Abstract
Objective:
To assess the impact of mammography capacity on appointment wait times.
Methods:
We surveyed by telephone all mammography facilities federally certified in 2008 in California, Connecticut, Georgia, Iowa, New Mexico and New York using a simulated-patient format. County-level mammography capacity, defined as the number of mammography machines per 10,000 women age 40 and older, was estimated from FDA facility certification records and US Census data.
Results:
1,614 (86%) of 1,882 mammography facilities completed the survey. Time until next available screening mammogram appointment was <1 week at 55% of facilities, 1-4 weeks at 34% of facilities, and >1 month at 11% of facilities. Facilities in counties with lower capacity had longer wait times, and a one-unit increase in county capacity was associated with 21% lower odds of a facility reporting a wait time >1 month (p<0.01). There was no association between wait time and the availability of evening or weekend appointments or digital mammography. Conclusion: Lower mammography capacity is associated with longer wait times for screening mammograms.
Impact:
Enhancement of mammography resources in areas with limited capacity may reduce wait times for screening mammogram appointments, thereby increasing access to services and rates of breast cancer screening.
BACKGROUND
In randomized controlled trials, screening mammography has been shown to reduce breast cancer mortality, particularly among women age 50 to 69.[1] Despite the well publicized benefits of screening, about one-third of US women age 40 and older report having no recent mammogram, and this proportion varies widely by state.[2, 3] After increasing for 25 years, screening mammography rates have declined. From 2000 to 2005, two national surveys found a significant decrease in the percentage of women age 40 and older who reported having a mammogram in the past two years.[4, 5] In addition, about 20% of women with a history of breast cancer do not adhere with guidelines for follow-up mammography.[6, 7]
Access to screening has been a particular concern in the US since the passage of the Mammography Quality Standards Act (MQSA) which established national uniform quality standards for mammography. The law requires certification of facilities by the US Food and Drug Administration (FDA) which enforces the MQSA and has authority to revoke certification from noncompliant facilities.[8] The MQSA has been credited with improvements in mammography quality, but its impact on access is uncertain.[9, 10] While prior reports suggest that overall mammography capacity in the US is large enough to meet existing needs, it is not clear whether resources are distributed proportionally to the population.[11, 12] Notably, facility closures in the 1990s may have disproportionately affected areas with substantial minority or rural populations.[13, 14]
Recent research suggests that women in counties with lower mammography capacity are less likely to have had a recent mammogram.[15] Several mechanisms may explain this relationship. In counties with limited capacity, long travel distances may be an impediment for women who live far from the nearest mammography facility. Alternatively, if demand for mammography exceeds the supply, then all women in low-capacity areas will face longer appointment wait times, regardless of geographic proximity.
Given the declines in screening and financial pressures facing mammography facilities,[16] it is especially critical to understand how the availability of mammography resources affects access and utilization. Our objective was to assess the impact of mammography capacity on appointment wait times.
METHODS
Sample
We identified all mammography facilities in California, Connecticut, Georgia, Iowa, New Mexico and New York that were legally certified to operate as of January 1, 2008. In accordance with the MQSA, the FDA has maintained administrative records on all mammography facilities in the US since 1994, including street addresses and dates of certification. All certified facilities in each state were contacted for the study.
Survey
The survey was administered by telephone using a simulated-patient format. One investigator (JGS) called each facility, stating that she recently celebrated her 40th birthday and was inquiring about scheduling a baseline screening mammogram. She asked about time until the next available screening mammogram appointment, availability of evening and weekend appointments, availability of digital mammography, insurance copayment requirements, and the method and time by which mammogram results would be delivered. Open-ended responses were recorded by the interviewer using standardized response categories (see survey instrument in Appendix). The study was reviewed by the Institutional Review Board at Memorial Sloan-Kettering Cancer Center and deemed exempt from informed consent requirements.
Mammography Capacity
For every county in the US (n=3,140), we estimated mammography capacity as the number of mammography machines per 10,000 women age 40 and older in 2007. Age-specific female population counts in 2007 were obtained from intercensal population estimates produced by the US Census Bureau. Machine counts were from annual facility inspection reports. Mammography capacity in 2007 included only machines at facilities whose FDA certification was effective for the entire year. Mobile facilities were assigned to the county of their mailing address.
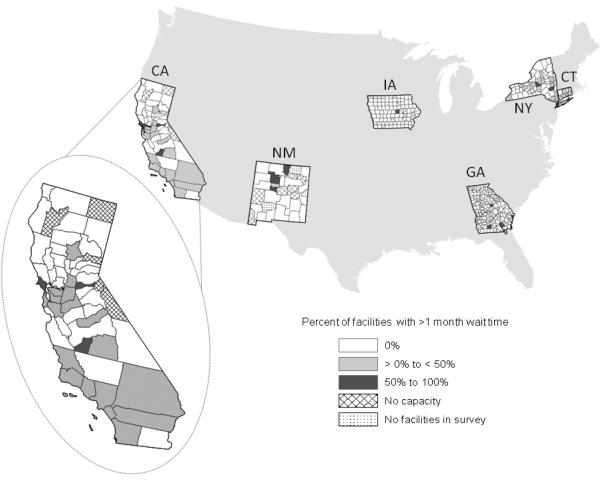
To illustrate the geographic distribution of appointment wait times, we created choropleth maps depicting the percent of facilities in a county with a wait time greater than 1 month (0, >0 to <50% of facilities, >50% of facilities in the county). For this county-level estimate, the denominator included only facilities that completed the survey. All facilities were georeferenced by street address, and all maps were created in ArcGIS (Version 9.2, ESRI, Redlands, California).
Statistical Analysis
In descriptive analysis, wait time for the next available appointment was categorized as <1 week, 1-4 weeks, 1-2 months or 3 months or longer. Time until notification of mammogram results was classified by recipient (patient or referring physician) and finding (normal vs. abnormal result). Relationships between facility characteristics and appointment wait times were assessed using chi-square tests. The relationship between county mammography capacity and appointment wait time was evaluated using multinomial logistic regression, with wait time categorized as <1 week, 1-4 weeks or >1 month until the next available appointment. We used generalized estimating equations with a logit link function to account for the correlation between facilities within the same county.[17] All statistical analyses were performed in SAS version 9.2 (SAS Institute, Cary, NC).
RESULTS
Of the 1,882 FDA-certified mammography facilities in the six states in 2008, 1,614 (86%) were successfully contacted by telephone and participated in the survey. Facility participation varied by state from 77% (CA) to 95% (CT and NY) (Table 1). Overall, 55% of facilities reported appointment wait time of less than one week for screening mammography, varying from 51% (CA and NY) to 78% (IA). Wait times of 1-2 months were reported by 1% (IA) to 13% (NM) of facilities. In most states few facilities reported a wait for next available screening mammogram appointment of 3 months or longer, with NY reporting the highest rate of this outcome (5%). Availability of evening or weekend appointments varied from 21% of facilities in NM to 50% in CT. Availability of digital mammography varied from 31% in NM to 70% in CT. Neither the availability of evening or weekend appointments or of digital mammography was associated with appointment wait times.
Table 1.
Mammography facility survey responses by state, 2008
| Percent of Facilities | ||||||
|---|---|---|---|---|---|---|
| State | CA | CT | GA | IA | NM | NY |
| Total facilities | 726 | 137 | 245 | 144 | 46 | 584 |
| Facilities in survey | 556 | 130 | 202 | 134 | 39 | 553 |
| Survey participation | 77% | 95% | 82% | 93% | 85% | 95% |
| Next available appointment | ||||||
| Less than 1 week | 51% | 57% | 61% | 78% | 67% | 51% |
| 1 to 4 weeks | 38% | 31% | 36% | 22% | 20% | 34% |
| 1 to 2 months | 8% | 10% | 3% | 1% | 13% | 10% |
| 3 months or longer | 3% | 2% | <1% | 0% | 0% | 5% |
| Evening/weekend appointments | ||||||
| Yes | 26% | 50% | 23% | 25% | 21% | 47% |
| No | 74% | 50% | 77% | 75% | 80% | 53% |
| Digital mammography | ||||||
| Yes or in process | 50% | 70% | 48% | 42% | 31% | 62% |
| No | 50% | 30% | 52% | 58% | 69% | 38% |
| Payment required at visit | ||||||
| Yes | 1% | 2% | 1% | 0% | 3% | 2% |
| No | 99% | 98% | 99% | 100% | 97% | 98% |
| Patient notified of result | ||||||
| By radiologist | 87% | 91% | 90% | 96% | 72% | 87% |
| By ordering MD only | 13% | 9% | 10% | 4% | 28% | 13% |
| Notification of normal finding | ||||||
| Within 1 week of mammogram | 59% | 72% | 61% | 82% | 72% | 80% |
| >1 week after mammogram | 38% | 20% | 36% | 18% | 26% | 16% |
| Missing | 3% | 8% | 3% | 0% | 3% | 4% |
| Notification method, normal | ||||||
| Phone | <1% | 2% | 1% | 0% | 4% | 1% |
| 96% | 92% | 96% | 98% | 96% | 74% | |
| Phone and mail | <1% | 1% | 2% | 0% | 0% | 0% |
| In person | 3% | 5% | 1% | 2% | 0% | 25% |
| Notification of abnormal finding | ||||||
| Within 1 week of mammogram | 65% | 90% | 67% | 87% | 74% | 88% |
| >1 week after mammogram | 35% | 8% | 32% | 13% | 26% | 11% |
| Missing | <1% | 2% | <1% | 0% | 0% | <1% |
| Notification method, abnormal | ||||||
| Phone | 15% | 59% | 16% | 19% | 14% | 20% |
| 81% | 22% | 81% | 79% | 86% | 55% | |
| Phone and mail | <1% | 11% | 2% | 0% | 0% | 1% |
| In person | 3% | 8% | 1% | 2% | 0% | 24% |
Most facilities (72% in NM to 96% in IA) reported that the patient would receive results directly from the facility. Four percent (IA) to 28% (NM) of facilities said that the ordering physician, but not the patient, would be notified directly by the facility. In all states but NM, notification of normal findings was more likely to occur within a week of the mammogram visit than notification of abnormal findings. In CA, GA and NM, a quarter to more than a third of facilities reported notification times of longer than one week for normal or abnormal findings. Notification of normal findings was conducted by mail at more than 90% of facilities, except in NY, where a quarter of facilities stated that the patient would be notified in person at the time of the mammogram. Notification of abnormal findings was conducted by telephone in 14% (NM) to 59% (NM) of facilities, but mail notification remained the standard method for abnormal results as well as normal results, in all states except for CT.
Median county mammography capacity was lowest in CA (1.46 machines per 10,000 women age 40 and older) and greatest in Iowa (2.96 machines per 10,000) (Table 2). Across all six states, there were mammography facilities in 339 of 419 counties and 80 counties with no facility (Figure 1). In 265 counties of those with any mammography facility, no facilities reported wait times greater than one month. In 52 counties fewer than 50% of facilities reported wait times longer than one month, and in 12 counties at least 50% of facilities reported wait times longer than one month. In California, the three counties with more than 50% of facilities reporting wait times longer than one month were Amador (1 facility in county; 10,113 women age 40+), Kings (3 facilities; 22,269 women age 40+) and Marin (5 facilities; 74,607 women age 40+).
Table 2.
County-level mammography capacity and wait times for screening mammogram by state, 2008
| Number of Counties | ||||||
|---|---|---|---|---|---|---|
| State | CA | CT | GA | IA | NM | NY |
| Total | 58 | 8 | 159 | 99 | 33 | 62 |
| Facilities in county with wait time >1 month |
||||||
| 0% | 31 | 2 | 94 | 84 | 19 | 35 |
| >0% - <50% | 19 | 6 | 3 | 0 | 1 | 23 |
| ≥50% | 3 | 0 | 3 | 1 | 3 | 2 |
| No facilities completing survey | 0 | 0 | 5 | 2 | 3 | 0 |
| No mammography facilities | 5 | 0 | 54 | 12 | 7 | 2 |
| Median county mammography capacity* |
1.46 | 1.85 | 2.02 | 2.96 | 1.62 | 1.80 |
County mammography capacity = number of mammography machines per 10,000 women age 40+
Fig 1.
Time to next screening mammogram appointment in California, Connecticut, Georgia, Iowa, New Mexico and New York, 2008
Maps depict the percent of facilities in each county with wait time of greater than 1 month for next available screening mammogram appointment. All states shown in US map, with enlarged view of California.
Among facilities reporting a wait of <1 week for the next available screening appointment, median county mammography capacity was 1.74 machines per 10,000 adult women. Facilities with appointment wait times of 1-4 weeks and >1 month were in counties with lower median capacity: 1.65 and 1.58 machines per 10,000, respectively. There was a statistically significant inverse relationship between county mammography capacity and appointment wait time. Exponentiating the parameter estimate of −0.23 (95%CI: −0.39 to −0.08, p<0.01) from a multinomial logistic regression, a one-unit increase in capacity was associated with 21% lower odds of a facility reporting a wait time >1 month for the next available appointment (compared with <1 week and 1-4 weeks).
DISCUSSION
Despite evidence of efficacy and endorsement from numerous organizations, screening mammography rates in the US declined in the past decade and still fall short of the 70% Healthy People 2010 target.[2] We previously found a positive association between the use of screening mammography and the availability of mammography machines.[18] In the current survey of more than 1,600 facilities in six states, facilities in counties with lower mammography capacity were more likely to report longer times until the next available appointment for a screening mammogram.
Our findings support a conceptual model in which resource capacity influences resource utilization through the relationship between supply and demand. In areas with lower mammography capacity, the demand for appointments exceeds the supply of appointments by a greater margin, and this difference likely creates longer appointment wait times. Our results do not exclude the possibility that longer travel distances also contribute to the relationship between resource capacity and utilization, although evidence for this association is mixed.[19-22] However, our results suggest that efforts to increase screening rates by reducing travel time or distance alone – by expanding the reach of mobile mammography units, for example – may not be effective if appointment wait times remain long due to limited capacity.
Of course, mammography capacity is not solely a function of the number of machines. Human resources, specifically the radiologic technologists who operate the machines and the radiologists who interpret the images, influence the overall availability of mammograms. Shortages of qualified radiologists and mammographic technologists have been reported in the past decade.[16, 23, 24] It is not clear whether efforts to increase the number of mammography machines or policies that enhance the supply of radiologists and technologists or facilitate image interpretation by radiologists at geographically remote sites will have the greatest impact on screening rates.
It is somewhat concerning that 12% of all facilities reported that the patient would receive mammogram results from the ordering physician but not directly from the facility. The MQSA requires that every patient receive a written report of results within 30 days of her mammogram. Although the simulated-patient format of the survey limited our ability to probe respondents for detailed explanations of their procedures or to verify responses with a facility director, our findings with regard to the reporting of mammogram results suggest that monitoring of adherence with this MQSA requirement may be warranted.
Both our survey and the trend of declining utilization of screening mammography preceded the US Preventive Services Task Force’s (USPSTF) change in breast cancer screening recommendations. In November, 2009, the USPSTF questioned the value of screening for women in their 40s, suggesting that at both population and individual levels the expected benefits of routine screening mammography might not exceed the potential harms, and advised women in this age group to make personalized screening decisions in partnership with their physicians. Before 2009 the trend of declining mammography utilization seemed to be reversing, with screening rates increasing slightly between 2005 and 2008.[2] It may be too soon to tell whether the USPSTF’s guideline revision or increasing recognition of the potential harms of radiation[25] has influenced screening mammography rates or mammography capacity.
Several limitations should be noted. Our data reflect the experience of mammography facilities in six states at one point in time. While results may not be generalizable to the entire country, the selected states are heterogenous in size, population density, geographic location and population characteristics. Thus our findings likely represent the experience of a wide cross section of facilities and health care markets. Information collected in our survey was reported by facility receptionists and schedulers, responding to inquires from a trained research assistant scheduling a baseline screening mammogram. In this context we could not assess the validity of responses, for example, by comparing reported wait times with facility logs or supervising administrative staff. Finally, mammography capacity was defined at the county level, although women may seek health care services outside their county of residence.
In a climate of economic uncertainty and severe fiscal constraints at federal, state and local levels, public health budgets are vulnerable. Results of this study combined with prior evidence of the relationship between mammography capacity and utilization suggest that efforts to reduce appointment wait times may improve screening mammography rates. Therefore, policies or programs to reduce appointment wait times may be most cost-effective if they target areas with limited mammography capacity. In the face of limited resources, these areas can be prioritized for efforts to improve adherence with cancer screening recommendations.
Funding Acknowledgement
This work was supported by grants from Susan G. Komen for the Cure (POP107806, PI: Elkin), the American Cancer Society (MRSG-06-127-01-CPHPS, PI: Elkin) and the National Cancer Institute (K07-CA118189, PI: Elkin).
Footnotes
Conflict of Interest Disclosure
The authors declare that they have no conflict of interest.
REFERENCES
- 1.Freedman DA, Petitti DB, Robins JM. On the efficacy of screening for breast cancer. International Journal of Epidemiology. 2004;33:43–55. doi: 10.1093/ije/dyg275. [DOI] [PubMed] [Google Scholar]
- 2.Breen N, Gentleman JF, Schiller JS. Update on mammography trends: comparisons of rates in 2000, 2005, and 2008. Cancer. 2010 doi: 10.1002/cncr.25679. 10.1002/cncr.25679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Miller JW, King JB, Ryerson AB, Eheman CR, White MC. Mammography use from 2000 to 2006: state-level trends with corresponding breast cancer incidence rates. AJR Am J Roentgenol. 2009;192:352–60. doi: 10.2214/ajr.08.1757. 192/2/352 [pii] 10.2214/AJR.08.1757. [DOI] [PubMed] [Google Scholar]
- 4.Use of mammograms among women aged >/= 40 years--United States, 2000-2005. MMWR Morb Mortal Wkly Rep. 2007;56:49–51. [PubMed] [Google Scholar]
- 5.Breen N, A.K. C, Meissner HI, Taplin SH, Tangka FK, Tiro JA, et al. Reported drop in mammography: is this cause for concern? Cancer. 2007;109:2405–9. 10.1002/cncr.22723. doi: 10.1002/cncr.22723. [DOI] [PubMed] [Google Scholar]
- 6.Geller BM, Kerlikowske K, Carney PA, Abraham LA, Yankaskas BC, Taplin S, et al. Mammography surveillance following breast cancer. Breast Cancer Res Treat. 2003;81:107–15. doi: 10.1023/A:1025794629878. [DOI] [PubMed] [Google Scholar]
- 7.Keating NL, Landrum MB, Guadagnoli E, Winer EP, Ayanian JZ. Factors related to underuse of surveillance mammography among breast cancer survivors. J Clin Oncol. 2006;24:85–94. doi: 10.1200/JCO.2005.02.4174. [DOI] [PubMed] [Google Scholar]
- 8.Mammography Quality Standards Act (1992) and Reauthorizations (1998, 2004) 1992.
- 9.U.S. General Accounting Office . Mammography Services: Impact of Federal Legislation on Quality, Access and Health Outcomes. U.S. General Accounting Office; Washington, DC: 1997. Report No.: GAO/HEHS-98-11. [Google Scholar]
- 10.U.S. General Accounting Office . Mammography Quality Standards Act: X-ray Quality Improved, Access Unaffected, but Impact on Health Outcomes Unknown. U.S. General Accounting Office; Washington, DC: 1998. Report No.: GAO/T-HEHS-98-164. [Google Scholar]
- 11.U.S. Government Accountability Office . Mammography: Capacity Generally Exists to Deliver Services. U.S. General Accounting Office; Washington, DC: 2002. Report No.: GAO-02-532. [Google Scholar]
- 12.U.S. Government Accountability Office . Mammography: Current Nationwide Capacity is Adequate, But Access Problems May Exist in Certain Locations. U.S. General Accounting Office; Washington, DC: 2006. Report No.: GAO-06-724. [Google Scholar]
- 13.Fischer R, Houn F, Van De Griek A, Tucker SA, Meyers D, Murphy M, et al. The impact of the Mammography Quality Standards Act on the availability of mammography facilities. Preventive Medicine. 1998;27:697–701. doi: 10.1006/pmed.1998.0347. [DOI] [PubMed] [Google Scholar]
- 14.Korn JE, Casey-Paal A, Lazovich D, Ball J, Slater JS. Impact of the Mammography Quality Standards Act on access in Minnesota. Public Health Rep. 1997;112:142–5. [PMC free article] [PubMed] [Google Scholar]
- 15.Elkin EB, Ishill NM, Snow JG, Panageas KS, Bach PB, Liberman L, et al. Geographic access and the use of screening mammography. Med Care. 2010;48:349–56. doi: 10.1097/MLR.0b013e3181ca3ecb. 10.1097/MLR.0b013e3181ca3ecb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Farria DM, Schmidt ME, Monsees BS, Smith RA, Hildebolt C, Yoffie R, et al. Professional and economic factors affecting access to mammography: a crisis today, or tomorrow? Results from a national survey. Cancer. 2005;104:491–8. doi: 10.1002/cncr.21304. [DOI] [PubMed] [Google Scholar]
- 17.Hanley JA, Negassa A, Edwardes MD, Forrester JE. Statistical analysis of correlated data using generalized estimating equations: an orientation. Am J Epidemiol. 2003;157:364–75. doi: 10.1093/aje/kwf215. [DOI] [PubMed] [Google Scholar]
- 18.Elkin EB, Ishill NM, Snow JG, Panageas KS, Bach PB, Liberman L, et al. Geographic access and the use of screening mammography. Med Care. 2010 doi: 10.1097/MLR.0b013e3181ca3ecb. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Elting LS, Cooksley CD, Bekele BN, Giordano SH, Shih YC, Lovell KK, et al. Mammography capacity impact on screening rates and breast cancer stage at diagnosis. Am J Prev Med. 2009;37:102–8. doi: 10.1016/j.amepre.2009.03.017. S0749-3797(09)00296-7 [pii] 10.1016/j.amepre.2009.03.017. [DOI] [PubMed] [Google Scholar]
- 20.Jackson MC, Davis WW, Waldron W, McNeel TS, Pfeiffer R, Breen N. Impact of geography on mammography use in California. Cancer Causes Control. 2009;20:1339–53. doi: 10.1007/s10552-009-9355-6. 10.1007/s10552-009-9355-6. [DOI] [PubMed] [Google Scholar]
- 21.Marchick J, Henson DE. Correlations between access to mammography and breast cancer stage at diagnosis. Cancer. 2005;103:1571–80. doi: 10.1002/cncr.20915. 10.1002/cncr.20915. [DOI] [PubMed] [Google Scholar]
- 22.Mobley LR, Kuo TM, Driscoll D, Clayton L, Anselin L. Heterogeneity in mammography use across the nation: separating evidence of disparities from the disproportionate effects of geography. Int J Health Geogr. 2008;7:32. doi: 10.1186/1476-072X-7-32. 1476-072X-7-32 [pii] 10.1186/1476-072X-7-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.D’Orsi C, Tu SP, Nakano C, Carney PA, Abraham LA, Taplin SH, et al. Current realities of delivering mammography services in the community: do challenges with staffing and scheduling exist? Radiology. 2005;235:391–5. doi: 10.1148/radiol.2352040132. 2352040132 [pii] 10.1148/radiol.2352040132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sunshine JH, Maynard CD. Update on the diagnostic radiology employment market: findings through 2007-2008. J Am Coll Radiol. 2008;5:827–33. doi: 10.1016/j.jacr.2008.02.007. S1546-1440(08)00089-6 [pii] 10.1016/j.jacr.2008.02.007. [DOI] [PubMed] [Google Scholar]
- 25.Yaffe MJ, Mainprize JG. Risk of radiation-induced breast cancer from mammographic screening. Radiology. 2011;258:98–105. doi: 10.1148/radiol.10100655. radiol.10100655 [pii] 10.1148/radiol.10100655. [DOI] [PubMed] [Google Scholar]