Abstract
Purpose
This study investigates whether motion density maps based on passive infrared (PIR) motion sensors and the average time out and average density per hour measures of the density map are sensitive enough to detect changes in mental health over time.
Method
Within the sensor network, data are logged from PIR motion sensors which capture motion events as people move around the home. If there is continuous motion, the sensor will generate events at 7 second intervals. If the resident is less active, events will be generated less frequently. A web application displays the data as activity density maps showing events per hour with hours on the vertical axis and progressive days on the horizontal axis. Color and intensity provide textural indications of time spent away from home and activity level. Texture features from the co-occurrence matrix are used to capture the periodicity pattern of the activity (including homogeneity, local variation, and entropy) and are combined with the average motion density per hour and the average time away from home. The similarity of two different density maps is represented by a number that is computed in feature space as the distance from one map to the other, or a measure of dis-similarity. Employing a retrospective approach, density maps were compared with health assessment information (Geriatric Depression Scale, Mini Mental State Exam, and Short Form Health Survey -12) to determine congruence between activity pattern changes and the health information20. A case by case study method, analyzed the density maps of 5 individuals with identified mental health issues. These density maps were reviewed along with the averages of time out of apartment per day per hour and average density per hour for hours at home and mental health assessment scores to determine if there were activity changes and if activity patterns reflected changes in mental health conditions.
Results & Discussion
The motion density maps show visual changes in the client’s activity, including circadian rhythm, time away from home, and general activity level (sedentary vs. puttering). The measures are sensitive enough, yielding averages of time out of apartment and average density per hour for hours at home that indicate significant change. There is evidence of congruence with health assessment scores. This pilot study demonstrates that density maps can be used as a tool for early illness detection. The results indicate that sensor technology has the potential to augment traditional health care assessments and care coordination.
Keywords: passive sensors, early illness detection, technology and mental illness, motion density mapping
As with other medical problems, the risk of depression and dementia in the elderly increases with other illnesses and with declines in functional abilities1. One conceptual framework that may be employed to assist in the detection of changes in mental health status is the Early Illness Detection Model. This model can be used to identify typical patterns of decline including plateaus and step downs that depict functional changes. Coupled with the deployment of sensor systems in the homes of older adults, and utilizing density mapping, changes in activity patterns that are likely to be associated with depression and dementia can be detected earlier with the goal of alerting health care practitioners of changes in medical conditions. Early alerts allow for medical interventions to be addressed sooner, which assists in the management of disease processes21–24. This article will describe the Early Illness Detection Model and the density mapping technology produced from a passive sensor system. Using a retrospective perspective, a case by case study analysis will be presented using the model and technology to track activity patterns associated with dementia and depression. This approach is used in an attempt to illustrate the use of this model for the management of behavioral health issues.
Conceptual Framework: Early Illness Detection Model
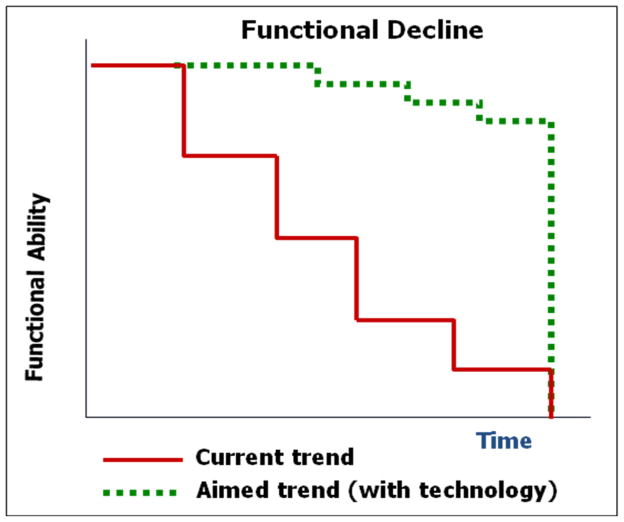
The conceptual model is based on what is known about aging through the research literature. Typical patterns of functional decline are depicted as elders age including plateaus where no measureable decline occurs and precipitous step-downs marked by dramatic functional declines, often the result of a significant health event or change in health status. The underlying premise is that if the beginning of the change or decline can be identified early through the use of technology enhancements, then medical interventions can be offered earlier and in a timely manner in order to stop or slow down the decline21–24. The result is increased functional ability and independence over the current trend.
Figure 1 depicts a trajectory pattern of health events where there is a normal baseline of functioning which is disrupted by a health event and a decline. This decline is followed by a plateau or new baseline of functional ability. This new baseline is maintained until the next serious health crisis or event. For older adults with chronic illnesses, their baseline for normal activity level and functional ability may change with each of these health events.
Figure 1.
Trajectory of Functional Decline
Functional declines often herald episodes of acute illness or exacerbation of chronic illness2. Delay in recognition of these events and appropriate notification of care providers leads to delayed treatment, delayed recovery, and higher risk of morbidity and mortality3. The key to continued function and independence is to identify problems (acute illness, exacerbation of chronic illness) while they are still small - before they become big problems- and offer timely interventions designed to change the trajectory in functional decline25.
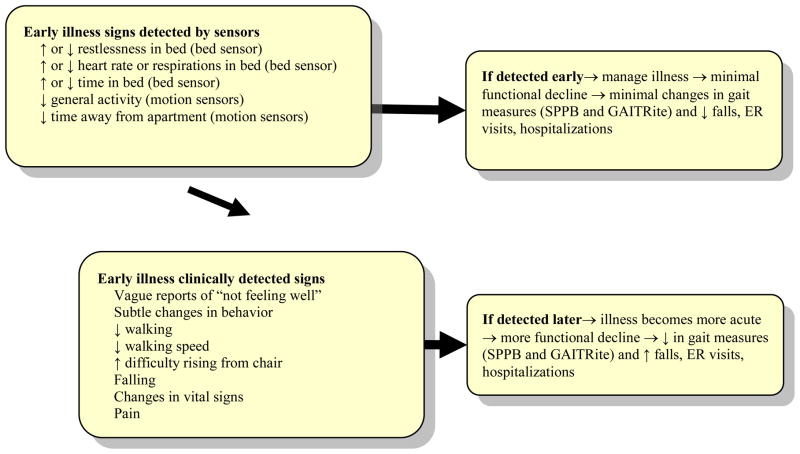
The original early illness detection model was developed to depict changes and exacerbations of physical illnesses. Figure 2 is the original version of the Early Illness Detection Model4. As stated above, this model is predicated on the theory that if physical illnesses and exacerbations in illnesses are detected earlier, medical intervention can be provided and the illnesses are treated before the medical condition becomes severe4, 25. Using sensor technology, our earlier work specifically looked at increases or decreases in bed restlessness, heart rate/respirations, amount of time in bed, and decreases in general activity and time away from apartment. Clinical indicators included verbal complaints, decreased walking, difficulty standing up, changes in vital signs, falls, and pain complaints. Our previous research has indicated that this model does indeed identify medical problems earlier and through timely intervention, residents have been able to avoid premature nursing home placement4, 25.
Figure 2.
Early Illness Detection Model
This study applies the model to detect early onset and exacerbations of episodes of dementia and depression. Technology in the form of sensor networks, offers an alternative approach that may be more feasible, cost effective and less intrusive in monitoring such illnesses5.
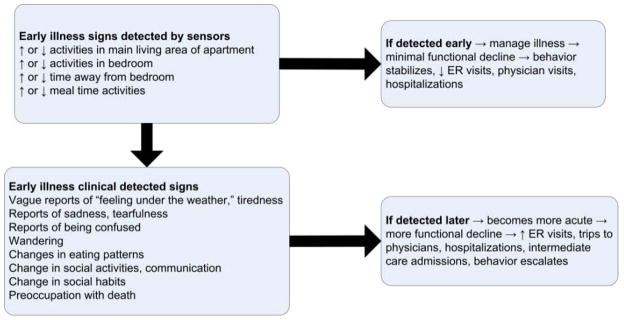
Figure 3 is the revised version of the Early Illness Detection Model modified for use with dementia and depression. This model guides the sensor system refinement and tracks the outcomes which are specific to early illness detection and clinical management of two behavioral health issues and the exacerbations of these illnesses. The same major premise drives this revised model – detection of early onset and/or exacerbations of mild dementia or depression provides opportunities for early clinical treatment of these behavioral health problems. Changes in activity patterns serve as an alert that further assessment is in order. Once activity pattern changes are identified then additional assessments can occur earlier. If illnesses and exacerbations are detected and managed at an earlier stage, it can prevent excessive visits to physicians’ offices with undifferentiated complaints, ER visits, hospitalizations and/or transfers to intermediate care facilities6, 21–24.
Figure 3.
Early Illness Detection Model Revised for Dementia and Depression
To detect activity pattern changes, a precursor for both dementia and depression, the identification of changes in participants’ level of regular or baseline activities is key to early recognition of changes in mental health status. Dementia and depression can both present with either decreases in activities and normal patterns of behavior or increases in activities and normal patterns of behavior. For instance, early symptoms of depression can manifest as an increase in sleep activity or a decrease in sleep activity. Early onset of dementia can present with increase in wandering out of the apartment or it might present with decreases in venturing away from the apartment. Therefore, it is important to measure each participant’s regular or normalized patterns of behavior in a baseline information assessment that can be obtained through medical assessments, interviews, clinical observations and technology enhancements. This baseline can then be compared with any changes in activity or patterns of behavior that are indicated by the sensor data and clinical observations. This baseline will change over time with each episode of functional decline.
METHOD
Sample
The sample population was drawn from residents at TigerPlace, which is an independent living facility that emphasizes the promotion of research and the development of new technologies that can eventually be expanded to other settings. Tiger Place is based on an aging in place philosophy, so the intent with residents is to help them remain in their apartments and maintain independence for as long as possible. Residents pay a monthly fee to live at Tiger Place, and if additional nursing or rehabilitative care is required, they pay extra for care packages. There are 65 residents at TigerPlace, 46 women and 19 men. All of the residents are white with the exception of one Asian male. There are 12 married couples and the 41 remaining residents are single. The age range is from 69 to 95 years. About 80% of the residents have at least one chronic disease, and many have more than one. Common chronic diseases include diabetes, heart disease, and arthritis. A few have early stage dementia related illnesses and a few have a mental illness diagnosis. They are not at above normal risk for depression or dementia as determined by health records and admission assessment tests.. Some residents use a variety of assisted mobility devices including scooters, wheelchairs, walkers, and canes. There are 56 apartments and a custom designed technology infrastructure which makes it a unique setting in which to test new and innovative approaches to the use of technology to detect illnesses. Motion sensor systems are currently deployed in 38 apartments (19 in the sensor study and 19 in the control group). There is IRB approval for this project and all residents participate in aging in place evaluations; therefore, each resident provides informed consent for the use of their health assessment information which is collected in the electronic health record maintained for this project. The case studies were drawn from this sample.
Technology Enhancements/Sensor Network System
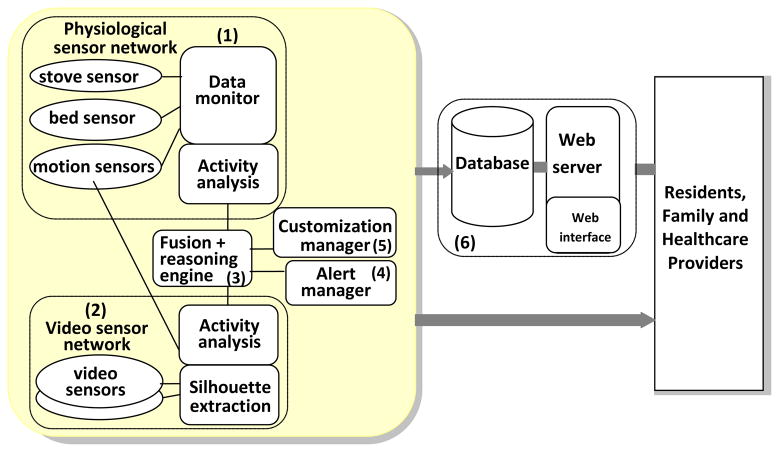
This research project used an integrated sensor network system. A pictorial representation is depicted in figure 4. The network includes six essential components : (1) a passive physiological sensor network with data monitor and motion sensors, stove sensors, and bed sensor7,8, (2) an event-driven, video sensor network that hides identifying features of the residents, through the use of a voxl character, (3) a reasoning engine that combines sensor and video data and analyzes patterns of behavioral activity, (4) a flexible alert manager, (5) a component for providing customization of sensor configuration, alert specification, and data access for each resident, and (6) a database server and web interface that provides interactive retrieval and visualization of the sensor data9 .The system is non-invasive and uses simple, low- cost sensor technologies coupled with specialized mathematical filtering and analysis. Passive infrared (PIR) motion sensors are installed to detect presence in a particular room (e.g., bathroom or kitchen) as well as for specific activities. For example, a motion sensor installed on the ceiling above the shower detects showering activity; motion sensors installed discretely in cabinets and refrigerator detect kitchen activity such as food preparation; one installed on the ceiling above the outside doorway detects exit activity. Through previous research, the PIR motion sensors are proven to be an effective and convenient way to monitor activity in a non obtrusive manner5.
Figure 4.
Integrated Sensor Network System
Activity Density Map
The main aim of our research is to measure patterns of movement and activity at a baseline and then to capture changes in these patterns which may be indicative of changes in physical and mental health functioning. The activity density map is one of the web based visual representations of movement and activity that is developed from the data obtained from the sensor network system. Both motion activity density and time away from home were captured using the visualization tool of a density map. In a motion density map, different colors represent different levels of density in the motion sensor data as shown in figure 5. The density d is computed as the number of all motion sensor hits s during an hour divided by time at home during that hour, t.
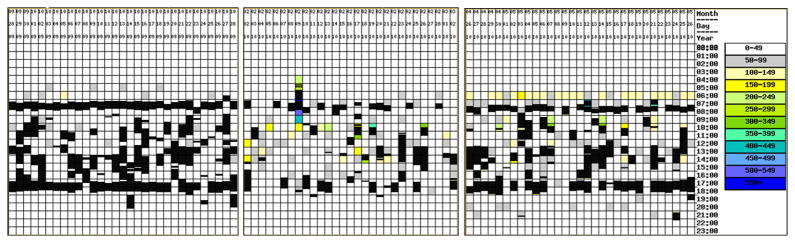
Figure 5.
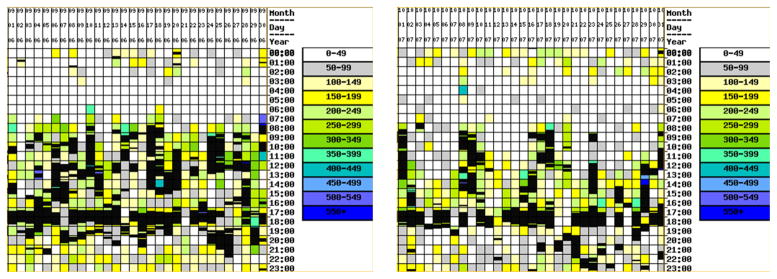
Monthly activity density maps generated using motion sensors for a resident showing a decline in mental health status over time. The vertical axis depicts time of day and the horizontal axis depicts day of the month. Colorful areas depict time and movement in apartment. Black areas depict time out of the apartment.
The density is defined as d = s/t. Motion sensors generate events every seven seconds if continuous motion is detected. Our lab tests captured one-sensor density values ranging from 14 hits/hour for near motionless sitting to over 300 hits/hour for pacing. The visualization results in a graphic representation of movement in the apartment including location of the movement, intensity of the movement, and a time recording of when the movement occurred. In Figure 5, the x-axis shows hours in a day; the Y-axis shows days in a month. Black represents time away from home, and the density levels range from 50 (gray) to 150 (yellow) to 300 (green) to 550 (blue). White indicates that no sensors were fired therefore, there is no movement. This mapping technique measures the intensity of the activity or movement in the area as well. It has the capability of differentiating between no activity to some activity to moderate activity to heavy activity and can depict the day and time in which the activity took place. This system also hides identifying features of the resident through the unique mapping display 9. In addition to the color mapping, we developed a line graph of daily activities which displays the amount of movement that occurs in the living environment over time with the X axis representing the numerical computation of sensor hits and the Y axis representing time in two week increments. Through using this passive sensor system, our research team has been able to identify health events and we found several cases of early illness detection. From our preliminary work, we have observed that the sensor data is capable of tracking changes in activity related to illness such as congestive heart failure, stroke, and others10, 11. Our attention now turns to the use of this technology for management of dementia and depression since both of these mental illnesses are prevalent in the older adult population.
Certain types of activity pattern changes are classically associated with depression and dementia12, 13. These changes in activity patterns are similar for both illnesses and include increases and decreases in movement within living areas, wandering or puttering behavior, changes in eating patterns, changes in self care, changes in social activity, to name a few. Due to the similar activity changes associated with each of these illnesses, we screened for both simultaneously. Using the Early Illness Detection Model, our hypothesis asserts that the sensor system will alert to earlier recognition of differences or changes in activity patterns associated with depression and dementia associated with the illnesses and exacerbations of the illnesses. Once differences in activity levels are identified, further assessment for mental illnesses can occur, and treatment, if indicated, may occur earlier. Changes in activity patterns are determined by comparing baseline data to the data collected over time. An example of a density map showing a resident with a decline in mental status is depicted in figure 5.
This figure depicts monthly activity density maps that illustrate changes in activity level and time out of the apartment as this resident’s dementia progressed. The first map (left) indicates that the resident was quite active. The black boxes show that this resident went out of the apartment frequently, and the color of the density map indicates a very high activity level. The second map (right) indicates less movement inside and outside of the apartment. The maps illustrate this resident’s active life before the cognitive decline and more sedentary life following the dementia diagnosis.
Health Assessment Records
Health and mental health screenings are conducted on each resident every 6 months using standard assessment instruments. The following instruments were used as part of the resident health assessment record:
Geriatric Depression Scale- Short Form (GDS-15) - This shortened version was developed by Sheikh and Yesavage14 and contains 15 items that had the highest correlation with depressive symptoms (r=.84). It is a self rating screening test for depression in older adults, intended primarily for clinical applications. The higher the score, the greater the likelihood that the patient has depression. Its psychometric properties have been tested in a variety of studies with differing results. Overall the scale has been found to have sufficient reliability and validity15. Scores of five or more indicate that depression is present.
Mini Mental State Exam (MMSE) – This instrument is an 11 question measure of mental status that assesses orientation, concentration, serial subtraction, immediate and delayed verbal memory, language, 3- step praxis, and ability to copy geometric design. A low score indicates cognitive impairment may be present. Its test-retest reliability has been reported at r=.89 and r= .9916. A normal score is considered 24 or higher with some variability for education level.
Short Form Health Survey (SF-12) – This instrument is a shortened version of the Rand 36 item Health Survey. It is used to measure perceptions of general health and mental health. The scale is based on 0 – 100 points. Higher scores indicate higher perceived health and mental health wellness. Psychometric test results have been varied; overall it has been found to have good reliability and validity17.
Scores obtained from these instruments were compared with the density map sensor data to determine if changes in the density maps were congruent with the resident health assessments.
RESULTS
Retrospective Analysis Using Case by Case Method
Using a retrospective case by case analysis approach, the density maps were compared with the health assessment record to determine congruence between the activity pattern changes and the health information. Both the health assessment data and the density map data were examined from past records. Health assessments are given ever 6 months. These assessments occur at different times for different residents depending on the resident’s date of admission to the facility. Upon entering the facility, each resident has an admission health assessment and then again at 6 month intervals. Activity data obtained from the density maps begins to be collected at the time the sensors are installed in a resident’s apartment and the resident consents to employ the sensors. Once the sensors are activated, data is collected continuously. Baseline activity patterns are determined through an examination of the data collected over time. In reviewing the data, normal patterns of activity emerge, along with deviations to these normal patterns. In our analysis, both the health assessment and density map data were examined to determine patterns and congruence between activity patterns and 6 month assessment scores. Our approach was employed to demonstrate the use of sensor mapping to depict activity pattern changes in relation to mental health. We used a case by case qualitative method of analysis to establish consistency in pattern changes between cases over time26. Specifically, five case studies are presented, Three in which there is a dual diagnosis of dementia and depression, one in which the resident was diagnosed with dementia only and one in which the resident was diagnosed with depression only. Summaries of assessment scores and other data determined through an examination of each case can be found in Table 1 which contains a time matrix for all cases. Further explanation of Table 1 occurs in the discussion section.
Table 1.
Time Matrix of Cases
| T1 First Map | T2 Second Map | T3 Third Map | Overall | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Cases | Assessment Scores & Sensor Results | Baseline or Decline | Assessment Scores & Sensor Results | Decline or Improvement | Intervention | Assessment Scores & Sensor Results | Decline or Improvement | Intervention | Congruence between map and scores |
| Case 1 |
SF-12 63.08 GDS 1 MMSE 27 ATO 4.48 AD 44.07 |
Baseline |
SF-12 48 GDS 2 MMSE 25 ATO 0.43 AD 38.49 |
Decline | Assessment by health care team |
SF- 12 62 GDS 1 MMSE 29 ATO 3.31 AD 65.38 |
Improvement | Medication change Physician intervention Counseling |
Yes Density map depict Baseline Decline Improvement Time away |
| Case 2 |
SF-12 37.87 GDS 9 MMSE 22 ATO 0.77 AD 97.47 |
Decline |
SF-12 53.04 GDS 2 MMSE 18 ATO 1.80 AD 110.41 |
Improvement | Physician Intervention Hospital Medication change More assistant care Counseling |
SF-12 54.6 GDS 7 MMSE 16 ATO 1.47 AD 129.36 |
Improvement & Decline | Increase physician monitoring Increase in attendant care Counseling |
Yes Density map depict Decline Improvement New Baseline Increased home activity Time away |
| Case 3 |
SF -12 51.32 GDS 6 MMSE 29 ATO 3.33 AD 24.18 |
Baseline |
SF-12 48.45 GDS 6 MMSE 22 ATO 0.38 AD 32.08 |
Decline | Assessment by health care team |
SF-12 49.84 GDS 6 MMSE 27 ATO 3.07 AD 76.88 |
Improvement | Psychiatric assessment Medication change Counseling Supportive CNA visits |
Yes Density map depict Baseline Decline Improvement Decrease home activity Time away |
| Case 4 |
SF-12 59.03 GDS 2 MMSE 30 ATO 4.23 AD 8.65 |
Baseline |
SF-12 20.55 GDS 9 MMSE 23 ATO 1.70 AD 25.86 |
Decline | Assessment by health care team |
SF-12 54.85 GDS 2 MMSE 28 ATO 3.38 AD 31.31 |
Improvement & Decline | Physician intervention Medication change Rehab hospital Counseling Family intervention |
Yes Density map depict Baseline Decline Improvement Increase home activity Time away |
| Case 5 |
SF-12 57.96 GDS 2 MMSE 30 ATO 4.85 AD 8.25 |
Baseline |
SF-12 28.09 GDS 10 MMSE 27 ATO 0.24 AD 37.66 |
Decline | Assessment by health care team |
SF-12 48.78 GDS 2 MMSE 23 ATO 1.70 AD 43.20 |
Improvement & Decline | Hospital Medication change Physician intervention Counseling Supportive CNA visits |
Yes Density map depict Baseline Decline Improvement Increase home activity Time away |
Key: ATO = Average time out per day per hour; AD = Average density per hour for hours at home
Case Study 1
Figure 6 displays the density map for one resident with a diagnosis of depression and dementia, with multiple health problems. The time period observed is from the end of June 2010 through the middle of February 2011. Figure 6 captures three density map snapshots for that period. The June 29 – July 29, 2010 period is when the resident was the most active. It serves as the baseline in terms of activity and behavior. Typical behavior includes a lot of activity outside of the apartment including going out of the apartment for breakfast, morning and afternoon events, going out for dinner in the evening and attending some activities after dinner. Depicted in the density map are frequent and numerous periods of leaving the apartment as indicated by the black areas. These black areas occur at meal times and other times during the day indicating that the resident is engaging in activities and appointments outside of the apartment. There are periods of moderate activity in the apartment as indicated by the yellow and green areas. These areas occur at times when the resident is home participating in self care activities. At this time, the resident’s SF-12 Mental Health (SF-12 MH) score was 63.8, indicating good mental health, the GDS score was 1 indicating no depression, and the MMSE score was 27, indicating healthy cognition.
Figure 6.
Density map showing three points in time (baseline, decline, and improvement) of a resident with dementia and depression
The next density map in figure 6 is for the time period September 4 – October 3, 2010. This map depicts an entirely different activity pattern. What is striking is the reduction in the black areas, and the prevalence of white and gray areas. The white and gray areas indicate little to no movement in the apartment. The increase in yellow areas means some moderate activity inside the apartment and also some attendant care. Scores for this period include a 15.8 point decline in the SF-12 MH to 48, an increase of one point in the GDS to 2, and a two point decline in the MMSE to 25. This resident typically withdraws when experiencing mental health changes and declines to participate in activities. The density map visualizes these very behavior changes. This density map depicts the resident’s decline.
The last density map on this resident is from the period January 10 – February 11, 2011 after health care intervention was complete. After receiving medication, medical treatment and counseling the resident is engaged once again in external activities and meals. While there are still gray and white areas, they are much more sporadic, and there is increasing patches of black. During this quarterly assessment, the SF-12 MH score increased to 62, the GDS decreased a point to 1, and the MMSE increased by 4 points to 29. Average time out per day per hour was 4.48 at baseline. At time 2, there is a decrease to 0.43 which depicts the decline. At time 3, there is an increase to 3.31 after health interventions were complete. Average density per hour for hours at home was 44.07 at baseline, 38.49 at time 2 when there was a status decline, and then an increase to 65.38 at time 3, after the health interventions. At time 3, this resident is reengaging in social activities and is more productive and active at home.
Case Study 2
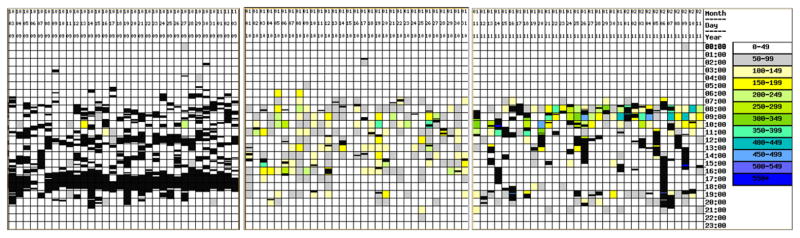
Figure 7 is a density map of a resident diagnosed with Lewy Body Dementia. The resident lives alone in the apartment. This figure shows three different time snapshots covering the period from April 2, 2010 – May 11, 2011. There is a strong support network including a daughter who visits daily. The resident receives attendant care which can be observed by the blue areas at the beginning of the day. We are able to discern that this is attendant care activity because the movement in the apartment is more intense than usual. Despite the support both from family and from the living environment, this resident experienced an exacerbation of the illness in 2010. This resident was hospitalized and upon returning, began to understand the reality of the diagnosis. This exacerbation and realization was followed by a low mood period in which the resident presented as depressed. At this time, a referral was made to a mental health expert. The density map below is for the period of April 2, 2010 – May 2, 2010. This case starts with a density map that indicates decline to depict how the technology can track decline and then improvement. There are areas of yellow and green which depicts moderate activity, particularly around meal time. There are periods of white indicating no movement. This resident watches several TV shows, and this accounts for some of the low movement. There are few black areas, and when they occur, they are short, indicating that the resident is not venturing out of the apartment much, and when the resident does venture out, there is a prompt return back to the apartment. Before the hospitalization, the resident enjoyed leaving her apartment frequently, so, for this resident this activity pattern is atypical. Normally, there is much movement and walking about the corridors of the facility. The resident is typically social and attends a variety of activities. Health assessment scores initially were 37.87 on the SF- 12 MH, a score of 9 on the GDS, and a score of 22 on the MMSE.
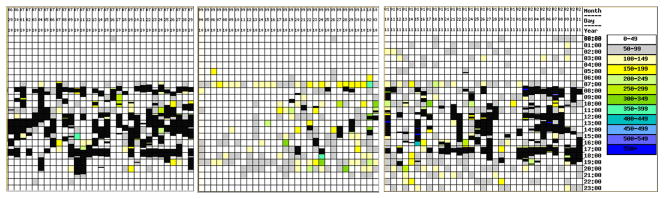
Figure 7.
Density map showing three points in time (decline, improvement, decline) of a resident with Lewy Body Dementia
Figure 7 depicts the activity pattern of this same resident during the July 24 – August 19, 2010. The resident’s mood has improved as the resident learns how to adjust and cope with the diagnosis. The resident received counseling and there was a medication adjustment made by her physician. During this period, the resident expressed determination to retain as much physical and mental functioning for as long as possible. There is a return to walking around the corridors, although the walking periods are shorter. The resident tries to attend as many activities as health permits. The black areas have increased both in frequency and duration. The activity in the apartment has increased and there are more blue areas, again indicating attendant care activity. The white areas depicting no movement are still present, however, there are fewer of them and of shorter duration. The resident is spending less time in the apartment watching TV and more time out of the apartment attending activities. The health assessment scores for this period are 53.04 on the SF-12 MH, a score of 2 on the GDS; and a score of 18 on the MMSE. These scores indicate the resident’s cognition has declined, which is expected for persons with this diagnosis. However, there was improvement in the GDS and SF-12 MH depression scores of this resident following treatment. The change in activity patterns within the density maps are consistent with the lessening of depressive symptoms. This resident was able to live independently and coped with the functional decline with increased support and assistance. The last figure on this resident is for the period April 11, 2011 – May 11, 2011. As the Lewy Body Dementia progressed, the resident’s activity patterns changed. There is less outside activity as the resident’s mobility became more difficult. However, the resident is managing to go outside of the apartment. There is more activity and attendant care provided in the apartment as depicted by the increases in green and blue. Health assessment scores for this period are 54.6 for the SF-12 MH, one point improvement over the last assessment, 7, on the GDS, an increase of 5 points, indicating more presence of depression, and an MMSE score of 16 which indicates another decline in cognitive functioning. Average time out was estimated to be 0.77 at time 1, point of decline, which increased to 1.80 at time 2, immediately after health care intervention. As time progressed there is a decrease to 1.47 at time 3, which is in line with the expected progressive nature of the illness. The average density per hour for hours at home was the lowest at the point of decline or time 1 at 97.47. After health care intervention, at time 2, the density increased to 110.41, and at time 3, we see another increase to 129.36. The density results depict more movement in the apartment overtime, partly as a result of the resident moving around more, and partly due to the increase in attendant care as the disease process progresses. This case was purposely examined with the first point in time indicating a decline due to the fact that Lewy Body Dementia quickly progresses. This case provides a rare opportunity to view improvement and stabilization from time 1 to time 3.
Case Study 3
Figure 8 is a density map of a resident with a diagnosis and history of depression which has been managed and followed by a geriatric psychiatrist. The typical pattern of activity for this resident includes many hours a day spent away from the apartment. This resident attends activities within the facility and outside the facility. The hours away are represented by the black areas on the density map. During the time period of August 17, 2009 – September 18, 2009, the resident’s density map shows a typical pattern of activity. The resident ventures out of the apartment consistently for breakfast and dinner, and participates in a variety of activities after breakfast. When in the apartment, the resident typically reads or watches TV, taking an occasional nap. These activities explain the white areas in the density map. Major grooming and showering activity occurs in the evening hours and this pattern is captured by the yellow areas at the end of the day. The resident’s assessment scores are 51.32 on the SF-12 MH, 6 on the GDS, and 29 on the MMSE.
Figure 8.
Density map showing three points in time (baseline, decline, improvement) of a resident with chronic Depression.
The next density map in Figure 8 is for the period of March 26 – April 25, 2010. This density map is very different and depicts changes in activity patterns. Due to a number of personal losses, this resident experienced an exacerbation of the depression. Low energy was reported which resulted in less movement out of the apartment. The resident withdrew to the apartment, and indicated being too tired to go out or participate in activities. The resident had trouble eating and stopped going to the dining room. In this density map, there is a noticeable reduction of black areas. There is an increase in gray, yellow, and green areas which are a result of an increased presence and activity in the apartment, and visits from care providers. The resident’s assessment scores for this period are 48.45 on the SF-12 MH a reduction of almost 3 points, a 6 on the GDS, no change on this score, and a 22 on the MMSE, a 7 point decrease from the last assessment. The resident’s assessment scores have decreased or remained the same for this period. It is important to point out that exacerbations of depressive illness can impact memory, which is how the depression presented in this case.
The next density map in Figure 8 is for the period October 1 – October 31, 2010. This period in time is after the resident received treatment for the depression including a medication change, counseling, and increased certified nursing assistant (CNA) visits for socialization. There is much more activity in the resident’s apartment during the early morning hours depicted by the yellow colors followed by black areas when the resident goes to the dining area for breakfast. The black areas have increased once again, indicating more movement outside of the apartment. The resident’s participation in outside activities increased as did meal attendance in the dining room. There is the occasional visit by family depicted by the aqua colors in the map. Assessment scores for this period are 49.84 on the SF-12, an increase of 2 points, a score of 6 on the GDS, indicating no change from the last assessment and a score of 27 on the MMSE which is an increase of 5 points from the last assessment. The residents’ assessment scores have improved or remained the same for this time period. It is not surprising that the GDS scores were consistent since the resident has been taking antidepressant medication for many years. The average time out scores at baseline was 3.33 which then declined to 0.38 at time of decline in mental health status. After receiving treatment, the average time out scores increased to 3.07. These numbers support that after treatment, the resident became more active outside of the home. The average density per hour was 24.18 at baseline which increased to 32.08 at time of decline and further increased to 76.88 after mental health treatment was obtained. These particular results can be explained by the fact that more care was provided to this resident during time 2 through time 3, and the resident spent more time in the apartment at time 2 and time 3.
Case Study 4
The next case study is of a resident who was assessed for depression and dementia. Figure 9 contains three density maps. The first density map records movements in and out of the apartment during the period of September 28, 2009 – October 28, 2009. As can be observed from this typical pattern, when the resident is in the apartment, there is low activity as depicted by the grey and white areas in the map. There is only one patch of color during this time period. There are many black areas indicating movement out of the apartment and this resident spends a lot of time out of the apartment, participating in breakfast and dinner in the dining room areas, and activities both in and out of the facility throughout the day. Typically this resident loves to move around. Baseline health assessment information was obtained by proxy of two health care providers who provided health care to this resident. The resident’s SF-12 MH score was 59.03, the GDS was 2, and the MMSE was 30.
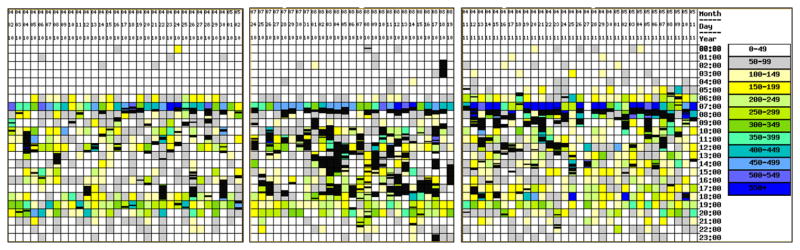
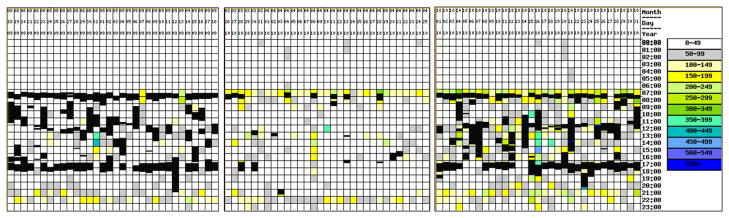
Figure 9.
Density map showing three points in time (baseline, decline, improvement and new baseline) of a resident with dementia and depression
The figure below is another density map of this resident in a different snap shot of time – February 2, 2010 – March 2, 2010. The resident’s physical functioning has declined and low mood is present. Health assessment scores for this period were a 20.55 on the SF-12 MH, a decline of 38 points; a score of 9 on the GDS, an increase of 7 points; and a score of 23 on the MMSE, a decline of 7 points. During this time period, there is a large reduction in time spent outside of the apartment. Meals are not consistently taken in the dining areas and the resident is attending fewer and fewer external activities. There is more intensity of movement in the apartment throughout the day and the map contains more yellow areas from light to dark and one green area.
This reflects more activities being done in the apartment and more visits from family and care providers occurred during this period. As activity declined, the medical team recommended intensive rehabilitation treatment and this resident was hospitalized, with the goal of a return to the apartment at a higher functioning level. The next figure is of a density map on this same resident post hospitalization from April 26, 2010 – May 26, 2010. There is more movement in and out of the apartment as depicted by the black areas. This resident’s mood and cognition improved after her hospitalization as indicted by her health assessment scores. On the SF-12 MH, the score during this time period was a 54.85; the score on the GDS was a 2, both scores indicating an improvement in mood. The score on the MMSE was a 28, indicating an improvement in cognition as well. However, the density map also has more yellow and green areas which indicate more intense movement within the apartment. Some of the increased movement is due to the resident receiving some attendant care in the morning. The resident’s physical functioning declined during this period to a 38.35 on the SF-12 Physical. The more intense movement in the apartment is due to increased attendant care provided to this resident to assist her post hospitalization. The average density per hour figures support this more intense movement from time 1, where the baseline was 8.65 to time 2, where there is an increase to 25.86, and after treatment, there continues to be an increase in apartment activity to 31.31. With the changes in the average density, there were also changes in the average time out scores. The resident’s baseline at time 1 was 4.23, which lowered to 1.70 at time of decline. After intervention and hospitalization, the average time out increased to 31.31, which is an improvement, however a decline from the baseline. The average time out at time 3 is this resident’s new baseline.
Case Study 5
This case study is of a resident with a history of dementia and depression as well as several health conditions including Peripheral Vascular Disease, and later on the resident had a severe leg laceration. The first density map in Figure 10 is for the period October 3 – November 3, 2009. This map indicates a baseline pattern of activity for this resident. The resident’s typical behavior is to primarily stay out of the apartment, as can be noted by the numerous black areas in the density map. The resident enjoys sitting in the lounge area, attending activities, and taking meals in the dining room. The resident is not in this apartment very much and when there, the door is frequently left open. The resident is a social, outgoing person. The assessment scores for this resident were obtained by proxy of two health care providers who provided hands on care to this resident. The assessment scores are a score of 57.96 on the SF-12 MH, and a score of 2 on the GDS. These scores indicate overall good mental health with no evidence of depression. The MMSE score for this period is a 30 which indicates no dementia present. The next density map is for the period January 1 – January 31, 2010. At this time, the resident is experiencing increased dementia and anxiety. There is a fall which results in a tear to the skin, and a trip to the hospital. The resident returns to the apartment and there are altered and noticeable mental health changes. The resident withdraws to the apartment and reduces activity outside of the apartment. There is a marked decrease in the black areas in the density map and when they do occur, they are around lunch time. There is not much movement in the apartment as indicated by the gray areas in the density map. Yellow areas appear in this map, which indicate more attendant care being provided to this resident. The assessment scores for this period are a score of 28.09 on the SF-12 MH, a score of 10 on the GDS, both scores indicating problems with mental health functioning. The MMSE for this period was a 27. The resident was hospitalized several times. Intervention included a medication change, counseling, and an increase in socialization visits by the nursing staff.
Figure 10.
Density map showing three points in time (baseline, decline, improvement and new baseline) of a resident with dementia and depression
The last density map on the resident is for the period January 11 – February 11, 2011. After many medical treatments, the resident’s condition stabilizes, and while the activity does not return to baseline, there is improvement in venturing out of the apartment, depicted by a return of some of the black areas. Movement in the apartment and attendant care has increased as noted by more yellow and blue areas. The resident experienced more physical and cognitive decline during this period requiring more assistance with her activities of daily living. Assessment scores for this period are a 48.78 on the SF-12 MH an increase of 20 points, a score of 2 on the GDS, a decrease of 8 points. These scores indicate an improvement in mental health status. The MMSE for this period is 23, a difference of 4 points which indicates decline in cognitive functioning. The steady decline is also apparent when examining the average time out scores which were a 4.85 at baseline, and then declining to a 0.24 at time 2, and then increasing to a 1.70 at time 3 after treatment was received. While the resident improved, the mental status continued to decline as indicated by the MMSE scores. Average density continued to increase from the baseline of 8.25. At time 2, the average density is 37.66, which then increases to 43.20 at time 3. This increase is a reflection of increased attendant care, and increased family involvement as the resident’s physical and mental status continued to decline.
DISCUSSION
These case studies demonstrate the potential that sensor technology has to augment traditional healthcare assessments and nurse care coordination. What is striking about the case by case analysis are the patterns displayed by the density maps depicting changes in movement in and out of the apartment for both the diagnoses of dementia and depression. Also the reduction of activity inside of the apartment at the time of an exacerbation of illness is evident for both mental health conditions. Another observation is the noticeable changes that occurred after medical intervention and treatment. As indicated by the density maps, residents’ movement increased after receiving assistance. It can be observed that there was more movement at home in some cases which is due in part to increased attendant care.
In the retrospective analysis, patterns of activity changes can be observed which coincide with exacerbations of mental illnesses (sometimes alongside co-morbid medical conditions) as verified by the health assessment data for these five cases. As best as can be determined from comparing existing records to the density maps, intuitively, the maps are depicting typical behavior that would be associated with recorded scores. In addition, the patterns of activity changes coincide with scores that indicate improvement in mental health functioning.
Table 1 is a descriptive time matrix depicting the changes in the health assessment data, changes in the density maps including average time away from home, and average density per day in home, along with noted interventions, and changes in the residents’ condition, across three points in time. This table captures the trends and similarities across cases. Our data indicate that measuring a baseline of activity while older adults are still active and healthy assists in the recognition of changes in patterns of activity for 4 cases. In one case, a new baseline was developed after treatment. In all 5 cases the density maps depicted both declines and improvements, and there was congruence with mental health assessment scores. The most striking features of the density maps are the capability to display and record changes in time away from home which can be an indication of changes in social and recreational behaviors; and the capability to display and record changes in activity inside the home which can be an indication of changes in the older adults’ behavior in relation to self care and household activities. Even with these overarching trends in the mapping, for every resident, the patterns are different which is to be expected since people have different routines, different types of movement, and different preferences for activity. Therefore each person has a different level of normal based on these individual characteristics.
Density map changes could be used in the future to provide an early warning to prompt health care providers to conduct mental health assessments and intervene to prevent or delay changes in mental health status. The density maps could also be used to monitor recovery after a hospitalization or significant health event. The density maps also can indicate the presence of a care provider if movements are spread apart or if the maps are displaying a higher density than what is normal. Our study also demonstrated that improvements in mental health conditions, as indicated by the health assessments are observed in the density maps in terms of changes in activity patterns. This method is meant to be an assistive tool for clinicians. It assumes that the clinician knows something about the resident, and what might be typical and atypical activity patterns.
There are limitations with this study. First, the sample size is small, and the results cannot be generalized to the larger public. Larger studies and additional case analyses may yield different results. Second, the analysis employed a retrospective analysis in which the health status of the residents is already known. Continued research in this area using prospective analysis will be a better measure of the usefulness of this technology in depicting early events. Thirdly, not all of the cases presented had health assessment information available for the baseline periods presented in the paper, although assessment information was provided during periods of activity pattern changes. Finally, the health assessments on all residents were completed by different health care providers, and sometimes across health care disciplines. This factor may have affected the way the health assessments were conducted. Even with these limitations, the preliminary results are promising.
CONCLUSION
New methods for monitoring the onset of dementia and depression are needed that are easy to use and unobtrusive. This study reports on a new innovative approach to early illness detection and management of these chronic mental health disorders using inexpensive sensors embedded in living environments. The first step in determining the usefulness of this approach is a retrospective approach. The next step will be to conduct a prospective study. As shown in the case studies, our vision is that this technology could eventually be used in community based settings, senior housing and private homes to enhance aging-in-place.
Examining patterns of activity level allows us to follow the onset and progression of dementia and depression since research indicates activity changes with advancement of these conditions 12, 18- 19. Furthermore, the severity of the symptoms of dementia and depression could be decreased and/or delayed, and ultimately assist older adults to successfully age-in-place and avoid premature institutionalization21- 24. Finding the means to enhance early detection leading to early intervention is essential to the promotion of independence and aging in place for older adults.
Acknowledgments
Research activities were supported by the National Institute for Nursing Research (NINR) of the National Institutes of Health (NIH) 1 R21 NR011197. Opinions are those of the authors and do not necessarily represent NINR.
Footnotes
The authors have no conflicts of interest relating to this article.
Contributor Information
Colleen Galambos, University of Missouri, School of Social Work.
Marjorie Skubic, Graduate Affiliate, University of Missouri, College of Engineering.
Shaung Wang, Graduate Affiliate, University of Missouri, College of Engineering.
Marilyn Rantz, University of Missouri, Sinclair School of Nursing.
References
- 1.National Institute of Mental Health. Older Adults: Depression and Suicide Facts. 2009 www.nimh.nih.gov/health/publications/older-adults-depression-and-suicide-facts-fact-sheet/index.shtml; retrieved April 3, 2009.
- 2.Onder G, Penninx BW, Ferrucci L, Fried LP, Guralnik JM, Pahor M. Measures of physical performance and risk for progressive and catastrophic disability: Results from the Women’s Health and Aging Study. Journals of Gerontology: Medical Science. 2005;60(1):74–79. doi: 10.1093/Gerona/60.1.74. [DOI] [PubMed] [Google Scholar]
- 3.Ridley S. The recognition and early management of critical illness. Annals of The Royal College of Surgeons of England. 2005;87(5):315–322. doi: 10.1308/003588405X60669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Alexander GL, Rantz M, Skubic M, Aud M, Wakefield E, Florea E, Paul A. Sensor systems for monitoring functional status in assisted living residents. Research in Gerontological Nursing. 2008;1(4):238–244. doi: 10.3928/19404921-20081001-01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Demiris G, Rantz MJ, Aud MA, Marek KD, Tyrer HW, Skubic M, Hassam AA. Older adults’ attitudes towards and perceptions of ‘smart home’ technologies: a pilot study. Informatics for Health and Social Care. 2004;29(2):87–94. doi: 10.1080/14639230410001684387. [DOI] [PubMed] [Google Scholar]
- 6.Shah M, Makinde KA, Thomas P. Cognitive and behavioral aspects affecting early referral of acute stroke patients to hospital. Journal of Stroke and Cerebrovascular Diseases. 2007;16(2):71–76. doi: 10.1016/j.jstrokecerebrovasdis.2006.11.004. [DOI] [PubMed] [Google Scholar]
- 7.Alwan M, Kell S, Dalal S, Turner B, Mack D, Felder R. In-home monitoring system and objective ADL assessment: Validation study. International Conference on Independence, Aging, and Disability; Washington, D.C. December, 2003.. [Google Scholar]
- 8.Alwan M, Leachtenauer J, Dalal S, Kell S, Turner B, Mack D, Felder R. Validation of rule-based inference of selected independent activities of daily living. Telemedicine and E-Health. 2005;11(5):594–599. doi: 10.1089/tmj.2005.11.594. [DOI] [PubMed] [Google Scholar]
- 9.Wang S, Skubic M. Density map visualization from motion sensors for monitoring activity level. Proceedings of the 4th IET International Conference on Intelligent Environments; Seattle, Washington. 2008. pp. 64–71. [Google Scholar]
- 10.Rantz MJ, Skubic M, Miller SJ. Using Sensor Technology to Augment Traditional Healthcare. Proceedings from 31st Annual International Conference of the IEEE EMBS; Minneapolis, MN. September 2–6, 2009; pp. 6159–62. [DOI] [PubMed] [Google Scholar]
- 11.Alexander G, Galambos C, Skubic M, Wang S. Density map visualization as a tool to monitor activity levels of older adults. Gerontechnology. 2010 Spring;9(2):186. doi: 10.4017/gt.2010.09.02.287.00. [DOI] [Google Scholar]
- 12.Binegar DL, Hynan LS, Lacritz LH, Weiner MF, Cullum CM. Can a direct IADL measure detect deficits in persons with MCI? Current Alzheimer’s Research. 2009;6(1):48–51. doi: 10.2174/156720509787313880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Callahan CM, Kroenke K, Counsell SR, Hendrie H, Perkins AJ, Katon W, Noel PH, Harpole L, Hunkeler EM, Unützer J. Treatment of depression improves physical functioning in older adults. Journal of the American Geriatrics Society. 2005;53(3):367–373. doi: 10.1111/j.1532-5415.2005.53151.x. [DOI] [PubMed] [Google Scholar]
- 14.Sheikh VI, Yesavage VA. Geriatric Depression Scale (GDS): Recent evidence and development of a shorter version. In: Brink TL, editor. Clinical gerontology: A guide to assessment and intervention. New York: Haworth Press; 1986. pp. 165–174. [Google Scholar]
- 15.Montoris I, Izal M. The Geriatric Depression Scale: A review of its development and utility. International Psychogeriatrics. 8(1):103–112. doi: 10.1017/s1041610296002505. [DOI] [PubMed] [Google Scholar]
- 16.Anthony JC, LeResche L, Niaz V, Vonkorff MR, Folstein MF. 1982 Limits of the mini-mental state as a screening test for dementia and delirium. Psychological Medicine. 1999;12:397–408. doi: 10.1017/s0033291700046730. [DOI] [PubMed] [Google Scholar]
- 17.Ware J, Kosinski M, Keller SD. A 12 item short form health survey: Construction of scales and preliminary tests of reliability and validity. Med Care. 1996;38(3):220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 18.Conwell Y, Brent D. Suicide and aging: Patterns of psychiatric diagnosis. International Psychogeriatrics. 1995;7(2):149–64. doi: 10.1017/S1041610295001943. [DOI] [PubMed] [Google Scholar]
- 19.Espiritu DA, Rashid H, Mast B, Fitzgerald J, Steinberg J, Lichtenberg PA. Depression, cognitive impairment and function in Alzheimer’s disease. International Journal of Geriatric Psychiatry. 2001;16(11):1098–1103. doi: 10.1002/gps.476. [DOI] [PubMed] [Google Scholar]
- 20.Wang S, Skubic M, Zhu Y, Galambos C. IEEE International Conference on Pervasive Computing and Communications; March, 2011; pp. 598–604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Waldemar G, Dubois B, Emre M, Georges J, McKeith IG, Rosser M, Scheltens P, Tariska P, Winblad BR. Recommendations for the diagnosis and management of Alzheimer’s disease and other disorders associated with dementia: EFNS guideline. European Journal of Neurology. 2007;14:1–26. doi: 10.1111/j.1468-1331.2006.01605.x. 101111/j 1468-1331.2006.01605.x. [DOI] [PubMed] [Google Scholar]
- 22.Neugroschl J, Sano M. Current treatment and recent clinical research in Alzheimer’s disease. Mount Sinai Journal of Medicine. 77(1):3–16. doi: 10.1002/msj.20165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Leifer BP. Early diagnosis of Alzheimer’s disease: Clinical and economic benefits. Journal of the American Geriatrics Society. 2003;51(5s2):s281–s288. doi: 10.1046/j1532-5415.5153.x. [DOI] [PubMed] [Google Scholar]
- 24.Leifer BP. Alzheimer’s disease: Seeing the signs early. Journal of the American Academy of Nurse Practitioners. 2009;21(11):588–595. doi: 10.1111/j.1745-7599.2009.00436.x. [DOI] [PubMed] [Google Scholar]
- 25.Rantz MJ, Skubic M, Koopman RJ, Alexander G, Phillips L, Musterman KI, Back JR, Aud MA, Galambos C, Guevara RD, Miller SJ. Automated technology to speed recognition of signs of illness in older adults. Journal of Gerontological Nursing. 2012 doi: 10.3928/00989134-20120307-01. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Miles MB, Huberman AM. Qualitative data analysis. 2. Thousand Oaks, CA: Sage; 1994. [Google Scholar]