Abstract
Purpose
We compared the clinical outcomes of patients with ureteral or renal stones treated with ureteroscopy, shock wave lithotripsy using HM3 (Dornier®) and nonHM3 lithotripters, and percutaneous nephrolithotomy.
Materials and Methods
A systematic literature search identified 6, 4 and 3 randomized, controlled trials of treatment of distal and proximal ureteral stones, and renal stones, respectively, published between 1995 and 2010. Overall stone-free, re-treatment and complication rates were calculated by meta-analytical techniques.
Results
Based on the randomized, controlled trials evaluated the treatment of distal ureteral stones with semirigid ureteroscopy showed a 55% greater probability (pooled RR 1.55, 95% CI 1.13–2.56) of stone-free status at the initial assessment than treatment with shock wave lithotripsy. Patients treated with semirigid ureteroscopy were also less likely to require re-treatment than those treated with shock wave lithotripsy (nonHM3) (RR 0.14, 95% CI 0.08–0.23). The risk of complications was no different between the 2 modalities. Only 2 of the 4 randomized, controlled trials identified for proximal ureteral stones evaluated flexible ureteroscopy and each focused specifically on the treatment of stones 1.5 cm or greater, limiting their clinical relevance. The degree of heterogeneity among the studies evaluating renal stones was so great that it precluded any meaningful comparison.
Conclusions
Semirigid ureteroscopy is more efficacious than shock wave lithotripsy for distal ureteral stones. To our knowledge there are no relevant randomized, controlled trials of flexible ureteroscopy treatment of proximal ureteral calculi of a size commonly noted in the clinical setting. Collectively the comparative effectiveness of ureteroscopy and shock wave lithotripsy for proximal ureteral and renal calculi is poorly characterized with no meaningful published studies.
Keywords: kidney, ureter, calculi, lithotripsy, ureteroscopy
Kidney stones are a common and costly disease. Recent epidemiological investigations show that approximately 10% of the population in the United States is affected by kidney stone disease in their lifetime and this rate is increasing.1 Medical evaluation for and treatment of kidney stones places a significant economic burden on society. The Urologic Diseases in America project estimated an annual cost of more than $2 billion in the United States alone.2
Most patients with symptomatic kidney stones are treated with SWL or URS.3 Each modality has relative advantages and disadvantages, and for certain clinical scenarios one may be more optimal than the other. However, selecting the optimal treatment can be challenging. Despite published Cochrane Reviews and clinical treatment guidelines there are no universally accepted paradigms to manage upper urinary tract calculi.4,5
In the years since the mentioned reviews were done a number of new clinical investigations have attempted to resolve this issue. Thus, we performed a systematic review and network meta-analysis to compare the outcomes of the treatment of ureteral and renal stones with SWL and URS based on currently available RCTs.
METHODS
Study Identification and Selection
We used certain criteria to consider published studies for review, including population (adults who required intervention for renal or ureteral calculi), intervention (SR-URS, flexible URS, SWL-HM3, SWL-other, that is second, third and fourth generations, and PNL), study design (RCTs comparing any of mentioned modalities) and publication date (URS and PNL studies from 1995 to 2010 and SWL studies from 1980 to 2010).
For the predefined search strategy of the MEDLINE ®, Embase™ and Cochrane databases we used terms related to renal and ureteral stones, URS, SWL and PNL. Titles and abstracts were screened to ascertain whether studies met predefined selection criteria. Those that met the criteria and those for which it was unclear whether the criteria had been met were further screened using the full text report. Two reviewers extracted details on study design, population characteristics, interventions, SFR, retreatment rate, auxiliary procedures and complications.
For SFR the fraction of patients with a successful outcome of the total number of patients treated was extracted for each time point reported. For studies describing SFR at only 1 time point the outcome was assigned to 1) the end of followup if it was reported that the evaluation time point varied by patients during followup, 2) a specific week if that information was provided, or 3) week 1 if no time related information was provided. In studies mentioning initial SFR and SFR after re-treatment the initial SFR was assigned to week 1 if no specific evaluation time was reported. Success after re-treatment was assigned to the time at the end of followup or to the time point reported.
All trials were evaluated for validity with the assessment instrument of Jadad et al, which comprises 7 items and assigns a score of 0 to 5 with 5 representing the highest quality.6 The results of this validity assessment were not explicitly used for analysis but they served as additional information to determine the quality of the evidence base when interpreting results.
Meta-Analysis
Bayesian network meta-analysis techniques were used to combine the results of the identified studies.7–10 Logistic regression models were applied to analyze initial SFR, re-treatment rate and complications. We also performed analysis using all available data on SFR with time.11 For each outcome goodness of fit to the data was compared for fixed and random effects models, as measured by deviance information criteria.12
Noninformative prior distributions were used for all parameters of interest to avoid the criticism of Bayesian analyses that prior beliefs (priors) influence results. Win-Bugs was used for analysis.13 Outcome measures are shown as the estimated RR. For the number of auxiliary procedures the rate ratio was used to reflect differences between treatments.
RESULTS
Study Identification and Selection
The literature search resulted in 2,641 potentially relevant studies. The abstract review excluded 2,425 studies (92%) from analysis, primarily since they did not provide comparisons of interest. Of the 216 remaining studies 203 (94%) were excluded by the full text review since they did not describe comparisons of interest (101 or 50%) or were observational (102 or 50%). Thus, 13 RCTs were included in analysis (tables 1 and 2).14–26
Table 1.
| Stone Site (references) | Country | Followup | Stone Site | Lithotripsy or Lithotomy (device) | Quality Score6 | No. Pts | Mean ± SD Age (range) | Stone Size Inclusion Criterion (cm) | Mean ± SD Stone (range) |
|---|---|---|---|---|---|---|---|---|---|
| Ureter: | |||||||||
| Verze et al14 | Italy | 3 Mos | Distal | SWL-other (Modulith SLX), SR-URS (Swiss LithoClast® Master) | 1 | 137, 136 | 50.5 (18–80), 49.4 (21–81) | 0.5–1.5 | Size 1.0 cm (0.5–1.5), 1.0 (0.6–1.5) |
| Zeng et al15 | China | 4 Wks | Distal | SWL-other (HB-SWL-V), SR-URS (ureteroscope, Richard Wolf, Knittlingen, Germany) | 1 | 210, 180 | 51, 40 | Size (0.5–2.1 cm), (0.6–2.0) | |
| Pearle et al16 | United States | 3 Mos | Distal | SWL-HM3, SR-URS (Ho:YAG) | 2 | 32, 32 | 41.2 ± 14.9, 25.7 ± 4.9 | Less than 1.5 | Size 0.7 ± 0.2 cm, 0.6 ± 0.3 |
| Hendrikx et al17 | Netherlands | 3 Mos | Distal | SWL-other (Dornier HM4), SR-URS | 1 | 69, 87 | Less than 0.5 | — | |
| Peschel et al18 | Austria | 6 Wks | Distal | SWL-other (Dornier MFL 5000), SR-URS (LithoClast) | 1 | 40, 40 | 47.8 (28–66) vs 40.1 (20–77), 49.1 (28–72) vs 40.6 (22–72) less vs greater than 0.5 cm stone | Size 0.4 (0.2–0.5) vs 0.9 cm (0.6–1.6), 0.4 (0.2–0.5) vs 0.9 (0.6–1.4) less vs greater than 0.5 cm stone | |
| Salem19 | Egypt | 3 Mos | Proximal | SR-URS (Swiss LithoClast), SWL-HM3 | 2 | 100, 100 | 41.2 (36–50) vs 36.7(20–48), 42.8(37–60) vs 35.4 (37–55) less than 1 vs 1 cm or greater stone | 0.5–2.0 | Size 0.7 cm (0.6–0.9) vs 1.2 (0.2–2.0), 0.6 (0.5–0.9) vs 1.3 (1.1–2.0) less than 1 vs 1 cm or less |
| Basiri et al20 | Iran | 3 Wks | Proximal | SR-URS, PNL | 2 | 50, 50 | 39.0 ± 15.0, 48.0 ± 13.0 | 1.5 or Less | Size 1.8 ± 0.2 cm, 2.0 ± 0.3 |
| Lee et al21 | Taiwan | Proximal | SWL-other (Lithostar® 2), flexible URS (ureteroscope, Richard Wolf) | 3 | 22, 20 | 54.2 ± 16.7, 48.5 ± 13.3 | Greater than 1.5 | Size 1.8 ± 0.4 cm, 1.8 ± 0.3 | |
| Francesca et al22 | Italy | 7 Days | Proximal/prevesical | SWL-HM3, SWL-other (PiezoLith, Richard Wolf) | 2 | 35, 35 | 2.0 or Less | Size 1.4 (0.8–2.0), 1.2 (0.8–1.7) | |
| Kidney: | |||||||||
| Yuruk et al24 | Turkey | 19.3 Mos | Lower pole | PNL (Swiss LithoClast Master), SWL-other (Dornier Compact Sigma) | 2 | 33, 33 | 44.1 ± 12.3 (24–77), 44.5 ± 9.4 (28–64) | Less than 2.0 (asymptomatic) | Burden 1.5 ± 0.4 cm2, 1.4 ± 0.7 |
| Pearle et al25 | United States + Canada | 3 Mos | Lower pole | Multiple SWL, SR/flexible URS | 3 | 39, 39 | 52.5 ± 12.3, 49.3 ± 14.2 | 1.0 or Less | Burden 0.4 ± 0.2 cm2, 0.4 ± 0.2 |
| Graber et al26 | Switzerland | 3 Mos | Pelvis | SWL-HM3, SWL-other (Lithostar Plus) | 2 | 87, 80 | 48.0 ± 16.2, 45.5 ± 15.8 | Less than 1.0 (solitary calix), less than 2.0 (renal pelvis) | Vol 0.45 ± 0.34 cm2, 0.48 ± 0.4 |
| Multiple (Chan et al23) | Canada | 3 Mos | Ureter + kidney | SWL-HM3, SWL-other (MFL 5000) | 1 | 108, 90 | (20–87), (24–79) | — |
Table 2.
Ureteral stone treatment, retreatment and complications
| No. Treatment/Total No. | No. Comparator/Total No. | RR (95% CI) | |
|---|---|---|---|
| Distal ureteral stones | |||
| Retreatment SR-URS vs SWL-other: | |||
| Verze e al14 | 10/136 | 57/137 | 0.18 (0.09–0.33) |
| Peschel et al18 | 0/40 | 4/40 | 0.20 (0.02–1.64) |
| Hendrikx et al17 | 8/87 | 31/69 | 0.20 (0.10–0.42) |
| Zeng et al15 | 4/180 | 25/210 | 0.19 (0.07–0.53) |
| Fixed effects meta-analysis | 0.14 (0.08–0.23) | ||
| Retreatment: | |||
| SR-URS vs SWL-HM316 | 0/32 | 0/32 | 1.00 (0.07–15.33) |
| SWL-other vs SWL-HM3 fixed effects model estimate indirect comparison | 5.62 (0.04–92.85) | ||
| Complications SR-URS vs SWL-other: | |||
| Verze e al14 | 26/136 | 24/137 | 1.09 (0.66–1.80) |
| Peschel et al18 | 0/40 | 0/40 | 1.00 (0.06–15.45) |
| Hendrikx et al17 | 30/87 | 14/69 | 1.70 (0.98–2.95) |
| Zeng et al15 | 12/180 | 12/210 | 1.17 (0.54–2.53) |
| Fixed effects meta-analysis | 1.28 (0.94–1.81) | ||
| Complications: | |||
| SR-URS vs SWL-HM316 | 8/32 | 3/32 | 2.67 (0.78–9.15) |
| SWL-other vs SWL-HM3 fixed effects model estimate indirect comparison | 2.26 (0.70–9.94) | ||
| Proximal ureteral stones | |||
| Retreatment: | |||
| SR-URS vs SWL-HM319 | 4/100 | 29/100 | 0.14 (0.05–0.38) |
| SWL-other vs SWL-HM322 | 27/30 | 22/27 | 1.10 (0.89–1.37) |
| SR-URS vs SWL-other fixed effects model estimate indirect comparison | 0.08 (0.02–0.32) | ||
| PNL vs SR-URS20 | 7/50 | 11/50 | 0.64 (0.27–1.51) |
| Flexible URS vs SWL-other21 | 8/19 | 7/19 | 1.14 (0.52–2.52) |
| Complications: | |||
| SR-URS vs SWL-HM319 | 13/100 | 23/100 | 0.57 (0.30–1.05) |
| SWL-other vs SWL-HM322 | 5/30 | 21/27 | 0.21 (0.09–0.49) |
| SR-URS vs SWL-other fixed effects model estimate indirect comparison | 8.71 (2.11–42.58) | ||
| PNL vs SR-URS20 | 9/50 | 0/50 | 10.00 (1.33–75.28) |
| Flexible URS vs SWL-other21 | 18/20 | 2/22 | 9.90 (2.62–37.41) |
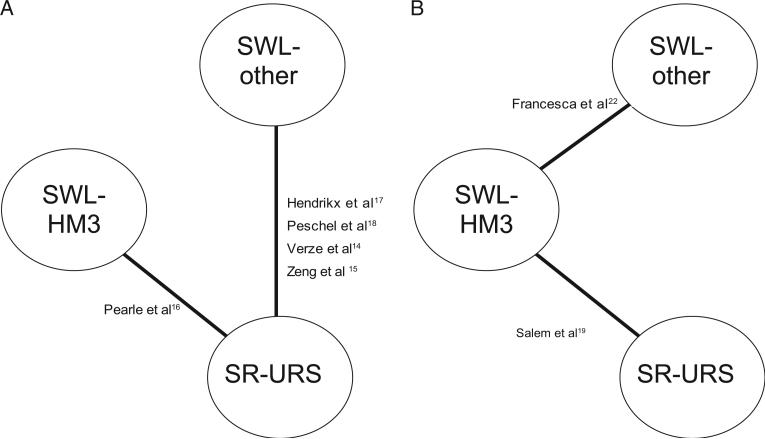
Verze,14 Zeng,15 Pearle,16 Hendrikx17 and Peschel18 et al assessed distal ureteral stone treatment. We constructed an evidence network to show different pairwise comparisons of these trials (fig. 1, A). There was direct evidence for the comparison of SR-URS vs SWL-other and SWL-HM3. There was no direct comparison of SWL-other vs SWL-HM3 but this was estimated indirectly with the available studies. The reported clinical and patient characteristics indicated that the distal ureteral stone studies reflected comparable populations (table 1).
Figure 1.
RCT network for distal (A) and proximal (B) ureteral stones
Four groups evaluated intervention for proximal ureteral stones.19–22 The evidence network shows that Francesca et al compared SWL-other with SWL-HM322 while Salem compared SR-URS with SWL-HM3.19 This allowed for an indirect comparison of SR-URS with SWL-other (fig. 1, B). The study by Lee et al comparing flexible URS with SWL-other21 and the study by Basiri et al comparing PNL with SR-URS20 were excluded from the network due to the large stone size in these populations. The series by Chan et al included stones at multiple sites but did not show results by stone location.23 Thus, this study could not be analyzed further.
Two renal stone studies included patients with stones in the lower renal pole and compared PNL with SWL-other and any URS with any SWL.24,25 These series showed differences in the average stone burden. Another study evaluated treatment of stones in the renal pelvis using SWL-other vs SWL-HM3.26 Due to the differences in clinical characteristics in the studies no quantitative comparison was done.
Study quality ranged from 1 to 3 on the scale of Jadad et al (table 1).6 While the maximum score is 5, due to the types of intervention in these studies double blinding was not feasible. Thus, the maximum possible score was 4.
Stone Treatment
Distal ureteral
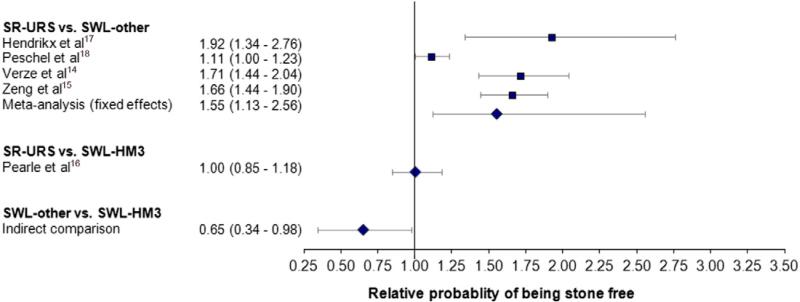
Figure 2 shows the efficacy of the evaluated interventions for distal ureteral stones based on the first reported or initial SFR. The pooled result obtained with a fixed effects model, which was considered appropriate given the goodness of fit comparisons, reflected a 55% greater probability of being stone-free with SR-URS than with SWL-other (RR 1.55). The random effects model showed a 69% greater probability of being stone-free, which was also significant. SR-URS and SWL-HM3 demonstrated a similar SFR.16 The indirect comparison of studies of SR-URS vs SWL-other and the study of SR-URS vs SWL-HM3 showed that SWL-other was 35% less efficacious than SWL-HM3 (RR 0.65).
Figure 2.
Meta-analysis of distal ureteral SFR at first available evaluation
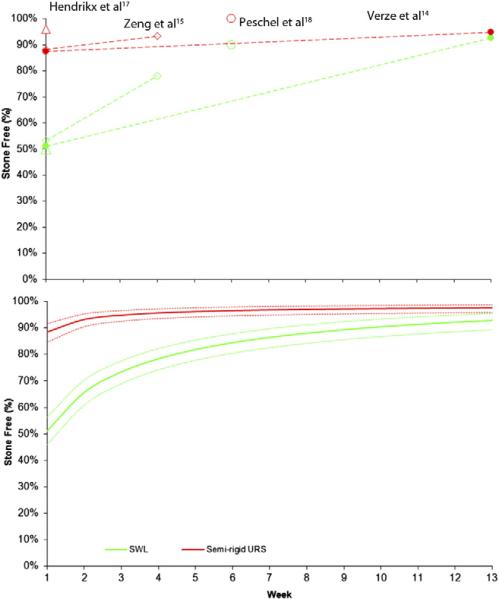
Figure 3 shows the results of the SFR meta-analysis with time between SR-URS and SWL-other. Results suggested that SR-URS is more efficacious then SWL-other for distal ureteral stones. However, with time SWL approached the SFR of SR-URS due to re-treatment of SWL cases.
Figure 3.
Meta-analysis of SR-URS vs SWL-other SFR and distal ureteral stones at all time points.
There was great variation in the reported use of auxiliary procedures across studies as a result of definitional differences. Furthermore, some studies included protocol directed auxiliary procedures.15,18 Overall SR-URS was associated with a greater rate of auxiliary procedures than SWL-other.
Patients treated with SR-URS were less likely to require re-treatment than patients treated with SWL-other for distal ureteral stones (table 2). The pooled RR indicated a sevenfold smaller re-treatment risk for SR-URS than for SWL-other (RR 0.14). A comparable number of patients experienced complications (pooled RR 1.28, 95% CI 0.94–1.81, table 2).
Proximal ureteral
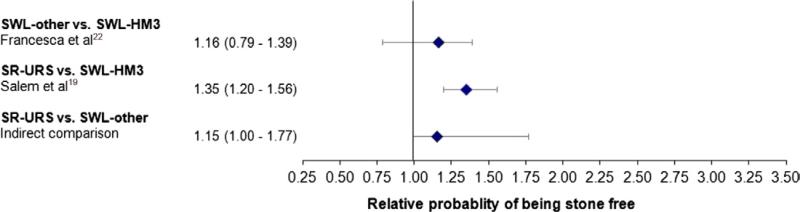
Figure 4 shows the initial SFR for proximal ureteral stone treatment. There was a 35% greater probability of being stone-free for SR-URS than for SWL-HM3 (RR 1.35) and a 15% greater probability than for SWL-other (RR 1.15). Salem reported an initial SFR of 96% for SR-URS, which increased to 100% by the 13-week followup. For SWL-HM3 the SFR increased from 71% to 96% during the 13-week followup. For large stones SFRs were similar for PNL, URS and SWL-HM3.20,21 There was no significant difference in auxiliary procedures among PNL, URS and SWL-HM3.19–21
Figure 4.
Indirect comparison of proximal ureteral SFR at first available evaluation
Patients treated with SR-URS for proximal ureteral stones required re-treatment less often than patients treated with SWL-HM3 (RR 0.14, 95% CI 0.05–0.38) or SWL-other (RR 0.08, 95% CI 0.02–0.32, table 2). There was no difference between SWL-other and SWL-HM3. The re-treatment rates for large proximal stones did not differ statistically by treatment option.20,21 Patients treated with SR-URS or SWL-other experienced less frequent complications than those treated with SWL-HM3 (table 2). Comparing the studies by Salem19 and Francesca et al22 revealed more frequent complications for SR-URS than for SWL-other. However, PNL for large proximal stones was associated with more frequent complications than SR-URS.20
Renal
Since there was insufficient data to perform a network meta-analysis for renal stones, a narrative review was done. PNL showed a 76% greater SFR than SWL-other for stones in the lower renal pole (RR 1.76, 95% CI 1.27–2.44).24 A comparison of URS with SWL for lower pole stones 1 cm or less showed no significant difference in SFR (RR 1.44, 95% CI 0.77–2.72).25 The risk of re-treatment with URS relative to SWL was comparable (RR 1.22, 95% CI 0.22–6.76).
Treatment of stones in the renal pelvis with SWLHM3 showed a 40% greater initial SFR than SWL-other (relative probability 1.40, 95% CI 1.18–1.67).26 At 3 months no difference was observed in the SFR (relative probability 1.02, 95% CI 0.90–1.15). SWL-other had a greater complication and re-treatment risk than SWL-HM3.
DISCUSSION
Systematic reviews of RCTs are valuable since they inform evidence-based health care decision making and the development of clinical treatment guidelines. Stone disease has many possible treatments, which makes comparative efficacy assessment particularly important. One of the first comparative assessments of ureteral calculi was the 1997 AUA Ureteral Stones Clinical Guidelines Panel summary report.27 At that time the panel stated that the quality of the reviewed literature was so poor that no recommendations could be made without including retrospective clinical case series. The panel ultimately concluded that SWL was first line treatment for stones 1 cm or less in the proximal ureter while stones in the distal ureter could be treated with SWL or URS.
Recognizing the intervening publication of several new RCTs since the guidelines panel summary,27 in 2007 the Cochrane Collaboration4 and the EAU/AUA Nephrolithiasis Guideline Panel28 provided systematic reviews and meta-analyses of ureteral calculus management. The Cochrane Collaboration indicated that URS was associated with a superior SFR but complications and hospitalization were also greater for the URS cohorts.4 However, overall the quality of evidence was poor and further studies were required to better define optimal treatment practices. This review had several design limitations, including the fact that no distinction was made between SWL done with the HM3 lithotripter and other devices. Based on observational data it is a generally accepted tenet that the HM3 is associated with significantly greater treatment success than subsequent lithotripters. Our indirect comparison also showed that the HM3 had results superior to those of other SWL devices for distal stones.
The recent RCT by Zehnder et al comparing the HM3 to the Modulith® SLX-F2 SWL device confirmed that the older HM3 device has better outcomes.29 That study was published too late to be included in our meta-analysis. Also, the Cochrane Review did not account for stone location, which is also a significant predictor URS success.4 In contrast, the EAU/AUA panel analysis was done according to stone site but it also did not account for the different generations of SWL devices used in the source studies, ie SWL-HM3 vs SWL-other.28 The EAU/AUA panel ultimately found that for patients with ureteral stones URS was associated with a greater SFR and this finding was particularly pronounced in the distal ureter. However, the EUA/AUA panel and the Cochrane Collaboration4 recommended that additional RCTs should be done to improve practice guidelines.
In an ideal system robust RCTs would simultaneously compare all interventions of interest. In the realm of stone disease such a trial would incorporate URS, SWL and PNL. However, since such studies are not readily available, indirect comparisons among studies can provide useful evidence. In our analysis the results of multiple RCTs were used to directly and/or indirectly compare treatments to each other in a network meta-analysis. We assessed unambiguous metrics associated with surgical stone treatment, which allowed the most equitable comparisons among treatment modalities, including SFR, retreatment procedures and surgical complications. However, this systematic literature search was limited to the published English language literature. Thus, unpublished conference abstracts, which may not have been published due to publication bias, would have been excluded from analysis.
Our network meta-analysis of patients with distal ureteral calculi showed that URS has advantages over SWL. Immediately after treatment URS was significantly superior to SWL in regard to SFR. However, that difference became smaller with time, which was a consequence of re-treatments. To that end when comparing the SWL and URS cohorts, patients initially treated with URS required fewer re-treatment procedures. In some regards our findings are not surprising or unexpected. The EAU/AUA Panel also reported that URS for distal ureteral calculi was associated with a greater SFR.28 As in the EAU/AUA analysis, in our series source studies were geographically diverse and likely included surgeons with varying skills and technology.
What may be as important as our mentioned findings on distal ureteral calculi is our inability to draw meaningful conclusions when assessing studies of proximal ureteral and renal calculi. Of the literature searched only 4 RCTs were identified for proximal ureteral calculi,19–22 of which 2 were restricted to a stone burden of 1.5 to 2 cm, much larger than the size stone routinely encountered in practice.20,21 The other 2 studies also included patients with renal stones with such great variability in clinical characteristics and outcome metrics that meaningful comparisons were not possible.19,22
Going forward, what is most needed to better elucidate the optimal treatment approaches to proximal ureteral and renal calculi are robustly designed RCTs. However, given the relative scarcity of such studies in the previous decade, it is unlikely that a significant number of these studies will rapidly populate the medical literature in the coming years. In the absence of such studies the next level of appropriate evidence would be well designed observational studies. Our review identified that there is no uniform approach to defining preoperative stone size or location, associated ancillary treatments or even the stone-free outcome. To maximize the benefit of observational studies it is important to develop a commonly accepted terminology that will best permit a comparison of interventions for stone disease.
CONCLUSIONS
Our systematic review and meta-analysis confirm that for patients with distal ureteral calculi URS is associated with a significantly greater SFR and fewer required re-treatment. Currently published RCTs do not permit any conclusions to be drawn on the most efficacious approach to proximal ureteral or renal calculi. The ideal resolution would be well designed RCTs. In the absence of such studies a greater degree of uniformity in terminology and outcomes would improve the usefulness of comparing observational studies.
ACKNOWLEDGMENTS
Chizanya Mpinja, Mapi Group, provided assistance.
Supported by Boston Scientific.
Abbreviations and Acronyms
- AUA
American Urological Association
- EAU
European Association of Urology
- PNL
percutaneous nephrolithotomy
- RCT
randomized, controlled trial
- SFR
stone-free rate
- SR
semirigid
- SWL
shock wave lithotripsy
- URS
ureteroscopy
REFERENCES
- 1.Stamatelou KK, Francis ME, Jones CA, et al. Time trends in reported prevalence of kidney stones in the United States: 1976–1994. Kidney Int. 2003;63:1817. doi: 10.1046/j.1523-1755.2003.00917.x. [DOI] [PubMed] [Google Scholar]
- 2.Pearle MS, Calhoun EA, Curhan GC. Urologic Diseases in America project: urolithiasis. J Urol. 2005;173:848. doi: 10.1097/01.ju.0000152082.14384.d7. [DOI] [PubMed] [Google Scholar]
- 3.Matlaga BR. Contemporary surgical management of upper urinary tract calculi. 2007 guideline for the management of ureteral calculi. J Urol. 2009;1181:2152. doi: 10.1016/j.juro.2009.01.023. [DOI] [PubMed] [Google Scholar]
- 4.Nabi G, Downey P, Keeley F, et al. Extra-corporeal shock wave lithotripsy (ESWL) versus ureteroscopic management for ureteric calculi. Cochrane Database Syst Rev. 2007:CD006029. doi: 10.1002/14651858.CD006029.pub2. [DOI] [PubMed] [Google Scholar]
- 5.Preminger GM, Tiselius HG, Assimos DG, et al. Guideline for the management of ureteral calculi. Eur Urol. 2007;2007;52:1610. doi: 10.1016/j.eururo.2007.09.039. [DOI] [PubMed] [Google Scholar]
- 6.Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17:1. doi: 10.1016/0197-2456(95)00134-4. [DOI] [PubMed] [Google Scholar]
- 7.Lu G, Ades AE. Combination of direct and indirect evidence in mixed treatment comparisons. Stat Med. 2004;23:3105. doi: 10.1002/sim.1875. [DOI] [PubMed] [Google Scholar]
- 8.Caldwell DM, Ades AE, Higgins JP. Simultaneous comparison of multiple treatments: combining direct and indirect evidence. BMJ. 2005;331:897. doi: 10.1136/bmj.331.7521.897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jansen JP, Fleurence R, Devine B, et al. Interpreting indirect treatment comparisons and network meta-analysis for health-care decision making: report of the ISPOR Task Force on Indirect Treatment Comparisons Good Research Practices: part 1. Value Health. 2011;14:417. doi: 10.1016/j.jval.2011.04.002. [DOI] [PubMed] [Google Scholar]
- 10.Hoaglin DC, Hawkins N, Jansen JP, et al. Conducting indirect-treatment-comparison and network-meta-analysis studies: report of the ISPOR Task Force on Indirect Treatment Comparisons Good Research Practices: part 2. Value Health. 2011;14:429. doi: 10.1016/j.jval.2011.01.011. [DOI] [PubMed] [Google Scholar]
- 11.Ouwens M, Philips Z, Jansen JP. Network meta-analysis of parametric survival curves. Res Synthesis Meth. 2010;1:258. doi: 10.1002/jrsm.25. [DOI] [PubMed] [Google Scholar]
- 12.Spiegelhalter DJ, Best NG, Carlin BP, et al. Bayesian measures of model complexity and fit. J R Stat Soc Series B Stat Methodol. 2002;64:583. [Google Scholar]
- 13.Spiegelhalter D, Thomas A, Best N, et al. Win-BUGS User Manual: Version 1.4. MRC Biostatistics Unit; Cambridge, United Kingdom: 2003. [Google Scholar]
- 14.Verze P, Imbimbo C, Cancelmo G, et al. Extracorporeal shockwave lithotripsy vs ureteroscopy as first-line therapy for patients with single, distal ureteric stones: a prospective randomized study. BJU Int. 2010;106:1748. doi: 10.1111/j.1464-410X.2010.09338.x. [DOI] [PubMed] [Google Scholar]
- 15.Zeng GQ, Zhong WD, Cai YB, et al. Extracorporeal shock-wave versus pneumatic ureteroscopic lithotripsy in treatment of lower ureteral calculi. Asian J Androl. 2002;4:303. [PubMed] [Google Scholar]
- 16.Pearle MS, Nadler R, Bercowsky E, et al. Prospective randomized trial comparing shock wave lithotripsy and ureteroscopy for management of distal ureteral calculi. J Urol. 2001;166:1255. [PubMed] [Google Scholar]
- 17.Hendrikx AJ, Strijbos WE, de Knijff DW, et al. Treatment for extended-mid and distal ureteral stones: SWL or ureteroscopy? Results of a multicenter study. J Endourol. 1999;13:727. doi: 10.1089/end.1999.13.727. [DOI] [PubMed] [Google Scholar]
- 18.Peschel R, Janetschek G, Bartsch G. Extracorporeal shock wave lithotripsy versus ureteroscopy for distal ureteral calculi: a prospective randomized study. J Urol. 1999;162:1909. doi: 10.1016/S0022-5347(05)68066-4. [DOI] [PubMed] [Google Scholar]
- 19.Salem HK. A prospective randomized study comparing shock wave lithotripsy and semirigid ureteroscopy for the management of proximal ureteral calculi. Urology. 2009;74:1216. doi: 10.1016/j.urology.2009.06.076. [DOI] [PubMed] [Google Scholar]
- 20.Basiri A, Simforoosh N, Ziaee A, et al. Retrograde, antegrade, and laparoscopic approaches for the management of large, proximal ureteral stones: a randomized clinical trial. J Endourol. 2008;22:2677. doi: 10.1089/end.2008.0095. [DOI] [PubMed] [Google Scholar]
- 21.Lee YH, Tsai JY, Jiaan BP, et al. Prospective randomized trial comparing shock wave lithotripsy and ureteroscopic lithotripsy for management of large upper third ureteral stones. Urology. 2006;67:480. doi: 10.1016/j.urology.2005.09.067. [DOI] [PubMed] [Google Scholar]
- 22.Francesca F, Grasso M, Da Pozzo L, et al. Ureteral lithiasis: in situ piezoelectric versus in situ spark gap lithotripsy. A randomized study. Arch Esp Urol. 1995;48:760. [PubMed] [Google Scholar]
- 23.Chan SL, Stothers L, Rowley A, et al. A prospective trial comparing the efficacy and complications of the modified Dornier HM3 and MFL 5000 lithotriptors for solitary renal calculi. J Urol. 1995;153:1794. [PubMed] [Google Scholar]
- 24.Yuruk E, Binbay M, Sari E, et al. A prospective, randomized trial of management for asymptomatic lower pole calculi. J Urol. 2010;183:1424. doi: 10.1016/j.juro.2009.12.022. [DOI] [PubMed] [Google Scholar]
- 25.Pearle MS, Lingeman JE, Leveillee R, et al. Prospective randomized trial comparing shock wave lithotripsy and ureteroscopy for lower pole caliceal calculi 1 cm or less. J Urol, suppl. 2008;179:S69. doi: 10.1016/j.juro.2008.03.140. [DOI] [PubMed] [Google Scholar]
- 26.Graber SF, Danuser H, Hochreiter WW, et al. A prospective randomized trial comparing 2 lithotriptors for stone disintegration and induced renal trauma. J Urol. 2003;169:54. doi: 10.1016/S0022-5347(05)64033-5. [DOI] [PubMed] [Google Scholar]
- 27.Segura JW, Preminger GM, Assimos DG, et al. Ureteral Stones Clinical Guidelines Panel summary report on the management of ureteral calculi. American Urological Association. J Urol. 1997;158:1915. doi: 10.1016/s0022-5347(01)64173-9. [DOI] [PubMed] [Google Scholar]
- 28.Preminger GM, Tiselius HG, Assimos DG, et al. Guideline for the management of ureteral calculi. J Urol. 2007;2007;178:2418. doi: 10.1016/j.juro.2007.09.107. [DOI] [PubMed] [Google Scholar]
- 29.Zehnder P, Roth B, Birkhauser F, et al. A prospective randomised trial comparing the modified HM3 with the MODULITH(R) SLX-F2 lithotripter. Eur Urol. 2011;59:637. doi: 10.1016/j.eururo.2011.01.026. [DOI] [PubMed] [Google Scholar]