Abstract
Achalasia is an uncommon esophageal motility disorder characterized by the selective loss of enteric neurons leading to absence of peristalsis and impaired relaxation of the lower esophageal sphincter. Per-oral endoscopic myotomy (POEM) is a novel modality for the treatment of achalasia performed by gastroenterologists and surgeons. It represents a natural orifice transluminal endoscopic surgery (NOTES) approach to Heller myotomy. POEM has the minimal invasiveness of an endoscopic procedure that can duplicate results of the surgical Heller myotomy. POEM is conceptually similar to a surgical myotomy without the inherent external incisions and post-operative care associated with surgery. Initial high success and low complications rates promise a great future for this technique. In fact, POEM has been successfully performed on patients with end-stage achalasia as an initial treatment reserving esophagectomy for those without good response. The volume of POEMs performed worldwide has grown exponentially. In fact, surgeons who have performed Heller myotomy have embraced POEM as the preferred intervention for achalasia. However, the niche of POEM remains to be defined and long term results are awaited. We describe our experience with POEM having performed the first POEM outside of Japan in 2009, the evolution of our technique, and give our perspective on its future.
Keywords: Per-oral endoscopic myotomy, Achalasia, Heller myotomy, Natural orifice transluminal endoscopic surgery, Per-oral endoscopic myotomy, Minimally invasive surgery
Core tip: Per-oral endoscopic myotomy (POEM) is a minimally invasive endoscopic procedure that duplicates results of the surgical Heller myotomy. This innovative technique has been performed by both gastroenterologists and surgeons. POEM has been shown to be safe and effective in patients with classic achalasia and modest follow-up data. POEM has also been successfully applied in patients with hypertensive esophageal motor disorders as well as end-stage achalasia. It is recommended that prior to performing POEM, operators should have experience in endoscopic submucosal dissection or substantial training in animal models.
INTRODUCTION
Achalasia is an esophageal motility disorder where there is aperistalsis of the distal one-third of the esophageal body and the lower esophageal sphincter (LES) fails to relax in response to swallowing. Achalasia is noted equally in both genders with prevalence that ranges up to 1 per 10000 persons and it occurs across the age span, though diagnosis is usually made in middle age or later[1]. The majority of cases are idiopathic, but the syndrome can be associated with malignancy (especially involving the gastro-esophageal junction) and as a part of the spectrum of Chagas disease. Rarely, achalasia is genetically transmitted[2]. Achalasia is an uncommon prototypical esophageal motility disorder with characteristic clinical and esophageal manometry findings. The cardinal presenting symptom is dysphagia; usually for both solids and liquids. Other symptoms can include chest pain, regurgitation, heartburn, cough related to aspiration, and weight loss. Advanced cases can result in malnutrition. Achalasia is suggested by characteristic contrast imaging demonstrating a dilated esophagus with smooth distal narrowing that can resemble a “bird’s beak”, but formal diagnosis requires esophageal manometry. The necessary feature on manometry is a LES that does not consistently relax after swallowing. Common but more variable features are a hypertensive LES and disordered peristalsis in the esophageal body. High resolution manometry has refined the delineation of various subtypes of achalasia as defined by the more variable features[3]. The classification has therapeutic importance as those with “classical” (aperistalsis of esophageal body) respond better to endoscopic and surgical interventions than those with “vigorous” achalasia[4].
PRIOR CONVENTIONAL TREATMENTS FOR ACHALASIA
Medical treatment of achalasia with calcium channel blockers and other agents is considered to be ineffective. Therapy instead is directed towards disrupting or weakening the LES. Diminution of LES pressure after therapy is paramount in attaining relief from dysphagia[5,6]. Until recently, the three traditional options for this were botulinum (Botox) injection (BTI) into the LES, pneumatic dilation (PD) of the LES and surgical myotomy (often with subsequent fundoplication to minimize reflux). BTI has been well validated as therapy for achalasia with good short-term benefit, but has poor long-term efficacy at diminishing dysphagia[7,8]. However, it is a safe and effective treatment option for the infirm and elderly[9]. Pneumatic dilation has a well validated track record in relieving dysphagia in achalasia, though repeated dilations are often needed and some require sequentially larger balloons[10,11]. A pivotal study demonstrated therapeutic equivalence between PD and laparoscopic Heller myotomy with Dor’s fundoplication at 43 mo post-intervention in terms of LES pressure and relief from dysphagia[12]. Despite this, surgical myotomy remains the preferred modality for achalasia in the United States; perhaps because of medical-legal concerns related to PD perforation and the usual more durable response with myotomy[13]. The degree of esophageal dilation of the achalasia esophagus is less of a concern to the surgeon then previously, but the operator must ensure an adequate myotomy and distal esophagectomy (6+ cm), and up to 20% of patients may require repeat intervention[14].
EMERGENCE OF PER-ORAL ENDOSCOPY MYOTOMY
Per-oral endoscopic myotomy (coined “POEM”) developed as an offshoot of a technique to access the mediastinum in Natural Orifice Transluminal Endoscopic Surgery (NOTES)[15]. The POEM technique was first tested in a porcine model[16]. A key feature was creation of a submucosal tunnel with closure of mucosal entry site a distance away from the myotomy. Inoue extrapolated this method to perform the first POEM in humans[17]. We performed our first POEM in 2009 (the first outside Japan) as part of an IRB-approved prospective trial protocol at Winthrop University Hospital[18]. We have integrated our series data into a comprehensive international POEM (IPOEMS) survey that was completed in July 2012[19]. The volume of POEMs performed worldwide has increased dramatically but appears to be concentrated at several select centers and literature concerning this new modality has also been increasing; albeit at a slower pace.
INDICATIONS AND CONTRAINDICATIONS FOR POEM
Patients considered candidates for POEM must have a confirmed diagnosis of achalasia via manometry and secondary achalasia related to malignancy must be excluded. Consensus contraindications to POEM include severe pulmonary disease, significant coagulation disorder and prior therapy that compromise esophageal mucosal integrity including endoscopic mucosal resection (EMR), radiofrequency ablation (RFA) and radiation. With experience, operators have been more liberal in performing POEM in a variety of achalasia subtypes as well as hypertensive esophageal motility disorders. The technique was used successfully on a patient with diffuse esophageal spasm[20]. Patients with longstanding achalasia may develop a markedly dilated (“sigmoid”) esophagus that can require esophagectomy[21]. Despite this, Inoue described POEM performed in 16 such patients in his series[22]. POEM offers a minimally invasive treatment option that can be used initially, reserving esophagectomy for failures.
POEM TECHNIQUE
The technique of POEM is centered on creation of a submucosal tunnel within the distal esophagus where a myotomy is performed within this tunnel with dissection of the inner circular muscle of the esophagus and minimally dissection of the LES circular muscle. Equipment required for POEM is readily available and compatible with existing endoscopy instruments[23] (Table 1). Endotracheal intubation is performed and it is paramount to use carbon dioxide for endoscopic insufflations to minimize the risk of mediastinal emphysema and minimize barotrauma if pneumoperitoneum occurs. Endoscopy is performed on the fasted patient and the esophagus is cleared of any residual contents. Liquid antibiotic (gentamicin) is used to lavage the esophagus. The sequence of POEM is (1) submucosal injection, mucosal entry; (2) creation of the submucosal tunnel with subsequent; (3) distal esophageal circular muscle dissection; (4) LES myotomy; and (5) finally closure of the mucosal incision (Figure 1).
Table 1.
Per-oral endoscopic myotomy equipment
| High-definition diagnostic gastroscope |
| Transparent 4 mm distal cap attachment |
| Electrosurgical device for injection of saline, incision and cautery ( T-type HK hybrid knife- with Erbe jet pump) |
| Electrosurgical device for incision and cautery (Triangle tip knife) and injection of saline with Injector force Max 4 mm, 23-gauge injection needle |
| Electrosurgical high frequency generator (e.g., ERBE VIO 300D) |
| Coagulation 5 mm grasper (Olympus) |
| Endoscopic clips (Boston-Scientific, Olympus, Wilson-Cook) |
| Needle or trocar for potential decompression of capnoperitoneum (angiocatheter, Veress needle 120 mm) |
| Endoscopic dilating balloons- CRE balloon dilator (5.5 cm, 10-11-12 mm) multiple manufacturers (rarely required) |
| Submucosal injection: Methylene blue or indigo carmine diluted in saline |
CRE: Controlled radial expansion.
Figure 1.
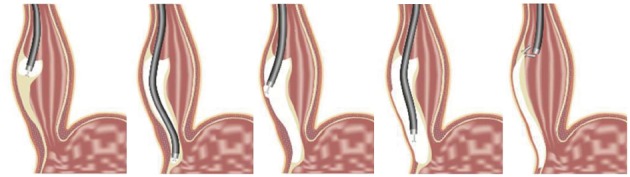
Per-oral endoscopic myotomy technique (© Winthrop University Hospital, 2012). A mucosal incision is performed after submucosal injection. Then, dissection of the submucosal tunnel is initiated and extended into the gastric cardia. Myotomy is performed of the circular layer and extended 2 cm into the gastric cardia. Finally, the entrance to the submucosal tunnel is closed with endoclips.
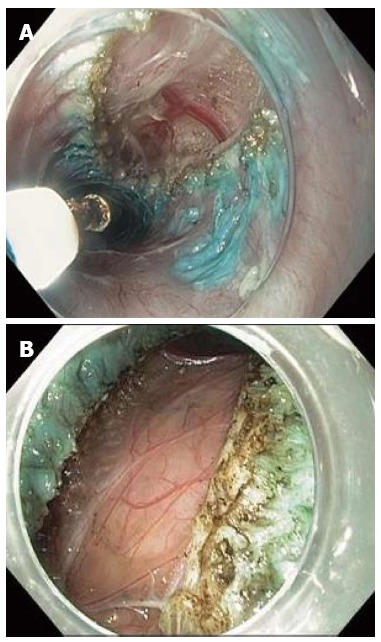
A submucosal injection of saline is used to expand the submucosal space ten to fifteen cm proximal to the LES and a two cm incision is then made (Figure 2A and B). The diagnostic gastroscope with cap is inserted into the submucosal space. The submucosal tunnel is extended with cautery and further injection. The submucosal tunnel located on the right side of the esophagus is extended to 2-3 cm distal to the LES and into the gastric cardia (Figure 2C). During dissection, if there is significant bleeding or the presence of larger vessels within the submucosa, the Olympus Coagrasper is employed to coagulate. The gastroscope is repositioned 2-3 cm distal to the initial mucosal incision site prior to initiating the myotomy. Dissection of the esophageal wall is performed with an electrical knife but actual dissection of the circular muscle is not performed until the plane between the inner circular and outer longitudinal esophageal muscles are clearly delineated (Figure 2D). The circular muscle myotomy is performed by hooking the inner muscle fibers with the knife and cutting them (Figure 2E and F). This dissection of muscle is continued distally until it is extended 1-2 cm into the cardia. This extension (cardiomyotomy) is partially based on the surgical myotomy experience where there is greater treatment efficacy with such extension[21]. This was also validated in a porcine POEM study[24]. The recognition of the LES in the tunnel can be quite challenging; especially for the inexperienced POEM operator. There may be cues such as submucosal palisading vessels (with less vasculature in the cardia) and widening of the submucosal space[20]. This can be correlated with tactile feedback of the endoscope entering the stomach. After the myotomy is completed with circular muscle excision from the mucosal entry to the cardia 1-2 cm distal to the LES, the endoscope is withdrawn into the esophageal lumen. The mucosal defect is closed with endoscopic clips (e.g., Boston Scientific Resolution) (Figure 2G and H). It is important to realize that the integrity of the esophageal mucosa is the barrier against mediastinal soiling after the procedure. Thus, it should not be breached during the tunnel creation and the entry site securely closed.
Figure 2.
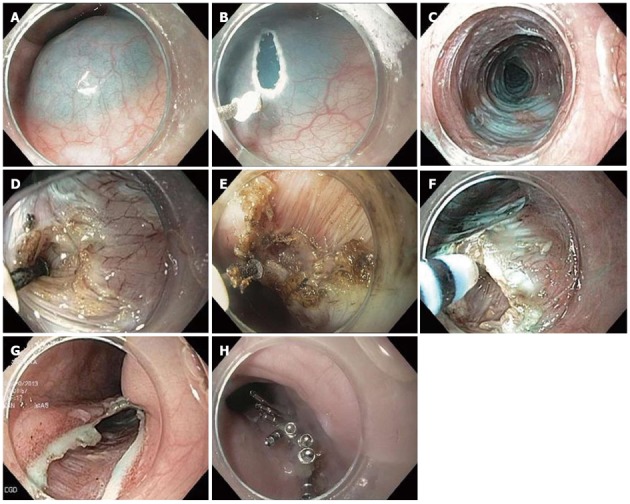
Per-oral endoscopic myotomy technique. A: Submucosal injection; B: Mucosal incision; C: Submucosal tunnel; D: Myotomy initiation; E: Dissection of the circular layer with longitudinal layer intact; F: Hooking of circular muscle layer with hybrid knife; G: Entrance to the submucosal tunnel; H: Closure.
EVOLUTION OF OUR POEM TECHNIQUE
There has been significant evolution of our technique due to our experience, newly available instruments and the experience of others worldwide (Table 2). We did not have access to endoscopic submucosal dissection (ESD) knives initially because they were not available in the United States. We partially overcame this by obtaining prototypes of ESD knives and using them in our animal lab, and thus are familiar with them prior to human use. We did our first POEM procedures with the tunnel created by a dilating balloon (often a biliary balloon). There is concern with the blunt dissection caused by the balloon in terms of possible mucosal damage. The myotomy was performed with a needle knife[17]. We used the triangular tip knife (Figure 3) when it became available and as described by Inoue[16]. Now, we employ the T-type hybrid knife (Figure 4) and avoid use of the balloon. Thus, submucosal injection can be made without need for exchanging devices. One POEM center (Shanghai group) touted the hybrid knife as superior to other knives and also used it in humans[25].
Table 2.
Evolution of per-oral endoscopic myotomy: A single center experience
| Initial | Subsequent | Rationale |
| Performed in operating room with surgeon present | Performed in endoscopy suite with surgeon available | Demonstrated to be a predictable and safe procedure. Moderate procedural time |
| Selected patients had no prior achalasia intervention | Selected patients include those with prior intervention (BTI, PD, HM) | POEM results here and elsewhere |
| Use of dilation balloons to dissect submucosal tunnel | No or little use of balloon. Evolution from needle knife to IT knife and now hybrid knife | Experience. More reliable dissection with knives. Hybrid knife with flushing capability |
| Variable orientation of initial incision site | Preference for 5 o’clock position | Improved dysphagia relief |
| Short myotomy-less than 6 cm | Myotomy tailored to manometry findings and components of Eckardt score | POEM results here and elsewhere |
| Partial LES myotomy of circular muscle only | Preference for complete myotomy unless low LESP on manometry | Concern for POEM efficacy. Post-POEM GERD usually manageable with medication |
POEM: Per-oral endoscopic myotomy; BTI: Botulinum (Botox) injection; LESP: Lower esophageal sphincter pressure; PD: Pneumatic dilation; HM: Heller myotomy; GERD: Gastroesophageal reflux disease.
Figure 3.
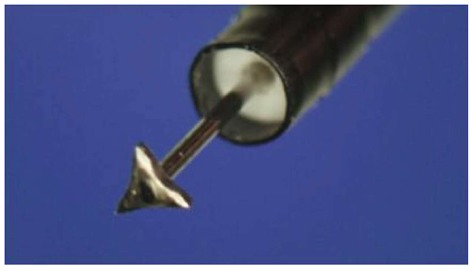
Triangular tip knife (Olympus) Courtesy Haruhiro Inoue.
Figure 4.

T-type hybrid knife (ERBE Elektromedizin GmbH). Courtesy John Day, ERBE (Marietta, GA).
LOWER ESOPHAGEAL MYOTOMY: ORIENTATION, DEPTH AND LENGTH
The LES in humans has multiple components that include a weaker thinner clasp (circular) part on the gastric lesser curvature centered at 2 o’clock with 12 o’clock defined as the most anterior point and a sling (oblique) fiber part centered on the left posterior lateral wall of the LES at 7 o’clock and draping over the anterior and posterior walls at 5 and 11 o’clock respectively[26] (Figure 5). The sling fibers represent a significant barrier to reflux. Laparoscopic Heller Myotomy usually involves transection of the sling fibers at 11 o’clock and thus reflux symptoms are common after laparoscopic heller myotomy (LHM). On the other hand, most POEM operators begin the SM tunnel at 2 o’clock which may minimize post-procedure reflux, but the tradeoff is with less than optimal efficacy because LES disruption is the key factor in achalasia intervention. We and others (Shanghai group) that employ a predominant 5 o’clock for the mucosal entry point and submucosal tunnel may have better relief of dysphagia because of dissection of the sling fibers but at the expense of mild reflux. At our center, patients with gastroesophageal reflux disease after POEM respond well to medical therapy. Conceivably, the decision regarding the mucosal entry site may be based on manometry findings where those achalasia patients with a normal or low LES pressure may receive a myotomy in the 2 o’clock while the majority of the other achalasia patients would be best served by a 5 o’clock incision. We can assess the quality of the myotomy by visualization and tactile assessment of the LES pressure by passage of the gastroscope. We and others assess the esophagogastric junction distensibility quantitatively with the EndoFlip system during POEM[27]. In one patient from our series, we were dissatisfied with the results of gastro esophageal junction distensibility after the 2 o’clock position myotomy was performed, so it was followed by a second complete myotomy at the 5 o’clock position with good results.
Figure 5.
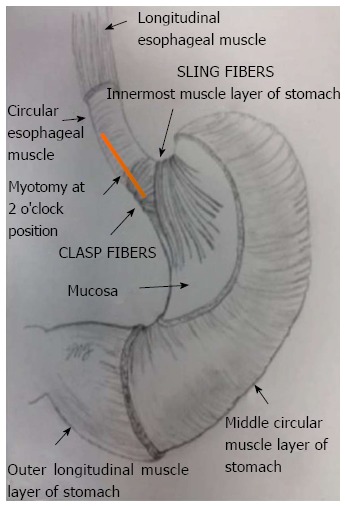
Human lower esophageal sphincter anatomy in relation to per-oral endoscopic myotomy myotomy orientation (© S.N. Stavropoulos, Winthrop University Hospital, 2012).
We, like Inoue, were conservative with our initial POEM patients, performing a myotomy less than 6 cm in length[16]. We have subsequently followed the consensus in the POEM literature where our myotomy usually is 8-10 cm. As with the mucosal incision site, we anticipate manometry findings to guide us in determining which patients would not require such a long myotomy (i.e., a patient with non-spastic achalasia). We tend to perform a full-thickness myotomy of the LES (Figure 6) because (1) we are concerned about relief of dysphagia; (2) the residual longitudinal layer seems flimsy and is easily disrupted after the circular muscle is resected; and (3) the longitudinal layer usually plays a lesser role in the barrier mechanism. Most POEM operators perform only a partial LES myotomy leaving the outer longitudinal muscle layer intact, but one group transitioned to a full-thickness myotomy and reported significant better esophageal emptying in treated patients after the transition[28].
Figure 6.
Full-thickness myotomy.
POSTOPERATIVE CARE
All patients are hospitalized after POEM. A gastrograffin swallow study is performed within 24 h to assess for leaks and gauge early efficacy. Antibiotics are often administered. The patient is usually given a liquid diet which is advanced and the patient is usually discharged within one-two days. Pain requiring narcotics is rarely reported and it seems less common than with LHM. A “second-look” endoscopy is usually not performed.
OUR POEM EXPERIENCE
We have performed POEM on 45 achalasia patients and have one year follow-up in more than half these patients (Table 3). These patients had a wide age range and many had significant co-morbid disease. The POEM is usually completed within two hours though additional time antecedent to the POEM is sometimes necessary to clear the esophagus. We have not excluded patients with prior intervention and have concluded like others that prior botulinum toxin injection creates more challenges for the POEM operator than prior pneumatic dilation in terms of scarring and that POEM can be performed successfully after laparoscopic Heller Myotomy[20]. We have performed POEM in patients with varying degrees of esophageal dilation including end-stage achalasia. Over 90% of our patients had relief of their dysphagia and improvement in global assessment (Eckardt scores). We are attempting to capture data recording post-therapy manometry. Data to date demonstrates at least 50% reduction in LES pressure post-myotomy. Other POEM groups have also generated excellent therapeutic results[29,30]. POEM failures were defined as patients with Eckardt scores > 4. There were two patients early in our experience that met this criterion and had salvage PD. Follow up Eckardt scores at one year post salvage PD for these patients are zero.
Table 3.
Per-oral endoscopic myotomy experience: Series data
| No. of patients |
| No. of completed POEMs |
| Age (mean, yr) |
| Achalasia by HRM subtype |
| I |
| II |
| III |
| Esophageal dilation > 6 cm or sigmoid |
| Percent of patients who failed prior conventional achalasia treatment (Endoscopic balloon dilation, Botulinum toxin injection, Heller myotomy) |
| Pre/Post eckardt score (mean) |
| Percent of patients with clinical success at 3 mo (Eckardt score £ 3) |
| Myotomy length (mean, centimeter) |
| Percent of technical errors |
| Minor mucosal perforations requiring clip closure |
| Needle decompression of capnoperitoneum |
| Percent of adverse events |
| Surgical intervention/conversion |
| ICU or step down unit stay |
| Prolonged hospital stay > 5 d |
| Significant blood loss or blood transfusion |
| POEM related readmission |
POEM: Per-oral endoscopic myotomy; HRM: High resolution manometry; ICU: Intensive care unit.
We had an excellent safety record thus with our POEM patients with no life-threatening complications (Table 3). There were several patients with capnoperitoneum early in the series possibly related to mucosal flap injury, but these were easily treated with needle decompression. We emphasized the necessity of carbon dioxide during POEM. One POEM group had an unduly high rate of subcutaneous and mediastinal emphysema and pneumothorax that may relate to room air used in POEM[31]. We are not aware of any documented POEM mortality. Published data on complications is sparse and the IPOEMS database infers a low rate (< 5%) of complications which include the above and bleeding within the submucosal tunnel and one reported para-esophageal abscess[18].
FUTURE PERSPECTIVES
There is a paucity of literature on POEM and to date only series from five centers[26-28,32,33]. We are unique in that our POEM operator is a gastroenterologist and procedures are now done in the endoscopy suite. In spite of our success with POEM, some insurers have not sanctioned the use of the procedure-some terming it “experimental.” We anticipate consensus guidelines in the near future to deal with the issues mentioned about variability of technique as well training and credentialing guidelines. Training will likely include an animal model due to the low incidence of achalasia[34]. A comparative trial between POEM and LHM yielded similar results for both arms[35] and we expect further such studies.
As mentioned, POEM was originally developed as an innovation for NOTES and this work continues[36]. The submucosal tunnel endoscopic resection technique (STER) is an offshoot of POEM, and allows removal of lesions in the muscularis propria and submucosa[37].
CONCLUSION
POEM for esophageal achalasia is a novel and seemingly effective technique. Further validation is expected, but it appears already to have carved a niche in the armamentarium for achalasia. There are some controversies regarding technique that need to be resolved. There may be obstacles in the future concerning available training and availability of skilled operators.
Footnotes
P- Reviewer Bassotti G S- Editor Wen LL L- Editor A E- Editor Wang CH
References
- 1.Sadowski DC, Ackah F, Jiang B, Svenson LW. Achalasia: incidence, prevalence and survival. A population-based study. Neurogastroenterol Motil. 2010;22:e256–e261. doi: 10.1111/j.1365-2982.2010.01511.x. [DOI] [PubMed] [Google Scholar]
- 2.Gockel HR, Schumacher J, Gockel I, Lang H, Haaf T, Nöthen MM. Achalasia: will genetic studies provide insights? Hum Genet. 2010;128:353–364. doi: 10.1007/s00439-010-0874-8. [DOI] [PubMed] [Google Scholar]
- 3.Kessing BF, Smout AJ, Bredenoord AJ. Clinical applications of esophageal impedance monitoring and high-resolution manometry. Curr Gastroenterol Rep. 2012;14:197–205. doi: 10.1007/s11894-012-0253-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bansal A, Kahrilas PJ. Has high-resolution manometry changed the approach to esophageal motility disorders? Curr Opin Gastroenterol. 2010;26:344–351. doi: 10.1097/MOG.0b013e32833aaf61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ghoshal UC, Rangan M, Misra A. Pneumatic dilation for achalasia cardia: reduction in lower esophageal sphincter pressure in assessing response and factors associated with recurrence during long-term follow up. Dig Endosc. 2012;24:7–15. doi: 10.1111/j.1443-1661.2011.01159.x. [DOI] [PubMed] [Google Scholar]
- 6.Yu L, Li J, Wang T, Zhang Y, Krasna MJ. Functional analysis of long-term outcome after Heller’s myotomy for achalasia. Dis Esophagus. 2010;23:277–283. doi: 10.1111/j.1442-2050.2009.01031.x. [DOI] [PubMed] [Google Scholar]
- 7.Martínek J, Siroký M, Plottová Z, Bures J, Hep A, Spicák J. Treatment of patients with achalasia with botulinum toxin: a multicenter prospective cohort study. Dis Esophagus. 2003;16:204–209. doi: 10.1046/j.1442-2050.2003.00329.x. [DOI] [PubMed] [Google Scholar]
- 8.Gutschow CA, Töx U, Leers J, Schäfer H, Prenzel KL, Hölscher AH. Botox, dilation, or myotomy? Clinical outcome of interventional and surgical therapies for achalasia. Langenbecks Arch Surg. 2010;395:1093–1099. doi: 10.1007/s00423-010-0711-5. [DOI] [PubMed] [Google Scholar]
- 9.Bassotti G, D’Onofrio V, Battaglia E, Fiorella S, Dughera L, Iaquinto G, Mazzocchi A, Morelli A, Annese V. Treatment with botulinum toxin of octo-nonagerians with oesophageal achalasia: a two-year follow-up study. Aliment Pharmacol Ther. 2006;23:1615–1619. doi: 10.1111/j.1365-2036.2006.02907.x. [DOI] [PubMed] [Google Scholar]
- 10.Zerbib F, Thétiot V, Richy F, Benajah DA, Message L, Lamouliatte H. Repeated pneumatic dilations as long-term maintenance therapy for esophageal achalasia. Am J Gastroenterol. 2006;101:692–697. doi: 10.1111/j.1572-0241.2006.00385.x. [DOI] [PubMed] [Google Scholar]
- 11.Eckardt VF, Gockel I, Bernhard G. Pneumatic dilation for achalasia: late results of a prospective follow up investigation. Gut. 2004;53:629–633. doi: 10.1136/gut.2003.029298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Boeckxstaens GE, Annese V, des Varannes SB, Chaussade S, Costantini M, Cuttitta A, Elizalde JI, Fumagalli U, Gaudric M, Rohof WO, et al. Pneumatic dilation versus laparoscopic Heller’s myotomy for idiopathic achalasia. N Engl J Med. 2011;364:1807–1816. doi: 10.1056/NEJMoa1010502. [DOI] [PubMed] [Google Scholar]
- 13.Weber CE, Davis CS, Kramer HJ, Gibbs JT, Robles L, Fisichella PM. Medium and long-term outcomes after pneumatic dilation or laparoscopic Heller myotomy for achalasia: a meta-analysis. Surg Laparosc Endosc Percutan Tech. 2012;22:289–296. doi: 10.1097/SLE.0b013e31825a2478. [DOI] [PubMed] [Google Scholar]
- 14.Sweet MP, Nipomnick I, Gasper WJ, Bagatelos K, Ostroff JW, Fisichella PM, Way LW, Patti MG. The outcome of laparoscopic Heller myotomy for achalasia is not influenced by the degree of esophageal dilatation. J Gastrointest Surg. 2008;12:159–165. doi: 10.1007/s11605-007-0275-z. [DOI] [PubMed] [Google Scholar]
- 15.Sumiyama K, Gostout CJ, Rajan E, Bakken TA, Knipschield MA. Transesophageal mediastinoscopy by submucosal endoscopy with mucosal flap safety valve technique. Gastrointest Endosc. 2007;65:679–683. doi: 10.1016/j.gie.2006.10.017. [DOI] [PubMed] [Google Scholar]
- 16.Pasricha PJ, Hawari R, Ahmed I, Chen J, Cotton PB, Hawes RH, Kalloo AN, Kantsevoy SV, Gostout CJ. Submucosal endoscopic esophageal myotomy: a novel experimental approach for the treatment of achalasia. Endoscopy. 2007;39:761–764. doi: 10.1055/s-2007-966764. [DOI] [PubMed] [Google Scholar]
- 17.Inoue H, Minami H, Kobayashi Y, Sato Y, Kaga M, Suzuki M, Satodate H, Odaka N, Itoh H, Kudo S. Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy. 2010;42:265–271. doi: 10.1055/s-0029-1244080. [DOI] [PubMed] [Google Scholar]
- 18.Stavropoulos SN, Harris MD, Hida S, Brathwaite C, Demetriou C, Grendell J. Endoscopic submucosal myotomy for the treatment of achalasia (with video) Gastrointest Endosc. 2010;72:1309–1311. doi: 10.1016/j.gie.2010.04.016. [DOI] [PubMed] [Google Scholar]
- 19.Stavropoulos SN, Modayil RJ, Friedel D, Savides T. The International Per Oral Endoscopic Myotomy Survey (IPOEMS): a snapshot of the global POEM experience. Surg Endosc. 2013:Apr 3; Epub ahead of print. doi: 10.1007/s00464-013-2913-8. [DOI] [PubMed] [Google Scholar]
- 20.Shiwaku H, Inoue H, Beppu R, Nakashima R, Minami H, Shiroshita T, Yamauchi Y, Hoshino S, Yamashita Y. Successful treatment of diffuse esophageal spasm by peroral endoscopic myotomy. Gastrointest Endosc. 2013;77:149–150. doi: 10.1016/j.gie.2012.02.008. [DOI] [PubMed] [Google Scholar]
- 21.Duranceau A, Liberman M, Martin J, Ferraro P. End-stage achalasia. Dis Esophagus. 2012;25:319–330. doi: 10.1111/j.1442-2050.2010.01157.x. [DOI] [PubMed] [Google Scholar]
- 22.Inoue H, Tianle KM, Ikeda H, Hosoya T, Onimaru M, Yoshida A, Minami H, Kudo SE. Peroral endoscopic myotomy for esophageal achalasia: technique, indication, and outcomes. Thorac Surg Clin. 2011;21:519–525. doi: 10.1016/j.thorsurg.2011.08.005. [DOI] [PubMed] [Google Scholar]
- 23.Oelschlager BK, Chang L, Pellegrini CA. Improved outcome after extended gastric myotomy for achalasia. Arch Surg. 2003;138:490–495; discussion 495-497. doi: 10.1001/archsurg.138.5.490. [DOI] [PubMed] [Google Scholar]
- 24.Bonin EA, Moran E, Bingener J, Knipschield M, Gostout CJ. A comparative study of endoscopic full-thickness and partial-thickness myotomy using submucosal endoscopy with mucosal safety flap (SEMF) technique. Surg Endosc. 2012;26:1751–1758. doi: 10.1007/s00464-011-2105-3. [DOI] [PubMed] [Google Scholar]
- 25.Zhou PH, Cai MY, Yao LQ, Zhong YS, Ren Z, Xu MD, Qin XY. Peroral Endoscopic Myotomy for Esophageal Achalasia by HybridKnife: A Case Report. Case Rep Gastrointest Med. 2012;2012:325479. doi: 10.1155/2012/325479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stein HJ, Liebermann-Meffert D, DeMeester TR, Siewert JR. Three-dimensional pressure image and muscular structure of the human lower esophageal sphincter. Surgery. 1995;117:692–698. doi: 10.1016/s0039-6060(95)80014-x. [DOI] [PubMed] [Google Scholar]
- 27.Rieder E, Swanström LL, Perretta S, Lenglinger J, Riegler M, Dunst CM. Intraoperative assessment of esophagogastric junction distensibility during per oral endoscopic myotomy (POEM) for esophageal motility disorders. Surg Endosc. 2013;27:400–405. doi: 10.1007/s00464-012-2484-0. [DOI] [PubMed] [Google Scholar]
- 28.von Renteln D, Inoue H, Minami H, Werner YB, Pace A, Kersten JF, Much CC, Schachschal G, Mann O, Keller J, et al. Peroral endoscopic myotomy for the treatment of achalasia: a prospective single center study. Am J Gastroenterol. 2012;107:411–417. doi: 10.1038/ajg.2011.388. [DOI] [PubMed] [Google Scholar]
- 29.Inoue H, Kudo SE. Per-oral endoscopic myotomy (POEM) for 43 consecutive cases of esophageal achalasia. Nihon Rinsho. 2010;68:1749–1752. [PubMed] [Google Scholar]
- 30.Swanstrom LL, Kurian A, Dunst CM, Sharata A, Bhayani N, Rieder E. Long-term outcomes of an endoscopic myotomy for achalasia: the POEM procedure. Ann Surg. 2012;256:659–667. doi: 10.1097/SLA.0b013e31826b5212. [DOI] [PubMed] [Google Scholar]
- 31.Ren Z, Zhong Y, Zhou P, Xu M, Cai M, Li L, Shi Q, Yao L. Perioperative management and treatment for complications during and after peroral endoscopic myotomy (POEM) for esophageal achalasia (EA) (data from 119 cases) Surg Endosc. 2012;26:3267–3272. doi: 10.1007/s00464-012-2336-y. [DOI] [PubMed] [Google Scholar]
- 32.Zhong YS, Li L, Zhou PH, Xu MD, Ren Z, Zhu BQ, Yao LQ. Effects of peroral endoscopic myotomy on esophageal dynamics in patients with esophageal achalasia. Zhonghua Wei Chang Wai Ke Zazhi. 2012;15:668–670. [PubMed] [Google Scholar]
- 33.Costamagna G, Marchese M, Familiari P, Tringali A, Inoue H, Perri V. Peroral endoscopic myotomy (POEM) for oesophageal achalasia: preliminary results in humans. Dig Liver Dis. 2012;44:827–832. doi: 10.1016/j.dld.2012.04.003. [DOI] [PubMed] [Google Scholar]
- 34.Eleftheriadis N, Inoue H, Ikeda H, Onimaru M, Yoshida A, Hosoya T, Maselli R, Kudo SE. Training in peroral endoscopic myotomy (POEM) for esophageal achalasia. Ther Clin Risk Manag. 2012;8:329–342. doi: 10.2147/TCRM.S32666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hungness ES, Teitelbaum EN, Santos BF, Arafat FO, Pandolfino JE, Kahrilas PJ, Soper NJ. Comparison of perioperative outcomes between peroral esophageal myotomy (POEM) and laparoscopic Heller myotomy. J Gastrointest Surg. 2013;17:228–235. doi: 10.1007/s11605-012-2030-3. [DOI] [PubMed] [Google Scholar]
- 36.Grund KE, Lehmann TG. Transesophageal NOTES--a critical analysis of relevant problems. Minim Invasive Ther Allied Technol. 2010;19:252–256. doi: 10.3109/13645706.2010.510670. [DOI] [PubMed] [Google Scholar]
- 37.Gong W, Xiong Y, Zhi F, Liu S, Wang A, Jiang B. Preliminary experience of endoscopic submucosal tunnel dissection for upper gastrointestinal submucosal tumors. Endoscopy. 2012;44:231–235. doi: 10.1055/s-0031-1291720. [DOI] [PubMed] [Google Scholar]


