SUMMARY
The peroneal artery perforator (PNAP) flap is a good choice for reconstruction in intraoral soft-tissue rehabilitation. In this article, the authors propose the use of a modified PNAP flap with pedicle extension.
KEY WORDS: Peroneal artery perforator flap, Free flap, Microsurgery, Squamous cell carcinoma
RIASSUNTO
Il lembo perforante peroniero (PNAP, peroneal artery perforator) rappresenta una buona opzione ricostruttiva nel trattamento chirurgico dei difetti dei tessuti molli del cavo orale. In questo articolo gli autori presentano un allestimento del lembo PNAP modificato con estensione del peduncolo.
Introduction
Intraoral soft-tissue reconstruction may be performed using various tissues of different qualities that should be correlated with oral anatomy and function. The anatomical and functional characteristics of the floor of the mouth, tongue, and soft palate differ, and the treatment of surgical defects may involve more than one of these structures. Thus, a single type of intraoral reconstructive flap is not appropriate for all situations.
For many years, the forearm free flap 1 was considered the best option for intraoral soft tissue reconstruction due to its pliability and long, large pedicle. The anterolateral thigh (ALT) perforator flap 2 3 is currently preferred, because it has characteristics similar to the forearm free flap but is associated with lower donor-site morbidity 4.
Herein, we propose the use of a modified peroneal artery perforator (PNAP) 5 6 flap with pedicle extension in intraoral soft-tissue rehabilitation. This flap has the same characteristics as a forearm flap and may be useful in cases where an anterolateral flap is too thick for functional soft-tissue reconstruction.
Case series
Description of clinical cases
Two patients affected by squamous cell carcinoma (SCC) of the anterior floor of the mouth (cT2N0M0) underwent surgical tumour resection through anterior pelvectomy associated with a bilateral supraomohyoid neck dissection (SOHND). The surgical defect in one patient was reconstructed with a PNAP flap. Microvascular ischaemia occurred 10 h after surgical flap transfer due to an excessively long portion of residual peroneal artery on the side opposite the microvascular anastomosis that caused flow turbulence and thrombosis. We resolved this problem and saved the flap by correcting the geometry of the microvascular anastomosis. Despite some difficulty with flap placement due to the short, small-calibre (< 1 mm) pedicle, we were able to maximize residual function with minimal tongue scarring or immobilization. We analyzed the efficacy of this reconstruction in terms of tongue-function recovery and speaking using the voice-related quality of life test (V-RQOL).
Our second patient presented with SCC in the same oncological phase. To obtain a longer pedicle that provided a better fit for the calibre of the recipient vessels in the lateral neck, we extended the pedicle to the interosseous vessel. The flap was harvested and transferred successfully, and the donor site was closed directly. Excellent tongue mobility allowed the patient to recover speech and deglutition, and achieve a high V-RQOL score.
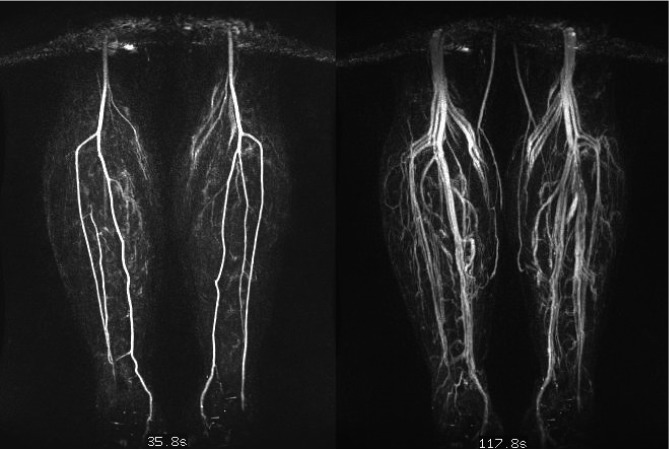
Patients must be safely and comprehensively evaluated for disease or significant anatomic variants before surgery. A magnetic resonance angiogram (MRA) was performed before surgery to establish the flap harvesting feasibility and 3 months after surgery to evaluate flow changes in the left peroneal artery and assess donor-site morbidity. The postoperative MRA showed normal leg vascularization with retrograde flow in the interosseous artery and normal vascularization in the collateral perforating vessels. A standard radiographic examination of the leg was performed 3 months after surgery. The radiograph showed that the fibula retained a normal and stable position due to adequate interosseous membrane preservation. Due to the optimal characteristics of this flap type, we were able to maximize tongue mobility in these two patients. They both showed a good recovery of speech ability and achieved VRQOL scores of 20 and 21, respectively (possible score range: 10-50).
Our extension of the traditional PNAP pedicle facilitated the microsurgical procedure and flap placement. Donorsite scarring was acceptable and the MRA (Fig. 1) showed a reverse flow into the peroneal artery that provided normal vascularization to the muscular structures and skin in the lower three-quarters of the leg. The fibula remained in position due to the preservation of the interosseus membrane and muscular anchorage.
Fig. 1.
AngioRM shows reverse peroneal artery flow a) arterial phase b) venous phase.
Surgical technique and microvascular flap
A tourniquet was first applied to the thigh. The size of the skin defect was measured and the flap was designed to overlay the course of the peroneal artery, which was mapped onto the skin surface using the palpable posterior fibular border.
Flap dissection began anterior to the posterior intermuscular septum and 5 cm distal of the fibular head, to avoid injury to the common peroneal nerve. An incision was made along the anterior border of the flap to the depth of the crural fascia. Dissection was performed carefully over the soleus muscle (proximal) and intermuscular septum (distal) in the proximity of the preoperatively located perforators. Magnification (4×) was used to facilitate the dissection of the pedicle to the intramuscular (soleus) passage of the perforating vessels beneath the fibula along the peroneal axis. A 6-cm fibular bone stock was then harvested.
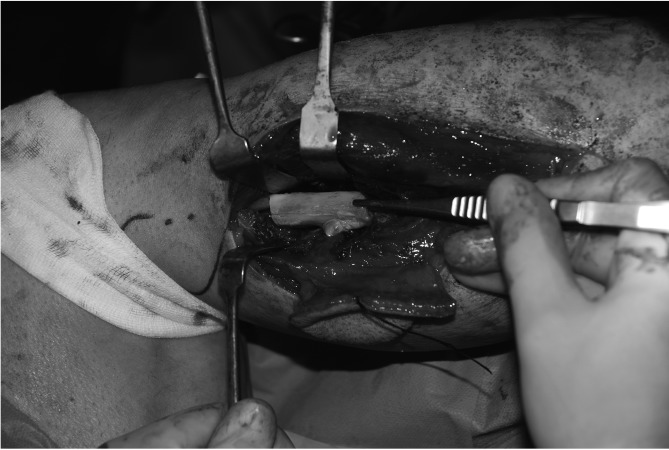
A reciprocating saw was used to make a 2-cm cut in the distal position to access the perforator vessels beneath the fibula and a 4-cm cut in the proximal position to access the perforator point (Fig. 2). After subperiosteal skeletonization, the osteotomy exposed an interosseous pedicle that could be readily dissected. Although we harvested the pedicle in a cranial direction, it would also be possible to take the vessel in a caudal direction. At this point in the procedure, we determined the required pedicle length (Figs. 3, 4).
Fig. 2.
Fibular ostectomy.
Fig. 3.
Extended PNAP pedicle.
Fig. 4.
Extended PNAP flap harvested: notice flap thickness and the long pedicle.
Our experience emphasizes the importance of paying attention to the geometry 7 of the pedicle (Fig. 5) because the perforator vessels arise perpendicularly from the main trunk. For this reason, it is important to close the side opposite the microvascular anastomosis very close to the origin of the perforator vessels, to avoid turbulence in the main arterial trunk that could cause thrombosis.
Fig. 5.
Microanastomosis: notice the calibre match between donor and recipient vessels.
Discussion
The progressive increase in the use of free flaps has furthered the development of this reconstructive technique in the last 25 years. Further innovation has occurred recently, following the increased popularity of perforator flaps. The term "perforator flap" was first used by Koshima 8 and defined specifically by Wei 9, although the harvesting of such flaps had been described in the literature about a decade earlier. Hallock 10 recently proposed a more detailed terminology that refers to indirect perforator flaps, indicating blood vessels that require intramuscular dissection, and direct perforator flaps, indicating vessels that pass through the intramuscular septa or a more direct path to the skin. All perforator flaps are characterized by the thinness of the cutaneous flap segment in comparison with myocutaneous flaps, a short pedicle length and relatively small vessel calibre, and minimal donor-site morbidity 11 . For many years, the forearm free flap was considered to be the best option for intraoral soft-tissue reconstruction, due to its pliability and the long, large-calibre pedicle 12. However, such flaps are associated with high donor-site morbidity 13-15. Currently, the ALT perforator flap is most commonly used because it has similar characteristics but is associated with lower donor-site morbidity 16 17. However, ALT flaps require thinning, which increases the risk of damage to the perforator vessels. In intraoral reconstruction, the risks of marginal flap necrosis and neck fistulization are high 18.
Pedicle calibre is also an important consideration. In a conventional axial free-tissue transfer in the head and neck area, the calibre of the flap pedicle 19 frequently fits well with those of recipient vessels, including the thyroid, facial, and lingual arteries. Perforator free flaps provide a less favourable match between the calibre of the pedicle (≤ 1 mm) and those of the recipient vessels. In our proposed technique, we sought to improve this match and provide a pedicle of adequate length for use with microvascular anastomosis in intraoral reconstruction.
For these reasons, we propose a thin and pliable perforator flap with an elongated pedicle, which improves the fit of the pedicle calibre and increases functional reliability in intraoral soft-tissue reconstructions.
PNAP flaps have the best characteristics for intraoral reconstruction and are associated with reduced donor-site morbidity, but are not widely used in maxillofacial surgery because the short and small-calibre pedicle has been assumed to increase complication rates. We have attempted to overcome this limitation by extending the pedicle to the peroneal artery origin. We have demonstrated that this technique is unproblematic and has no negative effect on the blood supply of the fibular donor site. The compromise of the fibula free flap for future osseous reconstructions is a disadvantage when preoperative magnetic resonance angiogram contraindicates contralateral harvesting. We have thus been able to combine the best flap features with low donor-site morbidity in a user-adjustable, long, large-calibre vessel flap. This technique offers a useful alternative in microvascular free-tissue transfer when a primary ultrathin pliable flap is required to cover intraoral mucosal defects.
References
- 1.Avery CM. Review of the radial free flap: is it still evolving, or is it facing extinction? Part one: soft-tissue radial flap. Br J Oral Maxillofac Surg. 2010;8:245–252. doi: 10.1016/j.bjoms.2009.09.004. [DOI] [PubMed] [Google Scholar]
- 2.Wei FC, Jain V, Celik N, et al. Have we found an ideal soft tissue flap? An experience with 672 anterolateral thigh flaps. Plast Reconstr Surg. 2002;109:2219–2226. doi: 10.1097/00006534-200206000-00007. [DOI] [PubMed] [Google Scholar]
- 3.Shieh SJ, Chiu HY, Yu JC, et al. Free anterolateral thigh flap for reconstruction of head and neck defects following cancer ablation. Plast Reconstr Surg. 2000;105:2349–2357. doi: 10.1097/00006534-200006000-00006. [DOI] [PubMed] [Google Scholar]
- 4.Kimata Y, Uchiyama K, Ebihara S, et al. Anterolaleral thigh flap donor side complications and morbidity. Plast Reconstr Surg. 2000;106:584–589. doi: 10.1097/00006534-200009030-00009. [DOI] [PubMed] [Google Scholar]
- 5.Ozalp T, Masquelet AC, Begue TC. Septocutaneous perforators of the peroneal artery relative to the fibula: anatomical basis of the use of pedicled fasciocutaneous flap. Surg Radiol Anat. 2006;28:54–58. doi: 10.1007/s00276-005-0059-7. [DOI] [PubMed] [Google Scholar]
- 6.Baj A, Bellocchio G, Marelli S, et al. Reconstruction of the anterior floor of the mouth using a peroneal perforator free flap. A case report. Acta Otorhinolaryngol Ital. 2010;30:47–51. [PMC free article] [PubMed] [Google Scholar]
- 7.Urken ML, Vickery C, Weinberg H, et al. Geometry of the vascular pedicle in free tissue transfers to the head and neck. Arch Otolaryngol Head Neck Surg. 1989;115:954–960. doi: 10.1001/archotol.1989.01860320064020. [DOI] [PubMed] [Google Scholar]
- 8.Koshima I, Soeda S, Yamasaki M, et al. The free or pedicled anteromedial thigh flap. Ann Plast Surg. 1988;21:480–485. doi: 10.1097/00000637-198811000-00015. [DOI] [PubMed] [Google Scholar]
- 9.Wei FC, Jain V, Suominen S, et al. Confusion among perforator flaps: What is a true perforator flap? Plast Reconstr Surg. 2001;107:874–876. doi: 10.1097/00006534-200103000-00037. [DOI] [PubMed] [Google Scholar]
- 10.Hallock GG. The complete nomenclature for combined perforator flaps. Plast Reconstr Surg. 2011;127:1720–1729. doi: 10.1097/PRS.0b013e31820a662b. [DOI] [PubMed] [Google Scholar]
- 11.Baj A, Ali Youssef D, Monteverdi R, et al. Recontruction of partial maxillary defects with the double-barrel fibula free flap. Acta Otorhinolaryngol Ital. 2010;30:299–302. [PMC free article] [PubMed] [Google Scholar]
- 12.Soutar DS, McGregor IA. The radial forearm flap in intraoral reconstruction: The experience of 60 consecutive cases. Plast Reconstr Surg. 1986;78:1–8. doi: 10.1097/00006534-198607000-00001. [DOI] [PubMed] [Google Scholar]
- 13.Lutz BS, Wei FC, Chang SC, et al. Donor site morbidity after suprafascial elevation of the radial forearm flap: a prospective study in 95 consecutive cases. Plast Reconstr Surg. 1999;103:132–137. doi: 10.1097/00006534-199901000-00021. [DOI] [PubMed] [Google Scholar]
- 14.Richardson D, Fisher SE, Vaughan ED, et al. Radial forearm flap donor site complications and morbidity: a prospective study. Plast Reconstr Surg. 1997;99:109–115. doi: 10.1097/00006534-199701000-00017. [DOI] [PubMed] [Google Scholar]
- 15.Pellini R, Mercante G, Spriano G. Step-by-step mandibular reconstruction with free fibula flap modelling. Acta Otorhinolaryngol Ital. 2012;32:405–409. [PMC free article] [PubMed] [Google Scholar]
- 16.Camaioni A, Loreti A, Damiani V, et al. Anterolateral thigh cutaneous flap vs. radial forearm free-flap in oral and oropharyngeal reconstruction: an analysis of 48 flaps. Acta Otorhinolaryngol Ital. 2008;28:7–12. [PMC free article] [PubMed] [Google Scholar]
- 17.Huang CH, Chen HC, Huang YL, et al. Comparison of the radial forearm flap and the thinned anterolateral thigh cutaneous flap for reconstruction of tongue defect: an evaluation of donor-site morbidity. Plast Reconstr Surg. 2004;114:1704–1710. doi: 10.1097/01.prs.0000142476.36975.07. [DOI] [PubMed] [Google Scholar]
- 18.Alkureishi LW, Shaw-Dunn J, Ross GL. Effects of thinning the anterolateral thigh flap on the blood supply to the skin. Br J Plast Surg. 2003;56:401–408. doi: 10.1016/s0007-1226(03)00125-5. [DOI] [PubMed] [Google Scholar]
- 19.Baj A, Ferrari S, Bianchi B, et al. Iliac crest free flap in oromandibular reconstruction. 13 cases study. Acta Otorhinolaryngol Ital. 2003;23:102–110. [PubMed] [Google Scholar]