Abstract
Objective
We conducted a multi-site, randomized controlled trial examining the strategy of switching from olanzapine, quetiapine, or risperidone to aripiprazole to ameliorate metabolic risk factors for cardiovascular disease.
Method
Patients with schizophrenia or schizoaffective disorder with BMI ≥ 27 and non-HDL cholesterol (non-HDL-C) ≥ 130 mg/dl on a stable dosage of olanzapine, quetiapine, or risperidone were randomly assigned to stay on the current medication (n=106) or switch to aripiprazole (n=109) for 24 weeks. All participants were enrolled in a behaviorally oriented diet and exercise program. Raters were blinded to treatment assignment. The primary and key secondary outcomes were non-HDL-C change and efficacy failure, respectively.
Results
The pre-specified primary analysis included 89 switchers and 98 stayers who had at least one post-baseline non-HDL-C measurement. The least squares mean estimates of non-HDL-C decreased more for the switch than the stay groups (−20.2 vs. −10.8 mg/dl). Switching was associated with larger reductions in weight (2.9 kg) and a net reduction of serum triglycerides of 32.7 mg/dl. Twenty-two (20.6%) switchers and 18 (17.0%) stayers experienced protocol-defined efficacy failure. Forty-seven (43.9%) switchers and 26 (24.5%) stayers discontinued the assigned antipsychotic before 24 weeks.
Conclusion
Switching to aripiprazole led to improvement of non-HDL-C and other metabolic parameters. Rates of efficacy failure were similar between groups, but switching to aripiprazole was associated with a higher rate of treatment discontinuation. In the context of close clinical monitoring, switching from an antipsychotic with high metabolic risk to one with lower risk to improve metabolic parameters is an effective strategy.
Some commonly used antipsychotic medications (e.g., olanzapine, quetiapine, and risperidone) are associated with increased rates of metabolic abnormalities that predispose patients to cardiovascular disease (CVD) (1–7). Recent evidence has demonstrated that individuals with severe mental disorders have substantially shortened life expectancy, with cardiovascular diseases among the leading causes of premature mortality (8). Thus, appropriate treatment strategies for patients who take antipsychotics and who also have significant risk factors for CVD are needed. Among the methods for managing this risk in patients treated with antipsychotic drugs, switching from drugs with a high liability for producing metabolic side effects to an antipsychotic with a low liability is a commonly chosen option, albeit with uncertain effectiveness. This is of particular interest for individuals with schizophrenia or schizoaffective disorder who are clinically stable on an antipsychotic medication that has a relatively high risk of metabolic side effects. The possible benefits of switching to a medicine associated with fewer adverse metabolic effects must be weighed against the potential risk of clinical instability associated with changing treatment.
There are numerous modifiable risk factors for cardiovascular disease, including obesity, dyslipidemias, hypertension, and impaired glucose metabolism (including insulin resistance and diabetes mellitus). Recent attention has focused on non-HDL cholesterol (non-HDL-C), which contains all known and potentially atherogenic lipid particles, and has been shown in large cohort studies to be strongly associated with cardiovascular morbidity and mortality. For example, the Lipid Research Clinics Program Follow-up Study, which followed a cohort of 2,462 middle-aged men and women for an average of 19 years, found that non-HDL cholesterol at study entry was a strong predictor of CVD mortality (9). An increase of 30 mg/dL of non-HDL-C was associated with a 19% increase in CVD mortality in men and a 15% increase in women. In the Bypass Angioplasty Revascularization Investigation (BARI), in which 1514 patients with multi-vessel coronary artery disease were followed for 5 years, non-HDL-C was strongly and independently associated with nonfatal myocardial infarction and angina pectoris, with an increase of 10 mg/dL associated with a 5% increase in both of these conditions (10).
We report the primary and key secondary efficacy and safety results of a 24-week, randomized controlled clinical trial that examined the effectiveness of switching patients with schizophrenia or schizoaffective disorder from treatment with olanzapine, quetiapine, or risperidone to treatment with aripiprazole as a strategy to reduce metabolic problems associated with antipsychotic medications. We considered studying the switch to other antipsychotics with favorable metabolic profiles, including ziprasidone and molindone (3, 6, 11–13), but chose aripiprazole because it was the newest option and we expected it would be of most clinical interest when the study was completed.
We hypothesized that switching to aripiprazole would result in an improvement in metabolic measures compared to staying on the current antipsychotic medication. We also sought to determine if clinical destabilization due to switching from an antipsychotic that was working well would accompany any metabolic benefits of switching to aripiprazole. The primary efficacy outcome was the difference in non-HDL-C change from baseline between the two treatment groups. The key secondary outcome was efficacy failure, defined in the protocol as psychiatric hospitalization, a 25% increase in the total Positive and Negative Syndrome Scale (PANSS)(14) score, or ratings of much worse or very much worse on the Clinical Global Impression-Change Scale (15).
Methods
The Comparison of Antipsychotics for Metabolic Problems (CAMP) was a multi-site, parallel-group, randomized controlled clinical trial. Participants were individuals with schizophrenia or schizoaffective disorder who had achieved clinical stability on treatment with olanzapine, quetiapine, or risperidone, and who were at increased risk for cardiovascular disease as indicated by a body-mass index (BMI) ≥ 27 and a non-HDL-C ≥130 mg/dl (if non-HDL-C was 130 to 139, then LDL cholesterol was required to be ≥ 100 mg/dl). Patients were required to be on the qualifying drug for a minimum of three months and without dosage adjustments or any other antipsychotic for one month prior to enrollment. The reason that patients entered the study was a desire to improve their metabolic risk profile. All participants provided written informed consent after study procedures had been fully explained. The study was conducted at 27 clinical research centers affiliated with the Schizophrenia Trials Network in the U.S.
Patients were randomly assigned on a 1:1 basis to switch to aripiprazole or to stay on their current antipsychotic medication. Treatment assignment (stay versus switch) was stratified by antipsychotic medication taken when entering the study (olanzapine, quetiapine, and risperidone) and implemented centrally via a web-based system accessed by the clinical centers. Individuals assigned to stay on their current antipsychotic treatment remained on the pre-study dosage with adjustments only as clinically indicated. The allowed dosages were as follows: olanzapine 5–20 mg daily, quetiapine 200–1200 mg daily, and risperidone 1–16 mg daily. Patients assigned to switch to aripiprazole began taking aripiprazole 5 mg daily and continued their previous antipsychotic medication and dose for one week. After one week the dosage of aripiprazole was increased to 10 mg daily and the previous drug’s dosage was reduced 25–50%. After two weeks dosage of aripiprazole could be increased to 15 mg daily while the previous drug’s dosage was reduced 50–75% from the original dosage. After 3 weeks the available range for aripiprazole was 5–20 mg daily and the previous drug was stopped. After 4 weeks the allowed dosage range for aripiprazole was 5–30 mg daily.
All participants received a manualized behavioral intervention, adapted from a group treatment (16, 17), which was aimed at improving exercise and diet habits to reduce the risk of cardiovascular disease. Patients returned to the clinic for weekly visits during the first month of the treatment period and every four weeks after that. Laboratory assessments were conducted every four weeks. The behavioral intervention was provided in person at all post-baseline study visits. After the first four weeks, study personnel made a telephone call to reinforce the behavioral treatment lessons between each of the monthly visits.
Raters of symptoms (PANSS), global clinical status (CGI), and extrapyramidal side effects (the Abnormal Involuntary Movement Scale (18), the Barnes Akathisia Scale (19), and the Simpson-Angus Extrapyramidal Symptoms Scale (20)) were blinded to treatment assignment. Participants and their physicians were aware of the medication assignment.
The addition of lithium, valproate, lipid lowering agents such as statins, or drugs prescribed for weight loss was not allowed during the trial because of effects on the primary study outcome. Individuals taking stable doses of lithium, valproate or lipid lowering medications at the time of study entry could continue these treatments, but dose adjustments during the treatment period were not allowed. Initiation or change in dose of one of these medicines was considered a protocol violation. All other medications, except for non-study antipsychotics, were allowed.
Statistical methods
The primary efficacy analysis was conducted on the efficacy evaluable population, defined as all randomized patients receiving at least one dose of study medication and completing at least one post-baseline efficacy assessment, and corresponded to a comparison between randomization groups (stay versus switch) in change from baseline to 24 weeks in non-HDL-C. Repeated measurements mixed effects linear models were fit for the primary analysis and secondary analyses of continuous outcomes that appropriately accounted for the correlation among repeated clinical assessments and randomly missing data (21). Models included fixed effects for stratification (incoming medication), pooled clinical site, baseline value, treatment, time (weeks in study), and time by treatment interactions. An unstructured variance- covariance matrix was assumed, and least squares means at 24 weeks was the a priori basis for the treatment comparisons. Outcome measurements obtained following a prohibited change in dose or initiation of a disallowed medication were excluded from all efficacy analyses, as specified a priori in the study protocol. The primary efficacy analysis was repeated using all available measurements to assess the sensitivity of results.
Secondary analyses of efficacy failure and treatment discontinuation were based on the intention-to-treat population (ITT), defined as all randomized patients receiving at least one dose of study medication. Cochran-Mantel-Haenszel tests stratified by incoming medication were used to compare treatment groups with respect to the proportion experiencing efficacy failure and the proportion discontinuing treatment. Kaplan-Meier curves were generated for time to efficacy failure and time to treatment discontinuation, and treatment group were compared using log rank tests. Cox proportional hazards models were additionally fit to compare time to event outcomes controlling for incoming medication and pooled clinical site.
Results
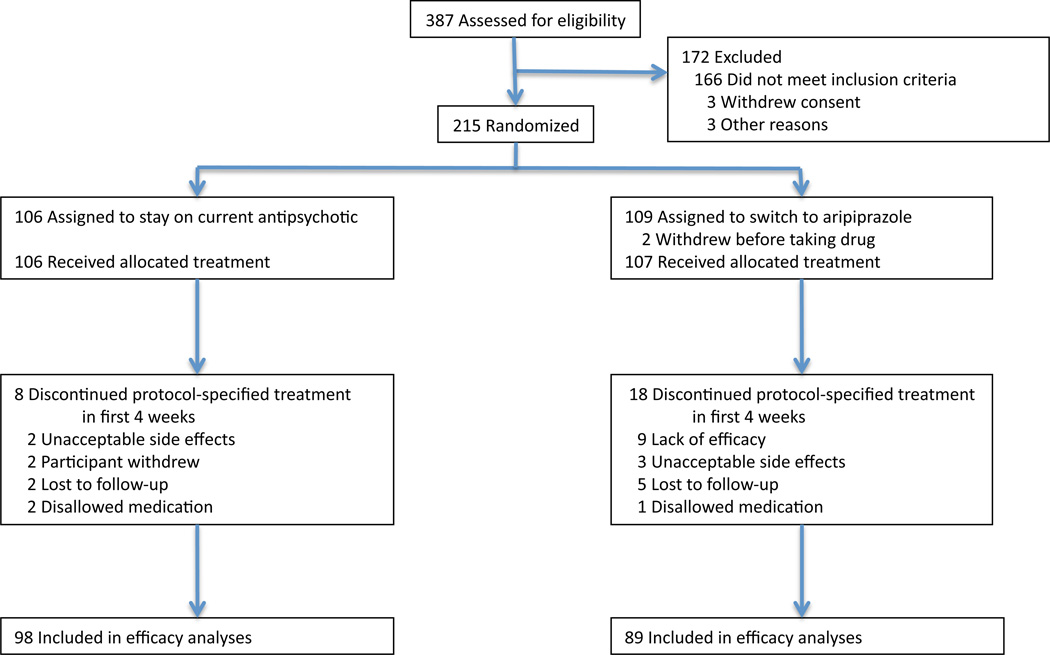
The study was conducted between January 2007 and March 2010. Figure 1 demonstrates the progress of patients screened and randomized. Of the 215 patients who were randomized, 109 were assigned to switch to aripiprazole and 106 to stay on the current antipsychotic. Baseline demographic and clinical characteristics of all randomized patients are shown in Table 1.
Figure 1.
Enrollment and follow-up
Table 1.
Baseline Demographic and Clinical Characteristics of Randomized Patients
| Total (N=215) |
Switch (N=109) |
Stay (N=106) |
||||
|---|---|---|---|---|---|---|
| Demographic characteristics | ||||||
| Mean | SD | Mean | SD | Mean | SD | |
| Age - yr | 41 | 11.1 | 40 | 11.7 | 42 | 10.5 |
| Education - yr | 12 | 2.5 | 12 | 2.3 | 13 | 2.6 |
| N | % | N | % | N | % | |
| Sex | ||||||
| Male | 137 | 63.7 | 68 | 62.4 | 69 | 65.1 |
| Female | 78 | 36.3 | 41 | 37.6 | 37 | 34.9 |
| Race | ||||||
| White | 123 | 57.2 | 65 | 59.6 | 58 | 54.7 |
| Black | 80 | 37.2 | 39 | 35.8 | 41 | 38.7 |
| Other | 10 | 4.7 | 4 | 3.7 | 6 | 5.7 |
| Spanish, Hispanic or Latino ethnicity | 39 | 18.1 | 19 | 17.4 | 20 | 18.9 |
| High school education or above | 166 | 77.2 | 83 | 76.1 | 83 | 78.3 |
| Marital Status | ||||||
| Married | 16 | 7.4 | 9 | 8.3 | 7 | 6.6 |
| Previously Married | 66 | 30.7 | 33 | 30.3 | 33 | 31.1 |
| Never Married | 133 | 61.9 | 67 | 61.5 | 66 | 62.3 |
| Living Situation | ||||||
| Independent/non-structured | 177 | 82.3 | 90 | 82.6 | 87 | 82.1 |
| Other | 38 | 17.7 | 19 | 17.4 | 19 | 17.9 |
| Clinical characteristics | ||||||
| Mean | SD | Mean | SD | Mean | SD | |
| Non-HDL Cholesterol - mg/dL | 173 | 32.8 | 169 | 31.9 | 176 | 33.5 |
| HDL Cholesterol - mg/dL | 44 | 11.4 | 45 | 12.4 | 43 | 10.2 |
| Weight - kg | 103 | 20.7 | 104 | 20.8 | 102 | 20.6 |
| Body Mass Index | 35 | 6.5 | 35 | 6.3 | 35 | 6.6 |
| Total Cholesterol - mg/dL | 217 | 33.3 | 214 | 33.5 | 220 | 33.0 |
| LDL Cholesterol - mg/dL | 140 | 28.0 | 138 | 25.6 | 142 | 30.3 |
| Triglycerides - mg/dL | 169 | 94.1 | 162 | 88.8 | 175 | 99.3 |
| TG/HDL ratio | 4 | 3.1 | 4 | 3.0 | 5 | 3.2 |
| HbA1c - % | 6 | 0.4 | 6 | 0.4 | 6 | 0.4 |
| Fasting glucose - mg/dL | 96 | 11.4 | 96 | 10.8 | 97 | 12.1 |
| 2-hour glucose - mg/dL | 127 | 41.1 | 126 | 37.9 | 127 | 44.4 |
| Fasting insulin - mU/L | 16 | 13.1 | 16 | 10.7 | 17 | 15.3 |
| 2-hour insulin - mU/L | 87 | 103.6 | 92 | 110.7 | 82 | 96.1 |
| C-reactive protein | 7 | 8.5 | 7 | 8.6 | 7 | 8.5 |
| PANSS Total | 66 | 16.3 | 65 | 16.0 | 67 | 16.6 |
| CGI-Severity score | 4 | 0.9 | 4 | 0.9 | 4 | 0.9 |
| SF-12 mntl health score | 45 | 11.5 | 44 | 11.4 | 46 | 11.4 |
| SF-12 phys health score | 45 | 10.3 | 46 | 9.9 | 45 | 10.6 |
| IWQoL Total | 66 | 28.8 | 65 | 28.8 | 66 | 29.0 |
Two patients who were assigned to switch never took study drug and were therefore not included in the ITT population. Eighteen (16.8%) of those in the switch group compared to 8 (7.5%) in the stay group stopped the protocol-specified treatment in the first four weeks, before completion of the time allowed for cross-titration to aripiprazole and before the first follow-up laboratory tests were conducted, and were therefore excluded from the efficacy evaluable population. Of these, 17 (15.9%) switchers and six (5.6%) stayers discontinued the assigned antipsychotic and the remaining three (one switcher and two stayers) took disallowed medications in the first month. The primary outcome and other metabolic parameters were evaluated in 89 switchers and 98 stayers who completed at least one month of study participation and thus had at least one post-baseline measurement of the primary outcome on the assigned treatment.
At study entry the mean daily doses of the qualifying medications were olanzapine 18.5 mg, quetiapine 502 mg, and risperidone 4.1 mg. Mean daily doses for patients during the study were 16.9 mg of aripiprazole, 18.0 mg of olanzapine, 572.0 mg of quetiapine, and 4.1 mg of risperidone.
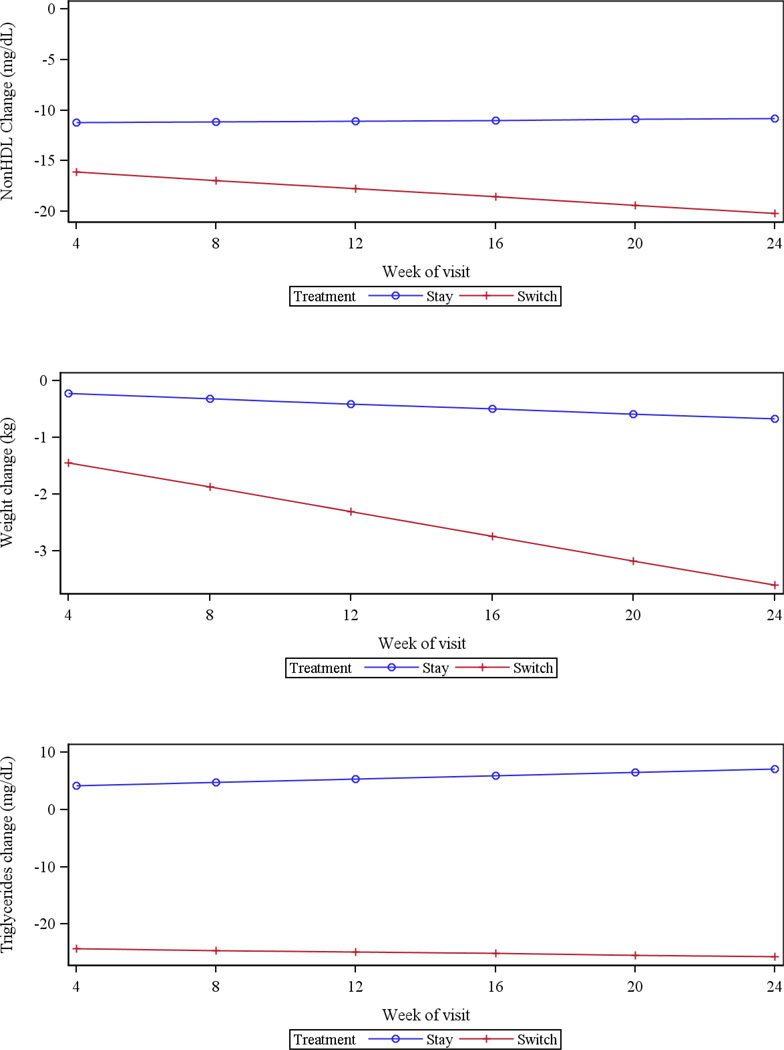
Metabolic outcomes
For the primary outcome, change in non-HDL-C , the least squares means decreased more for the switch than the stay groups (−20.2 vs. −10.8 mg/dl), with a difference of −9.4 mg/dl (95% Confidence Interval −2.2,−16.5, p = 0.010). Switchers lost more weight than stayers (−3.6 vs. −0.7 kg) with a difference of −2.9 kg (95% CI −1.6, −4.2, p < 0.001), and had a larger BMI reduction of −1.07 units (p < 0.001). Triglycerides decreased for the switch group and increased for the stay group (−25.7 vs. +7.0 mg/dl), yielding a difference of –32.7 mg/dl (95% CI −12.1, −53.4, p=0.002). As seen in Table 2, there were no differences between the treatment groups in changes in HDL or LDL cholesterol. The trend favoring switching compared to staying in reducing the inflammatory marker C-reactive protein was not significant. Figure 2 demonstrates the time course of changes in non-HDL-C, triglycerides, and weight. The benefit of switching on non-HDL-C and triglycerides was almost completely realized after only one month, while the advantage of switching on weight change accrued over the 24 weeks of the study. In our models, time and time by treatment parameters were significant for weight change but not for non-HDL-C or triglycerides. Mean (± standard deviation) weight change per month on study treatment was −0.8±1.4 kg for switchers and −0.1± 1.0 kg for stayers.
Table 2.
Outcome Measures of Effectiveness in the Efficacy Evaluable Population – by treatment
| Switch (N=89) |
Stay (N=98) |
||||||
|---|---|---|---|---|---|---|---|
| Mean | SE | Mean | SE | Difference | 95% CI | P value | |
| Primary Outcome | |||||||
| Change in nonHDL | −20.2 | 2.87 | −10.8 | 2.57 | 9.4 | (2.2,16.5) | 0.0102* |
| Other Secondary Outcomes | |||||||
| Metabolic Outcomes | |||||||
| Change in HDL Cholesterol | 0.6 | 0.76 | −0.1 | 0.68 | −0.7 | (−2.7,1.3) | 0.4693* |
| Change in weight (kg) | −3.6 | 0.48 | −0.7 | 0.44 | 2.9 | (1.6,4.2) | <.0001* |
| Change in BMI (kg/m2) | −1.3 | 0.17 | −0.2 | 0.15 | 1.1 | (0.6,1.5) | <.0001* |
| Change in Total Cholesterol | −19.6 | 2.99 | −10.8 | 2.69 | 8.8 | (1.5,16.1) | 0.0179* |
| Change in LDL Cholesterol | −15.4 | 2.76 | −12.5 | 2.54 | 2.9 | (−3.9,9.6) | 0.4003* |
| Change in Triglycerides | −25.7 | 8.10 | 7.0 | 7.20 | 32.7 | (12.1,53.4) | 0.0020* |
| Change in TG/HDL ratio | −0.8 | 0.25 | 0.2 | 0.22 | 1.0 | (0.3,1.6) | 0.0029* |
| Change in HBA1c | 0.0 | 0.03 | 0.1 | 0.03 | 0.0 | (−0.1,0.1) | 0.6413* |
| Change in fasting glucose | 0.5 | 1.43 | 4.0 | 1.25 | 3.5 | (−0.2,7.1) | 0.0607* |
| Change in fasting insulin | 1.0 | 2.58 | 6.7 | 2.26 | 5.7 | (−1.0,12.4) | 0.0963* |
| Change in 2-hour glucose | −10.3 | 4.19 | −6.1 | 3.75 | 4.3 | (−5.7,14.3) | 0.4012* |
| Change in 2-hour insulin | −31.1 | 7.72 | −6.8 | 6.83 | 24.2 | (4.8,43.6) | 0.0144* |
| Change in C-reactive protein | −1.7 | 1.28 | 1.5 | 1.15 | 3.2 | (−0.1,6.5) | 0.0557* |
| Measures of Clinical Status | |||||||
| Change in PANSS Total | −5.0 | 1.45 | −3.9 | 1.31 | 1.1 | (−2.3,4.6) | 0.5180* |
| Change in CGI-Severity Score | −0.2 | 0.09 | −0.2 | 0.09 | −0.0 | (−0.2,0.2) | 0.8566* |
| Chg in SF-12 mntl health score | 0.3 | 1.37 | 0.3 | 1.13 | −0.1 | (−3.6,3.4) | 0.9680** |
| Chg in SF-12 phys health score | 2.1 | 1.09 | −1.6 | 0.91 | −3.7 | (−6.5,−0.9) | 0.0105** |
| Chg in IWQoL Total | −14.2 | 2.57 | −4.7 | 2.22 | 9.6 | (3.3,15.8) | 0.0028** |
The P value is for the comparison of least squares means in change from baseline between stay and switch at the 24-week visit. A linear mixed model that appropriately accounts for correlations among clinic visits associated with a single patient and for randomly missing data is used to test for a difference in least squares means. Model effects include main effects corresponding to incoming medication, baseline, visit and treatment, as well as a treatment by visit interaction term. Pooled clinical center is a random effect.
The P value for the comparison of these outcomes, which are measured at the last follow-up only, are from a mixed model with fixed effects incoming study medication, baseline and treatment and random effect pooled site.
Least squares means and standard errors from the mixed model are presented.
Figure 2.
Values are from efficacy evaluable population (n=187), and least squares means from the mixed model are presented. Change from baseline was the outcome variable, and treatment, week, baseline value, incoming medication, treatment by week interaction were covariates in the mixed model. P-value for NonHDL change is 0.0102, p-value for weight change is <.0001, and p-value for triglycerides change is 0.0020.
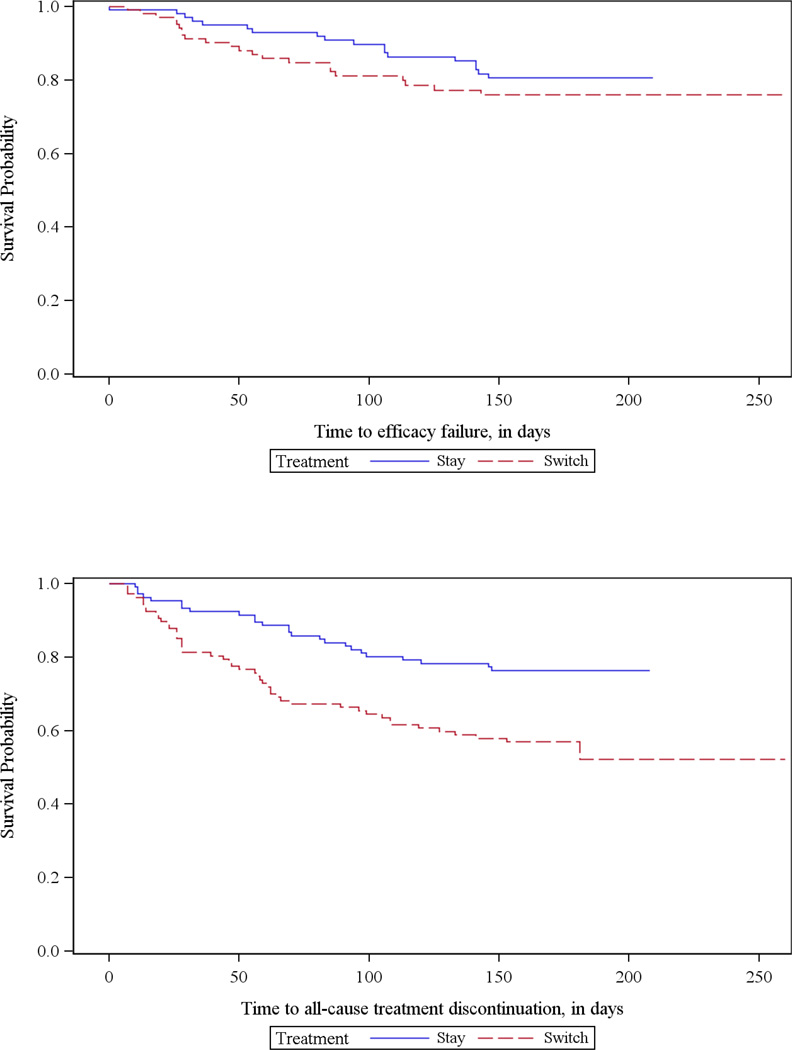
Kaplan-Meier curves on intent-to-treat population (n=215). Logrank test p-value is 0.2993 for time to efficacy failure in days and 0.0021 for time to all-cause treatment discontinuation in days.
On measures of glucose metabolism and insulin sensitivity, there was no difference between switchers and stayers on fasting glucose, fasting insulin, or glycosolated hemoglobin. Two hours following oral ingestion of 75 mg of glucose, there was no difference in glucose levels but the 2-hour insulin level decreased more for those assigned to switch compared to those assigned to stay (−31.1 vs. −6.8 mg/dl), with a difference of −24.2 mg/dl (p = 0.014).
Measures of clinical status
Twenty-two (20.6%) patients assigned to switch to aripiprazole and 18 (17.0%) assigned to stay on the current antipsychotic experienced efficacy failure (p=0.4872). There was no difference in time to efficacy failure (hazard ratio for switching 0.747; 95% CI 0.395–1.413, p=0.3703). There were no differences between groups in psychopathology changes as measured by the Positive and Negative Syndrome Scale (PANSS) total score (p=0.5180), change in CGI-Severity score (p=0.8566), or change in the Medical Outcomes Survey-Short Form 12 Item (SF-12)(22) mental health scores (p=0.9680). The SF-12 physical health score worsened slightly for the stayers and improved for the switchers, yielding an advantage for the switchers of 3.7 units (p=0.0105). On the IWQOL-lite, a validated measure of quality of life related to weight (23), switchers improved more than stayers (−14.2 vs. −4.7 units, p=0.0028).
Treatment discontinuation
Eighteen (16.8%) of those assigned to switch to aripiprazole discontinued the protocol-specified treatment before one month had elapsed, compared to eight (7.5%) of those assigned to stay on the current medication. Overall, 51 (47.7%) switchers and 29 (27.4%) stayers stopped the protocol-specified treatment (by stopping the assigned antipsychotic or beginning a prohibited medication) before 24 weeks (p=0.0019). Participants in the switch group discontinued the protocol-specified treatment (for any cause) earlier than those in the stay group (hazard ratio 0.456; 95% CI 0.285–0.728, p = 0.0010). Forty-seven (43.9%) switchers and 26 (24.5%) stayers stopped taking the assigned antipsychotic altogether before 24 weeks.
Adverse Effects
We systematically inquired about 20 adverse events commonly associated with antipsychotic medications. Table 3 demonstrates the frequency at which participants rated each of these side effects at a severity of “moderate” or “severe”. Considering the adverse effects reported after baseline with differences of approximately 5% or more between the stay or switch groups, insomnia was more common in the switch group but there was more sleepiness, hypersomnia, nausea, dry mouth, increased appetite, and akinesia among the stayers. Among the switchers, 18 patients (16.8%) experienced a total of 21 serious adverse events (SAEs; including medically significant or life-threatening events, hospitalizations, or extended hospitalizations), compared to 10 stayers (9.4%) who experienced 14 SAEs. One stayer and no switchers discontinued treatment due to akathisia/activation. Eight switchers (7.5%) and 5 stayers (4.7%) were hospitalized for psychiatric reasons. There were no deaths in the study.
Table 3.
CAMP General Safety Summary
| Total n=213 |
Switch n=107 |
Stay n=106 |
|||||
|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | p-value | |
| Procotol-specified efficacy failure* | 40 | 18.8 | 22 | 20.6 | 18 | 17.0 | 0.4782 |
| Early discontinuation of protocol-specified treatment** | 80 | 37.6 | 51 | 47.7 | 29 | 27.4 | 0.0019 |
| Discontinuation of study antipsychotic due to any cause | 73 | 34.3 | 47 | 43.9 | 26 | 24.5 | |
| Discontinuation of study antipsychotic due to inefficacy | 21 | 9.9 | 18 | 16.8 | 3 | 2.8 | |
| Discontinuation of study antipsychotic due to intolerability | 13 | 6.1 | 7 | 6.5 | 6 | 5.7 | |
| Dropped out - no information available | 23 | 10.8 | 15 | 14.0 | 8 | 7.5 | |
| Dropped out due to withdrawn consent | 14 | 6.6 | 5 | 4.7 | 9 | 8.5 | |
| Discontinuation of study antipsychotic due to other reasons | 2 | 0.9 | 2 | 1.9 | 0 | 0.0 | |
| Participants with any SAE*** | 28 | 13.1 | 18 | 16.8 | 10 | 9.4 | |
| Participants with any psychiatric hospitalization | 13 | 6.1 | 8 | 7.5 | 5 | 4.7 | |
| Deaths | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | |
| Participants with any AE+ | 160 | 75.1 | 81 | 75.7 | 79 | 74.5 | |
| Participants with at least one AE from Systematic Inquiry+ | 154 | 72.3 | 77 | 72.0 | 77 | 72.6 | |
| Insomnia | 73 | 34.3 | 44 | 41.1 | 29 | 27.4 | |
| Sleepiness | 62 | 29.1 | 27 | 25.2 | 35 | 33.0 | |
| Dry mouth | 60 | 28.2 | 24 | 22.4 | 36 | 34.0 | |
| Akathisia/activation | 55 | 25.8 | 29 | 27.1 | 26 | 24.5 | |
| Problems with sex drive | 50 | 23.5 | 24 | 22.4 | 26 | 24.5 | |
| Increased appetite | 44 | 20.7 | 18 | 16.8 | 26 | 24.5 | |
| Weight gain | 41 | 19.2 | 20 | 18.7 | 21 | 19.8 | |
| Constipation | 40 | 18.8 | 20 | 18.7 | 20 | 18.9 | |
| Akinesia | 39 | 18.3 | 14 | 13.1 | 25 | 23.6 | |
| Problems with sexual orgasm | 39 | 18.3 | 20 | 18.7 | 19 | 17.9 | |
| Problems with sexual arousal | 38 | 17.8 | 20 | 18.7 | 18 | 17.0 | |
| Hypersomnia | 37 | 17.4 | 16 | 15.0 | 21 | 19.8 | |
| Orthostatic faintness | 37 | 17.4 | 19 | 17.8 | 18 | 17.0 | |
| Nausea | 30 | 14.1 | 12 | 11.2 | 18 | 17.0 | |
| Incontinence/nocturia | 22 | 10.3 | 9 | 8.4 | 13 | 12.3 | |
| Skin rash | 20 | 9.4 | 8 | 7.5 | 12 | 11.3 | |
| Menstrual irregularities | 16 | 7.5 | 10 | 9.3 | 6 | 5.7 | |
| Sialorrhea | 15 | 7.0 | 8 | 7.5 | 7 | 6.6 | |
| Urinary hesitancy | 9 | 4.2 | 5 | 4.7 | 4 | 3.8 | |
| Gynecomastia/galactorrhea | 6 | 2.8 | 2 | 1.9 | 4 | 3.8 | |
Uses intent-to-treat population.
'Procotol-specified efficacy failure' are those participants who had either a psychiatric hospitalization, a 25 percent increase from baseline on the Positive and Negative Syndrome Scale (PANSS) (or a 10 point increase for individuals with a baseline total score of 40 or less), or substantial clinical deterioration on the Clinical Global Impressions-Change (CGI-C) Scale (i.e., 6- much worse or 7- very much worse). The p-value for the comparison of this binary outcome is from a Cochran-Mantel-Haenszel (CMH) test stratified by incoming antipsychotic (olanzapine, quetiapine or risperidone).
'Early discontinuation of protocol-specified treatment' includes both early treatment discontinuations AND participants who started/stopped/changed dose of a disallowed medication (Lipid Lowering Agent or Mood Stabilizer). The p-value for the comparison of this binary outcome is from a Cochran-Mantel-Haenszel (CMH) test stratified by incoming antipsychotic (olanzapine, quetiapine or risperidone).
'Discontinuation of study antipsychotic due to any cause' are those participants who did not complete 24 weeks on the assigned treatment.
'Discontinuation of study antipsychotic due to inefficacy' are the participants whose study treatment was stopped due to Positive Symptoms, Negative Symptoms, Mood Symptoms or Other Inefficacy/Inadequate Therapeutic Effect.
'Discontinuation of study antipsychotic due to intolerability' are the participants whose study treatment was stopped due to Weight, Lipids, Glucose, EPS, TD, Akathisia/activation, Sedation, Insomnia, Agitation, Sexual Side effects, Nausea, or Other unacceptable side effects).
'Dropped out due to withdrawn consent' are the participants whose study treatment was stopped due to the patient not seeing need for treatment or patient no longer wanting to participate in the study.
'Discontinuation of study antipsychotic due to other reasons' are participants whose study treatment was stopped due to administrative reasons.
Only events after randomization are included here.
Includes 'moderate' to 'severe' adverse events recorded post-baseline.
AE includes Adverse Events both from systematic inquiry and general inquiry.
Sensitivity Analysis
A sensitivity analysis of the primary efficacy outcome (change in non-HDL-C) was conducted using a modified ITT population of participants with at least one post-baseline non-HDL measurement. A repeated measurements mixed effects linear model was fit using all available measurements of non-HDL-C, regardless of disallowed medication usage or early discontinuation of the prescribed antipsychotic, to predict the change at week 24. The change remained greater among patients switching to aripiprazole than those remaining on original medication but statistical significance was not achieved. The difference in least squares means was 5.8 mg/dl (p= 0.104).
Discussion
The study was conducted at 27 research sites in the U.S. that were selected to include a demographically diverse population to enhance generalizability of the results. Enrollment criteria were designed to include a wide spectrum of individuals who might consider switching medications due to metabolic problems, although those with minimal metabolic problems and those with severe metabolic problems that needed immediate intervention were excluded. Thus the results of this study might best be generalized to individuals with chronic schizophrenia or schizoaffective disorder with moderate metabolic problems, for whom a medication change or a lifestyle intervention focused on diet and exercise is an appropriate first step.
In this study switching from olanzapine, quetiapine, or risperidone to aripiprazole was effective in helping many patients to improve their lipid profiles (lower non-HDL-C and lower triglycerides) and lose weight. The 9 mg/dl reduction of non-HDL-C is slightly less than the 10 mg/dl difference significantly reduced cardiovascular morbidity in the BARI study (10). The 1.1 unit reduction in BMI is above the 1 unit considered clinically significant by a panel of antipsychotic experts who created monitoring guidelines (24). Because weight loss was continuing at the end of the study, it is possible that our results underestimate the long-term benefit of switching on this secondary outcome. Because non-HDL-C was the primary pre-designated outcome, results pertaining to non-HDL-C are stronger evidence than those for secondary outcomes. These results are consistent with those in a randomized controlled trial reported by Newcomer and colleagues that examined switching from olanzapine to aripiprazole over 16 weeks (25). In that study, switchers had a 3.21 kg advantage in weight after 16 weeks, a reduction in triglycerides compared to an increase for the stayers, and approximately a 15.6 mg/dl larger reduction in non-HDL-C.
Aripiprazole is one of several antipsychotics, including ziprasidone and molindone, associated with a relatively low risk of metabolic problems. In studies, switching to ziprasidone has been associated with significant improvement in metabolic parameters (12, 13). In addition, other available strategies to address metabolic problems in patients taking antipsychotic medications include statins (i.e., HMG-coA reductase inhibitors) to reduce LDL-cholesterol (LDL-C) and metformin to reduce weight. Statins tend to have their greatest benefits on LDL and triglycerides rather than HDL or weight. The different statins have variable effects on LDL-C but typically associated with reductions in LDL-C of 30–60% (26). Short-term studies of metformin have shown that it is effective and well-tolerated in promoting weight loss among individuals who have recently gained weight while taking an antipsychotic (27), individuals experiencing a first-episode of psychosis (28), and even individuals whose increased weight is not of recent onset (29).
Switching antipsychotics by beginning aripiprazole at a low dose and titrating upward while slowly discontinuing the previous antipsychotic over one month was not associated with a significant increase in efficacy failures as indicated by need for hospitalization or substantial worsening of symptoms or global clinical status. However, a larger percentage of individuals assigned to switch to aripiprazole relative to individuals staying on their original antipsychotic discontinued the assigned treatment over the 24 weeks of the study. In some cases the medication discontinuation was attributed to inadequate efficacy by the study clinician but did not meet the study criteria for efficacy failure. The protocol, of course, was designed to minimize risks for participants, and allowed study physicians to intervene to prevent problems before they became severe. For example, when clinical worsening was detected study physicians could intervene by discontinuing the protocol-specified treatment, thus averting full-blown efficacy failure. We investigated this possibility by comparing the PANSS scores of participants who met the protocol’s efficacy failure criteria to the PANSS scores of participants whose treatment discontinuations were judged to be due to inadequate efficacy but did not meet the efficacy failure criteria; the mean (± standard deviation) PANSS scores of those who met efficacy failure criteria were higher (71.7±22.9 vs. 59.5±15.2). This suggests that careful clinical monitoring following a medication switch, accompanied by appropriate clinical intervention when poor efficacy is detected (e.g., stopping the new antipsychotic and restarting the previous one) can reduce the risk of severe symptom exacerbations and need for hospitalization.
Because the goal of the study was to evaluate the effect of switching antipsychotic medications on metabolic parameters, some common medication changes that were known to affect these parameters were not allowed. For those few patients who took the proscribed medications but continued the assigned antipsychotic, we only used measurements taken before the disallowed change occurred in the primary analyses. Seven such deviations from “protocol-specified” treatment occurred; four were in the switch group and three in the stay group. In addition, some patients contributed data after they had stopped taking the assigned antipsychotic. Results from the sensitivity analyses conducted to assess the impact of these exclusions and early dropouts for other reasons showed that the numerical advantage of switching remained, although statistical significance was not achieved.
This report is focused on the primary comparison of staying on current medication or switching. Secondary analyses examining the effects for each of the three allowed antipsychotics at study entry are provided in supplementary tables. These secondary analyses provide only suggestive information about the impact of switching from these drugs.
Open-label treatment is a limitation of this study, particularly for outcomes not measured in the laboratory but instead subject to clinical judgment. For example, a belief that olanzapine has superior efficacy could have contributed to the early discontinuations among those who entered the study taking olanzapine but were assigned to switch to aripiprazole (Supplemental Table 3). The excess of early treatment discontinuations in the olanzapine group suggests that switching from olanzapine was either more difficult than switching from the other drugs or, perhaps, resulted from an expectation bias that this change would be the most difficult.
In conclusion, switching from a medication associated with substantial risk of metabolic problems to one with a lower risk of these problems is a reasonable clinical option if careful cross-titration and close monitoring is possible. Careful clinical monitoring during and after a switch is necessary, and the diligence of clinicians is likely a principal reason that switchers did not experience a higher rate of efficacy failures than those who stayed on their original antipsychotic. If switching medications is unsuccessful, other approaches to reduce some of the risk factors for cardiovascular disease are available, including adding metformin or a statin. The switch in medications was effective in the presence of a behavioral intervention focused on improving diet and exercise habits, which had benefits even in the comparison group that did not change medications.
Supplementary Material
Acknowledgement
The study was funded by a grant from the Foundation for the National Institutes of Health (FNIH) and by a contract from the National Institute of Mental Health (N01 MH900001). Bristol Myers Squibb (BMS) provided aripiprazole and funds to FNIH in support of the study. BMS was not involved in the conduct of the study, data analysis, or the preparation of this manuscript.
Footnotes
Authors Disclosures of Competing Interests
Drs. Stroup and Nussbaum and Ms. Ring have no disclosures to make in the past year. (Within the past three years, Dr. Stroup has been a consultant for Janssen and Lilly.) Dr. McEvoy reports honoraria for speaking for Lilly; consultation, honorarium for educational lecture for staff for Hoffman LaRoche; advisory board for Merck; honoraria for speaking, research grant for Sunovion; and a research grant from GlaxoSmithKline. Dr. Swartz receives research support from Eli Lilly and consults with Novartis. Dr. Hamer reports that in the past three years he has served on a DSMB, an advisory board, consulted for or advised, or was involved in a contract between UNC and the following: Abbott, Acadia, Allergan, Alpharma, AstraZeneca, Cenerx, Corcept, Lilly, EnabledMD, Epix, Johnson and Johnson, Novartis, Pfizer, PureTechVentures, Schwartz, Sanofi-Aventis, Takeda, Wyeth, and I have served as an expert witness in lawsuits involving Forest, Lundbeck, Sun, Caraco, Teva, Barr, Mylan, Eurand, Cephalon, Anesta. Dr. LaVange has served on a DSMB for MAP Pharmaceuticals, consulted fro Parion Sciences, received an honorarium from GlaxoSmithKline, owns stock options from Inspire Pharmaceuticals, and has received research funding from Pfizer and Merck. Dr. Swartz has received research support from Eli Lilly and consulting fees from Novartis. Dr. Rosenheck has received research support from Janssen Pharmaceutica and Wyeth Pharmaceuticals in the last year and has consulted to RochePharamceuticals and has been a consultant to and is testifying expert in Jones ex rel. the State of Texas v. Janssen Phamaceutica et al. Dr. Perkins has been a consultant and speaker for Lilly and a consultant for Sunovion. Dr. Lieberman serves on the Advisory Board of Bioline, GlaxoSmithKline, Intracellular Therapies, Eli Lilly, Pierre Fabre and Psychogenics. He does not receive financial compensation or salary support for his participation as an advisor. He receives grant support from Allon, GlaxoSmithKline, Merck, Novartis, Pfizer, Sepracor and Targacept; and he holds a patent from Repligen.
The study was conducted by the following investigators:
Lawrence Adler, Glen Burnie, MD; Farooq Amin, Atlanta, GA; Michael Barber, Houston, TX; Peter Buckley, Augusta, GA; Matthew Byerly, Dallas, TX; Jose Canive, Albuquerque, NM; Stanley Caroff, Philadelphia, PA; Cyril D’Souza, New Haven, CT; Ira Glick, Palo Alto, CA; Daniel Mamah, St. Louis, MO; Don Goff, Boston, MA; Anita Kablinger, Shreveport, LA; Ahsan Kahn, Wichita, KS; Steven Lamberti, Rochester, NY; Jeffrey Lieberman, New York, NY; Theo Manschreck, Fall River, MA; Joseph McEvoy, Butner, NC; Alec Miller, San Antonio, TX; Del Miller, Iowa City, IA; Gurmeet Multani, Colson, CA; Henry Nasrallah, Cincinnati, OH; Stephen Olson, Minneapolis, MN; Jayendra Patel, Worcester, MA; Bruce Saltz, Boca Raton, FL; Richard Steinbook, Miami, FL; Scott Stroup, Chapel Hill, NC.
References
- 1.Consensus development conference on antipsychotic drugs and obesity and diabetes. Diabetes Care. 2004;27(2):596–601. doi: 10.2337/diacare.27.2.596. [DOI] [PubMed] [Google Scholar]
- 2.Newcomer JW, Ratner RE, Eriksson JW, Emsley R, Meulien D, Miller F, et al. A 24-week, multicenter, open-label, randomized study to compare changes in glucose metabolism in patients with schizophrenia receiving treatment with olanzapine, quetiapine, or risperidone. J Clin Psychiatry. 2009;70(4):487–499. doi: 10.4088/jcp.08m04132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Newcomer JW. Second-generation (atypical) antipsychotics and metabolic effects: a comprehensive literature review. CNS Drugs. 2005;19(Suppl 1):1–93. doi: 10.2165/00023210-200519001-00001. [DOI] [PubMed] [Google Scholar]
- 4.Meyer JM, Davis VG, McEvoy JP, Goff DC, Nasrallah HA, Davis SM, et al. Impact of antipsychotic treatment on nonfasting triglycerides in the CATIE Schizophrenia Trial phase 1. Schizophr Res. 2008;103(1–3):104–109. doi: 10.1016/j.schres.2008.04.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Meyer JM, Davis VG, Goff DC, McEvoy JP, Nasrallah HA, Davis SM, et al. Change in metabolic syndrome parameters with antipsychotic treatment in the CATIE Schizophrenia Trial: prospective data from phase 1. Schizophr Res. 2008;101(1–3):273–286. doi: 10.1016/j.schres.2007.12.487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lieberman JA, Stroup TS, McEvoy JP, Swartz MS, Rosenheck RA, Perkins DO, et al. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N Engl J Med. 2005;353(12):1209–1223. doi: 10.1056/NEJMoa051688. [DOI] [PubMed] [Google Scholar]
- 7.Kahn RS, Fleischhacker WW, Boter H, Davidson M, Vergouwe Y, Keet IP, et al. Effectiveness of antipsychotic drugs in first-episode schizophrenia and schizophreniform disorder: an open randomised clinical trial. Lancet. 2008;371(9618):1085–1097. doi: 10.1016/S0140-6736(08)60486-9. [DOI] [PubMed] [Google Scholar]
- 8.Parks J, Svendson D, Singer P, Foti M. Morbidity and Mortality in People with Serious Mental Illness. [Technical Report] 2006 In press. [Google Scholar]
- 9.Cui Y, Blumenthal RS, Flaws JA, Whiteman MK, Langenberg P, Bachorik PS, et al. Non-high-density lipoprotein cholesterol level as a predictor of cardiovascular disease mortality. Arch Intern Med. 2001;161(11):1413–1419. doi: 10.1001/archinte.161.11.1413. [DOI] [PubMed] [Google Scholar]
- 10.Bittner V, Hardison R, Kelsey SF, Weiner BH, Jacobs AK, Sopko G. Non-high-density lipoprotein cholesterol levels predict five-year outcome in the Bypass Angioplasty Revascularization Investigation (BARI) Circulation. 2002;106(20):2537–2542. doi: 10.1161/01.cir.0000038496.57570.06. [DOI] [PubMed] [Google Scholar]
- 11.Sikich L, Frazier JA, McClellan J, Findling RL, Vitiello B, Ritz L, et al. Double-blind comparison of first- and second-generation antipsychotics in early-onset schizophrenia and schizo-affective disorder: findings from the treatment of early-onset schizophrenia spectrum disorders (TEOSS) study. Am J Psychiatry. 2008;165(11):1420–1431. doi: 10.1176/appi.ajp.2008.08050756. [DOI] [PubMed] [Google Scholar]
- 12.Stroup TS, Lieberman JA, McEvoy JP, Swartz MS, Davis SM, Rosenheck RA, et al. Effectiveness of olanzapine, quetiapine, risperidone, and ziprasidone in patients with chronic schizophrenia following discontinuation of a previous atypical antipsychotic. Am J Psychiatry. 2006;163(4):611–622. doi: 10.1176/ajp.2006.163.4.611. [DOI] [PubMed] [Google Scholar]
- 13.Weiden PJ, Newcomer JW, Loebel AD, Yang R, Lebovitz HE. Long-term changes in weight and plasma lipids during maintenance treatment with ziprasidone. Neuropsychopharmacology. 2008;33(5):985–994. doi: 10.1038/sj.npp.1301482. [DOI] [PubMed] [Google Scholar]
- 14.Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13(2):261–276. doi: 10.1093/schbul/13.2.261. [DOI] [PubMed] [Google Scholar]
- 15.Guy W. Clinical Global Impressions. Rockville, Maryland: National Institute of Mental Health; 1976. pp. 218–222. [Google Scholar]
- 16.Ganguli R. Behavioral therapy for weight loss in patients with schizophrenia. J Clin Psychiatry. 2007;68(Suppl 4):19–25. [PubMed] [Google Scholar]
- 17.Brar JS, Ganguli R, Pandina G, Turkoz I, Berry S, Mahmoud R. Effects of behavioral therapy on weight loss in overweight and obese patients with schizophrenia or schizoaffective disorder. J Clin Psychiatry. 2005;66(2):205–212. doi: 10.4088/jcp.v66n0208. [DOI] [PubMed] [Google Scholar]
- 18.Abnormal Involuntary Movement Scale (AIMS) Psychopharmacol Bull. 1988;24(4):781–783. [PubMed] [Google Scholar]
- 19.Barnes TR. A rating scale for drug-induced akathisia. Br J Psychiatry. 1989;154:672–676. doi: 10.1192/bjp.154.5.672. [DOI] [PubMed] [Google Scholar]
- 20.Simpson GM, Angus JW. A rating scale for extrapyramidal side effects. Acta Psychiatr Scand Suppl. 1970;212:11–19. doi: 10.1111/j.1600-0447.1970.tb02066.x. [DOI] [PubMed] [Google Scholar]
- 21.Diggle PJ, Liang KY, Zeger SL. Analysis of Longitudinal Data. Oxford, England: Oxford Science; 1994. [Google Scholar]
- 22.Ware J, Jr., Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 23.Kolotkin RL, Crosby RD. Psychometric evaluation of the impact of weight on quality of life-lite questionnaire (IWQOL-lite) in a community sample. Qual Life Res. 2002;11(2):157–171. doi: 10.1023/a:1015081805439. [DOI] [PubMed] [Google Scholar]
- 24.Marder SR, Essock SM, Miller AL, Buchanan RW, Casey DE, Davis JM, et al. Physical health monitoring of patients with schizophrenia. Am J Psychiatry. 2004;161(8):1334–1349. doi: 10.1176/appi.ajp.161.8.1334. [DOI] [PubMed] [Google Scholar]
- 25.Newcomer JW, Campos JA, Marcus RN, Breder C, Berman RM, Kerselaers W, et al. A multicenter, randomized, double-blind study of the effects of aripiprazole in overweight subjects with schizophrenia or schizoaffective disorder switched from olanzapine. J Clin Psychiatry. 2008;69(7):1046–1056. doi: 10.4088/jcp.v69n0702. [DOI] [PubMed] [Google Scholar]
- 26.Treating Elevated Cholesterol and Heart Disease: The Statins. Consumer Reports Best Buy Drugs. 2007 [Google Scholar]
- 27.Wu RR, Zhao JP, Jin H, Shao P, Fang MS, Guo XF, et al. Lifestyle intervention and metformin for treatment of antipsychotic-induced weight gain: a randomized controlled trial. Jama. 2008;299(2):185–193. doi: 10.1001/jama.2007.56-b. [DOI] [PubMed] [Google Scholar]
- 28.Wu RR, Zhao JP, Guo XF, He YQ, Fang MS, Guo WB, et al. Metformin addition attenuates olanzapine-induced weight gain in drug-naive first-episode schizophrenia patients: a double-blind, placebo-controlled study. Am J Psychiatry. 2008;165(3):352–358. doi: 10.1176/appi.ajp.2007.07010079. [DOI] [PubMed] [Google Scholar]
- 29.Jarskog L, Hamer R, Catellier D, Stewart D, LaVange L, Golden L, et al., editors. Metformin in the Treatment of Antipsychotic-induced Weight Gain in Schizophrenia. New Orleans, LA: 65th Society of Biological Psychiatry; 2010. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.