Abstract
The aim of this study is to estimate the prevalence of Trichomonas vaginalis and Candida albicans in low-risk patients treated at a first level clinic (primary health care represents the first level of contact of individuals, families, and the community with the system national health). Using a cross-sectional study in patients treated in clinical laboratory of the Sanitary District no. 7 of the city of Orizaba during the months June-July, 252 urine samples were collected for the identification of T. vaginalis and C. albicans by PCR. Furthermore, we analyzed the sociodemographic characteristics of the studied population. We observed an overall prevalence of 23.41% (95% CI 22.10–24.72) for T. vaginalis and 38.88% (95% CI 37.73–40.03) for C. albicans. There was also presence of coinfection in 14.28% (95% CI 13.10–15.46), which was associated with the presence of pain. Most of the positive cases were observed in women house-maker (80%, 95% CI 50.36–48.98). The results of this study provide evidence that the majority of positive cases observed in the studied population are presented in an asymptomatic form and usually are not associated with any risk factor.
1. Introduction
Sexually transmitted infections (STIs) are the second leading cause of morbidity in young women in developing countries, after causes related to pregnancy and childbirth [1]. It is estimated that the number of people suffering from curable STIs in the world per year is approximately 340 million. Among the STIs considered curable by World Health Organization (WHO) [2] stand out those caused by etiological agents Neisseria gonorrhoeae, Chlamydia trachomatis, and Trichomonas vaginalis [3]. The impact of these STIs as a public health problem occurs not only for its high prevalence, but also due to the evolution of these infections in an acute phase and in a chronic phase with sequelae due to a lack of accurate diagnosis and appropriate treatment: the pelvic inflammatory processes, perinatal morbidity, and infertility [1]. T. vaginalis is a flagellated, parasitic protozoan, which causes trichomoniasis by infecting urogenital tract. Trichomoniasis is one of the most common causes of nonviral genitourinary sexually transmitted infection (STI) in humans, with a worldwide prevalence of 174 million cases annually. According to WHO estimation, it accounts for almost half of all curable STIs [3]. In spite of high prevalence, it is one of the poorly studied parasites with respect to virulence properties, pathogenesis, and immunopathogenesis. T. vaginalis infection is asymptomatic in about 50% of infected women and in over 90% of men; thus, re-infection and reexposure is problematic. Furthermore, coinfections among these three STIs are common [4].
C. albicans is a dimorphic fungus that colonizes different areas of the body from the gastrointestinal tract to oral and vaginal mucosa. It is usually a commensal microorganism but in immunocompromised or otherwise debilitated hosts it can cause disseminated and mucosal candidiasis [5]. Candida species are the second most common cause of vulvovaginitis worldwide. The prevalence of vulvovaginal candidiasis (VVC) is increasing due to the extensive utilization of broad-spectrum antibiotics as well as increased cases of immunocompromised patients; C. albicans is the most common and clinically relevant species, that is, present in 85–90% of VVC [6]. However, there has been a significant trend towards the emergence of other species, which ironically show more resistance to the first line antifungal treatments [7]. As Trichomonas prevalence depends on factors such as age, number of sexual partners, and pattern of sexual activity, a better understanding of the local epidemiology of the infection in women would be useful in planning prevention strategies [8]. In 2010, 124,310 cases for T. vaginalis were reported in Mexico and 293,530 candidiasis cases, with a higher incidence in 25- to 44-year-old persons and a national incidence rate of 114.68/100,000 and 270.79/100,000 in habitants, respectively, where the state of Veracruz was ranked in first place in the number of cases for both infections, with an incidence rate of 224.5/100,000 for trichomoniasis and 480.4/100,000 for candidiasis [9]. Shortages of basic data on the true incidence and prevalence of STIs do not allow reliable information to estimate the impact of the transmission of these diseases. The aim of this study was to estimate by PCR the prevalence of T. vaginalis and C. albicans and to describe trends of positiveness in patients attending at a first level clinic in Orizaba, Veracruz, Mexico.
2. Materials and Methods
2.1. Study
The cross-sectional study was conducted on patients, who received attention in the clinical laboratories of the health jurisdiction VII from Orizaba, Veracruz, between June 19, 2012 and July 10, 2012. Those who provided written informed consent were enrolled in this study. Patients treated at this clinic come from various locations all belonging to the state of Veracruz (Figure 1). Sociodemographic characteristics and gynecological complaints were obtained in private using structured questionnaires applied by one investigator. Criteria for inclusion in this study were belonging to the clinic population, being within the mentioned age group, and voluntariness of the patient. Exclusion criteria were patient refusal and inability to give informed consent. All participants provided a sample of 10 mL urine collected in the morning. The samples were received in the laboratory of the sanitary jurisdiction and stored at −20°C and transported to LADISER Inmunología y Biología Molecular for further processing.
Figure 1.
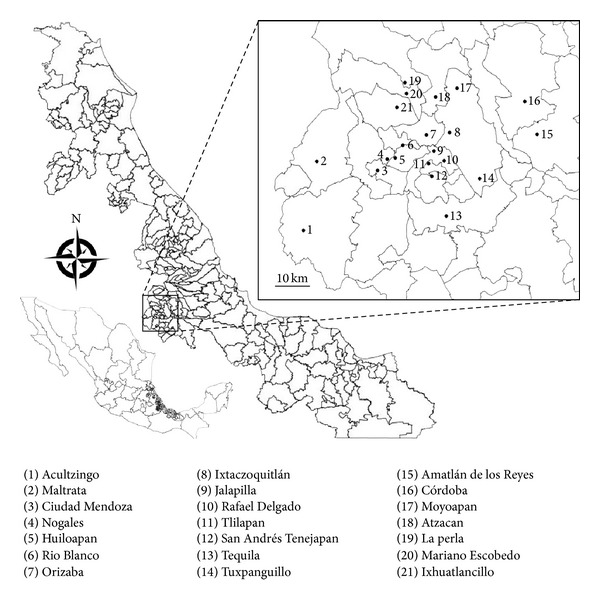
Mexico (bottom left), the state of Veracruz (center), and the study area (inset). Lines delimitating the respective municipalities. (1)–(21), indicate the name of the villages in the different municipalities.
2.2. Obtaining DNA of Urine Samples
252 urine samples were collected. The patient was also asked to provide 10 mL of urine which was pelleted in its entirety at 2,000 ×g for 10 min, the supernatant was removed, and the pellet was rinsed in 1 mL of phosphate buffered saline (PBS (137 mM NaCl, 2.7 mM KCl, 4.3 mM Na2HPO4, 1.4 mM KH2PO4, pH 7.4)) and repelleted at 2,000 ×g for 10 min. The supernatant was discarded, and the pellet was frozen at −20°C. DNA was extracted as previously described with some modification [10]. Briefly, thawed samples were resuspended in 600 μL of lysis buffer (1 M Tris, 0.5 M EDTA, 10% glucose, and lysozyme 2 mg/mL), heated at 80°C for 5 min, and then cooled to room temperature. The samples were RNase treated (Promega, Madison, WI, USA) (0.5 mg/mL) for 1 h at 37°C. Proteins were precipitated with 0.2 N NaOH, 1% sodium dodecyl sulfate, 5 M CH3COOK (pH 4.8) for 5 min on ice and then centrifuged for 3 min at 2,000 ×g. DNA was precipitated with 600 μL of isopropanol and then centrifuged for 3 min at 2,000 ×g, and then the DNA pellet was washed with 600 μL of 70% ethanol and centrifuged for 3 min at 2,000 ×g. The DNA pellet was dried, resuspended in 50 μL of 10 mM Tris (pH 7.4), 1 mM EDTA (pH 8.0), and heated at 65°C for 1 h. The presence of genomic DNA was confirmed in each sample by electrophoresis prior to PCR amplification.
2.3. PCR for T. vaginalis and C. albicans
T. vaginalis-specific primers TV3 (5′-ATT GTC GAA CAT TGG TCT TAC CCT C-3′) and TV7 (5′-TCT GTG CCG TCT TCA AGT ATG C-3′) [11] and C. albicans-specific primers Calb-1 (5′-AAG TAT TTG GGA GAA GGG AAA GGG-3′) and Calb-2 (5′-AAA ATG GGC ATT AAG GAA AAG AGC-3′) [12] were used for PCR amplification. The PCR mixture consisted of 5 μL of 10 x PCR buffer, 4 μL of deoxynucleoside triphosphates (2.5 mM each), 0.5 μL of each primer pair (10 pmol/μL), 0.5 μL of Taq DNA polymerase (Promega) (5 U/mL), 10 μL of sample (5 to 10 ng/mL), and 29.5 μL of distilled water. Positive and negative controls were included in all PCR runs. The positive control consisted of DNA from ATCC T. vaginalis isolate 30184 and ATCC C. albicans isolate 18804. Negative controls included DNA from T. cruzi MHOM/MX/1994/INC-1 strain, PCR mix with primers but no DNA, and human genomic DNA. PCR amplification consisted of 30 cycles of 1 min at 90°C, 30 s at 60°C, and 2 min at 72°C for T. vaginalis, and 40 cycles of 60 s at 94°C, 30 s at 55°C, and 45 s at 62°C for C. albicans. After amplification, there was an additional extension step at 72°C for 7 min, and then the samples were cooled to 4°C. Five microliters of amplified product was electrophoresed on a 1.8% agarose, 0.5 mg/mL ethidium bromide gel, viewed on a UV light box, and photographed. Samples containing a 300 bp fragment were considered positive for T. vaginalis, and samples containing a 310 bp fragment were considered positive for C. albicans.
2.4. Statistical Methods
Frequency distribution of demographic data, characteristics of the population, sexual history, and clinical manifestations were analyzed. The relationship between selected risk factors and the prevalence of trichomoniasis and candidiasis were compared using χ 2 or Fisher's exact test when appropriate. Ninety-five percent confidence intervals were calculated to evaluate statistically significant differences between collection methods. The relationship between age and seroprevalence rate was assessed by chi-square test and by regression analysis. All municipalities were referenced and the data were entered into a geographical information system database in Qgis version 1.8 to generate maps.
3. Results
The 252 samples were divided into 7 age groups (Table 1), age of the participants ranged from 14 to 90 years old, the group between 21 and 30 years had more number of samples: 46 samples (18.25%); education level showed that from the total studied population, 34.52% (CI 95% 33.01–36.03) have elementary school, 27.77% (CI 95% 25.97–29.57) have secondary education, 20.23% (CI 95% 18.31–22.18) have high school education, 4.36% (CI 95% 3.05–5.67) have university studies, and 0.39% (CI 95% −0.35–1.09) have postgraduate studies. In relation to marital status, 33.73% (CI 95% 32.82–34.64) declared to remain single, 35.31% (CI 95% 34.02–36.6) reported being married, and 30.95% (CI 95% 29.86–32.04) said that they are living together, being divorced, or widowed.
Table 1.
Socioeconomic characteristics and sexual behavior of the studied population.
| Age groups (years) | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 14–20 | 21–30 | 31–40 | 41–50 | 51–60 | 61–70 | >71 | Total | |||||||||
| N | (%) | N | (%) | N | (%) | N | (%) | N | (%) | N | (%) | N | (%) | N | (%) | |
| Schooling | ||||||||||||||||
| No study | 0 | — | 2 | 0.793 | 2 | 0.793 | 6 | 2.380 | 7 | 2.574 | 8 | 2.941 | 7 | 2.778 | 32 | 12.698 |
| Elementary | 1 | 0.397 | 9 | 3.571 | 12 | 4.761 | 13 | 5.159 | 18 | 6.618 | 24 | 8.823 | 10 | 3.968 | 87 | 34.524 |
| Secondary | 25 | 9.921 | 11 | 4.365 | 11 | 4.365 | 10 | 3.968 | 8 | 2.941 | 5 | 1.838 | 0 | — | 70 | 27.778 |
| High school | 17 | 6.746 | 17 | 6.746 | 6 | 2.380 | 4 | 1.587 | 6 | 2.206 | 0 | — | 1 | 0.397 | 51 | 20.238 |
| University | 1 | 0.397 | 6 | 2.381 | 3 | 1.190 | 1 | 0.397 | 0 | — | 0 | — | 0 | — | 11 | 4.365 |
| Postgraduate | 0 | — | 1 | 0.397 | 0 | — | 0 | — | 0 | — | 0 | — | 0 | — | 1 | 0.397 |
| Total | 44 | 17.460 | 46 | 18.253 | 34 | 13.492 | 34 | 13.492 | 39 | 15.476 | 37 | 14.682 | 18 | 7.142 | 252 | 100 |
| Marital status | ||||||||||||||||
| Single | 20 | 7.936 | 10 | 3.968 | 11 | 4.365 | 13 | 5.158 | 11 | 4.365 | 14 | 5.556 | 6 | 2.380 | 85 | 33.730 |
| Married | 8 | 3.174 | 17 | 6.746 | 15 | 5.952 | 11 | 4.365 | 23 | 9.126 | 11 | 4.365 | 4 | 1.587 | 89 | 35.317 |
| Other | 16 | 6.349 | 19 | 7.539 | 8 | 3.174 | 10 | 3.968 | 5 | 1.984 | 12 | 4.761 | 8 | 3.174 | 78 | 30.952 |
| Total | 44 | 17.460 | 46 | 18.253 | 34 | 13.492 | 34 | 13.492 | 39 | 15.476 | 37 | 14.682 | 18 | 7.142 | 252 | 100 |
| History of STIs | ||||||||||||||||
| Yes | 1 | 0.396 | 1 | 0.396 | 1 | 0.396 | 1 | 0.396 | 4 | 1.587 | 0 | — | 1 | 0.396 | 9 | 3.571 |
| No | 43 | 17.063 | 45 | 17.857 | 33 | 13.095 | 33 | 13.095 | 35 | 13.888 | 37 | 14.682 | 17 | 6.746 | 243 | 96.428 |
| Total | 44 | 17.460 | 46 | 18.253 | 34 | 13.492 | 34 | 13.492 | 39 | 15.476 | 37 | 14.682 | 18 | 7.142 | 252 | 100 |
| Smoking | ||||||||||||||||
| Smoker | 0 | — | 3 | 1.190 | 1 | 0.396 | 3 | 1.190 | 1 | 0.396 | 0 | — | 0 | — | 8 | 3.174 |
| Ex-smoker | 6 | 2.380 | 6 | 2.380 | 1 | 0.396 | 4 | 1.587 | 5 | 1.984 | 7 | 2.777 | 7 | 2.777 | 36 | 14.285 |
| Nonsmoker | 37 | 14.682 | 38 | 15.079 | 32 | 12.698 | 30 | 11.904 | 31 | 12.301 | 29 | 11.507 | 11 | 4.365 | 208 | 82.539 |
| Total | 44 | 17.460 | 46 | 18.253 | 34 | 13.492 | 34 | 13.492 | 39 | 15.476 | 37 | 14.682 | 18 | 7.142 | 252 | 100 |
| Consumption of alcohol | ||||||||||||||||
| Yes | 21 | 8.333 | 21 | 8.333 | 12 | 4.761 | 13 | 5.158 | 12 | 4.761 | 14 | 5.556 | 6 | 2.380 | 99 | 39.285 |
| No | 23 | 9.126 | 25 | 9.920 | 22 | 8.730 | 21 | 8.333 | 27 | 10.714 | 23 | 9.126 | 12 | 4.761 | 153 | 60.714 |
| Total | 44 | 17.460 | 46 | 18.253 | 34 | 13.492 | 34 | 13.492 | 39 | 15.476 | 37 | 14.682 | 18 | 7.142 | 252 | 100 |
| Sexual partners | ||||||||||||||||
| One | 20 | 7.936 | 23 | 9.126 | 18 | 7.142 | 14 | 5.556 | 23 | 9.126 | 21 | 8.333 | 8 | 3.174 | 127 | 50.396 |
| Two | 11 | 4.365 | 14 | 5.556 | 4 | 1.587 | 9 | 3.571 | 6 | 2.380 | 7 | 2.777 | 3 | 1.190 | 54 | 21.428 |
| More than two | 7 | 2.777 | 8 | 3.174 | 9 | 3.571 | 10 | 3.968 | 8 | 3.174 | 9 | 3.571 | 7 | 2.777 | 58 | 23.015 |
| None | 1 | 0.397 | 0 | — | 1 | 0.397 | 0 | — | 0 | — | 0 | — | 0 | — | 2 | 0.793 |
| Total | 44 | 17.460 | 46 | 18.253 | 34 | 13.492 | 34 | 13.492 | 39 | 15.476 | 37 | 14.682 | 18 | 7.142 | 252 | 100 |
| Condom use | ||||||||||||||||
| Yes | 5 | 1.984 | 4 | 1.587 | 3 | 1.190 | 1 | 0.397 | 1 | 0.397 | 0 | — | 0 | — | 14 | 5.556 |
| No | 39 | 15.476 | 42 | 16.666 | 31 | 12.302 | 33 | 13.095 | 38 | 15.079 | 37 | 14.683 | 18 | 7.143 | 238 | 94.444 |
| Total | 44 | 17.460 | 46 | 18.253 | 34 | 13.492 | 34 | 13.492 | 39 | 15.476 | 37 | 14.682 | 18 | 7.142 | 252 | 100 |
N: samples.
In order to establish a history about the presence of STIs in this study group, they were questioned whether they had ever suffered at least one STI in their lives; 96.42% (CI 95% 73.81–119.02) reported not having had an STI; the remaining 9 participants (3.57%, CI 95% 2.76–4.38) agreed to have suffered at least one STI but did not reveal the causal agent of it. Similarly, they were asked whether they regularly used condoms in their sexual relations; 5.55% (9/252, CI 95% 4.51–6.59) have indicated consistent condom use. In relation to smoking and consumption of alcohol, 3.17% (8/252, CI 95% 2.24–4.10) of the studied population is smokers, and 99/252 of them (39.28%, CI 95% 38.23–40.33) consume alcohol.
Finally, in relation to the number of sexual partners, 50.39% (127/252, CI 95% 49.45–51.33) mentioned to have only one partner, 21.42% (54/252, CI 95% 20.38–22.46) mentioned to have two sexual partners, 23.01% (58/252, CI 95% 22.73–23.29) mentioned to have more than two sexual partners, and 0.79% (2/252, CI 95% 0.12–1.46) did not mention sexual partners. 18.65% (47/252, CI 95% 17.87–19.43) mentioned a family history of cancer, and only 23.41% (59/252, CI 95% 22.22–24.60) of the patients have expressed discomfort (burning, itching, and vaginal secretion).
All 252 samples were used to identify the presence of T. vaginalis and C. albicans by PCR; molecular diagnosis of T. vaginalis showed an overall prevalence of 23.41% (59/252, CI 95% 22.10–24.72) (Table 2); all positive samples showed an amplification of 300 bp, finding a mean age of 43.3 years for patients positive for T. vaginalis. When we analyzed the presence of C. albicans genomic material in the 252 studied samples, 38.88% (98/252, CI 95% 37.73–40.03) (Table 2) samples resulted positive for amplification of 310 bp fragment specific for C. albicans, with an average age of 41.9 years, for patients who tested positive for the presence of C. albicans. When we analyzed the presence of coinfections, 14.28% (36/252, CI 95% 13.10–15.46) of the samples resulted positive, where 11.11% (28/252, CI 95% 10.16–12.06) turned out to be women devoted to housework and 3.17% (8/252, CI 95% 2.01–4.33) of co-infections were found in samples from men. The presence of co-infection (18/82) was associated with the presence of pain (32.5% versus 67.4%) (χ 2 = 4.942, degrees of freedom = 2, P = 0.026 with Yate's corrections). Moreover, of the total number of samples analyzed, 83.3% (210/252) correspond to samples of women, from which 80% (168/210, CI 95% 79.30–80.69) have as occupation housework. Surprisingly, in this group there are 41 samples of the 59 cases positive for T. vaginalis and 62 of the 98 cases positive for C. albicans, being a high percentage of the total positive samples, 16.26% (41/252, CI 95% 15.18–17.34) and 24.6% (62/252, CI 95% 23.77–25.43) for T. vaginalis and C. albicans, respectively, in an age range between 51 and 60 years, while 2.77% (7/252) of T. vaginalis positive cases and 6.34% (16/252) of the cases for C. albicans from the women group who are predominantly students in an age range of 14 to 20 years. However, during the association analysis between the occupation and the presence of infection, there existed no significant correlation with infection with T. vaginalis (P = 0.410, by Fisher's exact test) or infection with C. albicans (P = 1.0, by Fisher's exact test). It is noteworthy that positive male samples for T. vaginalis (11/59), representing 4.3% (11/252, 95% CI 3.14–5.58) of the total studied population, are at an age range above 42 years. Of the total female population (210/252), the 35.71% (75/210, CI 95% 32.24–39.07) were pregnant, of which 7.14% (15/210, CI 95% 5.79–8.49) were positive to T. vaginalis, 10.95% (23/210, CI 95% 9.06–12.84) were positive to C. albicans, and 5.23% (11/210, CI 95% 3.79–6.67) with a codetection of both pathogens; however, the presence of infection did not correlate with any risk factors.
Table 2.
Age groups and positivity to T. vaginalis and C. albicans by PCR in urine samples.
| Age (years) | Samples | Positive T. vaginalis | Negative T. vaginalis | Positive C. albicans | Negative C. albicans | Double positive | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | N | % | N | % | |
| 14–20 | 44 | 17.460 | 8 | 3.175 | 36 | 14.286 | 21 | 8.333 | 23 | 9.127 | 7 | 2.778 |
| 21–30 | 46 | 18.254 | 11 | 4.365 | 35 | 13.889 | 12 | 4.762 | 34 | 13.492 | 5 | 1.984 |
| 31–40 | 34 | 13.492 | 5 | 1.984 | 29 | 11.509 | 11 | 4.365 | 23 | 9.127 | 2 | 0.794 |
| 41–50 | 34 | 13.492 | 6 | 2.381 | 28 | 11.111 | 19 | 7.540 | 15 | 5.952 | 4 | 1.587 |
| 51–60 | 39 | 15.476 | 17 | 6.746 | 22 | 8.730 | 18 | 7.143 | 21 | 8.333 | 11 | 4.365 |
| 61–70 | 37 | 14.683 | 11 | 4.365 | 26 | 10.317 | 13 | 5.159 | 24 | 9.524 | 7 | 2.778 |
| >71 | 18 | 7.143 | 1 | 0.397 | 17 | 6.746 | 4 | 1.587 | 14 | 5.556 | 0 | — |
|
| ||||||||||||
| Total | 252 | 100 | 59 | 23.413 | 193 | 76.587 | 98 | 38.889 | 154 | 61.111 | 36 | 14.286 |
N: samples.
The stratification of patients indicated a significant difference in infection rate (T. vaginalis) according to age (χ 2 = 32.8, degrees of freedom = 6, P = 0.0001), as well as for C. albicans (χ 2 = 50.4, degrees of freedom = 6, P = 0.0001); however, prevalence rate was not significantly correlated with age (r 2 = 0.207, P = 0.97, by second-order polynomial regression) for T. vaginalis infection, as well as (r 2 = 0.234, P = 0.55 by second-order polynomial regression) for C. albicans infection; for both infections there was no association with marital status of participants (single versus married) (P = 0.729 for T. vaginalis infection, P = 0.466 for C. albicans infection, by Fisher's exact tests); there was no statistically significant association between the presence of infection with alcohol consumption (P = 0.761 for T. vaginalis infection, P = 1.000 for C. albicans infection, by Fisher's exact tests); when smoking was analyzed as a risk factor in this population, the results showed that the consumption of snuff (smoker, ex-smoker, and nonconsumer of snuff) had no association with the presence of infection for T. vaginalis (χ 2 = 0.906, degrees of freedom = 2, P = 0.636), as well as (χ 2 = 0.674, degrees of freedom = 2, P = 0.714) for C. albicans infection. Moreover, the presence of discomfort (burning, itching, and vaginal secretion) had no association with the presence of infections (P = 0.169 for T. vaginalis infection, P = 0.761 for C. albicans infection, by Fisher's exact tests). Finally, a significant association in the number of sexual partners (two versus more than two) was observed for T. vaginalis infection (P = 0.047, by Fisher's exact test) but not for C. albicans infection (P = 0.248, by Fisher's exact test).
4. Discussion
The diagnosis of Candida spp is difficult, existing up to 50% of asymptomatic cases, moreover, Candida spp, is considered endogenous flora normal of the vagina, in growth limited conditions [13]; on the other hand, the presence and trichomoniasis symptoms depend on local immunity and the amount of parasites inoculated, and transit may be asymptomatic in 50% of cases [14]. T. vaginalis and C. albicans are considered the pathogens found in a more frequent in vaginal infections. The culture is the gold standard test for diagnosis of C. albicans and T. vaginalis infections in cases of vaginitis [15]; however, PCR is currently used for diagnosis of T. vaginalis and C. albicans obtaining a sensitivity and specificity of 100% [16, 17].
As it is known, the frequency of cases of candidiasis and trichomoniasis varies according to the studied population [18]. In this study, we found a high prevalence rate in cases of trichomoniasis and candidiasis considering that the study was conducted in a low-risk population and that most women were homemakers, in relation to the data reported in Mexico in 2010 for cases of trichomoniasis and candidiasis [9], and compared with different work in different studied populations [19–22], even in high-risk populations such as sex workers [23]. Moreover, unlike other reports, this study found cases in all age groups, with a larger number of cases for T. vaginalis in people over 50 years old, and cases of candidiasis were observed in almost the same way in all groups with a slight increase in the group of 21–30 years.
Risk factors for acquisition, the clinical characteristics, and significance of candiduria have been published primarily in relation to intensive care unit and immunocompromised. Diabetes mellitus, prolonged use of antibacterial agents, indwelling urinary catheter, genitourinary tuberculosis, chronic renal failure, malignancy, neutropenia, immunosuppressive therapy, urinary tract instrumentation, surgery, renal graft, female sex, and extremes of age are known risk factors of acquisition of candiduria [24]. Moreover, the presence of Candida in urine may represent contamination of clinical sample, actual colonization of the lower urinary tract, or may be a true indicator of invasive infection of lower and/or upper urinary tract [25]; also, the epidemiology of Candida infections has changed over the last two decades. The number of patients suffering from such infections has increased dramatically and the Candida species involved have become more numerous [26].
A feature of this study is that the majority of participants reported no history of STIs submitted; furthermore, there was no relationship between the presence of positive case and the presence of symptoms, only in the case of coinfections (14%) where a significant association with the presence of pain was observed, these results indicated that the majority of individual infections with T. vaginalis and/or C. albicans remain in an asymptomatic form; presumably because pathogens can remain in low concentrations. These results strongly suggest that the symptoms not always must be a secure evidence of disease [27]. A limitation of this study was that most of the participants were women; only 16.6% of the population were males, a population where infection with T. vaginalis and generally any STI has been difficult to characterize [28]. But despite the low participation of the population, samples were positive for both pathogens, and in some cases in the presence of co-infections, these findings reinforced the absence of symptoms plus the presence of asymptomatic cases of this type of infection. Perhaps the lack of laboratory techniques for an accurate diagnosis, as well as early confirmation, is what affects the permanence of the infection as well as the likelihood of having any of the serious and important consequences caused by these pathogens.
The sociocultural and educational levels are crucial in sexual behavior and the risk of STIs, if you consider this aspect to be able to identify risk factors for use in these populations in intervention programs to change the sexual behavior of these people [29]. However, in this studied population not determining factors for the presence of infections was present. In addition, there is some degree of promiscuity not clearly detected in the survey because the partner or husband could not be interviewed; however, possessing more than one partner was significant in the presence of infection as previously reported [30].
One of the most common associations with T. vaginalis is the presence of bacteria and Candida spp [31], and the data obtained in the group of pregnant women showed no association with the presence of infection risk factors analyzed (pain, history of STIs, itching and vaginal secretion, smoking, alcohol, etc.), but the association was observed with C. albicans. It is known that environmental changes such as increased glycogen production during pregnancy and altered levels of estrogen and progesterone, by the use of oral contraceptives, allow adherence of C. albicans to vaginal epithelial cells and facilitate germination of yeast [32]. These changes can transform asymptomatic colonization in symptomatic infection. Patients with changes in the level of estrogens and progesterone, as well as raising the pH and glycogen, can cause the growth and virulence of T. vaginalis [32, 33]. Hormone changes produced during pregnancy predispose a higher incidence of infections of the lower genital tract. This leads to maternal and perinatological complications. The diagnosis of T. vaginalis infection during pregnancy is of great importance as such infections are related to premature rupture of membranes, preterm delivery, and low birth weight [34].
5. Conclusion
In conclusion, the codetection of T. vaginalis and C. albicans by PCR in urine samples in a low-risk population attended in a clinic first level in central Veracruz, Mexico, is of great importance because the diversity of results observed in this study enrich the evidence that the etiology of this type of infection is variable and requires the individual studies to know the characteristics of the population with which they are working.
Acknowledgment
The authors appreciate the support provided by Jurisdicción Sanitaria no. 7 for obtaining samples.
References
- 1.van Dam CJ. HIV, STD and their current impact on reproductive health: the need for control of sexually transmitted diseases. International Journal of Gynecology and Obstetrics. 1995;50(supplement 2):S121–S129. doi: 10.1016/0020-7292(95)02499-3. [DOI] [PubMed] [Google Scholar]
- 2.OMS. Global Strategy for the Preventions and Control of Sexually Transmitted Infections. Genebra, Switzerland: OMS; 2006. [Google Scholar]
- 3.WHO. First WHO Report on Neglected Tropical Diseases: Working to Overcome the Global Impact of Neglected Tropical Diseases. Geneva, Switzerland: WHO; 2011. [Google Scholar]
- 4.Sobngwi-Tambekou J, Taljaard D, Nieuwoudt M, Lissouba P, Puren A, Auvert B. Male circumcision and Neisseria gonorrhoeae, Chlamydia trachomatis and Trichomonas vaginalis: observations after a randomised controlled trial for HIV prevention. Sexually Transmitted Infections. 2009;85(2):116–120. doi: 10.1136/sti.2008.032334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vecchiarelli A, Pericolini E, Gabrielli E, Pietrella D. New approaches in the development of a vaccine for mucosal candidiasis: progress and challenges. Frontiers in Microbiology. 2012;3(294):1–7. doi: 10.3389/fmicb.2012.00294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chaim W, Mazor M, Sobel JD. Candida albicans vulvovaginitis-trends in care and implications. Harefuah. 1997;133(1-2):40–43. [PubMed] [Google Scholar]
- 7.Mahmoudi Rad M, Zafarghandi A, Amel Zabihi M, Tavallaee M, Mirdamadi Y. Identification of Candida species associated with vulvovaginal candidiasis by multiplex PCR. Infectious Diseases in Obstetrics and Gynecology. 2009;2012 doi: 10.1155/2012/872169.872169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Helms DJ, Mosure DJ, Metcalf CA, et al. Risk factors for prevalent and incident Trichomonas vaginalis among women attending three sexually transmitted disease clinics. Sexually Transmitted Diseases. 2008;35(5):484–488. doi: 10.1097/OLQ.0b013e3181644b9c. [DOI] [PubMed] [Google Scholar]
- 9.SINAVE/DGE/SALUD/Información Epidemiológica de morbilidad. Secretaria de Salud, 2011.
- 10.Shen AL, Porter TD, Wilson TE, Kasper CB. Structural analysis of the FMN binding domain of NADPH-cytochrome P-450 oxidoreductase by site-directed mutagenesis. Journal of Biological Chemistry. 1989;264(13):7584–7589. [PubMed] [Google Scholar]
- 11.Kengne P, Veas F, Vidal N, Rey JL, Cuny G. Trichomonas vaginalis: repeated DNA target for highly sensitive and specific polymerase chain reaction diagnosis. Cellular and Molecular Biology. 1994;40(6):819–831. [PubMed] [Google Scholar]
- 12.Baquero C, Montero M, Sentandreu R, Valentin E. Identification of Candida albicans by polymerase chain reaction amplification of a CaYST1 gene intron fragment. Revista Iberoamericana de Micologia. 2002;19(2):80–83. [PubMed] [Google Scholar]
- 13.Ziarrusta BG. Vulvovaginitis candidiásica. Revista Iberoamericana de Micología. 2002;19:22–24. [PubMed] [Google Scholar]
- 14.Plourd DM. Practical guide to diagnosing and treating vaginitis. Medscape Women's Health. 1997;2:p. 2. [PubMed] [Google Scholar]
- 15.Boeke AJP, Dekker JH, Peerbooms PGH. A comparison of yield from cervix versus vagina for culturing Candida albicans and Trichomonas vaginalis . Genitourinary Medicine. 1993;69(1):41–43. doi: 10.1136/sti.69.1.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Devillard E, Burton JP, Reid G. Complexity of vaginal microflora as analyzed by PCR denaturing gradient gel electrophoresis in a patient with recurrent bacterial vaginosis. Infectious Disease in Obstetrics and Gynecology. 2005;13(1):25–30. doi: 10.1080/10647440400025504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schwebke JR, Burgess D. Trichomoniasis. Clinical Microbiology Reviews. 2004;17(4):794–803. doi: 10.1128/CMR.17.4.794-803.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Flores-Paz R, García-Jiménez E, Arriaga-Alba M. Etiología de la infección cérvico vaginal en pacientes del Hospital Juárez de México. Salud Publica de Mexico. 2003;45(supplement 5):S694–S697. [PubMed] [Google Scholar]
- 19.Matini M, Rezaie S, Mohebali M, et al. Prevalence of Trichomonas vaginalis infection in Hamadan City, Western Iran. Iranian Journal of Parasitology. 2012;7:67–72. [PMC free article] [PubMed] [Google Scholar]
- 20.Ginocchio CC, Smith JS, Aslanzadeh J, Snook J, Hill CS, Gaydos CA. Prevalence of Trichomonas vaginalis and coinfection with Chlamydia trachomatis and Neisseria gonorrhoeae in the United States as determined by the Aptima Trichomonas vaginalis nucleic acid amplification assay. Journal of Clinical Microbiology. 2012;50(8):2601–2608. doi: 10.1128/JCM.00748-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Piperaki E, Theodora M, Mendris M, et al. Prevalence of Trichomonas vaginalis infection in women attending a major gynaecological hospital in Greece: a cross-sectional study. Journal of Clinical Pathology. 2010;63(3):249–253. doi: 10.1136/jcp.2009.070920. [DOI] [PubMed] [Google Scholar]
- 22.Pattullo L, Griffeth S, Ding L, et al. Stepwise diagnosis of Trichomonas vaginalis infection in adolescent women. Journal of Clinical Microbiology. 2009;47(1):59–63. doi: 10.1128/JCM.01656-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Haseen F, Hossain ME, Huq M, et al. Sexually transmitted infections and sexual behaviour among youth clients of hotel-based female sex workers in Dhaka, Bangladesh. International Journal of STD & AIDS. 2012;23(8):553–559. doi: 10.1258/ijsa.2012.011373. [DOI] [PubMed] [Google Scholar]
- 24.Fraisse T, Crouzet J, Lachaud L, et al. Candiduria in those over 85 years old: a retrospective study of 73 patients. Internal Medicine. 2011;50(18):1935–1940. doi: 10.2169/internalmedicine.50.5560. [DOI] [PubMed] [Google Scholar]
- 25.Singla N, Gulati N, Kaistha N, Chander J. Candida colonization in urine samples of ICU patients: determination of etiology, antifungal susceptibility testing and evaluation of associated risk factors. Mycopathologia. 2012;174(2):149–155. doi: 10.1007/s11046-011-9514-7. [DOI] [PubMed] [Google Scholar]
- 26.Rodloff AC, Koch D, Schaumann R. Epidemiology and antifungal resistance in invasive candidiasis. European Journal of Medical Research. 2011;16(4):187–195. doi: 10.1186/2047-783X-16-4-187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Anderson MR, Karasz A. How do clinicians manage vaginal complaints? An Internet survey. Medscape General Medicine. 2005;7(2):61–65. [PMC free article] [PubMed] [Google Scholar]
- 28.Munson KL, Napierala M, Munson E, et al. Trichomonas vaginalis male screening with transcription-mediated amplification in a community of high sexually-transmitted infection prevalence. Journal of Clinical Microbiology. 2013;51(1):101–104. doi: 10.1128/JCM.02526-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Periago MR, Fescina R, Ramón-Pardo P. Steps for preventing infectious diseases in women. Emerging Infectious Diseases. 2004;10(11):1968–1973. doi: 10.3201/eid1011.040555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Canchihuaman FA, Carcamo CP, Garcia PJ, et al. Non-monogamy and risk of infection with Chlamydia trachomatis and Trichomonas vaginalis among young adults and their cohabiting partners in Peru. Sexually transmitted infections. 2010;86:37–44. doi: 10.1136/sti.2010.045310. [DOI] [PubMed] [Google Scholar]
- 31.Perazzi BE, Menghi CI, Coppolillo EF, et al. Prevalence and comparison of diagnostic methods for Trichomonas vaginalis infection in pregnant women in Argentina. Korean Journal of Parasitology. 2010;48(1):61–65. doi: 10.3347/kjp.2010.48.1.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Secretaría de Salud. Guía de Práctica Clínica: Diagnóstico y Tratamiento de la Vaginosis Infecciosa en Mujeres en Edad Reproductiva, en el Primer Nivel de Atención. Tamaulipas, Mexico: Secretaría de Salud; 2008. [Google Scholar]
- 33.Owen MK, Clenney TL. Management of vaginitis. American Family Physician. 2004;70(11):2125–2140. [PubMed] [Google Scholar]
- 34.Cotch MF, Pastorek JG, II, Nugent RP, et al. Trichomonas vaginalis associated with low birth weight and preterm delivery. Sexually Transmitted Diseases. 1997;24(6):353–360. doi: 10.1097/00007435-199707000-00008. [DOI] [PubMed] [Google Scholar]


