Abstract
BACKGROUND
Clients with HIV infection have been conceptualized as a resilient population. Although a few researchers have documented resilience among clients with HIV infection, a theory of resilience in the context of HIV infection has not been developed. The purpose of this study was to describe the process by which resilience occurs for clients in the context of HIV infection.
METHOD
Grounded theory methodology was used to sample and analyze data from 15 qualitative interviews with adults with HIV infection. Data were collected until saturation was reached.
RESULTS
A theory, motivation, management, and mastery, a description of the process by which resilience occurs in the context of HIV infection, emerged from the data.
CONCLUSION
Many clients living with HIV infection are resilient, despite the physical, psychological, and social challenges of this chronic illness. Nursing interventions to promote resilience among clients with HIV infection should be directed toward identification of client motivation factors and disease management strategies that may influence health outcomes of people living with HIV infection.
Keywords: AIDS, HIV infection, resilience
Resilience is defined as a process that occurs when an individual is confronted with adversity, yet is able to surmount, respond, and adapt to adversity (Dyer & McGuinness, 1996).
For resilience to occur, an individual must be exposed to adversity or a threat to physical or psychological health. Despite this adversity or threat, the individual adapts without experiencing a risk to development (Luthar, Cicchetti, & Becker, 2000).
Resilience may be influenced by genetics, exposure and experience with adversity, the desire to succeed, the presence of mentors or role models, and prosocial skills that allow the individual to seek support from others (Dyer & McGuinness, 1996). Over the past 30 years, researchers have studied resilience in a number of populations (Georgas et al., 2006; Ungar, 2011). These studies have focused on individual traits, environmental traits, or processes/mechanisms that allow an individual to access these strengths when confronted with adversity (e.g., see Lester, Masten, & McEwen, 2006). However, recently, Ungar (2011) proposed that approaches to resilience should focus more on social and physical ecology and less on individual traits.
Theoretical support for the study of resilience as a process derives from the person–environment view. As a person is confronted with adversity, he or she assesses threats, challenges, and difficulties stemming from the adversity and constructs a protective environment to deal with the adversarial event (Kumpfer, 1999). From this view, resilience is the outcome of a process that most individuals can learn at any point in life when confronted with adversity (Flach, 1980).
Rutter (1985) supported the process approach and proposed that innate characteristics combined with previous experiences mediated the effects of adversity. Fine (1991) defined resilience as a process composed of two stages: the acute stage and the reintegration phase. In the acute stage, adversity creates a threat that the person learns to manage. Once management and adaptation to the threat has occurred, the individual reorganizes their life and incorporates the changes resulting from adversity into their lives, which results in resilience.
During the 1980s and early 1990s when there was few treatment options for HIV infection, persons with HIV were conceptualized as a vulnerable population because of the physical, psychological, and social sequelae of the disease (Flaskerud & Winslow, 1998). With the advent of antiretroviral therapy (ART) in the mid-1990s, HIV was recategorized as a chronic, manageable illness (Mahungu, Rodger, & Johnson, 2009). Adherence to ART decreases morbidity and mortality and dramatically increases the quality of life for clients infected with HIV (Lavalle et al., 2000). In this context, persons with HIV who can successfully manage their illness and live full mean- ingful lives may be viewed as resilient (Gosselink & Myllykangas, 2007; Thompson, 2003). However, despite the advances in HIV treatments and life expectancy, resilience in this population is not consistently defined (De Santis, 2008). In addition, the majority of the research that has been completed has focused on the researchers’ objective perception of resilience and not fully considered the subjective experiences of those experiencing resilience (Luthar et al., 2000).
Review of the Literature
Compared with the extant literature on resilience in children, relatively little is known about resilience among people with HIV. A study of resilience in the context of HIV infection is necessary because of the unique nature of HIV infection. The majority of people contract HIV infection as a result of high-risk sexual behaviors or substance abuse behaviors during adulthood. These behaviors are stigmatized by society (Herek, Capitanio, & Widaman, 2002), and people with HIV infection experience stigma, discrimination, and marginalization because of their diagnosis. No other illness or disease state in recent history has been accompanied by these social factors (Holzemer et al., 2009). Based on these unique factors, a diagnosis of HIV infection creates a unique adversarial situation that may make it more difficult for persons to develop of resilience when compared with other illnesses (Nightingale, Sher, & Hansen, 2010).
When examining resilience in the context of HIV, a majority of the available studies conceptualize resilience as a personal trait rather than a person–context interactional process (Bletzer, 2007; Emlet, Tozay, & Raveis, 2010; Farber, Schwartz, Schaper, Moonen, & McDaniel, 2000; Gosselink & Myllykangas, 2007; Thompson, 2003). Resilient persons with HIV infection differ from those without resilience in a number of ways, including level of knowledge of their illness, self-responsibility, persistence (Bletzer, 2007), an increased quality of life, low levels of psychological distress, positive beliefs, and the ability to relinquish control over the uncertainty of life with HIV infection (Farber et al., 2000). In addition, some evidence suggests that resilient persons with HIV infection have the ability to spiritually transcend their illness (Gosselink & Myllykangas, 2007).
Another critical gap in the existing knowledge base is evident in that studies that document the processes that promote resilience among people with HIV infection generally have not been conducted. Only one study could be located that used a process approach to describe resilience in the context of HIV infection. Dyer, Patsdaughter, McGuinness, O’Connor, and De Santis (2004) used four exemplar case studies of clients living with HIV infection to describe the process whereby these persons developed therapeutic relationships with their health care providers. The therapeutic relationships fostered and promoted resilience by modeling prosocial skills and assisting the client in developing coping skills.
Another important limitation of studies on resilience in HIV-infected persons is that all available studies detail resilience from the objective descriptions of the researchers and do not include the subjective experience of resilience from the viewpoint of the participants. Therefore, the purpose of this study is to develop a theory grounded in qualitative data that describes the participants’ subjective account of the process by which resilience occurs within the context of HIV infection.
Method
Design
Grounded theory was used to describe the process of resilience in the context of HIV infection. This type of qualitative research is used to generate a theory of an action, process, or interaction among phenomena (Creswell, 2007; Glaser & Strauss, 1967; Strauss & Corbin, 1990). Grounded theory involves a constant comparative method of collecting and coding data, identifying categories, and connecting the categories that generate a theory explaining the process of a phenomenon. The theory that is generated is an abstract description of a process that is grounded in the data (Glaser & Strauss, 1967).
This study is a report of unpublished data on resilience from a larger study of vulnerability and resilience among adults living with HIV infection. The data on vulnerability among adults living with HIV infection are available in De Santis and Barroso (2011).
Sample
Using theoretical sampling, a sample of 15 adults with HIV infection was recruited from a university-based Adult Immunology Research clinic. Theoretical sampling is the intentional sampling of a population with firsthand knowledge of the phenomenon that is used to generate theory (Strauss & Corbin, 1990).
Participants were required to meet eligibility criteria. Inclusion criteria included (a) a self-reported diagnosis of HIV or AIDS, (b) age 18 years or older, and (c) ability to read, write, and speak English.
The sample size for the study was established by saturation of the data. Saturation is a subjective determination made by the researcher that additional data will not result in new information or categories (Glaser & Strauss, 1967). Saturation was achieved by the 13th interview, but two subsequent interviews were completed to ensure consistency among the data. Participants were compensated with US$50 on completion of the interview.
The sample of 15 adults with HIV infection consisted of eight women and seven men ranging in age from 24 to 61 years. The sample consisted of eight Hispanics, six Blacks, and one Caucasian. These participants had lived with HIV infection from 2 to 28 years. Fourteen participants were receiving ART for HIV infection, and 11 participants reported at least one additional diagnosis in addition to HIV infection.
Data Collection
A semistructured interview guide was used to direct data collection. Questions that comprised the interview guide are included in Table 1. Consistent with grounded theory methodology, additional questions were added, deleted, or modified based on previous interviews (Creswell, 2007; Strauss & Corbin, 1990).
Table 1.
Interview Questionsa
People with HIV infection may experience resilience in their lifetime. Resilience occurs when someone is confronted with adversity or something negative happens to them (like being diagnosed with HIV), yet they are about to “bounce back” from this and move forward with their lives.b
|
Interview questions are based on grounded theory methodology as described by Creswell (2007), Glaser and Strauss (1967), and Strauss and Corbin (1990).
Based on Dyer and McGuinness (1996).
The duration of the interviews ranged from 1 to 1.5 hours. Field notes were written at the completion of each interview by the first author. The field notes were used to summarize the interview, list answered questions, and to describe tentative categories. Each interview was then transcribed verbatim by the first author, with assistance from the fourth author.
Ethical Considerations
The study was approved by the university’s institutional review board. Participants signed an informed consent to participate and an additional consent for audio recording of the interviews prior to participation.
To protect the confidentiality of participants, each participant was assigned a number on enrollment. Participants were instructed not to provide their names or other identifying information on the audiotape in order to protect confidentiality. Consents were stored separately from audiotapes and interview transcripts in a double-locked office.
Interviews were carried out in the private, unoccupied office free from interruption. Conducting interviews in a private space was necessary to protect the confidentiality and privacy of the participants as well as to provide a safe environment in which to discuss sensitive topics such as high-risk sexual behaviors and substance abuse behaviors that emerged during the interviews.
Data Analysis
The data were analyzed using techniques consistent with grounded theory methodology (Glaser & Strauss, 1967). Transcribed interviews were read and analyzed by the first author using the constant comparative method. In the first level of analysis, open coding was used to group data into codes. Axial coding was then employed to group the first-level codes into higher level categories and to explore the relationships between the categories. As each additional transcript was read, the transcript was constantly compared with previously analyzed transcripts, which allowed the data to be further grouped into categories and modified as needed. Individual quotes from the interviews were identified that supported categories to ensure credibility of the data and to ensure that the theory that emerged was grounded in the data (Glaser & Strauss, 1967).
Rigor
Two methods were used to establish rigor and to minimize researcher bias during data analysis. These methods were clarifying researcher bias and peer review/debriefing (Creswell, 2007). Clarifying researcher bias was essential because the first author had extensive clinical and research experience with clients with HIV infection. This experience had the potential to influence the study’s results. To decrease bias, two nurses and a physician who were not involved in data collection and who have had limited clinical and research experience with clients with HIV infection were selected to verify categories identified by the first author. The two nurses and the physician had previous experience with qualitative data analysis and verified the categories by comparing the categories with the data.
Peer review/debriefing was conducted by two health care providers specializing in HIV care and who were not involved in the data collection. The results of the study were made available to the health care providers to ensure that data analysis was congruent with clinical experiences in providing care to clients with HIV infection. The comments made by the nurses who assisted in clarifying researcher bias and by the health care providers who assisted with peer review/debriefing were incorporated into the theory that was grounded in the data.
Results
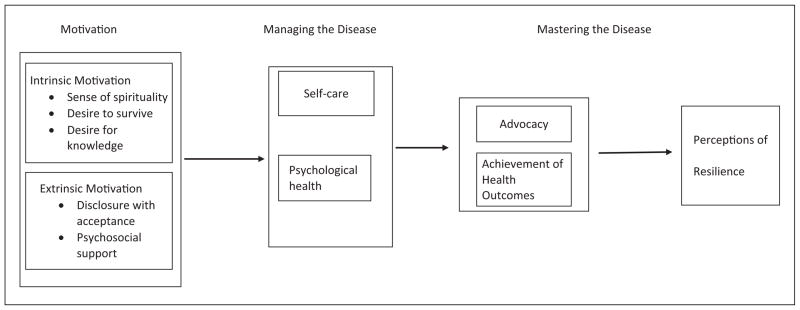
Participants provided rich descriptions of resilience in the context of HIV infection. Selected quotes provided by the participants are used to illustrate the categories and subcategories of the theory. These descriptions illustrating the process of resilience in the context of HIV infection are titled Motivation, Management, and Mastery. This process is presented in Figure 1.
Figure 1. Motivation, management, and mastery.
A theory of resilience in the context of HIV infection
Motivation
Participants reported that the origin of the process of resilience is motivating factors. These motivating factors are both intrinsic and extrinsic to the person living with HIV infection. Participants in this study detailed a number of factors that provided the initial motivation in their progress toward resilience. Motivation includes two subcategories that are called Intrinsic Motivators and Extrinsic Motivators Intrinsic motivators include Sense of Spirituality, Desire to Survive, and Desire for Knowledge. Extrinsic motivators include Disclosure With Acceptance and Psychosocial Support.
Intrinsic Motivators
Sense of spirituality
Spirituality was important to many of the participants and served as a significant intrinsic motivator. Spirituality was expressed as active participation in organized religious services as well as a personal relationship with a higher power, as described by Participant 6, who experienced both substance abuse and bipolar disorder in addition to HIV infection:
I got it [resilience] from church . . . I have always been in the church, and I thank God that is where I am today . . . I thank God for my life. I just thank God that I am sitting here today talking and hoping that my testimony would help somebody else, you know? To bounce back, you just have to give yourself to God and Jesus, you know? There is no other way. I gave it to God . . . I read the Word. I pray every morning. I have a prayer line . . . God is my all and what I am holding on to. That is who I owe my every minute, every moment to my Heavenly Father.
Spirituality for some of the participants equated to “surrendering to a higher power” because many of the participants also struggled with substance abuse. Participants realized the difficulty in abstaining from substance use without some sort of assistance or support. To gain some sense of control of their lives, participants reported the importance of spirituality as a motivator as described by Participant 5, who had experienced substance abuse in addition to HIV infection:
Medicine is not always good for everyone, you know? I feel like it is a miracle for me because I survived. I survived and got better because I believe in God. God is my everything. I don’t go to church or anything or have a religion exactly, you know? But I read the Bible. I believe in God and Christ, you know? I feel [that] I keep my faith. I believe it is a miracle for me. God made me a miracle.
The desire to survive
A second motivator reported by the majority of the participants was the desire to survive. In addition to the diagnosis of HIV, a chronic but potentially fatal illness, these participants stated they often struggled with substance abuse. According to participants, once they wanted to survive, the desire to survive became a motivator. Participant 13 summarized the desire to survive:
So you know, you got to come to the point where you say, “Well hey, I am going to fight this. This does not define me. It does not make me.” But you got to get through the denial stage and that pity party. Is this really happening to me? Getting past the denial and pity, now I want to live. I actually want to live.
Desire for knowledge
Building on all the other motivators, all 15 participants discovered a need to educate themselves about HIV infection. To achieve this education, many participants enrolled in classes and psycho-educational groups offered at the university-based HIV clinic where they received care. The knowledge gained in these classes and groups further motivated participants, as summarized by Participant 6:
What made me bounce back was when I started going to the classes, the adult HIV classes, which gave me the education I needed. That education helped me to improve the qualities in my life ‘cause it taught me what to do, how to do it, what not to do, and what to continue to do to keep me alive.
Extrinsic Motivators
Disclosure with acceptance
An extrinsic factor that served to motivate some of the participants was the willingness to disclose the diagnosis of HIV infection to others, and to receive acceptance from those to whom they had disclosed. According to these participants, disclosing the diagnosis of HIV infection to others was a risk because the potential for rejection existed. Participants stated they chose the person they trusted most to disclose this extremely intimate secret. After disclosing their diagnosis and being accepted by the person to whom they disclosed, participants reported feeling motivated by the experience, as described by Participant 12:
Well, then I told my mother my situation. I figured she was going to respond in a negative way and fall apart. And she didn’t. She was strong. So I said, “This is not as bad as I thought. This is something I can fight.” Before this I had a hard time with this, carrying all this inside me. And after telling her and seeing how she responded, that let me know that I can get stronger from this. I can rebuild myself and be the person I used to be.
Psychosocial support
After disclosing the diagnosis of HIV infection, some participants stated they were able to access psychosocial support from those to whom they had disclosed. According to these participants, support from family and friends is essential. In cases where psychosocial support was lost or not available from family, friends, and partners, participants found support from HIV-related support groups. As reported by Participant 6, psychosocial support obtained from others living with the same disease state helped motivate the person toward resilience:
I see that my other friends have gone through the same thing as me. I call them friends because they are in the same group, you know? Everybody with the same condition in that group is like a family to me. When I have these good people around me, it helps. They are waiting on you. This one needs you. They give you a purpose, and need and help [you] gain that self-esteem back.
Managing the Disease
Building on motivation to progress toward resilience, participants next began the process of managing HIV infection. All participants reported that management of the disease was an essential step toward resilience. Management of the Disease was the second category that emerged from the data. Management of the Disease is composed of two subcategories: Self-Care and Psychological Health.
Self-Care
The first subcategory of Managing the Disease includes participants gaining or attempting to gain control of their physical health. Most participants voiced many physical manifestations of HIV infection, such as weight loss and body changes, that required attention to stave off disease progression. These participants believed that during this focus on the physical self, they began to commit to managing the disease by adhering to ART, as described by Participant 6:
Because the more you try, the better your results are. If you don’t try to take your medicine, guess what? Your numbers [T cells] are going to go down. [In a mocking voice] “I can’t take the medicine! I don’t want to take the medicine!” You are going to go down. But then every day you say, “I went to the doctor today. My T cells went up to 200. Maybe they can go more. My viral load is undetectable!” It makes you want to go higher and higher.
Participant 7 reported,
‘Cause [taking care of yourself] is the only way. That’s the only way for a person that been positive with the virus to take care of themselves: without stress. And stress ain’t easy to get rid of, but we have doctors. There’s treatment, there’s medication. Things that we can do. And finding time to have for ourself. I find time to have to myself.
Psychological Health
In conjunction with physical health, some participants also reported the need to focus on psychological health. These participants reported that they had been diagnosed with co-occurring mental health and substance abuse disorders. Participants realized that to successfully manage this chronic illness, it was just as important to focus on psychological/mental health as it was to focus on physical health. Participant 15 provided a summary of the importance of managing the psychological aspects of HIV infection:
[By managing psychological health] it teaches you more patience. You are much better [mentally] than you were before about a lot of things. It gives you more willpower. It makes me fight harder. No matter what people throw at me about HIV now, it doesn’t bother me. It bothers me that people could be so ignorant, but it doesn’t put me in a depression and make me want to hide my head in the sand.
Mastering the Disease
Once physical and psychological health had been addressed, most participants reported that the next component of the process of resilience in the context of HIV infection is Mastering the Disease. For these participants, mastering the disease meant that they had learned to manage both the physical and psychological aspects of HIV infection and that they were able to regain a sense of control over their lives. By learning to manage the aspects of HIV infection, these participants were able to become experts in the management HIV infection by transforming management into mastery through advocacy and positive health outcomes.
Advocacy
An important component of mastery, according to all participants, is the ability to learn and master self-advocacy, and then become advocates for others living with HIV infection. Participants were able to engage in advocacy via participation in support groups, outreach, workshops, public speaking, volunteerism, and informal education of others in the community. All participants verbalized a strong desire to become peer educators so that they could formally educate others about HIV infection and to provide a platform for advocacy. Participant 3 described the importance of advocacy for self and others:
This [advocacy] makes you more savvy, stronger . . . You try to help other people. I see that with everybody that I know who is [HIV] positive. They are always trying to help each other in clinic. At first no one would listen to you and now you see these same people and they will be sitting down next to someone who recently found out [that they were infected with HIV]. [That person is] totally rigid and these people are talking openly about it . . . about their medications and the side effects. And you relay it to other people and you can teach them how to become resilient and that you need a positive attitude. No, you are not going to die and this is what you can do. So, it’s wonderful if you can teach someone else.
Achievement of Health Outcomes
The second subcategory of Mastering the Disease is Achieving Positive Health Outcomes. Positive health outcomes, according to nearly all of the participants, were described as ways that people with HIV infection could be healthy despite this chronic condition. By mastering the disease, participants were able to achieve positive health outcomes, as described by Participant 13:
I believe that the results or consequences of being resilient can be better health. I figure if you are [HIV] positive, you try to be resilient and try to be positive [in your thinking], your body will follow through on that. I figure you won’t be as sick. You will be sick less often. Your T cell count will be much higher.
Participant 7 further expanded this subcategory by including the importance of mastering all aspects of the disease:
[Resilience] is not just learning, but practicing safe(r) sex, practicing a clean life, practicing how to eat well—what to eat and what not to eat, to look and be healthy. You find a way to make it. You don’t quit or give up. I say no to drugs, to alcohol, to unprotected sex. Saying no and keeping moving.
Perceiving Resilience
Drawing on sources of motivation, learning to manage the disease, and mastering the disease all serve as antecedents of Perceiving Resilience for people living with HIV infection. After these processes have been completed, according to all participants, a person with HIV may become resilient. Becoming resilient for people with HIV infection had the following connotations or meanings for the participants:
[Resilience] is that which I wasn’t able to do at one time: talk about this. I could not express it and now it is something I have no problem doing. Now I can have my life back and be the best that I can be and be myself again. (Participant 12)
Well, [resilience is] going through adversity, going through something that is not a pleasant experience and learning from it, growing from it. (Participant 13)
I’ve got a lot to look forward to and I am not going to let this take me out. I’ve grown from this and I’ve gotten stronger. So resilience equals strength. I’ve gained strength through resilience from dealing with this over time. (Participant 14)
You’ve got to get a grip on it and manage through the depression, denial, anger, and hate. You got to get beyond that and work and work getting yourself as good as you can be. Life with AIDS is good. It’s exactly what you put into it, you get out of it. If you shut down, life is bad . . . but you learn to manage all these things and life is good. Life is good. (Participant 15)
Discussion
The purpose of this study was to describe the process by which resilience occurs in the context of HIV infection using grounded theory. A definition of resilience in the context of HIV infection emerged from the data: Resilience is the process by which an individual accesses internal motivation (e.g., a desire to survive) and external motivation (e.g., psychosocial support) that provide a basis for him or her to learn to manage the physical and psychological aspects of HIV infection. Once individuals with HIV infection learn to manage both the physical and psychological aspects of the illness, a sense of mastery develops from advocacy as well as achieving health outcomes. The end result is the perception of resilience from the perspective of the participants.
This subjective description of the process by which resilience develops in the context of HIV infection is consistent with the emic approach to research. The emic approach is important because it provides a subjective depiction situated within the narratives of those who have experienced the phenomenon. The use of the emic approach yields a more meaningful and accurate description of resilience by those closest to the experience (Headland, Pike, & Harris, 1990). Subjective perceptions of resilience are more important than observable coping, as subjective perceptions provide the most accurate depiction of the client’s appraisal of his or her situation along with a perception of available support (Waller, 2001). This client appraisal of their situation and the perception of resilience are crucial in providing researchers with an understanding of resilience from the client’s perspective. In this sense, the client’s perception of resilience is considered a proxy measure of stress, social support, and coping (Waller, 2001).
The process of developing resilience in the context of HIV infection has important implications for nurses, health care providers, and individuals with HIV infection. Resilience, or a lack thereof, can make the difference between succumbing to HIV or adapting and adjusting to life with a stigmatizing chronic illness (Emlet et al., 2010). Assessing for the factors of the first component of resilience in the context of HIV infection, Motivation, can assist clients to identify, access, and strengthen these factors.
Among individuals with HIV infection, a spiritual struggle has been found to affect self-care concerns such as HIV symptoms, medication and disclosure apprehension, and overall HIV mastery (Trevino et al., 2010). Spirituality also was used by the participants to assist them with coping with substance abuse. Many participants used aspects of spirituality to “surrender to their higher power” in combating substance abuse. This is consistent with the philosophy of many substance abuse support groups such as Alcoholic Anonymous and Narcotics Anonymous. These programs encourage participants to admit their helplessness in dealing with a substance abuse disorder and to submit to a “higher power” (Center for Substance Abuse Treatment, 2008). Perhaps participants in this study accessed these community support programs. As reported by the participants, these programs provided support and possibly a foundation for the motivation that helped them move toward the perception of resilience.
Although progress has been made in HIV treatment, for some people, learning they are infected with HIV results in a fear of imminent death (Enriquez et al., 2010). Early postdiagnosis interaction between clients and health care providers affords a unique opportunity for health care providers to focus on educational initiatives that introduce the manageable, chronic nature of HIV to clients, and provides information on how individuals infected with HIV can best promote health and prevent the development of subsequent illness. These first steps may be critical in fostering the desire to survive in individuals with HIV infection. By providing open, nonjudgmental discourse, providing clinical knowledge necessary to make informed decisions, and assisting individuals with HIV to access resources such as support groups, health care providers can ensure individuals are receiving the necessary accurate information and psychosocial support critical for more positive health outcomes (Teti et al., 2007; Teti et al., 2010).
To ensure clients are receiving the greatest degree of psychosocial support, encouragement, and information from peer support groups, it may be important to consider factors such as the experience, gender, sexual orientation, or culture of the peer facilitator. For clients to glean the most from a support group, health care providers can assist in locating support groups that closely mirror, to the extent possible, the facets of the client that he or she considers most important, such as culture or sexual orientation. A peer facilitator or educator of the same culture or sexual orientation as clients may be more acceptable to the client, thereby ensuring that clients are provided with needed psychosocial support and educational information (McKirnan, Tolou-Shams, & Courtenay-Quirk, 2010; Teti et al., 2007).
Disclosure of their serostatus to others is a challenging task for clients. However, disclosure has been found to improve multiple mental health conditions as well as promote effective family communication (Murphy, Armistead, Marelich, Payne, & Herbeck, 2011; Zea, Reisen, Poppen, Bianchi, & Echeverry, 2005). Assisting clients in decision making regarding serostatus disclosure through education based on the positive outcomes associated with disclosure can be accomplished in the clinical setting by health care providers, but guidance from peer support groups is helpful when considering both the facilitators and barriers of disclosure, as well as strategies to assist clients with disclosure.
After clients have accessed intrinsic and extrinsic sources of Motivation, they are ready to engage in Managing the Disease, which includes both physical and psychological self-care. Improved quality of life among individuals with HIV infection has been found to be associated with a healthy lifestyle (Vyavaharkar, Moneyham, Murdaugh, & Tavakoli, 2011). As such, clients must manage the physical aspects of HIV infection in conjunction with maintaining psychological health. Health care providers can assist in this process by assessing the level of self-care employed by clients. Issues requiring further education or intervention can be identified and addressed. Importantly, because HIV is only treatable through medication adherence, clients not taking medications as prescribed are at risk for disease progression. Assessment of factors influencing medication adherence, such as substance use (Parsons, Rosof, & Mustanski, 2008), intimate partner violence (Rose, House, & Stepleman, 2010), and depression (Tegger et al., 2008), should be an ongoing endeavor, and connection of clients to appropriate care and treatment should ensue if necessary.
Learning to manage physical health promotes a sense of accomplishment that may promote psychological health. For individuals with HIV infection who are adherent to their medication regimens, psychological health is the next step in gaining resilience in the context of HIV infection. It is important for health care providers to assess for psychological health conditions, such as depression, HIV-related stigma, or even employment status, that have the potential to impact quality of life in terms of mental health (Buseh, Kelber, Stevens, & Park, 2008; Rueda et al., 2011; Rueda et al., 2012; Vyavaharkar et al., 2010). On identification of conditions or influences, health care providers can help clients access needed mental health or social services.
Once a sense of physical and psychological health is achieved, individuals with HIV infection continue to gain resilience in the context of HIV infection through Mastering the Disease. Advocacy, for oneself and others, can be considered an aspect of mastery, as advocacy implies a sense of self-efficacy (Pearlin, Menaghan, Lieberman, & Mullan, 1981). As peer counselors or educators, clients living with HIV infection can provide practical examples of how to manage life with HIV infection for others living with the same illness (Hilfinger Messias, Moneyham, Vyavaharkar, Murdaugh, & Phillips, 2009). Advocacy helps those who receive these support services understand treatment of HIV infection, assists with adherence, and allows clients an avenue to discuss HIV and other health issues (Mutchler et al., 2011). Encouraging clients expressing interest in peer counseling or advocacy to connect with community-based organizations or other agencies offering these services serves two purposes, by promoting a sense of mastery for the peer counselor or educator and promoting motivating factors for those receiving advocacy services.
Achievement of Health Outcomes comprises the next piece of Mastering the Disease, as this component of mastery indicates control over significant influences on one’s life (Pearlin et al., 1981). The importance of achieving a sense of mastery should be emphasized to clients, as mastery has been found to combat depression and HIV-related stigma (Rueda et al., 2012). Health care providers can assist clients to draw on their relationships with others (e.g., family, intimate relationships, or those in peer support groups) during times of additional adversity and to assist them in achieving and maintaining resilience (Dyer et al., 2004).
The results of this study add some important information regarding the development of the construct of resilience in the context of HIV infection. First, the results support the conceptualization of resilience in the context of HIV infection as a process, and support the classic works on resilience as a process (Fine, 1991; Flach, 1980; Rutter, 1985). Second, the results of this study are important because they contribute knowledge related to resilience among adults. The majority of the resilience literature is based on children. Results of this study suggest that resilience can develop later in life. Additional research is needed that describe resilience across the life span (Luthar et al., 2000).
Directions for further theory development can be drawn from the results of the study. The development of a grounded theory of resilience in the context of HIV infection is important because resilience has been studied without a delineated theoretical framework (Luthar et al., 2000). The next logical step would be to design a quantitative study that would be used to test this theory. Further understanding of the relationships of the components of the theory would inform future studies that could be focused on developing interventions to promote resilience among people living with HIV infection.
Further research could be developed from the study’s findings. For example, because previous research has noted the importance of the client’s relationship with health care providers in promoting resilience (Dyer et al., 2004), more research needs to be conducted to study how health care providers can develop therapeutic relationships with clients that foster resilience. Second, more research needs to be conducted on methods of assisting clients to access the intrinsic and extrinsic motivating factors identified in this study. Because these motivating factors are the foundation of resilience and may promote self-care and management of HIV infection, it is important to know how health care providers can best educate clients about these factors or assist clients in accessing both intrinsic and extrinsic motivators. Because it is not currently known how to effectively educate clients about these factors or how to help clients access these motivators, more research is warranted.
Limitations
This study was designed to develop a theory of resilience in the context of HIV infection. Despite filling a gap in the knowledge base of resilience in the context of HIV infection, one major limitation of this study exists. This major limitation is the manner in which participants were recruited for the study. The sample was drawn from the population of clients at a large university-based HIV clinical research unit. In addition to receiving HIV care at the clinical unit, participants were eligible to receive mental health care that included substance abuse treatment. The inclusive care provided at the university-based HIV clinical research unit may have supported the participants in managing the physical and psychosocial aspects of HIV infection and may have contributed to their insights on resilience in the context of HIV infection.
Summary
Despite the physical and psychological changes that occur from a diagnosis of HIV infection, results of this study suggest that persons can become resilient over time. From qualitative interviews with adults living with HIV infection, the process by which they overcome the adversity of HIV infection and learn to manage their infection and life meaningful lives has been described. Additional empirical work is necessary to further develop the concept of resilience in the context of HIV infection.
Acknowledgments
The authors would like to thank the following people for their assistance with this research study: Dr. Allan Rodriguez, MD, Associate Professor of Medicine at the University of Miami Miller School of Medicine, Division of Infectious Diseases, for facilitating access to the client population; Dr. Barbara Blake, PhD, RN, ACRN, Associate Professor of Nursing at Kennesaw State University WellStar College of Health and Human Services, School of Nursing in Kennesaw, GA; Dr. Susan Gaskin, DSN, RN, ACRN, Professor of Nursing at the Capstone College of Nursing at the University of Alabama in Tuscaloosa, Alabama, for assisting with the peer review and debriefing aspects of data verification; and all of the participants who were willing to share their experiences with us. Special thanks to Doris N. Ugarriza, PhD, ARNP, BC, Professor of Nursing and Health Studies at the University of Miami for her assistance in the preparation of this article.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article:
This study was funded by the Beta Tau Chapter of Sigma Theta International (Joseph De Santis, PI). Support for this research was received from the Center of Excellence for Health Disparities Research: EL CENTRO, National Institute on Minority Health and Health Disparities Grant P60MD002266.
Footnotes
Reprints and permission: http://www.sagepub.com/journalsPermissions.nav
Author Roles
Dr. De Santis was the study’s PI. He conducted all of the qualitative interviews and led data analysis. Ms. Florom-Smith, Dr. Vermeesch, and Ms. Barroso transcribed the data and assisted with data analysis. Dr. DeLeon assisted with data analysis.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Bletzer KV. Identity and resilience among persons with HIV: A rural African American experience. Qualitative Health Research. 2007;17:162–175. doi: 10.1177/1049732306297885. [DOI] [PubMed] [Google Scholar]
- Buseh AG, Kelber ST, Stevens PE, Park CG. Relationship of symptoms, perceived health, and stigma with quality of life among urban HIV-infected African American men. Public Health Nursing. 2008;25:409–419. doi: 10.1111/j.1525-1446.2008.00725.x. [DOI] [PubMed] [Google Scholar]
- Center for Substance Abuse Treatment. An introduction to mutual support groups for alcohol and drug abuse. Substance Abuse in Brief Fact Sheet. 2008;5(1) Retrieved from http://kap.samhsa.gov/products/brochures/pdfs/saib_spring08_v5i1.pdf. [Google Scholar]
- Creswell JW. Qualitative inquiry and research design: Choosing among five approaches. 2. Thousand Oaks, CA: Sage; 2007. [Google Scholar]
- De Santis J. Exploring the concepts of vulnerability and resilience in the context of HIV infection. Research and Theory for Nursing Practice. 2008;22:273–287. doi: 10.1891/0889-7182.22.4.273. [DOI] [PubMed] [Google Scholar]
- De Santis JP, Barroso S. Living in silence: A grounded theory study of vulnerability in the context of HIV infection. Issues in Mental Health Nursing. 2011;32:345–354. doi: 10.3109/01612840.2010.550018. [DOI] [PubMed] [Google Scholar]
- Dyer JG, McGuinness TM. Resilience: Analysis of the concept. Archives of Psychiatric Nursing. 1996;10:276–282. doi: 10.1016/s0883-9417(96)80036-7. [DOI] [PubMed] [Google Scholar]
- Dyer JG, Patsdaughter CA, McGuinness TM, O’Connor CA, De Santis JP. Retrospective resilience: The power of the patient-provider alliance in disenfranchised persons with HIV/AIDS. Journal of Multicultural Nursing & Health. 2004;10:57–65. [Google Scholar]
- Emlet CA, Tozay S, Raveis VH. “I’m not going to die from AIDS”: Resilience in aging with HIV disease. The Gerontologist. 2010;51:101–111. doi: 10.1093/geront/gnq060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enriquez M, Kelly PJ, Witt J, Rodriguez L, Lopez N, Smueles J, Sweet D. Silence is not golden: Invisible Latinas living with HIV in the Midwest. Journal of Immigrant and Minority Health. 2010;12:932–939. doi: 10.1007/s10903-010-9346-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farber EW, Schwartz JAJ, Schaper PE, Moonen DJ, McDaniel JS. Resilience factors associated with adaptation to HIV disease. Psychosomatics. 2000;41:140–146. doi: 10.1176/appi.psy.41.2.140. [DOI] [PubMed] [Google Scholar]
- Fine SB. Resilience and human adaptability: Who rises above adversity? American Journal of Occupational Therapy. 1991;45:493–503. doi: 10.5014/ajot.45.6.493. [DOI] [PubMed] [Google Scholar]
- Flach FF. Psycho-biological resilience, psychotherapy, and the creative process. Comprehensive Psychiatry. 1980;21:510–519. doi: 10.1016/0010-440x(80)90054-1. [DOI] [PubMed] [Google Scholar]
- Flaskerud JH, Winslow BJ. Conceptualizing vulnerable populations health-related research. Nursing Research. 1998;47(2):69–78. doi: 10.1097/00006199-199803000-00005. [DOI] [PubMed] [Google Scholar]
- Georgas J, Berry JW, van de Vijver FJR, Kagitcibasi C, Porrtina YH. Families across cultures: A 30-nation psychological study. New York, NY: Cambridge University Press; 2006. [Google Scholar]
- Glaser BG, Strauss AL. The discovery of grounded theory. Hawthorne, NY: Aldine; 1967. [Google Scholar]
- Gosselink CA, Myllykangas SA. The leisure experiences of older U.S. women living with HIV/AIDS. Health Care for Women International. 2007;28:3–20. doi: 10.1080/07399330601001402. [DOI] [PubMed] [Google Scholar]
- Headland T, Pike K, Harris M. Emic and etic: The insider/outsider debate. Newbury Park, CA: Sage; 1990. [Google Scholar]
- Herek GM, Capitanio JP, Widaman KF. HIV-related stigma and knowledge in the United States: Prevalence and trends, 1991–1999. American Journal of Public Health. 2002;92:371–377. doi: 10.2105/ajph.92.3.371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hilfinger Messias DK, Moneyham L, Vyavaharkar M, Murdaugh C, Phillips KD. Embodied work: Insider perspectives on the work of HIV/AIDS peer counselors. Health Care for Women International. 2009;30:572–594. doi: 10.1080/07399330902928766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holzemer WL, Human S, Arudo J, Rosa ME, Hamilton MJ, Corless I, Maryland M. Exploring HIV stigma and quality of life for persons living with HIV infection. Journal of the Association of Nurses in AIDS Care. 2009;20:161–168. doi: 10.1016/j.jana.2009.02.002. [DOI] [PubMed] [Google Scholar]
- Kumpfer KL. Factors and processes contributing to resilience: The resilience framework. In: Glantz MD, Johnson JL, editors. Resilience and development: Positive life adaptations. New York, NY: Springer; 1999. pp. 179–224. [Google Scholar]
- Lavalle C, Aguilar JCD, Pena F, Estada-Aguilar JL, Avina-Zubieta JA, Madrazo M. Reduction in hospitalization costs, morbidity, disability, and mortality in patients with AIDS treated with protease inhibitors. Archives of Medical Research. 2000;31:515–519. doi: 10.1016/s0188-4409(00)00097-7. [DOI] [PubMed] [Google Scholar]
- Lester BM, Masten AS, McEwen B, editors. Resilience in children. Boston, MA: Blackwell; 2006. [Google Scholar]
- Luthar SS, Cicchetti D, Becker B. The construct of resilience: A critical evaluation and guidelines for future work. Child Development. 2000;71:543–562. doi: 10.1111/1467-8624.00164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahungu TW, Rodger AJ, Johnson MA. HIV as a chronic disease. Clinical Medicine. 2009;9:125–128. doi: 10.7861/clinmedicine.9-2-125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKirnan DJ, Tolou-Shams M, Courtenay-Quirk C. The treatment advocacy program: A randomized controlled trial of a peer-led safer sex intervention for HIV-infected men who have sex with men. Journal of Consulting and Clinical Psychology. 2010;78:952–963. doi: 10.1037/a0020759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy DA, Armistead L, Marelich WD, Payne DL, Herbeck DM. Pilot trial of a disclosure intervention for HIV+ mothers: The track program. Journal of Consulting and Clinical Psychology. 2011;79:203–214. doi: 10.1037/a0022896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mutchler MG, Wagner G, Cowgill BO, McKay T, Risley B, Bogart LM. Improving HIV/AIDS care through treatment advocacy: Going beyond client education to empowerment by facilitating client-provider relationships. AIDS Care. 2011;23(1):79–90. doi: 10.1080/09540121.2010.496847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nightingale VR, Sher TG, Hansen NB. The impact of receiving an HIV diagnosis and cognitive processing on psychological distress and posttraumatic growth. Journal of Traumatic Stress. 2010;23:452–460. doi: 10.1002/jts.20554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parsons JT, Rosof E, Mustanski B. The temporal relationship between alcohol consumption and HIV-medication adherence: A multilevel model of direct and moderating effects. Health Psychology. 2008;27:628–637. doi: 10.1037/a0012664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearlin LI, Menaghan EG, Lieberman MA, Mullan JT. The stress process. Journal of Health and Social Behavior. 1981;22:337–356. [PubMed] [Google Scholar]
- Rose RC, House AS, Stepleman LM. Intimate partner violence and its effects on the health of African American HIV-positive women. Psychological Trauma: Theory, Research, Practice, and Policy. 2010;2:311–317. [Google Scholar]
- Rueda S, Gibson K, Rourke SB, Bekele T, Gardner S, Cairney J. Mastery moderates the negative effect of stigma on depressive symptoms in people living with HIV. AIDS and Behavior. 2012;16:690–699. doi: 10.1007/s10461-010-9878-6. [DOI] [PubMed] [Google Scholar]
- Rueda S, Raboud J, Mustard C, Bayoumi A, Lavis JN, Rourke SB. Employment status is associated with both physical and mental health quality of life in people living with HIV. AIDS Care. 2011;23:435–443. doi: 10.1080/09540121.2010.507952. [DOI] [PubMed] [Google Scholar]
- Rutter M. Resilience in the face of adversity: Protective factors and resistance to psychiatric disorders. British Journal of Psychiatry. 1985;147:598–611. doi: 10.1192/bjp.147.6.598. [DOI] [PubMed] [Google Scholar]
- Strauss AL, Corbin J. Basics of qualitative research. Newbury Park, CA: Sage; 1990. [Google Scholar]
- Tegger MK, Crane HM, Tapia KA, Uldall KK, Holte SE, Kitahata MM. The effect of mental illness, substance use, and treatment for depression on the initiation of highly active antiretroviral therapy among HIV-infected individuals. AIDS Patient Care and STDs. 2008;22:233–243. doi: 10.1089/apc.2007.0092. [DOI] [PubMed] [Google Scholar]
- Teti M, Bowleg L, Cole R, Lloyd L, Rubinstein S, Spencer S, Gold M. A mixed methods evaluation of the effect of the protect and respect intervention on the condom use and disclosure practices of women living with HIV/AIDS. AIDS and Behavior. 2010;14:567–579. doi: 10.1007/s10461-009-9562-x. [DOI] [PubMed] [Google Scholar]
- Teti M, Bowleg L, Rubinstein S, Lloyd L, Berhane Z, Gold M. Present but not accounted for: Exploring the sexual risk practices and intervention needs of nonheterosexually identified women in a prevention program for women with HIV/AIDS. Journal of LGBT Health Research. 2007;3(4):37–51. doi: 10.1080/15574090802226592. [DOI] [PubMed] [Google Scholar]
- Thompson B. Lazarus phenomena: An exploratory study of gay men living with HIV. Social Work in Health Care. 2003;37:87–114. doi: 10.1300/J010v37n01_05. [DOI] [PubMed] [Google Scholar]
- Trevino KM, Pargament KI, Cotton S, Leonard AC, Hahn J, Caprini-Faigin CA, Tsevat J. Religious coping and physiological, psychological, social, and spiritual outcomes in patients with HIV/AIDS: Cross-sectional and longitudinal findings. AIDS and Behavior. 2010;14:379–389. doi: 10.1007/s10461-007-9332-6. [DOI] [PubMed] [Google Scholar]
- Ungar M. The social ecology of resilience: Addressing contextual and cultural ambiguity of a nascent construct. American Journal of Orthopsychiatry. 2011;81:1–17. doi: 10.1111/j.1939-0025.2010.01067.x. [DOI] [PubMed] [Google Scholar]
- Vyavaharkar M, Moneyham L, Corwin S, Saunders R, Annang L, Tavakoli A. Relationships between stigma, social support, and depression in HIV-infected African American women living in the rural southeastern United States. Journal of the Association of Nurses in AIDS Care. 2010;21:144–152. doi: 10.1016/j.jana.2009.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vyavaharkar M, Moneyham L, Murdaugh C, Tavakoli A. Factors associated with quality of life among rural women with HIV disease. AIDS and Behavior. 2012;12:295–303. doi: 10.1007/s10461-011-9917-y. [DOI] [PubMed] [Google Scholar]
- Wagnild GM, Young HM. Development and psychometric evaluation of the resiliency scale. Journal of Nursing Measurement. 1993;1(2):65–78. [PubMed] [Google Scholar]
- Waller MA. Resilience in ecosystemic context; Evolution of the concept. American Journal of Orthopsychiatry. 2001;71:290–297. doi: 10.1037/0002-9432.71.3.290. [DOI] [PubMed] [Google Scholar]
- Zea MC, Reisen CA, Poppen PJ, Bianchi FT, Echeverry JJ. Disclosure of HIV status and psychological well-being among Latino gay and bisexual men. AIDS and Behavior. 2005;9:15–26. doi: 10.1007/s10461-005-1678-z. [DOI] [PubMed] [Google Scholar]