Abstract
Background
This study examines the structure of the Personality Belief Questionnaire (PBQ), a self-report instrument designed to assess dysfunctional beliefs associated with personality pathology, as proposed by the cognitive theory of personality dysfunction.
Methods
The PBQ was examined using exploratory factor analysis with responses from 438 depressed outpatients, and confirmatory factor analysis with responses from 683 treatment-seeking psychiatric outpatients. All participants were assessed for personality disorder using a standard clinical interview. The validity of the resulting factor structure was assessed in the combined sample (N=1121) by examining PBQ scores for patients with and without personality disorder diagnoses.
Results
Exploratory and confirmatory analyses converged to indicate that the PBQ is best described by 7 empirically identified factors: 6 assess dysfunctional beliefs associated with forms of personality pathology recognized in DSM-IV. Validity analyses revealed that those diagnosed with a personality disorder evidenced a higher average score on all factors, relative to those without these disorders. Subsets of patients diagnosed with specific DSM-IV personality disorders scored higher, on average, on the factor associated with their respective diagnosis, relative to all other factors.
Conclusions
The pattern of results has implications for the conceptualization of personality pathology. To our knowledge, no formal diagnostic or assessment system has yet systematically incorporated the role of dysfunctional beliefs into its description of personality pathology. The identification of dysfunctional beliefs may not only aid in case conceptualization, but may provide unique targets for psychological treatment. Recommendations for future personality pathology assessment systems are provided.
The serious challenge of accurately defining and describing personality pathology is reflected in the numerous competing systems that have been proposed during the last several decades (Widiger & Simonsen, 2005). This fact is further reflected in the ongoing debate about how best to revise the official diagnostic system for personality disorders to be included in DSM-5 (e.g., Shedler et al., 2010; Bornstein, 2011; Clarkin & Huprich, 2011; Skodol et al., 2011). Although theorists place their emphasis differently, four psychological processes - cognition, emotion, motivation, and behavior - are commonly highlighted as the core domains that models of personality and personality pathology attempt to describe (Beck & Freeman, 1990; Mischel & Shoda, 1995; Westen, 1995; Millon & Davis, 1996; Livesley & Jang, 2000). Despite agreement that these four processes are integral to personality, no formal personality assessment system (past or present) has systematically incorporated all of these domains. In the following, we examine data from a measure of personality pathology that was designed specifically to capture information regarding the dysfunctional beliefs endorsed by individuals with personality dysfunction. Given that members of the DSM-5 work group have stated that “thoroughness in covering clinically relevant phenomena is among the most critical considerations for DSM-5 (Krueger et al., 2011, p. 174),” we offer these data to inform any future assessment or diagnostic scheme that attempts to capture the cognitive components of personality pathology.
Mischel and Shoda (1995) and Beck and Freeman (1990) independently developed theories of normal and abnormal personality, respectively, that fundamentally integrate the four core components of personality (cognition, emotion, motivation, and behavior) to explain the development, maintenance, and course of personality and personality pathology. Mischel and Shoda (1995) developed the cognitive-affective system theory of personality in order to reconcile the concept of personality, with its implication that behavior is stable over time, with empirical evidence showing that behavior is heavily influenced by situational factors. In this system, personality is a relatively stable structure of cognition, affect, and motivation that accounts for the selection, interpretation, and manifestation of behavioral and emotional responses to individually determined, salient features of the environment.
Beck and Freeman’s (1990) cognitive theory of personality disorders incorporates the same four psychological processes. It explains that genetic predispositions and environmental experiences combine to form schemas, cognitive structures that interpret information and assign meaning to events in the world. Personality pathology is explained by negative schemas that develop early in life and produce consistently biased judgments and cognitive errors (Beck, 1998). The combination of biased information processing and negative beliefs about the self, others, and interpersonal relationships generates affect, influences motivation, and eventually narrows the individual’s response tendencies to a small set of over-used emotional and behavioral dispositions that form the core clinical features of personality dysfunction (Beck & Freeman, 1990; Beck, 1998).
In recent years, criticisms of the current system for diagnosing personality disorder have been manifold (Widiger & Clark, 2000; First et al., 2002; Verheul & Widiger, 2004; Clark, 2005; Costa et al., 2005). Although a comprehensive review of this literature is beyond the scope of the current paper, one way to assess the quality with which the categories describe important features of personality dysfunction is to examine the extent to which the criteria sets adequately assess the four psychological processes described above. Others have observed that the criteria for some disorders assess single traits in a redundant fashion (Westen & Shedler, 2000), emphasize one psychological process over others across disorders (Millon & Davis, 1996), and identify pathology at different levels of description between disorders (Livesley & Jackson, 1992). For example, maladaptive beliefs are largely absent in the criteria sets for disorders such as Dependent, Histrionic, and Antisocial PDs. Criteria for these disorders focus instead on aspects of motivation, affect, and behavior. By contrast, dysfunctional beliefs form a high percentage of criteria for Paranoid PD, whereas behavior and motivation are each assessed by only one criterion, and no criteria assess affect. One possible explanation for this pattern is that some PDs might represent disorders of cognition, and others might represent disorders of motivation or behavior. However, there is no justification in the DSM system for emphasizing particular psychological processes over others for any of the disorders.
At the time of this writing, the revisions to the diagnostic system for personality disorder in the new edition of DSM have not been set firmly. A recent review explaining some of the proposed revisions (Skodol et al., 2011) states that the work-group is considering a revision to the descriptions of those personality disorder prototypes that will be retained in DSM-5 such that information will be added to describe the given pathology across a number of domains of functioning, including emotions, cognition, and behavior, among others. The work-group has not yet made clear whether the cognitive domain will consist of specific dysfunctional beliefs, or whether it will consist of more general qualities of thought content and process. In the following, we describe a measure that examines explicitly the dysfunctional beliefs that may be associated with personality pathology. We describe the psychometric properties of the measure, including its factor structure. Our aim is to facilitate, where relevant, the integration of specific dysfunctional beliefs in future systems intended to characterize personality pathology.
A Measure of Dysfunctional Beliefs in Personality Pathology
Using beliefs identified by Beck and Freeman (Beck & Freeman, 1990), Beck and Beck (Beck & Beck, 1991) developed the Personality Belief Questionnaire (PBQ) to assess the dysfunctional beliefs hypothesized to underlie the personality disorders that were officially recognized at the time. The measure has been shown to have adequate internal consistency and test-retest reliability in a large, outpatient psychiatric sample, and many of the subscales have differentiated patients diagnosed with different personality disorders (Beck et al., 2001). The measure likewise demonstrated good internal consistency in a non-clinical sample, but it failed to relate strongly to two well-validated measures of personality dysfunction (Trull et al., 1993). This result is not surprising given that the PBQ was developed to address the failure of other measures to consider systematically the dysfunctional beliefs that accompany personality disorders.
Using a sample that included and expanded on the sample used by Beck and colleagues (2001), Butler et al. (2007) condensed the PBQ item set into a short form, using item-total correlations as a guide (Butler et al., 2002, Butler personal communication 10/6/2010; Butler et al., 2007). Indexes of internal consistency and test-retest reliability were acceptable for many of the scales on the PBQ-short-form (Butler et al., 2007). However, Butler did not provide a structural analysis of the PBQ-short-form from these data. There are no published factor-analytic investigations of any version of the PBQ.
In the current study, we conducted an exploratory factor analysis of the reduced 65 PBQ-short-form item pool in a sample of depressed outpatients who participated in a clinical trial. We then attempted to cross-validate the structure identified in that sample using confirmatory factor analysis in a separate sample of adult psychiatric outpatients with a variety of Axis-I and Axis-II diagnoses. Finally, we examined the concurrent validity of the PBQ by comparing scores on the PBQ between subgroups formed on the basis of the personality disorders recognized in DSM-IV.
Method
Sample Characteristics
Exploratory Factor Analysis (EFA) Sample
The EFA sample consisted of 438 depressed outpatients participating in an ongoing, multi-site randomized treatment outcome study. All participants were diagnosed with either chronic or recurrent depression, and all scored 14 or higher on the modified 17-item version of the Hamilton Rating Scale for Depression (Hamilton, 1960). Exclusion criteria were: history of bipolar disorder, active substance abuse, psychosis, or the presence of another Axis-I disorder judged to be primary. Patients with medical conditions that prevented administration of study medications were also excluded as were patients requiring immediate hospitalization for suicidality.
The majority of patients, 88%, had at least some college education, and 49% had 16 or more years of education. The average age of participants was 43 years, 59% of the sample was female, 86% identified themselves as Caucasian, and 36% of patients were married or cohabiting with a significant other.
PD diagnoses were made at intake using the Structured Clinical Interview for DSM-IV Personality Disorders (First et al., 1997). Preliminary diagnoses were reviewed in diagnostic team meetings during which a final consensus diagnosis was made. Patients with Antisocial, Borderline, or Schizotypal Personality Disorders were excluded from participation in the parent study, and none of their data were available for the present report.
Approximately 42% of the sample was diagnosed with at least one personality disorder, and 12% of the sample was diagnosed with more than one. Cluster A disorders were diagnosed in 5% of the sample, 4% were diagnosed with Cluster B disorders, and 34% were diagnosed with Cluster C PDs.
Confirmatory Factor Analysis (CFA) Sample
The CFA sample was distinct from the EFA sample, and consisted of the subset (N=683) of the patients included in Beck et al (Beck et al., 2001) and Bulter et al (Butler et al., 2007) studies for whom the requisite data were available. Original sample characteristics and data collection procedures are described elsewhere (Beck et al., 2001; Butler et al., 2007). All participants were psychiatric outpatients seeking treatment. The mean age was 35 years (SD=11.5; range=16–18), and there were 351 women and 350 men. Demographic information was not available for two participants. The sample was collected between 1995 and 2001. Anyone entering prior to January 1995 was assessed using the Structured Clinical Interview for the DSM-III-R Personality Disorders (Spitzer et al., 1992). Those entering after this date were assessed using the Structured Clinical Interview for the DSM-IV Personality Disorders (First et al., 1997). 53% of patients had a primary Axis-I mood disorder, and 25% had a primary Axis-I anxiety disorder. 72% were diagnosed with at least one personality disorder, and 19% were diagnosed with more than one. Cluster A disorders were diagnosed in 5% of the sample, 19% were diagnosed with Cluster B disorders, and 49% were diagnosed with Cluster C disorders.
Measure
Participants completed the full version of PBQ, which contains 126 beliefs organized into nine scales: avoidant, dependent, obsessive-compulsive, histrionic, passive-aggressive, narcissistic, paranoid, schizoid, and antisocial personality pathologies. In the following, only data from the 65 items identified for inclusion in the short-form (Butler et al., 2007, Butler personal communication 10/6/2010) were included in the analyses. These items represent the 9 original PBQ scales (7 items each) as well as a 10th scale with items that represent beliefs identified by the short-form authors as corresponding to borderline personality pathology. Five of the items from the borderline scale appear as well on other scales; two are unique to the borderline scale. The instructions for the PBQ ask participants to read each statement and to judge the degree to which they believe the statement on a five-point Likert scale from 0 (“I don’t believe it at all”) to 4 (“I believe it totally”).
Procedures
After complete description of the studies from which these data originate, all subjects provided written informed consent. Participants in both samples completed the PBQ and the SCID-II self report questionnaires, after which the SCID-I and SCID-II clinical interviews were administered by masters- and doctoral-level diagnostic evaluators. Diagnostic evaluators were blind to the participants’ responses on the PBQ.
Statistical Analyses
For both exploratory and confirmatory factor analytic models, scores on the PBQ items were treated as representing ordinal categories, and polychoric correlations (Holgado-Tello et al., 2010) were used to estimate the models. EFA and CFA models were estimated using the robust weighted-least squares estimator (estimator=WLSMV), implemented in MPLUS version 5 software (Muthen & Muthen, 2009).
Exploratory factor analysis was conducted using an oblique geomin rotation (Yates, 1987). Factor loadings >0.40 were considered to be salient. The number of factors to be extracted was based on both empirical (the scree test) and theoretical (the proposed structure of the PBQ short-form) considerations. Each model was evaluated to determine if it (a) retained at least three salient item loadings on each factor; (b) produced adequate internal consistency (alpha>.70) for unit-weighted salient items; (c) maximized parsimonious coverage and simple structure (i.e., achieved maximum assignment of items to factors while minimizing the number of items that loaded on multiple factors); and (d) was interpretable.
Confirmatory factor models were assessed using the independent CFA sample. Model fit was assessed with the comparative fit index (CFI, Bentler, 1990), the Tucker-Lewis index (TLI, Tucker & Lewis, 1973) and the root mean square error of approximation (RMSEA, Steiger & Lind, 1980). There is considerable controversy surrounding the criteria for establishing adequate fit in confirmatory factor models (Hu & Bentler, 1999; Marsh et al., 2004). Values greater than .90 or .95 for the CFI and TLI commonly reflect adequate fit; RMSEA values <.05 were taken to represent close fit and values <.08 to reflect reasonable fit (Marsh et al., 2004).
As an additional test of the measure’s psychometric properties, item invariance was evaluated for three variables (gender, age, and diagnosis of major depressive disorder) with a MIMIC (Multiple Indicators, Multiple Causes) model (Muthen & Muthen, 2009). This model examines the relationship between the covariates and individual items and tests whether the items function differently for different subgroups of patients.
The criterion validity of the PBQ factors was examined in the combined sample (N=1121) by comparing the distributions of the unit-weighted factor scores (prorated to account for missing data) obtained from groups formed on the basis of personality disorder status. A multivariate analysis of variance (MANOVA) was conducted in which scores on each of the factors served as the dependent variables and presence/absence of a personality disorder was the independent variable. In addition, sufficient sample sizes were available to examine withingroup differences for patients with each of five personality disorder diagnoses: Avoidant (N=244), Obsessive Compulsive (N=207), Dependent (N=72), Narcissistic (N=34), and Paranoid (N=48). Separate repeated measures ANOVAs were conducted for each disorder subgroup to examine whether there were differences in the mean scores among the factors within each group.
Results
Factor Structure
The scree test suggested a 7-factor solution, whereas the short-form of the PBQ was intended to contain 10 subscales. Consequently, oblique solutions ranging from 7 to 10 factors were initially examined. The model retaining 7 oblique factors met all pre-specified criteria. For the other models, at least one factor failed to meet the established criteria. For example, the 8-factor solution contained no items that loaded >40 on the 8th factor, and the first 7 factors were quite similar to those extracted in the 7-factor solution.
The final exploratory model retained 59 of the 65 items designated for the short form, with 2 items loading on more than one factor. When these items were removed, the factor structure for the remaining items remained unchanged. Table 1 displays the 57 items composing the 7 factors, as well as the scales from which they originated, the exploratory and confirmatory factor loadings, and the factor reliability.
Table 1.
Exploratory and Confirmatory Factor Structure for the Personality Belief Questionnaire Short Form.
| Original Sub-scalea |
Personality Belief | EFAb | CFAc |
|---|---|---|---|
| Dependent & Avoidant (alpha = 0.91) | |||
| Dependentd | I am helpless when I'm left on my own. | 0.77 | 0.81 |
| Dependentd | I am needy and weak. | 0.74 | 0.78 |
| Dependentd | I need somebody around available at all times to help me to carry out what I need to do or in case something bad happens. | 0.72 | 0.80 |
| Borderline | I can't cope as other people can. | 0.72 | 0.74 |
| Dependent | I need others to help me make decisions or tell me what to do. | 0.71 | 0.77 |
| Dependent | I am basically alone -- unless I can attach myself to a stronger person. | 0.67 | 0.76 |
| Dependent | The worst possible thing would be to be abandoned. | 0.66 | 0.72 |
| Avoidant | I should avoid situations in which I attract attention, or be as inconspicuous as possible. | 0.52 | 0.55 |
| Dependent | I must maintain access to him or her [significant other] at all times. | 0.50 | 0.73 |
| Avoidant | I should avoid unpleasant situations at all cost. | 0.49 | 0.71 |
| Avoidantd | Unpleasant feelings will escalate and get out of control. | 0.49 | 0.75 |
| Avoidant | I cannot tolerate unpleasant feelings. | 0.48 | 0.68 |
| Avoidant | If people get close to me, they will discover the “real” me and reject me. | 0.41 | 0.70 |
| Obsessive-Compulsive (alpha = 0.90) | |||
| Obs. Comp | It is necessary to stick to the highest standards at all times, or things will fall apart. | 0.91 | 0.83 |
| Obs. Comp | If I don't perform at the highest level, I will fail. | 0.77 | 0.87 |
| Obs. Comp | It is important to do a perfect job on everything. | 0.75 | 0.74 |
| Obs. Comp | Any flaw or defect of performance may lead to a catastrophe. | 0.75 | 0.90 |
| Obs. Comp | Flaws, defects, or mistakes are intolerable. | 0.73 | 0.90 |
| Obs. Comp | If I don't have systems, everything will fall apart. | 0.69 | 0.74 |
| Obs. Comp | Details are extremely important. | 0.63 | 0.62 |
| Narcissistic (alpha = 0.88) | |||
| Narcissistic | Since I am so superior, I am entitled to special treatment and privileges. | 0.76 | 0.76 |
| Antisocial | I should do whatever I can get away with. | 0.69 | 0.77 |
| Antisocial | If I don't push around other people, I will get pushed around. | 0.68 | 0.76 |
| Narcissistic | Other people should satisfy my needs. | 0.67 | 0.70 |
| Narcissistic | I don't have to be bound by the rules that apply to other people. | 0.65 | 0.75 |
| Narcissistic | Since I am so talented, people should go out of their way to promote my career. | 0.61 | 0.72 |
| Antisocial | If I want something, I should do whatever is necessary to get it. | 0.57 | 0.54 |
| Narcissistic | Only people as brilliant as I am understand me. | 0.57 | 0.68 |
| Narcissistic | Other people should recognize how special I am. | 0.56 | 0.71 |
| Antisocial | I have been unfairly treated and am entitled to get my fair share by whatever means I can. | 0.55 | 0.77 |
| Antisocial | Force or cunning is the best way to get things done. | 0.45 | 0.74 |
| Autonomous (alpha = 0.85) | |||
| Pass. Agg. | If I follow the rules the way people expect, it will inhibit my freedom of action. | 0.76 | 0.81 |
| Pass. Agg. | Rules are arbitrary and stifle me. | 0.70 | 0.76 |
| Pass. Agg. | Making deadlines, complying with demands, and conforming are direct blows to my pride and self- sufficiency. | 0.61 | 0.81 |
| Pass. Agg. | Authority figures tend to be intrusive, demanding, interfering, and controlling. | 0.52 | 0.73 |
| Pass. Agg. | If I regard people as too bossy, I have a right to disregard their demands. | 0.49 | 0.67 |
| Pass. Agg. | I have to resist the domination of authorities but at the same time maintain their approval and acceptance. | 0.44 | 0.79 |
| Paranoid (alpha = 0.94) | |||
| Paranoid | Others will try to use me or manipulate me if I don't watch out. | 0.98 | 0.89 |
| Paranoid | People will take advantage of me if I give them the chance. | 0.90 | 0.84 |
| Paranoid | If people act friendly, they may be trying to use or exploit me. | 0.86 | 0.85 |
| Paranoid | Other people have hidden motives. | 0.85 | 0.82 |
| Paranoidd | I have to be on guard at all times. | 0.81 | 0.90 |
| Borderline | I cannot trust other people. | 0.78 | 0.76 |
| Paranoid | Other people will deliberately try to demean me. | 0.67 | 0.82 |
| Paranoid | If other people find out things about me, they will use them against me. | 0.64 | 0.79 |
| Histrionic (alpha = 0.86) | |||
| Histrionic | If I don't keep others engaged with me, they won't like me. | 0.85 | 0.90 |
| Histrionic | Unless I entertain or impress people, I am nothing. | 0.84 | 0.90 |
| Histrionic | The way to get what I want is to dazzle or amuse people. | 0.74 | 0.85 |
| Histrionic | In order to be happy I need other people to pay attention to me. | 0.62 | 0.74 |
| Histrionic | If I entertain people, they will not notice my weaknesses. | 0.58 | 0.76 |
| Histrionic | It is awful if people ignore me. | 0.49 | 0.76 |
| Schizoid (alpha = 0.85) | |||
| Schizoid | I enjoy doing things more by myself than with other people. | 0.84 | 0.68 |
| Schizoid | In many situations, I am better off to be left alone. | 0.82 | 0.81 |
| Schizoid | It's better to be alone than to feel “stuck” with other people. | 0.62 | 0.64 |
| Schizoid | My privacy is much more important to me than closeness to people. | 0.59 | 0.65 |
| Schizoid | It is important for me to be free and independent of others. | 0.53 | 0.64 |
| Schizoid | Relationships are messy and interfere with freedom. | 0.43 | 0.84 |
Note. EFA = Exploratory Factor Analysis, CFA = Confirmatory Factor Analysis.
Entries refer to the original scales on the PBQ-short-form from which the beliefs originated. Some scales have been abbreviated (Pass. Agg. = Passive Aggressive; Obs. Comp. = Obsessive Compulsive).
Entries are factor loadings from the exploratory factor analysis using an oblique geomin rotation.
Entries are standardized loadings from the confirmatory factor analyses.
The belief also appeared on the original borderline subscale of the PBQ-short-form.
The first factor (Dependent & Avoidant) was composed of beliefs from the original dependent, avoidant, and borderline scales. These included beliefs about the need for others, the danger of situations and feelings, and the affinity for avoidance as a coping strategy. The second factor (Obsessive-Compulsive) was composed of beliefs regarding perfectionism, and the importance of systems and details. The third factor (Narcissistic) had a mixture of salient loadings from items written for the antisocial and narcissistic scales. Salient items reflected grandiosity, entitlement, and the need to be recognized.
The fourth factor was composed of items from the original passive-aggressive scale, but the items do not appear to describe passive-aggressive personality disorder as defined in DSM-IV. Instead, they reflect the importance of self-reliance and the untoward consequences of being dominated by others. Salient items included, “If I follow the rules the way people expect, it will inhibit my freedom” and “Authority figures tend to be intrusive, demanding, interfering, and controlling.” These beliefs appear to be more consistent with the cognitive-personality construct identified by Beck (Beck, 1983) as Autonomy and the personality configuration labeled Introjective by Blatt and colleagues (Blatt et al., 2001). These concepts refer to a pattern of concern for: (1) individualistic achievement, (2) freedom from the control of others, and (3) focus on the self and maintaining a strong self-concept. The fourth factor was labeled Autonomy to reflect this concept.
The fifth factor (Paranoid) contained salient loadings from all 7 of the original paranoid beliefs and an additional belief from the Borderline scale, “I cannot trust other people.” The sixth factor (Histrionic) contained salient items that appear to address the importance of entertaining others and the negative consequences of failing to do so. Finally, the seventh factor (Schizoid) retained beliefs concerning privacy, independence, and the lack of concern about judgments by others.
Confirmatory Factor Analysis
Standardized loadings from the confirmatory factor analysis are displayed in Table 1. All items loaded >.50 on their respective factors. Fit indices for the model revealed a TLI=.97, reflecting good fit, an RMSEA=.076, reflecting reasonable fit, and a CFI=.88, which falls just short of “acceptable fit” using standard definitions.
As an additional test of the robustness of the instrument, measurement invariance was assessed for each item on three variables: age, gender, and diagnosis of major depressive disorder. Only one of the fifty-seven items displayed differential item functioning, and it did so for only one of the covariates. Namely, for a given score on the Dependent & Avoidant factor, patients with MDD scored lower on the following item than did non-depressed patients “I must maintain access to [significant other] at all times.”1 Thus, 56 of the 57 items did not function differently across subgroups of patients.
Validity
MANOVA analysis of the combined sample (N=1121) revealed a significant difference between patients with vs. without a personality disorder on the mean scores of the 7 factors, Wilks’-Lambda=0.89, Multivariate F(7,1111)=20.51, p<0.001. Post-hoc Individual t-tests revealed significant differences (at p<0.001) for each of the 7 factors between patients with and without personality disorders. Table 2 displays unit-weighted factor scores (converted to T-scores; Grand Mean=50, SD=10) on each of the 7 factors for patients with and without personality disorders.
Table 2.
Unit-Weighted Scores on Each of the 7 Factors for Patients With and Without Personality Disorders
| Factor Scoresa | ||||
|---|---|---|---|---|
| PBQ Factor | PD (676) | Non-PD (445) | t | d-typec |
| Dependent & Avoidant | 52 | 46 | 10.42 | 0.64 |
| Obsessive Compulsive | 52 | 47 | 7.43 | 0.46 |
| Narcissistic | 51 | 48 | 6.30 | 0.38 |
| Autonomous | 52 | 47 | 8.39 | 0.51 |
| Paranoid | 52 | 47 | 8.87 | 0.54 |
| Histrionic | 52 | 47 | 8.80 | 0.54 |
| Schizoid | 51 | 48 | 6.18 | 0.38 |
| Total scoreb | 53 | 46 | 12.04 | 0.71 |
Note. PD = participants diagnosed with a personality disorder; Non-PD = participants without a personality disorder diagnosis. All entries represent T-scores (M=50, SD=10). All comparisons are significant at p < 0.001.
Entries are least squares means estimates of the factor scores.
Values represent means for the total PBQ-short-form score for all of the items retained by the factor analysis. The variances of the two groups for this comparison were not equal (F (675 444)=1.40, p<0.001), so the Satterthwaite method was used in calculating the t-test.
Values represent the d-type effect size difference between patients with and without personality disorders for each factor. Pooled standard deviations were used to calculate effect sizes.
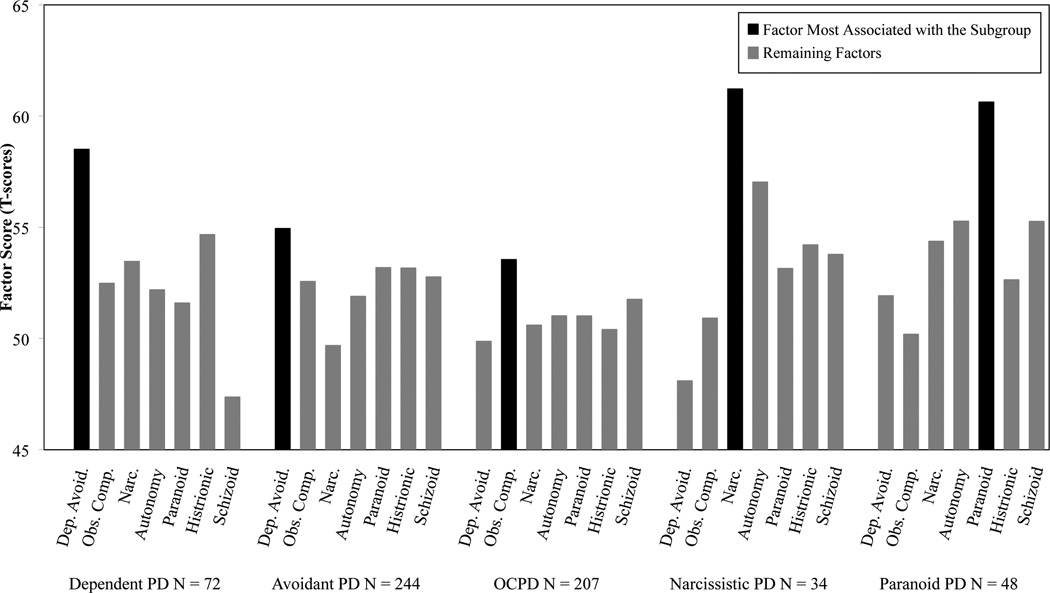
Within-group differences among the PBQ factor scores were examined for patients with each of five personality disorder diagnoses: Avoidant, Obsessive-Compulsive, Dependent, Narcissistic, and Paranoid. Separate repeated measures ANOVAs were conducted for each disorder subgroup, and the omnibus tests of within-group differences among the factor scores were significant for each, (all Fs>5.0, all ps<0.001). The Figure displays raw means for each factor within each diagnostic subgroup. The figure also depicts that within each diagnostic category, patients scored significantly higher on the factor corresponding to that disorder than they did on any of the remaining factors.
Figure.
Within-Group Comparison of Factor Scores within 5 Personality Disorder Diagnoses
Subgroups were formed on the basis of 5 personality disorder diagnoses: Dependent, Avoidant, Obsessive-Compulsive, Narcissistic, and Paranoid. The height of each bar represents the raw mean score for that factor within the given subgroup. Within each subgroup, the black bar represents the factor most closely associated with that type of personality pathology. The gray bars represent the remaining factors. Separate repeated measures ANOVAs were conducted for each disorder subgroup, and the omnibus tests of within-group differences among the factor scores were significant for each, (all ps<0.001). d-type effect sizes were calculated from the raw means and standard deviations by comparing the value of the black bar (the index factor for a given group) to the value of each gray bar within each subgroup. Statistical significance for each comparison was determined by the repeated measures ANOVA models. For each subgroup, scores on the index factor for that group were significantly higher than scores on the remaining factors. The specific comparisons are as follows:
Dependent subgroup: Avoidant & Dependent > Obs. Comp. d=0.61***, Narc. d=0.43***, Autonomy d=0.59***, Paranoid d=0.66***, Histrionic d=0.37**, Schizoid d=1.21***
Avoidant subgroup: Avoidant & Dependent > Obs. Comp. d=0.24**, Narc. d=0.55***, Autonomy d=0.31***, Paranoid d=0.17*, Histrionic d=0.17*, Schizoid d=0.22**
Obsessive Compulsive subgroup: Obsessive-Compulsive > Dep. Avoid. d=0.37***, Narc. d=0.29***, Autonomy d=0.25***, Paranoid d=0.26***, Histrionic d=0.32***, Schizoid d=0.17*
Narcissistic subgroup: Narcissistic > Dep. Avoid. d=1.13***, Obs. Comp. d=0.85***, Autonomy d=0.33*, Paranoid d=0.67***, Histrionic d=0.57**, Schizoid d=0.64***
Paranoid subgroup: Paranoid > Dep. Avoid. d=0.82***, Obs. Comp. d=0.95***, Narc. d=0.54***, Autonomy d=0.5**, Histrionic d=0.7***, Schizoid d=0.5**
PD = Personality Disorder; OCPD = Obsessive Compulsive Personality Disorder; Dep. Avoid. = Dependent & Avoidant; Obs. Comp = Obsessive Compulsive; Narc. = Narcissistic. * p < .05, ** p< .01, *** p < .001.
Discussion
Evidence from this study suggests that the content of the PBQ can be captured by 7 empirically identified factors. The results of confirmatory and item-invariance analyses suggest that the structures uncovered in this study are robust and replicable. These results provide support for the cognitive theory of personality disorder, which posits that dysfunctional beliefs about the self, others, and the world represent an important feature of pathological personality functioning. Beliefs relevant to eight of the disorders recognized in DSM-IV were identified in this work, however, the structure of those beliefs did not map perfectly onto the categories represented in DSM-IV. Beliefs for avoidant and dependent personality disorders, for example, loaded on a single factor, as did beliefs for narcissistic and antisocial personality disorders. These findings suggest some degree of overlap within each of these sets of disorders. An additional factor, not well represented in any past or proposed DSM scheme, emerged that is closely related to the personality feature labeled Autonomy by Beck and colleagues (Beck, 1983). Finally, no factors representing borderline or schizotypal personality disorders were obtained. Although the short-form of the PBQ used in this study did contain a subscale for beliefs associated with borderline pathology, the majority of those beliefs also appeared on other subscales. The borderline subscale was not recovered by the EFA analysis. When Beck and colleagues originally drafted the lists of dysfunctional beliefs (Beck & Freeman, 1990), they argued that patients with borderline personality disorder endorse several beliefs from many of the other categories and that individuals with schizotypal personality disorder suffer from dysfunction in the process of thinking as opposed to pathology in thought content.
Although the future of personality disorder diagnoses in DSM-5 is unclear at the present time, the results of the current study suggest that it may be important in any future diagnostic system to describe systematically the dysfunctional beliefs endorsed by individuals with personality pathology. Specifically, the pattern of results obtained herein demonstrates that beliefs related to avoidant, dependent, narcissistic, antisocial, paranoid, histrionic, obsessive-compulsive and schizoid personality pathology are captured well by coherent sets of dysfunctional beliefs that can be identified and confirmed in independent clinical samples. Validity analyses revealed that individuals with diagnosed personality disorders scored higher on each of the 7 PBQ factors than did individuals without personality disorders. Sample sizes were adequate for five of these diagnostic categories (Dependent, Avoidant, Obsessive-Compulsive, Narcissistic, and Paranoid) to investigate the relationship between categorical diagnosis and dysfunctional beliefs. In each case, patients with a given disorder scored significantly higher on the factor representing the beliefs for that disorder than they scored on any other factor. These findings provide support for the concurrent validity for these prototypes of pathology. This kind of validity was one of three identified by Kendler and colleagues (2009) as important for the DSM-5 work groups to consider when making determinations about which disorders should be included and which should be deleted from the next revision. Despite the strong support for the concurrent validity of the five disorders examined more closely in this report, patients with these disorders displayed a range of dysfunctional beliefs from across the other factors. These results further highlight the importance of retaining in future diagnostic systems the ability to assess aspects of cognition, motivation, behavior and affect from across a wide variety of personality disorder prototypes.
Indeed, the factors identified in the current work describe clinically meaningful sets of beliefs that have the potential to translate directly into unique targets for psychological treatment. The identification of dysfunctional beliefs is a core element of cognitive-based treatments for personality pathology. In Beck and Freeman’s original description of cognitive therapy for personality disorders (Beck & Freeman, 1990), they note that simple endorsement of a belief does not necessarily constitute personality pathology. Rather, it is the intensity with which a dysfunctional belief is held that contributes to pathology. Thus, the identification of dysfunctional beliefs may be more difficult for individuals with personality dysfunction than for individuals with acute Axis-I disorders. Beliefs endorsed by a patient with personality pathology may be more longstanding, more firmly held, and more integral to the way in which the patient sees the world. As such, these beliefs may seem natural to the patient. Assessment systems that can help practitioners and patients to identify these cognitions could be expected to have enormous clinical utility. Once identified, the treatment provider could work with the patient to gradually challenge the long-standing dysfunctional sets of core cognitions and to build, over time, more accurate and adaptive constellations of beliefs about him/herself, others, and the world (Beck & Freeman, 1990).
Limitations
Given that the PBQ was designed for clinical populations, one strength of the present study is the use of two independent clinical samples in which sizeable percentages of individuals were diagnosed with a personality disorder. Still, the samples had properties that may limit some of the conclusions that can be drawn. Individuals with diagnosed Borderline, Schizotypal, and Antisocial personality disorders were not included in the EFA sample due to the nature of the study from which the data originated. In addition, the EFA sample consisted entirely of depressed individuals, which may have lowered the percentages of individuals with features of particular personality disorders, such as narcissistic, antisocial, and schizoid (Doyle et al., 1999). The EFA sample was predominantly Caucasian and relatively highly educated, which may also limit the generalizability of the results. Participants in the Beck (Beck et al., 2001) and Butler (Butler et al., 2007) samples who were used in previous work to identify items to be retained in the short form of the PBQ were also used in the current study to form the CFA sample. An independent sample would have allowed for firmer conclusions from the CFA, however, the fact that the current analysis tested a different structure than that originally proposed for the PBQ-short-form should tend to mitigate any bias that the use of this sample may have caused.
Although two of the CFA fit indices were within the range of acceptable model fit, one fell just short. Poor CFA model fit in personality research is common. A recent examination of CFA research in personality measurement found that the closest fitting model among seven popular personality trait measures was represented by TLI=.70, CFI=.79, RMSEA=.09 (Hopwood & Donnellan, 2010). The authors concluded that “any omnibus personality inventory that shows adequate fit in CFA models by the criteria we selected … [CFA>.90, TLI>.90, RMSEA<.10] would mark quite an achievement ( p.342).” The results of the current paper came close to satisfying that goal.
In addition to the specific limitations of the current study, a number of limitations of the PBQ itself are suggested by a consideration of its properties. First, the full PBQ measure is structured such that the items on each of the scales are presented together. The fact that only a subset of items (those identified for the short-form version) were selected for the current analysis should mitigate this concern. Second, all items are keyed in the same direction, exposing the questionnaire to the possible presence of positive or negative response sets. Future revisions of the scale should address this concern.
Conclusions
Despite the fact that several personality theorists emphasize the importance of cognition, motivation, behavior and affect in the conceptualization of personality dysfunction, official descriptions of personality disorder have not yet systematically incorporated these features. Recent indications regarding the forthcoming revisions to DSM are promising in that they may contain descriptions of dysfunction in each of these domains for the disorders that will be retained. It is not clear, however, whether these descriptions will include specific dysfunctional beliefs, and whether dysfunctional cognition will also be systematically incorporated into the individual trait descriptions. In the present work, we report the underlying structure of a measure of the cognitive components of personality pathology and demonstrate its validity in discriminating among patients diagnosed with the personality disorders that have been recognized to this point. Revisions to the diagnostic and classification system for personality disorder should endeavor to assess adequately the four psychological processes involved in personality dysfunction. Indeed, the results of this study indicate that there are at least seven coherent patterns of dysfunctional cognition that describe meaningful constellations of personality pathology. Future work should examine the incremental validity achieved by measuring these beliefs as well as the clinical utility of targeting these beliefs directly during treatment.
Acknowledgments
We would like to acknowledge the other members of the research team responsible for the study from which some of these data originate: Steven D. Hollon, Jay D. Amsterdam and Richard C. Shelton. We would also like to thank Stephanie Stepp for providing methodological advice; Brent Freeman for his efforts in managing the data, and we wish to thank Dianne L. Chambless, Ayelet M. Ruscio, Andrew C. Butler, Robert A. Steer, and Sunil S. Bhar for their comments on a previous draft of this manuscript.
This research was supported by grant MH060998 (DeRubeis) from the National Institute of Mental Health, Bethesda, MD.
Footnotes
The MIMIC model used to assess item invariance also simultaneously assesses the degree to which the mean score on a factor differs as a function of the covariates. We have no expectation that mean factor scores will be identical for different subgroups, and we have no hypotheses regarding the direction of any differences. The following is a summary of the results at p < .05: All factor scores except the Narcissistic factor were higher for patients diagnosed with MDD compared to non-depressed patients. Scores on all factors except for Autonomy decrease with increasing Age. Men have higher scores on the Narcissistic and Autonomy factors and lower scores on the Dependent & Avoidant factor compared to women.
Disclosures Drs. Fournier and DeRubeis have no conflicts of interest to disclose. Dr. Beck is the author of the Personality Belief Questionnaire (in the public domain) and six questionnaires (none regarding personality disorders) published by The Psychological Corporation. He is also the president of the Beck Institute for Cognitive Therapy, a nonprofit institution providing psychotherapy and training that receives income through patient fees and trainee payments; he receives no income from this organization.
Contributor Information
Jay C. Fournier, Department of Psychiatry, University of Pittsburgh School of Medicine, Pittsburgh, PA
Robert J. DeRubeis, Department of Psychology, University of Pennsylvania, Philadelphia, PA
Aaron T. Beck, Department of Psychiatry, Perelman School of Medicine at the University of Pennsylvania, Philadelphia, PA
References
- Beck AT. Cognitive Therapy of Depression: New Perspectives. In: Clayton PJ, Barrett JE, editors. Treatment of Depression: Old Controversies and New Approaches. New York: Raven Press; 1983. [Google Scholar]
- Beck AT, Beck JS. The Personality Belief Questionnaire. Bala Cynwyd, PA: The Beck Institute for Cognitive Therapy and Research; 1991. [Google Scholar]
- Beck AT, Butler AC, Brown GK, Dahlsgaard KK, Newman CF, Beck JS. Dysfunctional beliefs discriminate personality disorders. Behaviour Research and Therapy. 2001;39(10):1213–1225. doi: 10.1016/s0005-7967(00)00099-1. [DOI] [PubMed] [Google Scholar]
- Beck AT, Freeman A. Cognitive Therapy of Personality Disorders. New York: The Guilford Press; 1990. [Google Scholar]
- Beck JS. Complex cognitive therapy treatment for personality disorder patients. Bulletin of the Menninger Clinic. 1998;62(2):170–194. [PubMed] [Google Scholar]
- Bentler PM. Comparative fit indexes in structural models. Psychological Bulletin. 1990;107(2):238–246. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Blatt SJ, Shahar G, Zuroff DC. Anaclitic (sociotropic) and introjective (autonomous) dimensions. Psychotherapy: Theory, Research, Practice, Training. 2001;38:449–454. [Google Scholar]
- Bornstein RF. Reconceptualizing Personality Pathology in DSM-5: Limitations in Evidence for Eliminating Dependent Personality Disorder and Other DSM-IV Syndromes. Journal of Personality Disorders. 2011;25(2):235–247. doi: 10.1521/pedi.2011.25.2.235. [DOI] [PubMed] [Google Scholar]
- Butler AC, Beck AT, Cohen LH. The Personality Belief Questionnaire-Short Form: Development and preliminary findings. Cognitive Therapy & Research. 2007;31:357–370. [Google Scholar]
- Butler AC, Brown GK, Beck AT, Grisham JR. Assessment of dysfunctional beliefs in borderline personality disorder. Behaviour Research and Therapy. 2002;40:1231–1240. doi: 10.1016/s0005-7967(02)00031-1. [DOI] [PubMed] [Google Scholar]
- Clark LA. Temperament as a unifying basis for personality and psychopathology. Journal of Abnormal Psychology. Special Issue: Toward a Dimensionally Based Taxonomy of Psychopathology. 2005;114(4):505–521. doi: 10.1037/0021-843X.114.4.505. [DOI] [PubMed] [Google Scholar]
- Clarkin JF, Huprich SK. Do DSM-5 Personality Disorder Proposals Meet Criteria for Clinical Utility? Journal of Personality Disorders. 2011;25(2):192–205. doi: 10.1521/pedi.2011.25.2.192. [DOI] [PubMed] [Google Scholar]
- Costa PT, Patriciu NS, McCrae RR. Lessons from longitudinal studies for new approaches to the DSM-V: The FFM and FFT. Journal of Personality Disorders. Special Issue: Longitudinal studies. 2005;19(5):533–539. doi: 10.1521/pedi.2005.19.5.533. [DOI] [PubMed] [Google Scholar]
- Doyle TJ, Tsuang MT, Lyons MJ. Comorbidity of depressive illnesses and personality disorders. In: Tohen M, editor. Comorbidity in Affective Disorders. New York: Marcel Dekker, Inc; 1999. pp. 105–156. [Google Scholar]
- First M, Gibbon M, Spitzer R, Williams J, Benjamin L. Structured Clinical Interview for DSM-IV Axis II Personality Disorders, (SCID-II) Washington, D.C: American Psychiatric Press, Inc; 1997. [Google Scholar]
- First MB, Bell CC, Cuthbert BN, Krystal JH, Malison R, Offord DR, Reiss D, Shea T, Widiger TA, Wisner KL. Personality disorders and relational disorders: A research agenda for addressing crucial gaps in DSM. In: Kupfer DJ, editor. A research agenda for DSM-V. Washington, DC: American Psychiatric Association Press; 2002. pp. 123–200. [Google Scholar]
- Hamilton MA. A rating scale for depression. Journal of Neurology, Neurosurgery, and Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holgado-Tello FP, Chacón-Moscoso S, Barbero-García I, Vila-Abad E. Polychoric versus Pearson correlations in exploratory and confirmatory factor analysis of ordinal variables. Qual Quant. 2010;44:153–166. [Google Scholar]
- Hopwood CJ, Donnellan MB. How should the internal structure of personality inventories be evaluated? Pers Soc Psychol Rev. 2010;14:332–346. doi: 10.1177/1088868310361240. [DOI] [PubMed] [Google Scholar]
- Hu L-t, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6(1):1–55. [Google Scholar]
- Kendler K, Kupfer D, Narrow W, Phillips K, Fawcett J. Guidelines for making changes to DSM-V. 2009 Revised 10/21/09. Unpublished manuscript available at www.dsm5.org.
- Krueger RF, Eaton NR, Clark LA, Watson D, Markon KE, Derringer J, Skodol A, Livesley WJ. Deriving an Empirical Structure of Personality Pathology for DSM-5. Journal of Personality Disorders. 2011;25(2):170–191. doi: 10.1521/pedi.2011.25.2.170. [DOI] [PubMed] [Google Scholar]
- Livesley WJ, Jackson DN. Guidelines for developing, evaluating, and revising the classification of personality disorders. Journal of Nervous and Mental Disease. 1992;180(10):609–618. doi: 10.1097/00005053-199210000-00001. [DOI] [PubMed] [Google Scholar]
- Livesley WJ, Jang KL. Toward an empirically based classification of personality disorder. Journal of Personality Disorders. 2000;14(2):137–151. doi: 10.1521/pedi.2000.14.2.137. [DOI] [PubMed] [Google Scholar]
- Marsh HW, Hau K-T, Wen Z. In search of golden rules: Comment on hypothesis-testing approaches to setting cutoff values for fit indexes and dangers in overgeneralizing Hu and Bentler's (1999) findings. Structural Equation Modeling. 2004;11(3):320–341. [Google Scholar]
- Millon T, Davis RO. Disorders of personality: DSM-IV and beyond. New York: John Wiley & Sons, Inc; 1996. [Google Scholar]
- Mischel W, Shoda Y. A cognitive-affective system theory of personality: reconceptualizing situations, dispositions, dynamics, and invariance in personality structure. Psychological Review. 1995;102(2):246–268. doi: 10.1037/0033-295x.102.2.246. [DOI] [PubMed] [Google Scholar]
- Muthen LK, Muthen BO. Mplus: Statistical Analysis with Latent Variables User's Guide. Los Angeles: Muthen & Muthen; 2009. [Google Scholar]
- Shedler J, Beck A, Fonagy P, Gabbard GO, Gunderson J, Kernberg O, Michels R, Westen D. Personality disorders in DSM-5. Am J Psychiatry. 2010;167(9):1026–1028. doi: 10.1176/appi.ajp.2010.10050746. [DOI] [PubMed] [Google Scholar]
- Skodol AE, Bender DS, Morey LC, Clark LA, Oldham JM, Alarcon RD, Krueger RF, Verheul R, Bell CC, Siever LJ. Personality Disorder Types Proposed for DSM-5. Journal of Personality Disorders. 2011;25(2):136–169. doi: 10.1521/pedi.2011.25.2.136. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Williams JBW, Gibbon M, First MB. The Structured Clinical Interview for DSM-III-R (SCID), I: History, rationale and description. Archives of General Psychiatry. 1992;49:624–629. doi: 10.1001/archpsyc.1992.01820080032005. [DOI] [PubMed] [Google Scholar]
- Steiger JH, Lind JM. Statistically based tests for the number of common factors; Paper Presented at the Annual Meeting of the Psychometric Society; Iowa City, IA. 1980. [Google Scholar]
- Trull TJ, Goodwin AH, Schopp LH, Hillenbrand TL, Schuster T. Psychometric properties of a cognitive measure of personality disorders. Journal of Personality Assessment. 1993;61(3):536–546. doi: 10.1207/s15327752jpa6103_10. [DOI] [PubMed] [Google Scholar]
- Tucker LR, Lewis C. A reliability coefficient for maximum likelihood factor analysis. Psychometrika. Vol. 1973;38(1):1–10. [Google Scholar]
- Verheul R, Widiger TA. A meta-analysis of the prevalence and usage of the Personality Disorder Not Otherwise Specified (PDNOS) diagnosis. Journal of Personality Disorders. 2004;18(4):309–319. doi: 10.1521/pedi.18.4.309.40350. [DOI] [PubMed] [Google Scholar]
- Westen D. A clinical-empirical model of personality: life after the Mischelian Ice Age and the NEO-lithic Era. Journal of Personality. 1995;63(3):495–524. doi: 10.1111/j.1467-6494.1995.tb00504.x. [DOI] [PubMed] [Google Scholar]
- Westen D, Shedler J. A prototype matching approach to diagnosing personality disorders: Toward DSM-V. Journal of Personality Disorders. 2000;14(2):109–126. doi: 10.1521/pedi.2000.14.2.109. [DOI] [PubMed] [Google Scholar]
- Widiger TA, Clark LA. Toward DSM--V and the classification of psychopathology. Psychological Bulletin. Special Issue: Psychology in the 21st Century. 2000;126(6):946–963. doi: 10.1037/0033-2909.126.6.946. [DOI] [PubMed] [Google Scholar]
- Widiger TA, Simonsen E. Alternative Dimensional Models Of Personality Disorder: Finding A Common Ground. Journal of Personality Disorders. 2005;19(2):110–130. doi: 10.1521/pedi.19.2.110.62628. [DOI] [PubMed] [Google Scholar]
- Yates A. Multivariate Exploratory Data Analysis: A Perspective on Exploratory Factor Analysis. Albany: State University of New York Press; 1987. [Google Scholar]