SUMMARY
Mucoepidermoid carcinoma is the most common malignant salivary gland tumour. However, short series or individual case reports have identified this tumour in the maxilla, mandible, breast tissue and thymus. Mucoepidermoid carcinoma originates from minor salivary glands, and it is therefore surprising that it is not more commonly seen in the tonsil. To date, we believe there has been only one previously reported case in the world literature of mucoepidermoid carcinoma occurring in the tonsil 1. We present a very rare case of mucoepidermoid carcinoma arising from within the structure of the palatine tonsil, rather from the adjacent pharyngeal wall, together with a short review of the literature.
KEY WORDS: Palatine tonsil, Mucoepidermoid carcinoma
RIASSUNTO
Il carcinoma mucoepidermoide rappresenta la neoplasia maligna più comune delle ghiandole salivari. Tuttavia numerosi studi fanno riferimento a casi isolati in cui questo tipo di tumore origina dal mascellare, dalla mandibola, dalla ghiandola mammaria e dal timo. Poiché il carcinoma mucoepidermoide origina solitamente nelle ghiandole salivari, l'origine dalla tonsilla palatina è considerata alquanto insolita. Fino ad oggi riteniamo sia stato precedentemente riportato in letteratura solo un caso di carcinoma mucoepidermoide nella tonsilla 1. Presentiamo un caso molto raro di carcinoma muco epidermoide che originante dalla tonsilla palatina piuttosto che dalla adiacente parete faringea, insieme a una revisione dei casi riportati in letteratura.
Introduction
Mucoepidermoid carcinoma is the most common malignant salivary gland tumour 2-4. It has been reported in all ages with peak incidence at the 4th and 5th decades, with females affected more than males in a 3:1 ratio. It is the most frequent malignant salivary gland neoplasm in children 5. In the major salivary glands, 89.6% of cases present in the parotid 6. Mucoepidermoid carcinoma demonstrates a broad spectrum of aggressiveness, which can be predicted by microscopic grading.
High-grade tumours are highly aggressive and regional lymph node spread is common. The low-grade variant usually demonstrates a favourable outcome, but it is important to note that metastasis may also be present 7. Distant metastasis is rare, but case reports of metastases to the lungs, brain, ovary and peritoneum have been reported 8. Histologically, the tumour is composed of mucous, basaloid, intermediate and epidermoid cells. We present an unusual case of mucoepidermoid carcinoma arising in the tonsil.
Case report
A 48-year-old male presented with an asymptomatic lump in the neck at level II. The lump was progressively increasing in size over 4 weeks. Intra-oral examination and flexible nasoendoscopy was normal. A fine-needle aspiration cytology specimen showed malignant cells with no obvious architecture to determine the tissue of origin. Ultrasound detected the presence of a suspected necrotic node. A CT scan of the neck and chest confirmed a right-sided pathologic node at level II. No other abnormalities were evident. Examination under anaesthesia (EUA) was performed, which was suggestive of a bulky mass within the ipsilateral tonsil, and tonsillectomy was performed. Biopsy confirmed a high-grade mucoepidermoid carcinoma arising from entirely within the substance of the ipsilateral tonsil, and not from the adjacent pharyngeal wall. Management involved complete tonsillectomy with ipsilateral neck dissection level II-IV. Histology of the resected specimen confirmed metastatic carcinoma from the tonsil. He underwent postoperative radiotherapy.
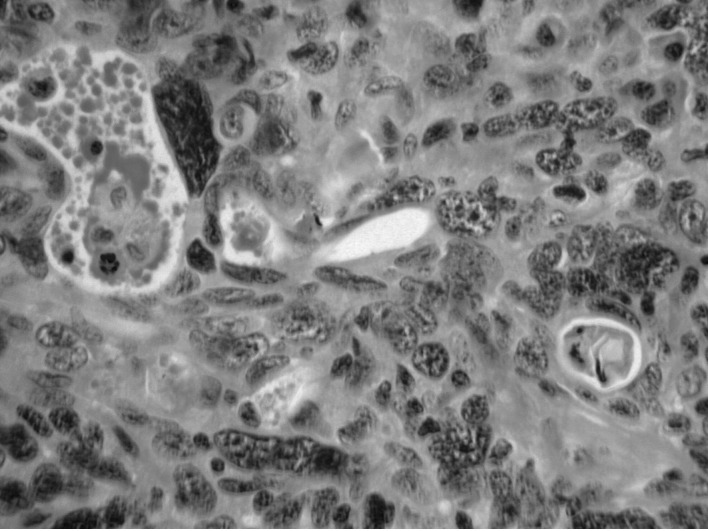
Fig. 1.
High-power haematoxylin and eosin (H&E) staining demonstrating nuclear pleomorphism.
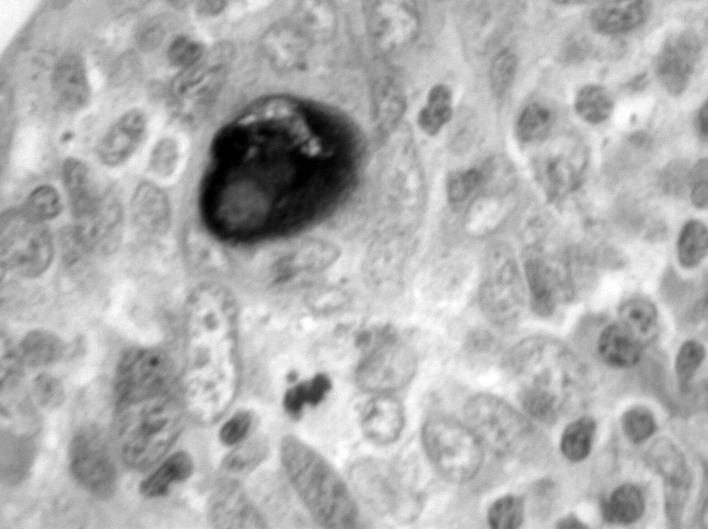
Fig. 2.
High-power combined Alcian blue/periodic acid Schiff stain demonstrating mucin (purple).
Discussion
Mucoepidermoid carcinoma is the most common malignant salivary gland neoplasm 2. Its occurrence in the maxilla, mandible, breast and thymus have been reported 9 10. To date, only one other case of primary mucoepidermoid carcinoma of the tonsil has been documented 1. These tumours arise from reserve cells in the salivary duct system and therefore differentiate into mucin-producing cells, or duct-like epidermoid cells. Interestingly, both cell types are altered neoplastic cells. Mucoepidermoid carcinoma is a malignancy in which histological grading and clinical behaviour correlate well and have a predictive outcome 2. Treatment is therefore based on histological grading of the tumour according primarily to the relative mix of cell types. Other factors that contribute are growth pattern and cellular atypia. The incidence of occult regional metastasis varies from 6 to 46%. Metastasis has been found even in cases with very small tumours.
Management of the tumour depends on its primary site. Low-grade tumours arising in the parotid with no metastasis are treated with superficial parotidectomy, while high-grade tumours are treated by total parotidectomy with or without neck dissection depending on the neck staging. Tumours arising at other sites such as the palate are treated with a minimum of 1 cm excision margin or hemimaxillectomy for high-grade palatal tumours. In the presence of nodal metastasis, radiotherapy in addition to surgery is recommended for both the primary site and the neck. The 5-year survival rate has been reported to be as high as 95% in low-grade tumours, and 50% in intermediate/high-grade tumours. Survival falls dramatically with an age over 55 years 11.
Tamiolakis et al. concluded that in cases of unknown primaries, diagnostic procedures should be aimed at clarifying the histology of the nodal metastases and detecting the primary tumour site 12. In the management of occult primary tumours, bilateral tonsillectomy has been suggested as the minimum investigative procedure at the time of EUA 13. Our case highlights the need for tonsillar biopsy even in those patients with normal EUA findings.
Conclusions
Although mucoepidermoid carcinoma is the most common malignant salivary gland tumour, it is a very rare occurrence within the substance of the palatine tonsil. In cases of an unknown primary, diagnostic procedures should be aimed at clarifying the histology of the nodal metastases and detecting the primary tumour site. Our case highlights the need to biopsy the tonsil in all cases of unknown primary, even in the presence of normal findings on EUA.
References
- 1.Li JX. Clinico-pathologic studies on 143 cases of tonsillar malignancies with special reference to lymphomas. Zhonghua Zhong Liu Za Zhi. 1992;14:433–436. [PubMed] [Google Scholar]
- 2.Loyola AM, Araujo VC, Sousa SOM, et al. Minor salivary gland tumours. A retrospective study of 164 cases in a Brazilian population. Eur J Cancer B Oral Oncol. 1995;31B:197–201. doi: 10.1016/0964-1955(95)00001-x. [DOI] [PubMed] [Google Scholar]
- 3.Lopes MA, Kowalski LP, Santos G, et al. A clinicopathologic study of 196 intraoral minor salivary gland tumours. J Oral Pathol Med. 1999;28:264–267. doi: 10.1111/j.1600-0714.1999.tb02036.x. [DOI] [PubMed] [Google Scholar]
- 4.Jones AS, Beasley NJ, Houghton DJ, et al. Tumours of the minor salivary glands. Clin Otolaryngol. 1998;23:27–33. doi: 10.1046/j.1365-2273.1998.00088.x. [DOI] [PubMed] [Google Scholar]
- 5.Hicks J, Flaitz C. Mucoepidermoid carcinoma of salivary glands in children and adolescents: assessment of proliferation markers. Oral Oncol. 2000;6:454–460. doi: 10.1016/s1368-8375(00)00033-6. [DOI] [PubMed] [Google Scholar]
- 6.Eversole LR. Mucoepidermoid carcinoma: review of 815 reported cases. J Oral Surg. 1970;28:490–495. [PubMed] [Google Scholar]
- 7.Goode RK, Auclair PL, Ellis GL. Mucoepidermoid carcinoma of the major salivary glands: clinical and histopathologic analysis of 234 cases with evaluation of grading criteria. Cancer. 1998;82:1217–1224. doi: 10.1002/(sici)1097-0142(19980401)82:7<1217::aid-cncr2>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]
- 8.Buyukkurt S, Altintas A, Gumurdulu D, et al. Mucoepidermoid carcinoma of the parotid gland with ovarian and peritoneal metastasis. J Obstet Gynaecol Res. 2008;34:271–273. doi: 10.1111/j.1447-0756.2008.00769.x. [DOI] [PubMed] [Google Scholar]
- 9.Hornychova H, Ryska A, Betlach J, et al. Mucoepidermoid carcinoma of the breast. Neoplasma. 2007;54:168–172. [PubMed] [Google Scholar]
- 10.Noda T, Higashiyama M, Oda K, et al. Mucoepidermoid carcinoma of the thymus treated by multimodality therapy: a case report. Ann Thorac Cardiovasc Surg. 2006;12:273–278. [PubMed] [Google Scholar]
- 11.Hiroyuki O, Toshiki T, Koji S, et al. Mucoepidermoid carcinoma of the head and neck: clinical analysis of 43 patients. Jpn J Clin Oncol. 2008;38:414–418. doi: 10.1093/jjco/hyn045. [DOI] [PubMed] [Google Scholar]
- 12.Tamiolakis D, Thomaidis V, Tsamis I, et al. Malignant mucoepidermoid tumor arising in the accessory parotid gland: a case report. Acta Medica (Hradec Kralove) 2003;46:79–83. [PubMed] [Google Scholar]
- 13.Kazi RA. Oncologic rationale for bilateral tonsillectomy in head and neck squamous cell carcinoma of unknown primary source. Internet Journal of Oncology. 2004;2(1) doi: 10.1067/mhn.2001.114309. [DOI] [PubMed] [Google Scholar]