Abstract
In the setting of traditional residency training programs, physician–scientists are often limited in their ability to pursue research training goals while meeting clinical training requirements. This creates a gap in research training at a critical developmental stage. In response, Columbia University Medical Center’s Department of Psychiatry, in partnership with the New York State Psychiatric Institute, has created a formal Research Track Program (RTP) for psychiatry residents so that interested individuals can maintain their attention on research training during formative residency years. Clinical and research training are integrated through core clinical rotations on research units. With protected research time and clear developmental milestones for each year of training, the RTP allows research track residents to meet both clinical and research training goals while maintaining a healthy work–life balance. In coordination with existing postdoctoral research fellowship programs, research track residents can effectively jump-start fellowship training with advanced course work and consistent, continuous mentorship bridging residency and fellowship years. A key element of the program is its provision of core training in research literacy and extensive research opportunities for all residents, stimulating research interest across the whole residency program. Supported by the National Institutes of Health and a private foundation, this RTP capitalizes on a unique academic–private partnership to address many of the challenges facing physician–scientists. By integrating clinical and research exposures and offering protected research time, careful mentoring, and financial resources, the program aims to further the development of those most poised to establish careers in translational research.
Despite extensive advancements, translating science into clinical practice remains a challenge as evidenced by the 15- to 20-year gap between development of new knowledge and established standards for patient care.1 The reason for this gap is complex and multifaceted; however, it is increasingly apparent that highly trained physician–scientists are needed to design and conduct the translational research necessary to bridge bench and bedside.
The Roots of the Research Track Program
Columbia University Medical Center’s Department of Psychiatry, in partnership with the New York State Psychiatric Institute (NYSPI), has had a core mission of supporting the research careers of physician–scientists since being awarded its first National Institutes of Health (NIH) T32 postdoctoral research fellowship in 1988. However, the trajectory for physician–scientists has become increasingly arduous and lengthy as the process for becoming an independent investigator has become more competitive and uncertain.2 Physician–scientists generally apply for NIH career development awards seven to nine years after receiving their degrees, in contrast to their PhD counterparts, who apply between three to five years post degree. In addition, the average age of awardees receiving their first R01 is now in the 40s.3
Moreover, Physician–scientists are often faced with having to restart their research careers in the context of traditional residency programs. Lack of integration and attention to the unique developmental needs of these physicians during residency contributes to significant delays in attaining independence and increases the risk that talented scientists will choose other career paths. In response, Columbia’s Residency Training Program in Psychiatry developed a formalized Research Track Program (RTP) to better support and prepare residents with demonstrated interest and experience in research for careers in translational and clinical research. The program draws on faculty resources from previously established T32 fellowship training programs in order to jump-start mentorship, training, and research development during residency. Following other successful models at the University of Pittsburgh and the Medical University of South Carolina, the program also includes an appointed RTP director, clear developmental milestones, research-specific didactics, and consolidated protected time for research.4,5
The stepwise development of this RTP began in 2006 with the institution of monthly research track seminars and career development workshops and the addition of an RTP director in 2008. This was followed by a major reorganization of the clinical training program starting in 2009 and rolled out across two years. The goal of this reorganization was to consolidate core clinical training earlier in the program and decrease rotation lengths to time requirements set by the psychiatry residency review committee (RRC) while balancing clinical service needs and freeing up additional time for dedicated research during the latter two years of training.
Specifics and Opportunities of the RTP
Up to three residents are selected for the RTP within each resident class (25%); however, the vast majority of resources built into the RTP (mentorship, additional seminars, workshops, and didactic classes) are available to all residents. All residents have 20% time in the third year of residency and 80% in the fourth year to pursue elective interests. By decreasing inpatient rotations from eight months to the RRC requirement of six months, research track residents (RTRs) have two additional months for research (or approximately 20% more time) during the third year of residency.
Funded by an NIH R25 grant starting in 2009, the program provides RTRs with research supplies, statistical assistance, and travel support to attend scientific meetings. Since receiving a privately funded grant in 2010, the program has also been able to provide supplemental salary support to select RTRs. These stipends are competitively awarded to RTRs on the basis of prior research accomplishments, a dedicated research focus in translational neuroscience, and a firm commitment to pursue a research fellowship after graduation. This novel funding structure is modeled after Medical Scientist Training Programs for MD/PhD candidates, which provide additional stipends to offset the cost of living in exchange for committed research training6 with the goal of enhancing recruitment and retention of Physician–scientists pursuing translational research. Private funding also supports competitively awarded pilot grants available to all residents, not only RTRs, which may mediate the enhanced interest in research observed in non-RTP residents.
Creating the Integrated RTP
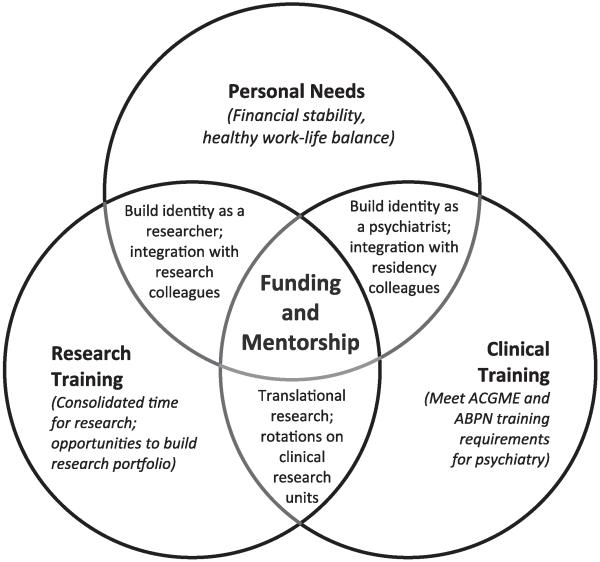
Barriers to supporting physician–scientists are numerous and stem from the inherent complexities of meeting dual clinical and research training goals. In developing our RTP, we considered frequent barriers facing Physician–scientists and proposed strategies to address these challenges during training (Table 1). Our RTP attempts to integrate research training, clinical training, and a healthy work–life balance. Below, we detail our approach to these components with a particular focus on mentorship and financial support, central to our conceptual model (Figure 1).
Table 1. Delineation of Specific Challenges Facing Physician–Scientist Training Goals Within Residency, and Proposed Solutions Within Columbia’s Research Track Program (RTP)*.
| Specific challenges | Proposed solutions within the RTP |
|---|---|
| Research training | |
| Delay in research endeavors |
|
| Limited opportunities to build research portfolio |
|
| Limited research mentorship |
|
| Limited integration with research colleagues |
|
| Limited integration with next level of training |
|
| Clinical training | |
| Competing clinical demands |
|
| Limited integration with residency colleagues |
|
| Personal needs | |
| Financial demands |
|
| Work–life balance |
|
This RTP is situated in Columbia University Medical Center’s Department of Psychiatry in partnership with the New York State Psychiatric Institute.
Figure 1.
A model for the Research Track Program (RTP) at Columbia University Medical Center’s Department of Psychiatry in partnership with the New York State Psychiatric Institute. The RTP adopts an integrated approach to clinical and research training while maintaining a focus on individual resident needs. The clinical training and research training goals overlap with personal needs as the resident develops his or her own identity as both a clinician and a researcher. A specific focus in translational research experiences within the program bridges clinical and research training. Extensive mentorship and financial support are critical for each component of the model. ACGME indicates Accreditation Council for Graduate Medical Education; ABPN, American Board of Psychiatry and Neurology.
The research training program
Hands-on research experience fosters competence and confidence critical to stoking and maintaining interest in research.7 However, protected time within residency training is often fragmented by clinical training requirements, limiting the opportunity to develop or cultivate a research focus.5,8 A consolidated structure that allows flexibility may foster a seamless integration of research and clinical goals, without compromising one for the other.
As an example, our training program initially had three months available for research during the first residency year and eight months during the fourth year. In between, some residents managed to carve out additional time for research. However, verbal feedback from residents suggested that this gap stalled momentum and created a significant obstacle to developing research goals. In response, we reoriented the training program with the first two years dedicated to cultivating mentorship and developing research proposals followed by concentrated, escalating research time within the latter years, leading up to fellowship training. Setting clear expectations and opportunities for RTRs within a structured, developmental framework helps residents prioritize training demands and balance clinical and research interests.4
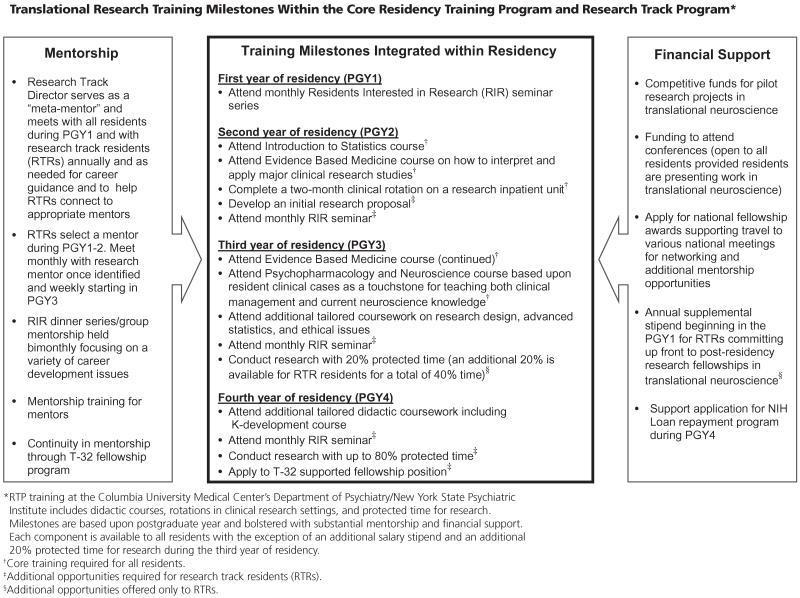
Within the RTP, specific research milestones are set for each year of training bolstered by significant mentorship and financial support (Chart 1). Required monthly seminars keep RTRs connected to their research goals and allow opportunities for networking and collaborating with peers. In these seminars, residents present their plans/work and receive feedback from peers and senior faculty. Seminars complement the core didactic curriculum for all residents. Additional course work is tailored to each RTR and selected from the extensive training infrastructure available to research fellows including courses on research design, advanced statistics, ethical issues, and research/grant writing skills.
Chart 1.
Senior residents are encouraged to participate in a K development course. This yearlong course breaks down the various elements of a K award grant application and encourages participants to share drafts within the class. Mock study sections are held with panels of experienced reviewers from the senior faculty, and a presubmission review service is also offered.
Mentorship is not only a crucial part of training for scientists but also perhaps the single most important element in securing progression in academia.9,10 Studies in biomedical and behavioral research in general, and in mental health and psychiatry in particular, have demonstrated that individuals who become successful, independent investigators are more likely to have had extended mentoring.9 This is especially true for women and minorities.11 Therefore, starting with application to the residency program, RTRs meet with research faculty in order to choose a long-term research mentor. Choosing a mentor and initial project by the end of the second year allows RTRs time to consolidate their identity as researchers and find their “niche.” During the third and fourth years, training turns toward a specific research project. RTRs are expected to have at least two first-authored, peer-reviewed publications by graduation. Manuscripts can be based on the mentor’s data or extant, publicly available data sets and/or literature reviews, provided they form the scaffolding for the “background and significance” section of a career development grant (K application).
Integration with the next phase of training, postresidency research fellowship, is critical.8 Thus, mentors are drawn from core faculty from T32-supported research fellowship programs available in the department. The RTP director helps residents select mentors who share their scientific interests, have a track record in supporting and launching the independent careers of mentees, and are a good “fit” in terms of chemistry. Mentor and mentee meet weekly during research portions of the training and ideally once a month during clinical rotations. Mentors are expected to attend seminars, workshops, and other educational programs of the RTP. Incentives to attract mentors include direct financial support of the RTRs through the RTP and subsequent fellowships, research supplies and pilot project funds available through the research track and other programs with in the department, and mentorship training.
Through the RTP, funds are competitively available for pilot projects and attendance at scientific meetings. The intent is to provide residents with a realistic experience in grant writing and proposal submission as well as to provide them with resources to support small-scale research projects. Projects that form the basis for future proposals and provide a head start toward K award development are prioritized. Funds to attend scientific meetings allow residents an opportunity to present their work, network with other researchers, and obtain additional mentorship.
Integration with clinical training
Early exposure to clinical research is key to stimulating ideas for translational research among basic science trainees. This is provided through clinical rotations on inpatient research services. While participating in clinical day-to-day management of patients before, during, and after their participation in research protocols, residents develop their clinical skills. Simultaneously, RTRs learn about research design by studying active clinical protocols and gain firsthand experience in their execution.
Throughout the RTP we aim to balance clinical training and research opportunities while maintaining residency class cohesion and meeting training requirements set by the psychiatry RRC and American Board of Psychiatry and Neurology. To minimize possible perceptions of inequality, we ensure that administrative responsibilities and call schedules are evenly distributed, and RTRs participate in all general residency course work. In addition, protected research time for RTRs does not translate into extra work for non-RTR peers. Because NIH R25 funds provide direct salary support for RTRs, departmental funds can be reallocated to other clinical staff to support ongoing patient care.
For example, the aforementioned reorganization of our curriculum included decreasing the consultation liaison rotation from four to two residents at a time. In addition, the rotation was shifted from the fourth year of residency to the second. To offset this change in manpower and clinical expertise, we were able to reallocate resident salaries to support additional consultation liaison fellows (fifth-year residents). In addition, although RTRs do two months less of inpatient psychiatry, attending physicians provide more direct care when resident staffing is lower so that the resident caseloads are not higher.
Most important, opportunities for general residents to participate in research are widely available (Chart 1). This includes facilitated mentorship, use of elective time for research, availability of pilot funds, participation in research seminars and workshops, and opportunities to join didactic experiences open to the RTRs. In addition, all residents receive core didactics in research literacy and rotate through a clinical research inpatient unit during the second year of residency.
As an added bonus, implementation of an RTP during residency has a “ripple effect” on research interests for all trainees. Clinical experiences that foster resident interest in patient-oriented research are critical for modeling clinical research as a priority and recruiting residents to the field.8 Experience suggests that required clinical research rotations along with an active RTP can attract general residents into research. For example, although each class has a maximum of three RTRs, 75% (9/12) of third-year residents during the 2011–2012 academic year elected to pursue research interests during the 20% time available for either research or additional training in outpatient psychopharmacology or psychotherapy. Four residents from this cohort are now applying to research-oriented fellowships. Only one of the four has a dual MD/PhD degree and was officially part of the RTP. Indeed, since 2006, 45% (9/20) of graduating residents pursuing research-oriented fellowships or faculty positions did not hold dual MD/PhD degrees. Of note, focus on recruiting MD/PhDs seems well placed, given that 11 of 18 (61%) MD/PhDs pursued research on graduation, whereas 9 of 66 (14%) other graduates did so.
Balancing personal factors
Although enhancing research opportunities within residency training is critical, it is unlikely to be sufficient if it neglects the financial and personal challenges facing promising physician–scientists.8,12,13 A key component of our RTP includes an environment that supports, models, and enables RTRs to effectively balance work–life priorities, an increasingly important value articulated by the current physician workforce.14,15 By providing a structured program with protected time, research is not limited to after hours, where it would be placed in direct competition with other personal obligations.
An annual workshop, “Work and Family: An Attainable Balancing Act,” directly addresses strategies for balancing an academic career with a rich family life. This workshop includes a panel of academic psychiatrists at various stages of their career sharing personal stories about managing family and work commitments. The format is question based, with content drawn from the residents’ specific interests, and is part of a group mentorship experience available through a Residents Interested in Research (RIR) dinner series. Bimonthly dinners allow informal interaction between residents, faculty, and research fellows. RIR attendance is expected for RTRs and open to all psychiatry residents. A resident committee selects topics focused on a variety of career issues, such as balancing clinical and research responsibilities, getting the most out of mentorship, choosing and using a research fellowship, and developing writing skills.
Financial strain is also a significant impediment to pursuing a research career. Data from 2002 indicate that over 80% of medical students have loans with an average debt of $104,000.8 On graduation, residents committing to research fellowship training are faced with a reduced income compared with their peers. As an example, 2012 T32 stipends for fourth- through seventh-year fellows range between $47,820 and $54,180,16 in contrast to a median annual salary of $154,500 for beginning psychiatrists in 2011 according to the Association of American Medical Colleges.17 This is compounded by the uncertainty of future grant funding necessary to sustain research endeavors.
Residents are often at a life stage with significant family and financial obligations. Through partnership with a private foundation, the RTP provides RTRs committed to fellowship training in translational neuroscience an annual stipend starting in the PGY1 year and each year of their clinical training. Although this could engender a sense of inequality among the residents, all residents are aware that the “price” of this support is an up-front commitment to a full-time research fellowship post graduation, in lieu of an attending salary and potentially lucrative private practice. RTRs are also encouraged to apply to the NIH Loan Repayment Program for clinical researchers during their senior year.18
Putting the RTP in Context
The Columbia–NYSPI RTP provides a customized approach to research training during a critical period in the development of a physician–scientist which combines and builds on the resident’s dual expertise in science and medicine during residency. Thus, the RTP targets a developmental stage often underaddressed in training programs.8
Similar to other successful psychiatry research tracks,4,5 this program has a formalized structure which begins with a focus on identifying mentors and developing research goals within the first two years and consolidates available research time into the third and fourth years. The program differs in its unique funding support, integration with the residency training program with widespread availability of research opportunities for non-RTRs, and coordination with T32 fellowships.
According to our review of data available from the American Medical Association, 294 residency training programs report research track options across pediatrics, general surgery, obstetrics–gynecology, family medicine, internal medicine, and psychiatry combined.19 Although this RTP has been developed for a psychiatry residency, the key components are likely applicable across disciplines. In a recent survey of pediatric residents, the most commonly identified influences on the decision to conduct research during residency training included the availability of time, mentorship, and opportunity.20 Similarly, a review of research programs within family medicine training noted that successful programs combined time for research, faculty involvement, a research curriculum, professional support, and opportunities for presenting research.10 The key goal of this program is to enhance the likelihood that trainees, especially MD/PhDs, will stay in research and tackle vexing scientific challenges facing psychiatry, in line with NIMH goals of augmenting the “pipeline.”21 Moreover, we aim to maximize the likelihood that trainees applying for K awards secure such funding earlier than recently observed. Through mentoring, protected time, and formal didactics in statistics, ethics, research design, and other topics, we seek to boost knowledge, confidence, and competence of trainees prior to fellowship.
Fundamentally, research training is a resource-intensive enterprise. It can pay back over time as researchers obtain grants and bring additional income to the department. However, at its core, it requires investment in trainees, with both money and time.
Despite these challenges, many components of this RTP could be maintained without external funding, as evidenced by the fact that the program began in 2006 without substantial financial support until 2009. Having a research infrastructure with accessible mentors is essential along with a critical mass of some research activity; however, smaller programs could partner with other departments or institutions to provide such resources. Within our own RTP, residents have occasionally collaborated with mentors at outside institutions. Internal resources can also be augmented by competitive national fellowship awards that provide travel funds to conferences and networking and mentorship opportunities. Departmental pilot grants do not have to be substantial, but they may require philanthropic efforts or reallocation of other funds. To free up protected research time, faculty may need to provide more direct patient care. All of this requires buy-in from top administration and a departmental culture supporting research development. It would be essential to tailor the basic principles, infrastructure, and components of this model to the specific resources, strengths, needs, setting, and culture of another department interested in implementing such a program.
The RTP at Columbia has had considerable success in recruiting and developing residents interested in research-oriented careers. Since 2007, each entering class of residents has been consistently above the 75 percentile in the mean number of publications and mean number of research experiences when compared with other categorical psychiatry programs, based on National Resident Matching Program data. The current RTP seeks to augment the pipeline of high-quality candidates continuing on to psychiatric research careers. Programs with the best track record in recruiting trainees who pursue research careers are those that provide protected time for research within a specific research curriculum and have concrete expectations and opportunities to present research.10,22 Thus, developing a RTP is an important step toward recruiting research-oriented medical students. As noted by others, “If you build it, they will come.”2
Future Directions
Additional advances in recruiting and retaining physicians in translational research careers may depend on the direction of national funding priorities and residency training requirements. For example, we recommend that the NIH reevaluate the current funding structure for research fellowships, particularly as it pertains to stipends which are woefully low. With science and technology considered a major driver of long-term economic growth,23 more foundations may be willing to consider investing in research training. The Accreditation Council for Graduate Medical Education may also play a role in creating additional flexibility for research within residency training. For example, as each RRC rolls out specific developmental milestones, opportunities for research could expand if training outcomes were based on demonstrated clinical competency and prioritized over meeting specified time requirements.24
Acknowledgments
Funding/Support: This work was supported by grants from the NIMH (5R25MH086466) and the Leon Levy Foundation.
Footnotes
Other disclosures: None.
Ethical approval: Not applicable.
Contributor Information
Dr. Melissa R. Arbuckle, Department of Psychiatry, Columbia University Medical Center and New York State Psychiatric Institute, New York, New York.
Dr. Joshua A. Gordon, Department of Psychiatry, Columbia University Medical Center and New York State Psychiatric Institute, New York, New York.
Dr. Harold A. Pincus, Department of Psychiatry, and codirector, Irving Institute for Clinical and Translational Research, Columbia University, New York, New York; New York-Presbyterian Hospital, New York, New York; RAND Corporation, Pittsburgh, Pennsylvania.
Dr. Maria A. Oquendo, Department of Psychiatry, Columbia University Medical Center and New York State Psychiatric Institute, New York, New York.
References
- 1.Proctor EK, Landsverk J, Aarons G, Chambers D, Glisson C, Mittman B. Implementation research in mental health services: An emerging science with conceptual, methodological, and training challenges. Adm Policy Ment Health. 2009;36:24–34. doi: 10.1007/s10488-008-0197-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ley TJ, Rosenberg LE. The physician-scientist career pipeline in 2005: Build it, and they will come. JAMA. 2005;294:1343–1351. doi: 10.1001/jama.294.11.1343. [DOI] [PubMed] [Google Scholar]
- 3.National Institutes of Health [Accessed February 18, 2013];National Institutes of Health Individual Mentored Career Development Awards Program. http://grants.nih.gov/training/K_Awards_Evaluation_FinalReport_20110901.pdf.
- 4.Gilbert AR, Tew JD, Jr, Reynolds CF, 3rd, et al. A developmental model for enhancing research training during psychiatry residency. Acad Psychiatry. 2006;30:55–62. doi: 10.1176/appi.ap.30.1.55. [DOI] [PubMed] [Google Scholar]
- 5.Back SE, Book SW, Santos AB, Brady KT. Training Physician–scientists: A model for integrating research into psychiatric residency. Acad Psychiatry. 2011;35:40–45. doi: 10.1176/appi.ap.35.1.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.National Institute of General Medical Sciences [Accessed February 18, 2013];Medical Scientist Training Program. http://www.nigms.nih.gov/Training/InstPredoc/PredocOverview-MSTP.htm.
- 7.Fraker LD, Orsay EM, Sloan EP, Bunney EB, Holden JA, Hart RG. A novel curriculum for teaching research methodology. J Emerg Med. 1996;14:503–508. doi: 10.1016/0736-4679(96)00090-x. [DOI] [PubMed] [Google Scholar]
- 8.Abrams MT, Patchan K, Thomas F. Research Training in Psychiatry Residency: Strategies for Reform. National Academies Press; Washington, DC: 2003. [PubMed] [Google Scholar]
- 9.Pincus HA, Haviland MG, Dial TH, Hendryx MS. The relationship of postdoctoral research training to current research activities of faculty in academic departments of psychiatry. Am J Psychiatry. 1995;152:596–601. doi: 10.1176/ajp.152.4.596. [DOI] [PubMed] [Google Scholar]
- 10.DeHaven MJ, Wilson GR, O’Connor-Kettlestrings P. Creating a research culture: What we can learn from residencies that are successful in research. Fam Med. 1998;30:501–507. [PubMed] [Google Scholar]
- 11.Leibenluft E, Dial TH, Haviland MG, Pincus HA. Sex differences in rank attainment and research activities among academic psychiatrists. Arch Gen Psychiatry. 1993;50:896–904. doi: 10.1001/archpsyc.1993.01820230066006. [DOI] [PubMed] [Google Scholar]
- 12.Draznin J. The “mommy tenure track.”. Acad Med. 2004;79:289–290. doi: 10.1097/00001888-200404000-00003. [DOI] [PubMed] [Google Scholar]
- 13.Wolf M. Clinical research career development: The individual perspective. Acad Med. 2002;77:1084–1088. doi: 10.1097/00001888-200211000-00004. [DOI] [PubMed] [Google Scholar]
- 14.Bunton SA, Corrice AM. Evolving workplace flexibility for U.S. medical school tenure-track faculty. Acad Med. 2011;86:481–485. doi: 10.1097/ACM.0b013e31820ce51d. [DOI] [PubMed] [Google Scholar]
- 15.Kirch DG, Salsberg E. Association of American Medical Colleges. The physician workforce challenge: Response of the academic community. Ann Surg. 2007;246:535–540. doi: 10.1097/SLA.0b013e3181571a39. [DOI] [PubMed] [Google Scholar]
- 16.National Institutes of Health [Accessed February 18, 2013];Ruth L. Kirschstein National Research Service Award (NRSA) stipends, tuition/fees and other budgetary levels effective for fiscal year 2012. http://grants.nih.gov/grants/guide/noticefiles/not-od-12-033.html.
- 17.Association of American Medical Colleges [Accessed February 18, 2012];AAMC Faculty Salary Survey Reports. Summary Statistics on Medical School Faculty Compensation for All Schools M.D. or Equivalent Degree, Clinical Science Departments/Specialties. 2010-2011. http://services.aamc.org/fssreports/ AAMC user ID and password required.
- 18.National Institutes of Health [Accessed February 18, 2013];Extramural Loan Repayment Program for Clinical Research. http://www.lrp.nih.gov/about_the_programs/clinical.aspx.
- 19.American Medical Association [Accessed February 18, 2013];FREIDA Online. Residency Fellowship Training Program Search. https://freida.ama-assn.org/Freida/user/viewProgramSearch.do.
- 20.Ullrich N, Botelho CA, Hibberd P, Bernstein HH. Research during pediatric residency: Predictors and resident-determined influences. Acad Med. 2003;78:1253–1258. doi: 10.1097/00001888-200312000-00014. [DOI] [PubMed] [Google Scholar]
- 21.National Advisory Mental Health Council Workgroup on Research Training [Accessed February 18, 2013];Investing in the Future. 2008 http://www.nimh.nih.gov/about/advisory-boards-and-groups/namhc/reports/investing-in-the-future.pdf.
- 22.Frieden C, Fox BJ. Career choices of graduates from Washington University’s medical scientist training program. Acad Med. 1991;66:162–164. doi: 10.1097/00001888-199103000-00008. [DOI] [PubMed] [Google Scholar]
- 23.Lane NF. [Accessed February 18, 2013];Science is the key to growth. New York Times. 2012 Oct 28; http://www.nytimes.com/2012/10/29/opinion/want-to-boost-the-economy-invest-in-science.html?_r=0. [Google Scholar]
- 24.ten Cate O, Scheele F. Competency-based postgraduate training: Can we bridge the gap between theory and clinical practice? Acad Med. 2007;82:542–547. doi: 10.1097/ACM.0b013e31805559c7. [DOI] [PubMed] [Google Scholar]