SUMMARY
Benign paroxysmal positioning vertigo (BPPV) is the most frequent vertiginous syndrome. It is caused either by free-floating otoliths in the semicircular canals (canalolithiasis) or by otoconial debris adhering to a canal cupula (cupulolithiasis). The posterior canal is the most frequently involved (80%), while the lateral canal is involved less frequently (15%), and the rarest conditions are anterior canalolithiasis and apogeotropic posterior canalolithiasis (5%). The main diagnostic sign of lateral canal BPPV is paroxysmal horizontal bidirectional positioning nystagmus evoked through Pagnini-McClure's test (head roll in the yaw plane in supine position). In the geotropic variant, which is more frequent, the fast phase of the nystagmus is directed towards the lowermost ear, when the patient lies on the affected side or on the healthy side; in the apogeotropic variant, which is less frequent, the fast phase is directed always toward the uppermost ear, regardless of which side the patient lies on. Paroxysmal nystagmus is more intense on the affected side in the geotropic form, and more intense on the healthy side in the apogeotropic form. The authors describe five cases of another primitive and rare form of lateral BPPV, defined as "direction-fixed paroxysmal nystagmus lateral canal BPPV", which has previously been described by other authors as a transitory step observed during the transformation from an apogeotropic into a geotropic form. It is characterized by typical BPPV symptoms and diagnosed by the presence of a paroxysmal horizontal unidirectional positioning nystagmus, evoked through Pagnini-McClure's test, which is apogeotropic on the affected side and geotropic on the healthy side. In the reported cases, direction-fixed horizontal paroxysmal nystagmus was always transformed into a typical geotropic form. The clinical features and pathophysiology of direction-fixed nystagmus lateral canal BPPV are discussed.
KEY WORDS: Lateral canalolithiasis, Horizontal canalolithiasis, Direction-fixed nystagmus, Lateral geotropic canalolithiasis, Lateral Apogeotropic canalolithiasis
RIASSUNTO
La vertigine parossistica posizionale benigna (VPPB) è la sindrome vertiginosa di più frequente osservazione. Essa è determinata dalla presenza di otoliti liberi nei canali semicircolari (canalolitiasi) o da detriti otolitici adesi alla cupula canalare (cupulolitiasi). Il canale semicircolare posteriore è quello più frequentemente interessato (80%), seguito da quello laterale (15%), mentre molto più rare sono le forma da canalolitiasi anteriore e da canalolitiasi posteriore apogeotropa (5%). Il segno diagnostico primario della VPPB laterale è il nistagmo parossistico orizzontale bidirezionale da posizionamento evocato dalla manovra diagnostica di Pagnini-McClure (rotazione rapida della testa in posizione supina sul piano frontale): nella più frequente forma geotropa, il nistagmo batte verso il lato posto in basso, sia quando il paziente decombe sul lato malato, ove esso è più intenso, sia quando decombe sul lato sano; nella forma apogeotropa, il nistagmo, invece, batte verso il lato posto in alto, sia quando il paziente decombe sul lato malato, ove esso è meno intenso, sia quando decombe sul lato sano. Gli Autori descrivono una nuova forma primitiva di canalolitiasi laterale, definita "canalolitiasi laterale con nistagmo parossistico a direzione fissa", precedentemente descritta da altri Autori come una forma transitoria osservabile durante la trasformazione di una forma apogeotropa in una forma geotropa. Essa è caratterizzata dalla presenza di un nistagmo parossistico orizzontale unidirezionale da posizionamento, evocato dalla manovra diagnostica di Pagnini-McClure, apogeotropo quando il paziente decombe sul lato malato, geotropo quando decombe sul lato sano. Nei casi descritti, la canalolitiasi laterale con nistagmo parossistico a direzione fissa è stata sempre convertita in una forma geotropa. Gli aspetti clinici e fisiopatologici di tale forma sono discussi.
Introduction
Benign paroxysmal positional vertigo (BPPV) is the most common vertiginous syndrome, characterized by recurrent short-lasting episodes of vertigo when the patient changes his/her position. It is usually caused by freefloating otoconia dislodged from the utricle in the semicircular canals (canalolithiasis). Less frequently, otoliths adhere to a semicircular canal cupula, rendering it heavier than the surrounding endolymph (cupulolithiasis). Both conditions are able to change the firing rate of the vestibular nerve 1 2.
There are several known variants of BPPV 3: posterior canalolithiasis and cupulolithiasis, including their rare variants, namely short arm BPPV 4 or posterior apogeotropic canalolithiasis 5; anterior canalolithiasis; geotropic lateral canalolithiasis, caused by the presence of otoliths in the non-ampullary arm; apogeotropic lateral canalolithiasis, caused by either otoliths in the ampullary arm or by lateral cupololithiasis.
The most frequent form is posterior canal BPPV (80% of observed cases), followed by both geotropic and apogeotropic lateral canal BPPV (15%); anterior canal BPPV and apogeotropic posterior canal BPPV are less frequent (5%). The main diagnostic sign of lateral canal BPPV is paroxysmal horizontal bidirectional positioning nystagmus, evoked through Pagnini-McClure test (head roll in the yaw plane in supine position) 6-8; in the geotropic form the fast phase of the nystagmus always beats towards the lowermost ear and the affected side is where nystagmus is the strongest; instead, in apogeotropic lateral canal BPPV paroxysmal nystagmus is directed always toward the uppermost ear and the affected side is where the nystagmus is the weakest.
This study reports five cases of lateral canal BPPV which we define as "direction-fixed paroxysmal nystagmus lateral canal BPPV" because horizontal paroxysmal positioning nystagmus, evoked through Pagnini-Mc Clure's test, is always directed towards the healthy side, when the patient is positioned either on the affected side (apogeotropic nystagmus) or the healthy one (geotropic nystagmus): thus, nystagmus is unidirectional. A similar form was first reported by Vannucchi 9 who observed it as a transitory step of the transformation from an apogeotropic lateral canal BPPV to a geotropic lateral canal BPPV after a certain number of head rotations from side to side in supine position.
The present research for the first time describes a form of "direction-fixed paroxysmal nystagmus lateral canal BPPV" since its diagnosis.
Material and methods
From September 2010 to June 2012, we observed 1234 BPPV, 925 from the posterior canal (75%), 37 from the anterior canal (3%), 272 from the latera1 canal (22%) of which l89 were geotropic lateral canal BPPV (69.5%), 78 apogeotropic lateral canal BPPV (28.7%) and 5 "direction- fixed paroxysmal nystagmus lateral canal BPPV" (1.8%). Herein, we report clinical data for only these five patients,: three males and two females, with an mean age of 52.8 years; before our observation they had suffered from positional vertigo for a period of 1 to 10 days and none had used vestibular suppressant medications for at least 24 hours before the visit or had undergone physical therapy for BPPV in another centre.Patients underwent pure tone audiometry and a bed-side vestibular examination in sitting and supine positions to evaluate spontaneous and evoked nystagmus: gaze-evoked nystagmus – head shaking induced nystagmus (HSIN) – vibration induced nystagmus - paroxysmal positioning nystagmus through Dix-Hallpike test and Pagnini-McClure test.
Paroxysmal horizontal positioning nystagmus as evoked by Pagnini-Mc Clure test was considered the primary diagnostic sign of lateral canal BPPV.
In addition, the following secondary signs of lateralization were considered:
in the sitting position: pseudo-spontaneous nystagmus 10 - Leaning and Bowing nystagmus 11 - HSIN;
in the supine position: the sitting to supine evoked positional horizontal nystagmus 12.
Transformation from an apogeotropic to a geotropic form (geotropization) was attempted through head pitching manoeuvre (HPM) in the sitting position 13-15 and, when HPM failed, through side to side rotations in the supine position 16.
Caloric stimulation was performed according to Fitzgerald- Hallpike's technique (FH) 17. It was performed during the first observation and before that patients underwent therapeutic maneuvers.
Canal paresis was evaluated through Jongkees's formula 18, assuming as significant a labyrinthine prevalence > 25%.
Patients underwent Gufoni's liberatory manoeuvre 19 after geotropization occurred; it was performed five times towards the healthy side. "Forced prolonged position" on the healthy side 20 was then prescribed for the next 8-10 hours. A successful outcome was defined as the absence of paroxysmal horizontal positioning nystagmus evoked through Pagnini-Mc Clure test during the 24 hour-followup examination.
Nystagmus was observed in darkness, through infrared videonystagmoscopy.
Due to a relapse of the disease six months after the first observation, Patient 1 underwent high resolution computed tomography (CT) and magnetic resonance imaging (MRI) of the inner ear (1.5 Tesla). MRI generated threedimensional models of the inner ear. Because of the benign course of their disease, the other four patients did not undergo neuroimaging.
Results
All cases were considered idiopathic due to the absence of significant risk or favouring factors; in particular, recent traumatic events were absent and audiological data were always normal.
Observations in sitting position
Horizontal pseudo-spontaneous nystagmus was observed in three cases, Bowing nystagmus in three cases and Leaning nystagmus in four cases.
In patients 1, 2 and 5, Bowing and Leaning nystagmus occurred toward the left side; in Patient 4, Bowing and Leaning nystamus were directed both towards the left. Leaning nystagmus always occurred in the same direction as pseudo-spontaneous nystagmus, when they occurred together; HSIN was observed in two cases, in Patient 1 in the same direction as Bowing Nystagmus (Table I).
Table I.
Secondary signs of lateralization before geotropization.
| Pseudo-spontaneus nystagmus |
Leaning nystagmus | Bowing nystagmus | HSIN | Sitting to supine nystagmus | |
|---|---|---|---|---|---|
| Patient 1 | Right | Right | Left | Left | Right |
| Patient 2 | Right | Right | Left | Absent | Right |
| Patient 3 | Absent | Absent | Absent | Right | Left |
| Patient 4 | Left | Left | Left | Absent | Left |
| Patient 5 | Absent | Right | Left | Absent | Right |
HSIN: Head shaking induced nystagmus
Observations in supine position
Sitting-to-supine-evoked positional horizontal nystagmus was observed in all subjects; it was directed in the same direction as either pseudo-spontaneous or Leaning nystagmus, except Patient 3 where they did not occur (Table I).
Pagnini-McClure test evoked unidirectional paroxysmal horizontal positioning nystagmus, i.e. on one side we observed an apogeotropic horizontal nystagmus, on the other we observed a geotropic horizontal nystagmus. In four subjects apogeotropic nystagmus was more intense than geotropic, in one subject (Patient 4) vice versa (Table II).
Table II.
Positioning paroxysmal nystagmus before and after geotropization.
| Right Pagnini-Mc Clure's test |
Left Pagnini-Mc Clure's test |
Diagnosis | Geotropization | Bipositional geotropic nystagmus |
|
|---|---|---|---|---|---|
| Patient 1 | Apogeotropic Nystagmus +++ |
Geotropic Nystagmus ++ |
Direction-fixed paroxysmal nystagmus right lateral canalithiasis |
HPM | Right ++++ Left ++ |
| Patient 2 | Apogeotropic Nystagmus +++ |
Geotropic Nystagmus ++ |
Direction-fixed paroxysmal nystagmus right lateral canalithiasis |
Head rotation on right side | Right ++++ Left ++ |
| Patient 3 | Geotropic Nystagmus ++ |
Apogeotropic Nystagmus ++++ |
Direction-fixed paroxysmal nystagmus left lateral canalithiasis |
Head rotation on left side | Left ++++ Right++ |
| Patient 4 | Geotropic Nystagmus ++++ |
Apogeotropic Nystagmus ++ |
Direction-fixed paroxysmal nystagmus left lateral canalithiasiss |
Head rotation on left side | Left ++++ Right +++ |
| Patient 5 | Apogeotropic Nystagmus +++ |
Geotropic Nystagmus ++ |
Direction-fixed paroxysmal nystagmus right lateral canalithiasis |
HPM | Right ++++ Left ++ |
HPM: Head pitching manoeuvre
In Patient 1, the right side, where apogeotropic nystagmus had been evoked, was identified as the affected side: indeed, both HSIN towards the left side and a hyporesponsive right labyrinth on the caloric test allowed us to identify a right-sided labyrinthine disease 21. In addition, directions of both leaning nystagmus and sitting-to-supine horizontal nystagmus were consistent with a diagnosis of a right lateral canal apogeotropic BPPV.
The same interpretation, i.e. the side where apogeotropic nystagmus had been evoked was the affected one, was also assumed for the following four patients too. Geotropization was obtained in two cases by HPM and in three cases by side to side head rotations in the supine position (Table II).
HPM successfully obtained geotropization in one case with one attempt (Patient 1), and in the other case with four attempts (Patient 5). In one case, geotropization occurred during the leaning phase, indicated by a severe horizontal nystagmus towards the healthy side; in the other case, it occurred during the bowing phase, as indicated by a severe horizontal nystagmus towards the healthy side.
Geotropization by HPM was confirmed by the results of Pagnini-McClure's test, which showed the typical paroxysmal horizontal positioning geotropic nystagmus on both the affected and healthy sides.
In three cases (Patients 2, 3 and 4), geotropization was obtained by side to side head rotations in the supine position; on average, four attempts were necessary, with a progressive reduction in intensity of apogeotropic nystagmus; geotropization caused intense geotropic nystagmus 1-3 seconds after the acquisition of the lateral position on the affected side, where apogeotropic nystagmus had been previously evoked.
Post-geotropization observation confirmed the initial diagnosis of the affected side: in Patients 1, 2 and 5 the right semicircular canal was involved; in Patients 3 and 4 the left one was involved, as correctly assumed at initial examination (Table II). After geotropization occurred, secondary signs of lateralization changed their direction, except HSIN (Table III). A significant labyrinthine prevalence on the caloric test (left labyrinth prevalence > 25%) was present before treatment in only Patient 1. Gufoni's manoeuver and the "Forced prolonged position" on the healthy side were able to successfully treat all patients who presented a negative Pagnini-McClure test at the control.
Table III.
Secondary signs of lateralization after geotropization.
| Pseudo-spontaneous nystagmus |
Leaning nystagmus | Bowing nystagmus | HSIN | Sitting to supine nystagmus |
|
|---|---|---|---|---|---|
| Patient 1 | Left | Left | Right | Left | Left |
| Patient 2 | Left | Left | Absent | Absent | Left |
| Patient 3 | Right | Right | Absent | Right | Right |
| Patient 4 | Right | Right | Left | Absent | Right |
| Patient 5 | Absent | Left | Right | Absent | Left |
HSIN: Head shaking induced nystagmus
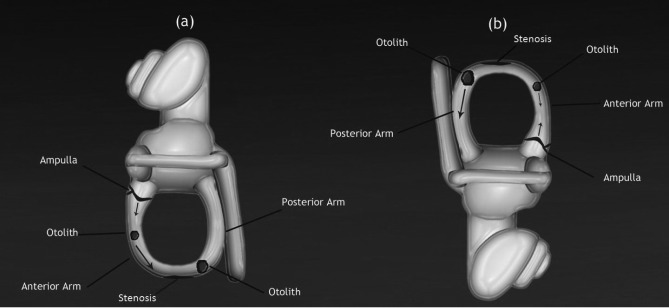
Patient 1 relapsed six months later, presenting the same clinical picture of the first observation; both CT scans and MRI did not show significant alterations of the morphology of his semicircular canals (Fig. 1). All other subjects are still disease-free.
Fig. 1.
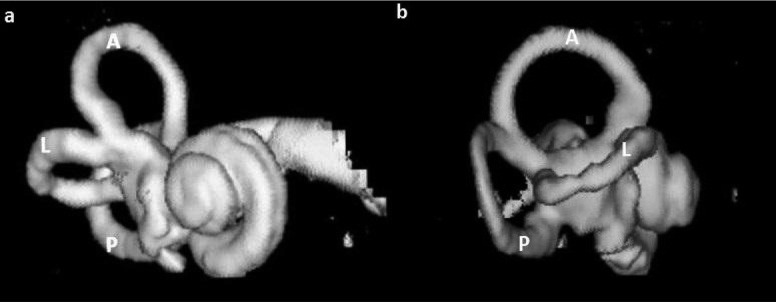
MRI 3D reconstrution of patient's 1 right inner ear. No significant morphological alterations are present (a) Front view. (b.) Right view. A: Anterior semicircular canal; L: Lateral semicircular canal; P: Posterior semicircular canal.
Discussion
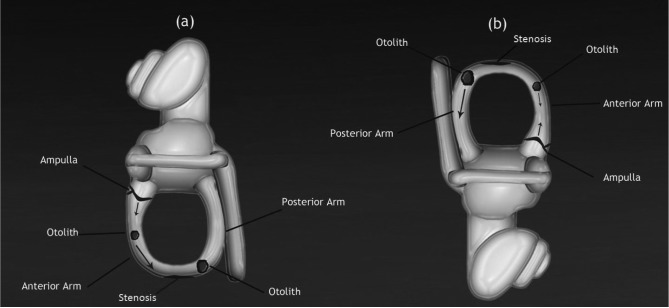
The geotropic form is the most frequent form of lateral canal BPPV. It is caused by free-floating otoconia in the non-ampullary arm of the lateral semicircular canal (Fig. 2). When the patient is lying down on the affected side, the position of the affected canal causes an excitatory ampullopetal endolymphatic flow which provokes a horizontal paroxysmal geotropic nystagmus; when the patient is lying down instead on the healthy side, the position of the affected canal causes an inhibitory ampullofugal endolymphatic flow, which provokes a nystagmus in the opposite direction of the previous one, and therefore again geotropic.
Fig. 2.
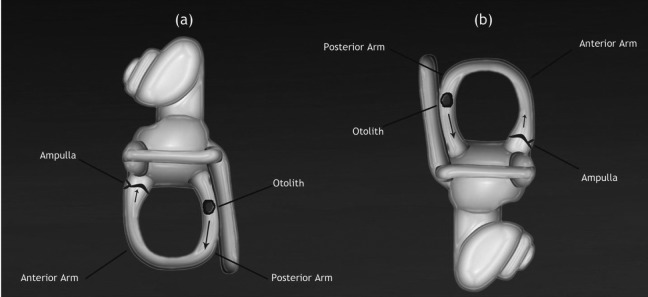
Geotropic left lateral canalolithiasis (left view): (a) on the affected side otoliths in the non-ampullary arm cause ampullopetal flow; (b) on the healthy side otoliths in the non-ampullary arm cause ampullofugal flow (inner arrows).
The apogeotropic form is rarer; it is usually caused by either free-floating otoconial debris in the ampullary arm, or by debris adhering to the canal cupula (lateral cupulolithiasis) (Fig. 3): in both cases, when the patient is lying down either on the affected or healthy sides endolymphatic flow in the affected lateral canal provokes an apogeotropic nystagmus.
Fig. 3.
Apogeotropic left lateral canalolithiasis (left view): (a) on the affected side otoliths in the ampullary arm cause ampullophugal flow; (b) on the healthy side otoliths in the ampullary arm cause ampullopetal flow (inner arrows).
Geotropization improves therapeutic outcome 16. It is achieved through several different manoeuvres: HPM in the sitting position 13, side to side rotations in the supine position 16, Gufoni's liberatory manoeuvre towards the affected side 19, Forced liberatory position on the affected side 20 and HST 22.
Vannucchi 9 first described a case of a two-step lateral apogeotropic canalolithiasis geotropization through head rotations in the supine position: the first step provoked a unidirectional paroxysmal horizontal positioning nystagmus, that was apogeotropic on the affected side, geotropic on the healthy one. In the second step, complete geotropization was achieved through further head rotations.
In all the cases described in the present study, instead, unidirectional paroxysmal horizontal positioning nystagmus, evoked through Pagnini-McClure test, allowed us to diagnose a new form of lateral canal BPPV.
The observation of Patient 1 helped us to diagnose a right lateral canal BPPV because of the presence of signs of distress of the right labyrinth, namely left HSIN and vestibular loss of function of the right side on the caloric test; in addition, secondary signs of lateralization were compatible with the above diagnosis (Table I). Thus, we concluded that the right side was the affected side, where the apogeotropic nystagmus was present. The above criterion was also adopted for the following four patients.
After geotropization occurred, in all patients geotropic nystagmus was stronger on the side where apogeotropic nystagmus was initially observed (Table II): thus it was assumed that this was the affected side.
Therefore, we now propose the following definition: direction- fixed paroxysmal nystagmus lateral canal BPPV is characterized by typical BPPV symptoms and diagnosed due the presence of a paroxysmal horizontal unidirectional positioning nystagmus, evoked through Pagnini-McClure's test; in the observed cases, the side where the apogeotropic nystagmus has been evoked is the affected one.
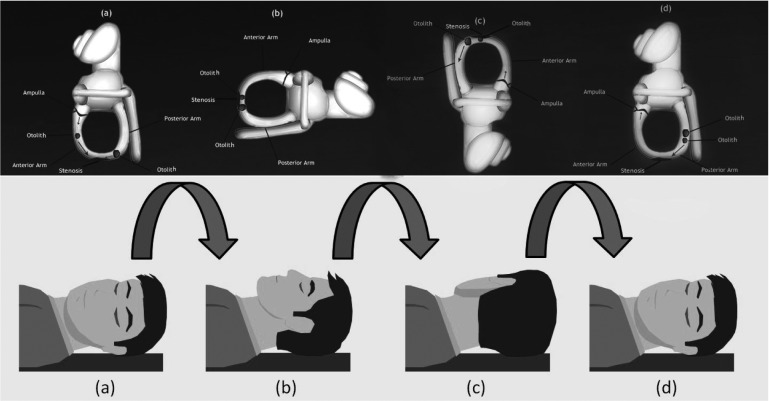
Since the transformation into a classical geotropic form always occurred in the reported subjects, its pathophysiological mechanism is canalolithiasis rather than cupulolithiasis, so we agree with the explanation proposed by Vannucchi 9. Free floating otoliths in either the ampullary and non-ampullary arm of the lateral canal are the main cause of paroxysmal horizontal unidirectional positioning nystagmus; otoliths stand in the lowermost part of the non-ampullary arm of the canal, and thus they are not able to cause an endolymphatic flow, either excitatory or inhibitory, when the patient lies down on the affected side; in this position, ampullofugal flow due to the presence of otoliths in the ampullary arm prevails, so that apogeotropic nystagmus is present (Fig. 4).
Fig. 4.
Direction-fixed paroxysmal nystagmus left lateral canal BPPV on the affected side (a) and the healthy side (b) (left view): one of the possible explanations. Otoliths are either in the non-ampullary arm or in the most declive part of the canal; a higher amount is in the declive part of the canal. A putative stenosis in the declive part of the canal does not allow the largest otolith to pass into the ampullary arm. The ampullofugal flow prevails either on the affected side or on the healthy side (inner arrows).
The presumed explanation of the geotropic nystagmus on the healthy side is more complex.
It must be provoked by the prevalence of an ampullofugal flow in the affected lateral canal, according to Ewald's second law.
The endolymphatic flow, caused by the head rotation, could push otoliths of both the ampullary and non-ampullary arms toward the utricle, but ampullofugal flow could also result from the algebraic sum of an ampullopetal flow, caused by otoliths in the ampullary arm, and prevalent ampullofugal flow, due to a higher amount of otoliths in the declive part of the canal that are pushed toward the utricle (Fig. 5).
Fig. 5.
Geotropization of a direction-fixed paroxysmal nystagmus left lateral canal BPPV by side-to-side head rotations in supine position (left view). (a) decubitus on the affected side; (b) intermediate position during rotation; (c) decubitus on the healthy side; (d) Complete geotropization is achieved when all otoliths pass in the non-ampullary arm; the endolymphatic flow on the affected side becomes ampullopetal (inner arrows).
Side to side rotations progressively move otoliths from the anterior to the posterior aspect of the lateral canal and geotropization is achieved when all otoliths shift from the ampullary to the non-ampullary arm.
This event is always characterized by the occurrence of a sudden paroxysmal geotropic nystagmus on the affected side, which begins after a few seconds of latency from the acquisition of the lateral position. Latency is related to the time that otoliths take to fall down due to the force of gravity.
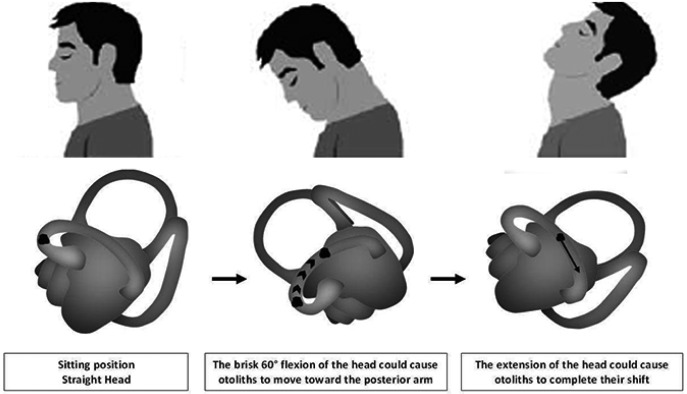
Geotropization through HPM is characterized by the same dynamics (Fig. 6): complete geotropization is achieved when all the debris moves from the anterior arm to the posterior arm of the lateral canal by head-pitching movements; in this case, however, geotropization must be confirmed through Pagnini-McClure test.
Fig. 6.
Geotropization through the head pitching manoeuvre in sitting position.
Why does a direction-fixed paroxysmal nystagmus lateral canal BPPV happen? According to Vannucchi's multi-step interpretative model, it is possible that the patient has instinctively self-undergone a "forced prolonged position", which partially moved otoliths from the ampullary arm to the lowermost part of the non-ampullary arm.
Here, we draw attention to Patient 1's intriguing history: he relapsed six months after our first observation, the oculomotor pattern was the same of the first observation and we again diagnosed a direction-fixed paroxysmal nystagmus lateral canal BPPV.
The repetition of the event in the same terms as the first time let us think that putative alterations of lateral canal morphology, stenoses, obturation, or anatomic variations 23 could be possible reasons for the entrapment of otoliths in both the anterior and posterior aspects of the lateral canal, causing endolymphatic currents responsible of the oculomotor pattern of the direction-fixed paroxysmal nystagmus lateral canal BPPV. However, neither CT scans or MRI showed significant alterations of the morphology of the semicircular canals (Fig. 1), but this could be related to the fact that current imaging techniques offer insufficient sensitivity in detecting subtle canal alterations.
What is the importance of "direction-fixed paroxysmal nystagmus lateral canal BPPV"?
First of all, a new form of lateral canal BPPV has been identified; the transformation into a geotropic form, always occurring in the patients described in the present study, sustains, in our opinion, more effectively the hypothesis of "canalolithiasis" rather than "cupulolithiasis" as the pathophysiological mechanism of most lateral canal BPPV.
The second consideration has practical relevance: an erroneous diagnosis of acute unilateral vestibular loss of function could be made if only directional characteristics of positional nystagmus were evaluated. Patients usually arrive in the emergency room still in the supine position, with severe neurovegetative symptoms and, sometimes, a complete vestibular examination cannot be performed; furthermore, pseudo-spontaneous nystagmus and/or sitting to supine positioning nystagmus, with direction opposite to the nystagmus evoked through Pagnini-McClure's test, could be interpreted as a variable direction nystagmus, sign of a possible central vestibular disease, which requires complex and expensive diagnostic procedures, which are unnecessary if a correct diagnosis is made.
Conclusions
BPPV was previously considered as a simplex phenomenon, caused by otoconial material adhering to the cupula of the posterior canal, making it heavier. However, it is a more complex condition, since otolith deposition and drift can involve all the tracts of the semicircular canals and occur simultaneously in different parts of a single canal or in multiple canals, causing, depending on the location and size of otoconial debris, several and sometimes atypical oculomotor patterns which do not always need to be considered as indicators of central nervous system diseases.
"Direction-fixed paroxysmal nystagmus lateral canal BPPV" is the rarest form of lateral canal BPPV; its pathogenesis is still unclear and the observed cases are still too few to allow definitive conclusions.
Finally, both the knowledge of all possible BPPV subtypes as well as careful and complete vestibular examination, in both sitting and supine positions, can prevent specialists from making erroneous diagnoses.
References
- 1.Raiguru SM, Rabbitt RD. Afferent responses during experimentally induced semicircular canalithiasis. J Neurophysiol. 2007;97:2355–2363. doi: 10.1152/jn.01152.2006.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Valli P, Botta L, Zucca G, et al. Simulation of cupulolithiasis and canalolithiasis by an animal model. J Vestib Res. 2008;18:89–96. [PubMed] [Google Scholar]
- 3.Bhattacharyya N, Baugh RF, Orvidas L, et al. Clinical practice guideline: Benign paroxismal positional vertigo. Otolaryngology- Head and Neck Surgery. 2008;139:47–81. doi: 10.1016/j.otohns.2008.08.022. [DOI] [PubMed] [Google Scholar]
- 4.Cherian N, Oas J. Short-Arm BPPV. Does It Really Exist? 2006. Feb, http://www.aro.org/archives/2006/2006_1255.html 30th Midwinter Meeting, Feb 2006; Abstract 1255.
- 5.Vannucchi P, Pecci R, Giannoni B. Posterior semicircular canal benign paroxysmal positional vertigo presenting with torsional downbeating nystagmus: an apogeotropic variant. Int J Otolaryngol. 2012 doi: 10.1155/2012/413603. article ID 413603, 9 pages, doi:10.1155/2012/413603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cipparrone L, Corridi G, Pagnini P. Cupulolitiasi. In: Boots-Formenti, editor. V Giornata Italiana di Nistagmografia Clinica. Milano: 1985. pp. 36–53. [Google Scholar]
- 7.McClure A. Lateral canal BPPV. J Otolaryngol. 1985;14:30–35. [PubMed] [Google Scholar]
- 8.Pagnini P, Nuti D, Vannucchi P. Benign paroxysmal vertigo of the horizontal canal. ORL J Otorhinolaryngol Relat Spec. 1989;51:161–170. doi: 10.1159/000276052. [DOI] [PubMed] [Google Scholar]
- 9.Vannucchi P, Pecci R. About nystagmus transformation in a case of apogeotropic lateral semicircular canal benign paroxysmal positional vertigo. Int J Otolaryngol. 2011;2011:687921–687921. doi: 10.1155/2011/687921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Asprella-Libonati G. Pseudo-spontaneous nystagmus: a new sign to diagnose the affected side in lateral semicircular canal benign paroxysmal positional vertigo. Acta Otorhinolaryngol Ital. 2008;28:73–78. [PMC free article] [PubMed] [Google Scholar]
- 11.Lee S-H, Choi K-D, Jeong S-H, et al. Nystagmus during neck flexion in the pitch plane in benign paroxysmal positional vertigo involving the horizontal canal. J Neurol Sci. 2007;256:75–80. doi: 10.1016/j.jns.2007.02.026. [DOI] [PubMed] [Google Scholar]
- 12.Nuti D, Vannucchi P, Pagnini P. Benign paroxysmal positional vertigo of the horizontal canal: a form of canalolithiasis with variable clinical features. J Vest Res. 1996;6:173–184. [PubMed] [Google Scholar]
- 13.Califano L, Melillo MG, Mazzone S, et al. Converting apogeotropic into geotropic lateral canalolithiasis by head-pitching manoeuvre in the sitting position. Acta Otorhinolaryngol Ital. 2008;28:287–291. [PMC free article] [PubMed] [Google Scholar]
- 14.Asprella-Libonati G. Lateral semicircular canal benign paroxysmal positional vertigo diagnostic signs. Acta Otorhinolaryngol Ital. 2010;30:222–222. [PMC free article] [PubMed] [Google Scholar]
- 15.Califano L. Converting apogeotropic into geotropic lateral canalolithiasis by head-pitching manoeuvre in the sitting position. Acta Otorhinolaryngol Ital. 2010;30:224–224. [PMC free article] [PubMed] [Google Scholar]
- 16.Nuti D, Vannucchi P, Pagnini P. Lateral canal BPPV: which is the affected side? Audiological Medicine. 2005;3:16–20. [Google Scholar]
- 17.Fitzgerald G, Hallpike CS. Studies on human vestibular function: I. Observations on the directional preponderance of caloric nystagmus resulting from cerebral lesions. Brain. 1942;65:115–137. [Google Scholar]
- 18.Jongkees L. The value of the caloric test of the labyrinth. Arch Otorhinolaryngol. 1948;48:402–417. [Google Scholar]
- 19.Gufoni M, Mastrosimone L. Trattamento con manovra di riposizionamento per la canalolitiasi orizzontale. Acta Otorhinolaryngol Ital. 1998;18:363–367. [PubMed] [Google Scholar]
- 20.Vannucchi P, Giannoni B, Giuffreda P, et al. The therapy of benign paroxysmal positional vertigo of the lateral semicircular canal. In: Versino M, Zambardieri D, editors. International Workshop on Eye Movements. Pavia: 1994. pp. 321–324. [Google Scholar]
- 21.Strupp M, Brandt T, Steddin S. Horizontal canal benign paroxysmal positioning vertigo: reversible ipsilateral caloric hypoexcitability caused by canalolithiasis? Neurology. 1995;45:2072–2076. doi: 10.1212/wnl.45.11.2072. [DOI] [PubMed] [Google Scholar]
- 22.Oh SY, Kim JS, Jeong SH, et al. Treatment of apogeotropic benign positional vertigo: comparison of therapeutic Head-shaking and modified Semont Maneuver. J Neurol. 2009;256:1330–1336. doi: 10.1007/s00415-009-5122-6. [DOI] [PubMed] [Google Scholar]
- 23.Horii A, Kitahara T, Osaki Y, et al. Intractable benign paroxysmal positioning vertigo: long-term follow-up and inner ear abnormality detected by three-dimensional magnetic resonance imaging. Otol Neurotol. 2010;31:250–255. doi: 10.1097/MAO.0b013e3181cabd77. [DOI] [PubMed] [Google Scholar]