ patients in our cohort (56 per 1000 person-years) than for uninfected patients (33 per 1000 person-years; p-value p<.001) and time to death was shorter for HIV+ compared to uninfected patients (3.9 years vs. 4.8 years, p-value p<.001). After adjusting for age, race/ethnicity, income, number of comorbidities, depression, substance abuse, and HIV status, isolation was independently associated with increased risk of all-cause mortality during the study period (HR=1.28, 95% CI=1.06–1.54) in combined analyses of HIV+ and uninfected patients (Table 3 and Figure 2).
Figure 2.
Survival Analysis for Socially-Isolated vs. Non-Isolated Veterans
Discussion
We found that while social isolation has similar effects on hospitalization and death for both HIV+ and uninfected individuals, those with HIV are at substantially higher risk of being socially isolated. While the effects of social isolation on mortality have been well-documented among older adults,32 ours is the first study to include a large number of older HIV+ individuals. Additionally, our study presents novel findings on the effects of social isolation on acute care utilization (incident hospitalization) in this population and suggests a need to reframe current paradigms about hospitalization in HIV+ older adults. Existing studies of hospitalization in HIV+ patients focus on acute presentations or specific complications of HIV infection33 but, in the current era of potent anti-retroviral therapies, HIV+ patients are frequently admitted for (and die from) chronic conditions that characterize the aging population as a whole.34 Rather than focusing on HIV-related comorbidities, our findings suggest a need to understand aging HIV+ patients’ risks for hospitalization and mortality in the broader context of their social lives and to increase preventative efforts for those with low social support. While we found that social isolation affects these outcomes for both HIV+ and uninfected patients in our cohort, our finding that the prevalence of social isolation is higher among HIV+ older adults, particularly at older ages, underscores the need to prioritize such efforts for this population.
Our findings that social isolation is more prevalent among HIV+ compared to uninfected older adults with increasing difference by age (figure 1) may be explained by several factors. First, older adults with HIV are significantly more economically and politically marginalized than uninfected counterparts at all ages which may predispose them to social isolation.35,36 Second, it may be that increased stress levels associated with long-term HIV survival37 and intensified geriatric syndromes in HIV+ patients such as cognitive impairment further inhibit their ability to establish and maintain social ties.38 Third, low social support itself is a predictor for delay in HIV testing39 and treatment40 thus placing older, more isolated individuals at risk for worsening health and compounding isolation.41 Fourth, many older adults with HIV experience a heightened sense of loneliness which may lead to anxiety, depression, and further withdrawal from social networks that can have protective effects on isolation.42, 43 Moreover, the relatively young age for half of our sample (53% under age 60) likely attenuates the overall difference in prevalence of isolation seen between HIV+ (59%) and uninfected in this study (51%); this overall difference seem likely to increase as this population continues to age. Finally, given recent research showing important effects of loneliness on overall health,44, 45 disability and mortality,46 our findings underscore the need to study overlapping effects of social isolation and loneliness for aging populations.
Our findings also have several important health policy implications. First, our study focused on patients in the VA system for who access to care is not an issue; the health effects and associated costs of isolation may be even greater for patients outside this system. Second, while the number of older, HIV+ patients is rising, the number of providers in HIV medicine and geriatrics remains very small.47 Thus, efforts to address social isolation in older, HIV+ adults will also need to engage hospitalists, emergency medicine physicians, and others in acute care specialties as well as leverage non-physician resources such as case management and community-based organizations.48 Third, there is also growing evidence that interventions to address social isolation through activities such as support groups, social activities, home visits, and Internet engagement can reduce isolation in older adults.49 While these interventions will have associated costs in terms of time, effort, and funding, they may be less expensive than high rates of acute care utilization and may result in better outcomes as well. Fourth, socio-economic status likely plays an important role in mediating social isolation as well as outcomes we report. While further study is needed to explore this relationship as well as possible effects on overall quality of life, we recommend that clinicians prioritize screening for social isolation among their most vulnerable patients first: the oldest and poorest with the worst quality of life may be most likely to be clinically affected by social isolation. Finally, as HIV+ individuals age, high levels of social isolation may place additional strain on an over-burdened system of nursing homes skilled nursing facilities.50, 51 Previous studies have shown that living alone52,53, fewer family contacts,53, 54 and fewer non-kin social supports52 are all correlated with NH placement; however, a more comprehensive assessment of isolation factors such as those contained in our SIS has not been studied. This is an important area for future aging research with a specific focus needed for HIV+ patients given their increased risk for isolation as they age.
Our study has several limitations. First, this is a longitudinal study using observational data so we cannot make inferences about causality between social isolation and inpatient admission or mortality. Second, we used data from baseline surveys to create our social isolation score and thus considered components of this measure to have “fixed effects” on overall social isolation. Third, we did not adjust for severity of illness in our final analysis because when we included scores from a validated HIV morbidity and mortality prediction tool (the VACS Risk Index)55 in our models, we found that differences in our outcomes of interest were no longer significant. Given that social isolation may well mediate poor disease control and overall severity of illness,56 we felt that inclusion of these risk index scores in our models would be over-adjustment. Indeed, the causal pathways between social isolation and outcomes remain unknown and represent an important area for future research. Fourth, while we carefully selected items for our Social Isolation Scale based on current literature on this topic and tested for construct validity, we did not perform more formal psychometric testing for internal and external validity. Our scale also differs from one of the most rigorously-validated instruments to assess social isolation (the Lubben Social Network Scale or LSNS-6 which focuses on closeness and redundancy of social contacts among family and friends) in that our score incorporates forms of social engagement beyond family and friends such as community volunteering, self-help groups, and religious activity which are not captured in the LSNS-6. Finally, our sample of Veterans is predominantly male and non-white so our results may not be generalizable to women and whites.
In conclusion, we found that social isolation is associated with increased risk of hospitalization and death among both HIV+ and uninfected older Veterans. Despite similar effects in both groups, the population level impact of social isolation may be even greater in those who are HIV+ because of the higher prevalence of social isolation, particularly among the oldest patients. As the “graying” of HIV+ population is projected to accelerate in the coming decades, a broader understanding of social isolation and the application of geriatric principles of inpatient care for this population is needed.
Acknowledgments
The authors would like to thank the Robert Wood Johnson Foundation Clinical Scholars program and US Department of Veterans Affairs for funding support. Dr. Horwitz is supported by the National Institute on Aging (K08 AG038336) and by the American Federation for Aging Research through the Paul B. Beeson Career Development Award Program.
Role of Sponsors:
No sponsor (The Robert Wood Johnson Foundation, US Department of Veterans Affairs, the National Institute on Aging, or the American Federation for Aging Research) had any role in the study design; in the collection, analysis, and interpretation of data; in the writing of the report; or in the decision to submit the article for publication.
Footnotes
This paper was presented at the 2012 Annual Meeting of the American Geriatrics Society.
Conflicts of Interest:
The authors have declared they have no financial, personal, or other conflicts of interest relevant to this study.
Author Contributions:
S.R. Greysen: study conception and design, analysis and interpretation of data; drafting and revising of manuscript; final approval of manuscript for publication.
L.I. Horwitz: data interpretation; manuscript revision; final approval for publication.
K.E. Covinsky: data interpretation; manuscript revision; final approval for publication.
K. Gordon: data interpretation; manuscript revision; final approval for publication.
M.E. Ohl: data interpretation; manuscript revision; final approval for publication.
A.C. Justice: study conception and design, analysis and interpretation of data; revising of manuscript; final approval of manuscript for publication.
References
- 1.Cornwell EY, Waite LJ. Social disconnectedness, perceived isolation, and health among older adults. J Health Soc Behav. 2009 Mar;50(1):31–48. doi: 10.1177/002214650905000103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cornwell B, Laumann EO, Schumm LP. The Social Connectedness of Older Adults: A National Profile. Am Sociol Rev. 2008;73(2):185–203. doi: 10.1177/000312240807300201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stringhini S, Berkman L, Dugravot A, et al. Socioeconomic status, structural and functional measures of social support, and mortality: The British Whitehall II Cohort Study, 1985–2009. Am J Epidemiol. 2012 Jun 15;175(12):1275–83. doi: 10.1093/aje/kwr461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tilvis RS, Routasalo P, Karppinen H, et al. Social isolation, social activity and loneliness as survival indicators in old age; nationwide survey with a 7-year follow-up. European Geriatric Medicine. 2012;3:18–22. [Google Scholar]
- 5.Faulkner KA, Cauley JA, Zmuda JM, et al. Is social integration associated with the risk of falling in older community-dwelling women? The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences. 2003;58:M954–M959. doi: 10.1093/gerona/58.10.m954. [DOI] [PubMed] [Google Scholar]
- 6.Barnes LL, Mendes de Leon CF, Wilson RS, et al. Social resources and cognitive decline in a population of older African Americans and whites. Neurology. 2004 Dec 28;63(12):2322–6. doi: 10.1212/01.wnl.0000147473.04043.b3. [DOI] [PubMed] [Google Scholar]
- 7.Unger JB, McAvay G, Bruce ML, et al. Variation in the impact of social network characteristics on physical functioning in elderly persons: MacArthur Studies of Successful Aging. J Gerontol B Psychol Sci Soc Sci. 1999 Sep;54(5):S245–51. doi: 10.1093/geronb/54b.5.s245. [DOI] [PubMed] [Google Scholar]
- 8.Berkman LF, Leo-Summers L, Horwitz RI. Emotional support and survival after myocardial infarction. A prospective, population-based study of the elderly. Ann Intern Med. 1992 Dec 15;117(12):1003–9. doi: 10.7326/0003-4819-117-12-1003. [DOI] [PubMed] [Google Scholar]
- 9.Barefoot JC, Burg MM, Carney RM, et al. Aspects of social support associated with depression at hospitalization and follow-up assessment among cardiac patients. J Cardiopulm Rehabil. 2003 Nov-Dec;23(6):404–12. doi: 10.1097/00008483-200311000-00002. [DOI] [PubMed] [Google Scholar]
- 10.Zhou ES, Penedo FJ, Lewis JE, et al. Perceived stress mediates the effects of social support on health-related quality of life among men treated for localized prostate cancer. J Psychosom Res. 2010 Dec;69(6):587–90. doi: 10.1016/j.jpsychores.2010.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Liu L. Social connections, diabetes mellitus, and risk of mortality among white and African-American adults aged 70 and older: an eight-year follow-up study. Ann Epidemiol. 2011 Jan;21(1):26–33. doi: 10.1016/j.annepidem.2010.10.012. [DOI] [PubMed] [Google Scholar]
- 12.Graying plague: by 2015 over half of HIV in U.S. will be in those over 50. Late diagnoses contribute to problem. AIDS Alert. 2010 Mar;25(3):25–8. [PubMed] [Google Scholar]
- 13.Emlet CA, Gerkin A, Orel N. The graying of HIV/AIDS: preparedness and needs of the aging network in a changing epidemic. J Gerontol Soc Work. 2009 Nov;52(8):803–14. doi: 10.1080/01634370903202900. [DOI] [PubMed] [Google Scholar]
- 14.CDC. HIV/AIDS Surveillance Report, 2005. Vol. 17. Atlanta: U.S. Department of Health and Human Services, CDC; 2007. pp. 1–54. Rev ed. [Google Scholar]
- 15.Sikkema KJ, Kalichman SC, Hoffmann R, et al. Coping strategies and emotional wellbeing among HIV-infected men and women experiencing AIDS-related bereavement. AIDS Care. 2000 Oct;12(5):613–24. doi: 10.1080/095401200750003798. [DOI] [PubMed] [Google Scholar]
- 16.Sikkema KJ, Kochman A, DiFranceisco W, et al. AIDS-related grief and coping with loss among HIV-positive men and women. J Behav Med. 2003 Apr;26(2):165–81. doi: 10.1023/a:1023086723137. [DOI] [PubMed] [Google Scholar]
- 17.Wohl AR, Galvan FH, Myers HF, et al. Do social support, stress, disclosure and stigma influence retention in HIV care for Latino and African American men who have sex with men and women? AIDS Behav. 2011 Aug;15(6):1098–110. doi: 10.1007/s10461-010-9833-6. [DOI] [PubMed] [Google Scholar]
- 18.George S, Garth B, Wohl AR, et al. Sources and types of social support that influence engagement in HIV care among Latinos and African Americans. J Health Care Poor Underserved. 2009 Nov;20(4):1012–35. doi: 10.1353/hpu.0.0210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rosenfeld D, Bartlam B, Smith RD. Out of the Closet and Into the Trenches: Gay Male Baby Boomers, Aging, and HIV/AIDS. Gerontologist. 2012 Jan 31; doi: 10.1093/geront/gnr138. [DOI] [PubMed] [Google Scholar]
- 20.Sankar A, Nevedal A, Neufeld S, et al. What do we know about older adults and HIV? A review of social and behavioral literature. AIDS Care. 2011 Oct;23(10):1187–207. doi: 10.1080/09540121.2011.564115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Capeau J. Premature Aging and Premature Age-Related Comorbidities in HIV-Infected Patients: Facts and Hypotheses. Clin Infect Dis. 2011 Dec;53(11):1127–9. doi: 10.1093/cid/cir628. [DOI] [PubMed] [Google Scholar]
- 22.Önen NF, Overton ET. A review of premature frailty in HIV-infected persons; another manifestation of HIV-related accelerated aging. Curr Aging Sci. 2011 Feb;4(1):33–41. [PubMed] [Google Scholar]
- 23.Justice AC, Dombrowski E, Conigliaro J, et al. Veterans Aging Cohort Study (VACS): overview and description. Med Care. 2006;44:S13–24. doi: 10.1097/01.mlr.0000223741.02074.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nicholson NR. A review of social isolation: an important but underassessed condition in older adults. J Prim Prev. 2012 Jun;33(2–3):137–52. doi: 10.1007/s10935-012-0271-2. [DOI] [PubMed] [Google Scholar]
- 25.Cornwell EY, Waite LJ. Measuring social isolation among older adults using multiple indicators from the NSHAP study. J Gerontol B Psychol Sci Soc Sci. 2009 Nov;64( Suppl 1):i38–46. doi: 10.1093/geronb/gbp037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Thoits PA, Hewitt LN. Volunteer work and well-being. Journal of Health and Social Behavior. 2001;42:115–131. [PubMed] [Google Scholar]
- 27.Benjamins MR. Religion and functional health among the elderly: Is there a relationship and is it constant? Journal of Aging and Health. 2004;16:355–374. doi: 10.1177/0898264304264204. [DOI] [PubMed] [Google Scholar]
- 28.Lillard LA, Waite LJ. ‘Til death do us part:’ Marital disruption and mortality. American Journal of Sociology. 1995;100:1131–1156. [Google Scholar]
- 29.Waite LJ, Hughes ME. At risk on the cusp of old age: Living arrangements and functional status among Black, White, and Hispanic adults. Journal of Gerontology. 1999;54B:S136–S144. doi: 10.1093/geronb/54b.3.s136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Saunders JB, Aasland OG, Babor TF, et al. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption-II. Addiction. 1993;88(6):791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- 31.Bush K, Kivlahan DR, McDonell MB, et al. The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Ambulatory Care Quality Improvement Project (ACQUIP). Alcohol use disorders identification test. Arch Intern Med. 1998;158:1789–95. doi: 10.1001/archinte.158.16.1789. [DOI] [PubMed] [Google Scholar]
- 32.House JS, Landis KR, Umberson D. Social relationships and health. Science. 1988;29;241(4865):540–5. doi: 10.1126/science.3399889. [DOI] [PubMed] [Google Scholar]
- 33.Betz ME, Gebo KA, Barber E, et al. HIV Research Network. Patterns of diagnoses in hospital admissions in a multistate cohort of HIV-positive adults in 2001. Med Care. 2005 Sep;43(9 Suppl):III3–14. doi: 10.1097/01.mlr.0000175632.83060.eb. [DOI] [PubMed] [Google Scholar]
- 34.Berry SA, Fleishman JA, Moore RD, Gebo KA For the HIV Research Network. Trends in Reasons for Hospitalization in a Multisite United States Cohort of Persons Living With HIV, 2001–2008. J Acquir Immune Defic Syndr. 2012 Apr 1;59(4):368–375. doi: 10.1097/QAI.0b013e318246b862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gorbach PM, Ryan C, Saphonn V, Detels R. The impact of social, economic and political forces on emerging HIV epidemics. AIDS. 2002;16( Suppl 4):S35–43. doi: 10.1097/00002030-200216004-00006. [DOI] [PubMed] [Google Scholar]
- 36.Soskolne V, van Griensven F. Epidemiology, social, cultural and political. AIDS. 2002;16( Suppl 4):S33–4. doi: 10.1097/00002030-200216004-00005. [DOI] [PubMed] [Google Scholar]
- 37.Chesney MA, Chambers DB, Taylor JM, Johnson LM. Social support, distress, and well-being in older men living with HIV infection. J Acquir Immune Defic Syndr. 2003 Jun 1;33( Suppl 2):S185–93. doi: 10.1097/00126334-200306012-00016. [DOI] [PubMed] [Google Scholar]
- 38.Atkins JH, Rubenstein SL, Sota TL, et al. Impact of social support on cognitive symptom burden in HIV/AIDS. AIDS Care. 2010 Jul;22(7):793–802. doi: 10.1080/09540120903482994. [DOI] [PubMed] [Google Scholar]
- 39.Grosso A. Social support as a predictor of HIV testing in at-risk populations: a research note. J Health Hum Serv Adm. 2010 Summer;33(1):53–62. [PubMed] [Google Scholar]
- 40.McCoy SI, Strauss RP, MacDonald PD, et al. Social support and delays seeking care after HIV diagnosis, North Carolina, 2000–2006. AIDS Care. 2009 Sep;21(9):1148–56. doi: 10.1080/09540120902730021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Shippy RA, Karpiak SE. The aging HIV/AIDS population: fragile social networks. Aging Ment Health. 2005 May;9(3):246–54. doi: 10.1080/13607860412331336850. [DOI] [PubMed] [Google Scholar]
- 42.Shippy RA, Karpiak SE. Perceptions of support among older adults with HIV. Research on Aging. 2005;27( 3):290–306. [Google Scholar]
- 43.Grov C, Golub SA, Parsons JT, et al. Loneliness and HIV-related stigma explain depression among older HIV-positive adults. AIDS Care. 2010;16:1–10. doi: 10.1080/09540120903280901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Shankar A, McMunn A, Banks J, Steptoe A. Loneliness, social isolation, and behavioral and biological health indicators in older adults. Health Psychol. 2011;30(4):377–385. doi: 10.1037/a0022826. [DOI] [PubMed] [Google Scholar]
- 45.Segrin C, Domschke T. Social support, loneliness, recuperative processes, and their direct and indirect effects on health. Health Commun. 2011;26(3):221–232. doi: 10.1080/10410236.2010.546771. [DOI] [PubMed] [Google Scholar]
- 46.Perissinotto CM, Stijacic Cenzer I, Covinsky KE. Loneliness in older persons: a predictor of functional decline and death. Arch Intern Med. 2012 Jul 23;172(14):1078–84. doi: 10.1001/archinternmed.2012.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kovner CT, Mezey M, Harrington C. Who cares for older adults? Workforce implications of an aging society. Health Aff (Millwood) 2002 Sep-Oct;21(5):78–89. doi: 10.1377/hlthaff.21.5.78. [DOI] [PubMed] [Google Scholar]
- 48.Katz MH, Cunningham WE, Fleishman JA, et al. Effect of case management on unmet needs and utilization of medical care and medications among HIV-infected persons. Ann Intern Med. 2001 Oct 16;135(8 Pt 1):557–65. doi: 10.7326/0003-4819-135-8_part_1-200110160-00006. [DOI] [PubMed] [Google Scholar]
- 49.Dickens AP, Richards SH, Greaves CJ, Campbell JL. Interventions targeting social isolation in older people: a systematic review. BMC Public Health. 2011 Aug 15;11:647. doi: 10.1186/1471-2458-11-647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Selwyn PA, Goulet JL, Molde S, et al. HIV as a chronic disease: implications for long-term care at an AIDS-dedicated skilled nursing facility. J Urban Health. 2000 Jun;77(2):187–203. doi: 10.1007/BF02390530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Linsk NL, Marder RE. Medical social work long-term care referrals for people with HIV infection. Health Soc Work. 1992 May;17(2):105–15. doi: 10.1093/hsw/17.2.105. [DOI] [PubMed] [Google Scholar]
- 52.Wolinsky FD, Callahan CM, Fitzgerald JF, Johnson RJ. The risk of nursing home placement and subsequent death among older adults. J Gerontol. 1992 Jul;47(4):S173–82. doi: 10.1093/geronj/47.4.s173. [DOI] [PubMed] [Google Scholar]
- 53.Gaugler JE, Duval S, Anderson KA, Kane RL. Predicting nursing home admission in the U.S: a meta-analysis. BMC Geriatr. 2007 Jun 19;7:13. doi: 10.1186/1471-2318-7-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wong A, Elderkamp-de Groot R, Polder J, van Exel J. Predictors of long-term care utilization by Dutch hospital patients aged 65+ BMC Health Serv Res. 2010 May 6;10:110. doi: 10.1186/1472-6963-10-110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. [Accessed March 18, 2013];The VACS Index – Summary of Evidence as of May 2012. Available on the VACS website at: http://www.vacohort.org/welcome/75_144255_Summary%20of%20Evidence%20Supporting%20Veterans%20Aging%20Cohort%20Study%20Index%20as%20of%20Jan%2024%202013.doc.
- 56.McQueen DV, Celentano DD. Social factors in the etiology of multiple outcomes: the case of blood pressure and alcohol consumption patterns. Soc Sci Med. 1982;16(4):397–418. doi: 10.1016/0277-9536(82)90049-1. [DOI] [PubMed] [Google Scholar]