In 2005, Vitaliano et al.1 called in the American Journal of Geriatric Psychiatry for more caregiver research in geriatric psychiatry. Since 2005, caregiver outcomes have been addressed in more than 800 studies and reviews. This great outpouring of research reflects the perceived need for caregiver support that will inevitably accompany the vast increase in size of the older adult population in coming decades. As well, it reflects growing understanding of the complex determinants of adverse health outcomes of caregiver burden, and therefore the study of approaches to its mitigation.
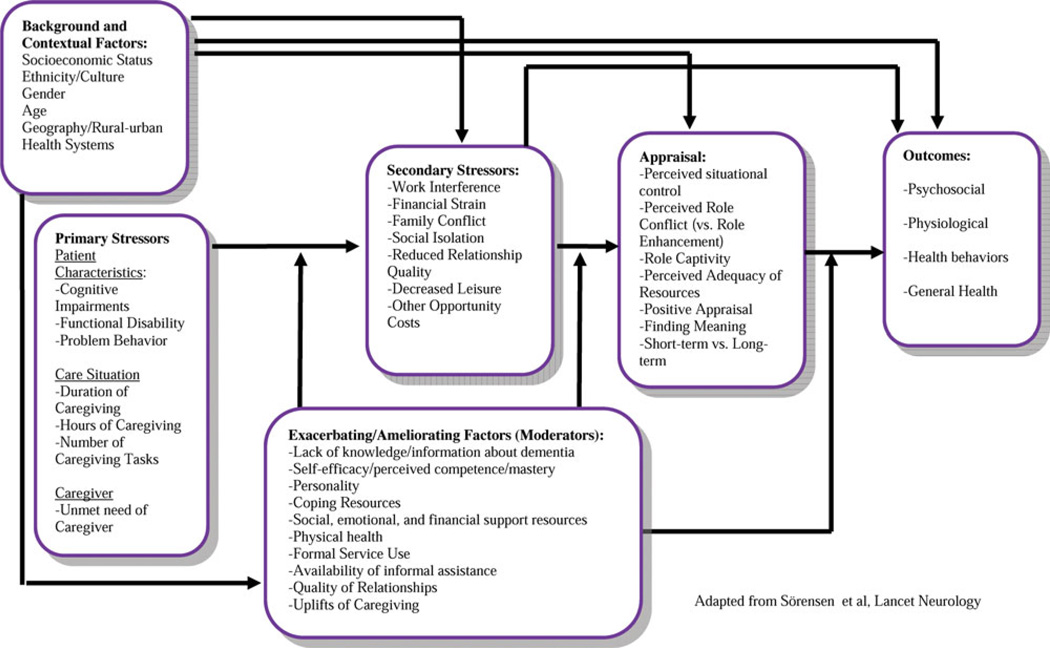
This issue of the Journal adds three studies to this growing and increasingly sophisticated literature. One by Gaugler et al.2 highlights the important role that caregiver burden plays in mediating the oft-noted relationship between patient behavioral disturbance and nursing home admission. Two others report on results of multifaceted interventions tested in randomized controlled trials. Bakker et al.3 show that an intervention with multiple components assembled to meet the specific needs of an individual older adult and their caregiver resulted in caregiver assessments of significantly reduced neuropsychiatric symptoms and perceived burden. Examining implementation of care in a “real world” community context, Spijker et al.4 tested whether training of health professionals in the delivery of an intervention designed to support caregivers’ effectiveness reduced the need for institutional care. Revealing no significant impact, the findings provide helpful insights into the program and provider characteristics that may influence an intervention’s effectiveness, and which require additional study. Together, the studies build on an increasingly robust body of evidence to guide development and implementation of interventions to reduce caregiver burden and its related costs. We will attempt to place them in context by combining the Stress Process Model5 and the Appraisal Model6 into one heuristic conceptual framework (Figure 1). The models suggest that caregivers appraise caregiving events and then respond with particular behaviors. Emotional, psychological, and health outcomes follow these behaviors.
FIGURE 1.
WHAT ARE THE COSTS OF CAREGIVING?
Caregiving can have both psychosocial and physical health effects. Women, spouses, and those in lower socioeconomic groups appear more vulnerable.7 Compared to noncaregivers, dementia caregivers report higher levels of stress, more depression and anxiety symptoms, and lower levels of subjective well-being, self-efficacy,8 and anxiety.9 In addition, they experience worse physical health outcomes, including higher levels of stress hormones, compromised immune response, antibodies, greater medication use,10 and greater cognitive decline.11
However, some individuals vulnerable to poor health outcomes may self-select into the caregiver role, and high distress levels and attendant morbidity could partially be explained by personal or family variables not related to the caregiving experience per se.12 Caregivers who have negative beliefs about their ability to cope and those who feel trapped in their role have higher rates of morbidity, and depressive symptoms, and they turn to institutionalization of the patient more quickly.13
WHY IS CAREGIVING STRESSFUL?
For dementia caregivers the strongest predictor of caregiver burden, depressive symptoms, and physical health issues are primary stressors, such as the patient’s behavior problems, including day and nighttime wandering, emotional outbursts, and inappropriate behavior.14,15 However, the type of dementia and the type of behavioral problems most closely associated with it may play a role in caregiver distress as well.16,17 Dementia caregivers experience more burden when caregiving intensity is higher and when they experience fewer perceived benefits or uplifts. Interestingly, although patient physical impairments increase burden for caregivers of nondemented patients, this is rarely the case for dementia caregivers.14
WHAT FACTORS MODERATE OR MEDIATE THE IMPACT OF STRESS ON CAREGIVERS?
Recent studies and meta-analyses have identified several important moderators and mediators captured in our conceptual model (Figure 1) as “secondary stressors,” “exacerbating/ameliorating factors,” and “appraisal,” as well as “background factors.” First, cultural background may change the strength of relationships between certain caregiving stressors and their outcomes.18 Asian Americans and Latinos do not differ from whites in reported burden but they do report more depression symptoms. Interestingly, African Americans and Hispanics exhibit more perceived uplifts of caregiving than whites.18 Differences in coping styles may be the key mediator to understanding these differences.19–21 Despite better mental health outcomes, however, ethnic minority caregivers often report more physical health problems than white caregivers, indicating that low reports of distress do not always imply the absence of risk for caregivers.18
Other important moderators include gender, knowledge/ information, social, economic, and community resources as well as intrapersonal resources or vulnerabilities. Female caregivers report more symptoms of depression than males.7 Lack of knowledge about dementia causes caregivers to overestimate patient’s abilities,22 which may lead to greater anger, frustration, and depression. Lower socioeconomic status or income is also a risk factor for greater distress,11 especially among African Americans.23
Larger social networks,20 frequent social contact, and the ability to arrange for assistance from friends are moderators of depressive symptoms and caregiver burden with largely protective effects. Dysfunctional family interaction patterns, emotional detachment, negativity, and overinvolvement, are moderators that exacerbate the relationship between objective burden and caregiver distress.24 Dysfunctional coping strategies, for example, avoidance/ denial, put caregivers at risk for anxiety, whereas approach-based coping is associated with reduced hemostatic reactivity in response to stress.25 Other exacerbating factors may include personal vulnerabilities, such as high levels of neuroticism or preexisting medical conditions.26,27
Mediators include secondary stressors, that is, reactions or outcomes of the primary stressors that account for the caregiving effect or exacerbate/weaken it over time. Unmet need with regard to help with different care activities, information, and respite support, for example, exacerbates the negative effects of caregiving.28,29 Gaugler’s article in this issue suggests, in fact, that overall burden is not only a direct predictor of nursing home admission but fully mediates the effect of particular behavior problems.2 Certain problem behaviors may be better tolerated by caregivers if overall burden can be kept under control.
Geographic and systemic care-delivery issues may also account for different levels of distress for caregivers. Innes30 points to a remarkable lack of consideration of rural-urban differences in informal caregivers’ experience.30 The two studies in this issue that address interventions in the Dutch medical system point to drastic differences from the United States in available services under the “usual care” condition.
CAREGIVER INTERVENTIONS
Research to date indicates that, overall, intervention effects are relatively small. Of the numerous types of caregiver interventions,31 psychoeducational approaches are most effective at improving caregiver knowledge, reducing caregiver burden and depression symptoms, and increasing subjective wellbeing and caregiver satisfaction. However, except for knowledge increase, these effects are present only if the interventions call for active participation and behavior management skills-building.32 Interestingly, psychoeducational interventions may improve the symptoms of the patient as well,33 perhaps by training the caregiver to redirect the patient to avoid escalating problem behavior.34
Not surprisingly, psychotherapy (primarily cognitive-behavioral therapy), support groups, consultation/case management, respite care, and cognitive training of patients tend to have domain-specific effects. For example, psychotherapy improves caregiver burden, depression,33 and anxiety,35 but not necessarily knowledge about dementia; consultation/case management has moderate effects on burden, but not depression; care receiver training affects the patient’s symptoms, but not always the caregiver’s; and respite care reduces burden and depression symptoms and increases subjective wellbeing. 33 Because different intervention types share elements (e.g., homework and role-playing are part of both psychotherapy and psychoeducation), it may be more important to focus on components, rather than compare packaged programs.
Reducing secondary stressors, such as social isolation, is an effective strategy in assisting caregivers,36 as are interventions that reduce caregivers’ perceived pressure and burden. However, such interventions still require further testing. A recent review and meta-analysis37 found that cholinesterase inhibitors have a small but statistically significant benefit to caregivers, both reducing caregiver burden and hours spent caregiving. However, we do not recommend relying solely on patient medication to address caregiver distress because effect sizes for pharmacotherapy are quite small and because many patients may not have access to cognitive enhancement medications. Furthermore, Mittelman et al.38 report that medicating dementia patients is only effective in reducing caregiver burden when it is combined with counseling.
Multicomponent treatments encompass a diverse group of programs some of which are considerably more systematic in their application of components than others. Interventions are more effective in delaying nursing home placement when they expose participants to all components in a structured fashion.33 The interventions tested by Bakker et al. and Spijker et al. (this issue) fall into this category as well. These programs are likely effective when they simultaneously target several of the primary stressors, secondary stressors, and moderators depicted in Figure 1.
WHAT FACTORS MODERATE THE EFFECTIVENESS OF INTERVENTIONS?
Characteristics of the Intervention
Individualized interventions can be more easily adapted to the specific needs of the caregivers and may, therefore, be more effective for modifying burden or distress for caregivers in general.32 However, interventions in groups are more effective in increasing social support and those that avoid dilution of the participant’s active involvement are likely to be as effective as individual approaches. Longer interventions generally are more effective at reducing distress and delaying institutionalization. Even single-component interventions, if they last longer or involve more frequent interactions, tend to have stronger effects than less intense interventions that have multiple components.32,33
Characteristics of the Caregiver
Older caregivers may have less access to information about dementia care in their daily lives and therefore show greater improvements in knowledge.32 Women show more improvements in depression and knowledge but less improvement in subjective well-being than men.32 Caregivers with less education may respond more favorably to a multicomponent intervention39 while African Americans may respond less to interventions with regard to depression and burden outcomes even as they derive benefits in quality of life.40 Finally, spouses benefit more from interventions with regard to decreasing the number and bother of patient’s problem behaviors as well as delays in nursing home placement.33 Thus, interventions should be individualized to caregivers’ cultural and educational background, current knowledge and skill, mental health status, physical health status, and personality.
ISSUES IN CURRENT CAREGIVING RESEARCH AND FUTURE RESEARCH DIRECTIONS
We have identified several continuing areas of need for caregiving research. First, the identification of the most vulnerable caregivers requires additional attention. These are often individuals with preexisting mental or physical health conditions. Individualization of interventions requires adequate preintervention assessment to identify caregivers who would most benefit from interventions before they develop clinically significant symptoms. Several studies have addressed the pressing need for screening tools and protocols that are developed and validated specifically for caregivers.26,41Their clinical utility, however, remains to be determined.
Second, understanding the variation in caregiver experience and risk due to the moderators and mediators requires additional attention, especially with regard to their implications for interventions. Third, although there has been an increase in prospective studies, as suggested by Vitaliano et al. in 2005 and exemplified by the new contributions in this issue of the Journal, many now focus on nursing home placement either as an outcome (e.g., Gaugler et al.42) or as an additional stressful transition (e.g., Gaugler et al.43). More studies that examine caregiving’s “dynamic predictors of change” to investigate how changes in certain indicators confer long-term risk, describe and compare trajectories and patterns, and identify which subgroups are most distress-prone or resilient (e.g., Lafortune et al.44) are needed to help us understand why some caregivers thrive while others do poorly or provide poor care. How different appraisals, behaviors, and emotional reactions interact with or mediate each other over time remains an area of need as well. Gaugler’s article (this issue) is one example of such a study, as it includes both longitudinal and mediation effects.
Fourth, a promising recent body of work delves further into the biological mechanisms of the stress process. Understanding the role of physiological factors in stress responses, such as cardiovascular reactivity, atypical diurnal cortisol patterns, and increased proinflammatory protein levels, may allow interventions to target caregivers stress-management abilities, as has been piloted through yoga interventions.45
Fifth, the role of sleep disturbance in caregiver outcomes is an emerging area that is currently being translated effectively into interventions.46 Additional studies that carefully deconstruct existing interventions to identify the most effective components are still needed, as is research to address necessary and sufficient dosage and intensity of interventions and their cost-effectiveness. This includes a closer look at novel approaches, such as employer-based interventions, telephone support groups, and novel technologies.
Finally, collaborative and integrated care models have received increasing attention in the treatment of late life mood disorders in primary care47 and they have proved an effective approach to minimizing behavioral symptoms among dementia patients and reducing caregiver burden and distress as well.48 These approaches integrate multicomponent interventions into existing care systems. Components may include case management, psychoeducation, and coping skills training; legal and financial advice; resources and guidelines to enhance patient exercise; and information from the Alzheimer’s association. “Integrated support models”49 and “memory clubs”50 are other innovative approaches combining patient and caregiver support that, along with the complex interventions tested by Bakker et al. and Spijker et al. (this issue), warrant further testing.
The explosion of caregiver research over the last 15 years is a hopeful sign that help is on the way for chronically ill older adults and those who provide for their care in the community. However, what that care should consist of, to whom it should be prescribed, in what setting, and at what dose remain questions of pressing importance.
References
- 1.Vitaliano PP, Katon W, Unützer J. Making the case for caregiver research in geriatric psychiatry. Am J Geriatr Psychiatry. 2005;13(10):834–843. doi: 10.1176/appi.ajgp.13.10.834. [DOI] [PubMed] [Google Scholar]
- 2.Gaugler J, Wall MM, Kane RL, et al. Does caregiver burden mediate the effects of behavioral disturbances on nursing home admission? Am J Geriatr Psychiatry. 2011;19:497–506. doi: 10.1097/JGP.0b013e31820d92cc. [DOI] [PubMed] [Google Scholar]
- 3.Bakker TJ, Duivenvoorden HJ, Van Der Lee J, et al. Integrative psychotherapeutic nursing home program to reduce multiple psychiatric symptoms of cognitively impaired patients and caregiver burden: randomized controlled trial. Am J Geriatr Psychiatry. 2011;19:507–520. doi: 10.1097/JGP.0b013e3181eafdc6. [DOI] [PubMed] [Google Scholar]
- 4.Spijker A, Wollersheim H, Teerenstra S, et al. Systematic care for caregivers of patients with dementia: a multicentre, cluster-randomized, controlled trial. Am J Geriatr Psychiatry. 2011;19:521–531. doi: 10.1097/JGP.0b013e3182110599. [DOI] [PubMed] [Google Scholar]
- 5.Pearlin LI, Mullan JT, Semple SJ, et al. Caregiving and the stress process: an overview of concepts and their measures. Gerontologist. 1990;30(5):583–594. doi: 10.1093/geront/30.5.583. [DOI] [PubMed] [Google Scholar]
- 6.Lawton MP, Moss M, Kleban MH, et al. A two-factor model of care-giving appraisal and psychological well-being. J Gerontol. 1991;46(4):P181–P189. doi: 10.1093/geronj/46.4.p181. [DOI] [PubMed] [Google Scholar]
- 7.Pinquart M, Sörensen S. Gender differences in caregiver stressors, social resources, and health: an updated meta-analysis. J Gerontol: Psychol Sci. 2006;61B(1):P33–P45. doi: 10.1093/geronb/61.1.p33. [DOI] [PubMed] [Google Scholar]
- 8.Pinquart M, Sörensen S. Differences between caregivers and non-caregivers in psychological health and physical health: a meta-analysis. Psychol Aging. 2003;18(2):250–267. doi: 10.1037/0882-7974.18.2.250. [DOI] [PubMed] [Google Scholar]
- 9.Mahoney R, Regan C, Katona C, et al. Anxiety and depression in family caregivers of people with Alzheimer disease: the LASER-AD study. Am J Geriatr Psychiatry. 2005;13(9):795–801. doi: 10.1176/appi.ajgp.13.9.795. [DOI] [PubMed] [Google Scholar]
- 10.Vitaliano PP, Young HM, Zhang J. Is caregiving a risk factor for illness? Curr Direct Psychol Sci. 2004;13(1):13–16. [Google Scholar]
- 11.Vitaliano PP, Echeverria D, Yi J, et al. Psychophysiological mediators of caregiver stress and differential cognitive decline. Psychol Aging. 2005;20(3):402–411. doi: 10.1037/0882-7974.20.3.402. [DOI] [PubMed] [Google Scholar]
- 12.Hooker K, Monahan D, Bowman SR, et al. Personality counts for a lot: Predictors of mental and physical health of spouse caregivers in two disease groups. J Gerontol: Psychol Sci. 1998;53B:P73–P85. doi: 10.1093/geronb/53b.2.p73. [DOI] [PubMed] [Google Scholar]
- 13.Pinquart M, Sörensen S. Associations of stressors and uplifts of caregiving with caregiver burden and depressive mood: a meta-analysis. J Gerontol Ser B-Psychol Sci Soc Sci. 2003;58(2):P112–P128. doi: 10.1093/geronb/58.2.p112. [DOI] [PubMed] [Google Scholar]
- 14.Pinquart M, Sörensen S. Associations of caregiver stressors and uplifts with subjective well-being and depressive mood: a meta-analytic comparison. Aging Ment Health. 2004;8(5):438–449. doi: 10.1080/13607860410001725036. [DOI] [PubMed] [Google Scholar]
- 15.Pinquart M, Sörensen S. Correlates of physical health of informal caregivers: a meta-analysis. J Gerontol Ser B-Psychol Sci Soc Sci. 2007;62(2):P126–P137. doi: 10.1093/geronb/62.2.p126. [DOI] [PubMed] [Google Scholar]
- 16.Yeager CA, Hyer LA, Hobbs B, Coyne AC. Alzheimer’s disease and vascular dementia: the complex relationship between diagnosis and caregiver burden. Issues Ment Health Nurs. 2010;31(6):376–384. doi: 10.3109/01612840903434589. [DOI] [PubMed] [Google Scholar]
- 17.Leggett AN, Zarit S, Taylor A, Galvin JE. Stress and burden among caregivers of patients with Lewy Body dementia. Gerontologist. 2011;51(1):76–85. doi: 10.1093/geront/gnq055. [DOI] [PubMed] [Google Scholar]
- 18.Pinquart M, Sörensen S. Ethnic differences in stressors, resources, and psychological outcomes of family caregiving: a meta-analysis. Gerontologist. 2005;45(1):90–106. doi: 10.1093/geront/45.1.90. [DOI] [PubMed] [Google Scholar]
- 19.Haley WE, Gitlin LN, Wisniewski SR, et al. Well-being, appraisal, and coping in African-American and Caucasian dementia caregivers: findings from the REACH study. Aging Ment Health. 2004;8(4):316–329. doi: 10.1080/13607860410001728998. [DOI] [PubMed] [Google Scholar]
- 20.Sayegh P, Knight BG. The effects of familism and cultural justification on the mental and physical health of family caregivers. J Gerontol Ser B Psychol Sci Soc Sci. 2011;66B(1):3–14. doi: 10.1093/geronb/gbq061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hebert RS, Dang Q, Schulz R. Religious beliefs and practices are associated with better mental health in family caregivers of patients with dementia: findings from the REACH study. Am J Geriatr Psych. 2007;15(4):292–300. doi: 10.1097/01.JGP.0000247160.11769.ab. [DOI] [PubMed] [Google Scholar]
- 22.Ala TA, Berck LG, Popovich AM. Knowledge of personal information and caregiver awareness in Alzheimer’s disease. Am J Alzheimers Dis Other Dement. 2005;20(2):119–125. doi: 10.1177/153331750502000202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Roff LL, Burgio LD, Gitlin L, et al. Positive aspects of Alzheimer’s caregiving: the role of race. J Gerontol B Psychol Sci Soc Sci. 2004;59(4):P185–P190. doi: 10.1093/geronb/59.4.p185. [DOI] [PubMed] [Google Scholar]
- 24.Mitrani VB, Lewis JE, Feaster DJ, et al. The role of family functioning in the stress process of dementia caregivers: a structural family framework. Gerontologist. 2006;46(1):97–105. doi: 10.1093/geront/46.1.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Aschbacher K, Patterson TL, von Kanel R, et al. Coping processes and hemostatic reactivity to acute stress in dementia caregivers. Psychosom Med. 2005;67(6):964–971. doi: 10.1097/01.psy.0000188458.85597.bc. [DOI] [PubMed] [Google Scholar]
- 26.Marziali E, McCleary L, Streiner DL. Evaluation of an assessment battery for estimating dementia caregiver needs for health and social care services. Am J Alzheimers Dis Other Demen. 2010;25(5):446–454. doi: 10.1177/1533317510370958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vitaliano PP, Zhang J, Scanlan JM. Is caregiving hazardous to one’s physical health? A meta-analysis. Psychol Bull. 2003;129(6):946–972. doi: 10.1037/0033-2909.129.6.946. [DOI] [PubMed] [Google Scholar]
- 28.Gaugler JE, Anderson KA, Leach CR, et al. The emotional ramifications of unmet need in dementia caregiving. Am J Alzheimers Dis Other Demen. 2004;19(6):369–378. doi: 10.1177/153331750401900605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Robison J, Fortinsky R, Kleppinger A, et al. A broader view of family caregiving: effects of caregiving and caregiver conditions on depressive symptoms, health, work, and social isolation. J Gerontol Ser B Psychol Sci Soc Sci. 2009;64B(6):788–798. doi: 10.1093/geronb/gbp015. [DOI] [PubMed] [Google Scholar]
- 30.Innes A, Morgan D, Kostineuk J. Dementia care in rural and remote settings: a systematic review of informal/family caregiving. Maturitas. 2011;68(1):34–46. doi: 10.1016/j.maturitas.2010.10.002. [DOI] [PubMed] [Google Scholar]
- 31.Sörensen S, Duberstein P, Gill D, et al. Dementia care: mental health effects, intervention strategies, and clinical implications. Lancet Neurol. 2006;5(11):961–973. doi: 10.1016/S1474-4422(06)70599-3. [DOI] [PubMed] [Google Scholar]
- 32.Pinquart M, Sörensen S. Helping caregivers of persons with dementia: which interventions work and how large are their effects. Int Psychogeriat. 2006;18(4):577–595. doi: 10.1017/S1041610206003462. [DOI] [PubMed] [Google Scholar]
- 33.Brodaty H, Green A, Koschera A. Meta-analysis of psychosocial interventions for caregivers of peoplewith dementia. J AmGeriatr Soc. 2003;51(5):657–664. doi: 10.1034/j.1600-0579.2003.00210.x. [DOI] [PubMed] [Google Scholar]
- 34.de Vugt ME, Stevens F, Aalten P, et al. Do caregiver management strategies influence patient behaviour in dementia? Int J Geriatr Psychiatry. 2004;19(1):85–92. doi: 10.1002/gps.1044. [DOI] [PubMed] [Google Scholar]
- 35.Akkerman RL, Ostwald SK. Reducing anxiety in Alzheimer’s disease family caregivers: the effectiveness of a nine-week cognitive-behavioral intervention. Am J Alzheimers Dis Other Demen. 2004;19(2):117–123. doi: 10.1177/153331750401900202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Roth DL, Mittelman MS, Clay OJ, et al. Changes in social support as mediators of the impact of a psychosocial intervention for spouse caregivers of persons with Alzheimer#x02019;s disease. Psychol Aging. 2005;20(4):634–644. doi: 10.1037/0882-7974.20.4.634. [DOI] [PubMed] [Google Scholar]
- 37.Lingler JH, Martire LM, Schulz R. Caregiver-specific outcomes in antidementia clinical drug trials: a systematic review and meta-analysis. J Am Geriatr Soc. 2005;53(6):983–990. doi: 10.1111/j.1532-5415.2005.53313.x. [DOI] [PubMed] [Google Scholar]
- 38.Mittelman MS, Brodaty H, Wallen AS, et al. A 3 country randomized controlled trial of a psychosocial intervention for caregivers combined with pharmacological treatment for patients with Alzheimer’s disease: effects on caregiver depression. Am J Geriatr Psychiatry. 2008;16(11):893–904. doi: 10.1097/JGP.0b013e3181898095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Elliott AF, Burgio LD, DeCoster J. Enhancing caregiver health: findings from the Resources for enhancing Alzheimer’s caregiver health II intervention. J Am Geriatr Soc. 2010;58(1):30–37. doi: 10.1111/j.1532-5415.2009.02631.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Belle SH, Burgio L, Burns R, et al. Enhancing the quality of life of dementia caregivers from different ethnic or racial groups. Ann Intern Med. 2006;145(10):727–738. doi: 10.7326/0003-4819-145-10-200611210-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Czaja SJ, Gitlin LN, Schulz R, et al. Development of the risk appraisal measure: a brief screen to identify risk areas and guide interventions for dementia caregivers. J Am Geriatr Soc. 2009;57(6):1064–1072. doi: 10.1111/j.1532-5415.2009.02260.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gaugler J, Duval S, Anderson K, et al. Predicting nursing home admission in the U.S.: a meta-analysis. BMC Geriatrics. 2007;7(1):13. doi: 10.1186/1471-2318-7-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gaugler J, Mittelman M, Hepburn K, et al. Clinically significant changes in burden and depression among dementia caregivers following nursing home admission. BMC Med. 2010;8(1):85. doi: 10.1186/1741-7015-8-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lafortune L, Béland F, Bergman H, et al. Health status transitions in community-living elderly with complex care needs: a latent class approach. BMC Geriatr. 2009;9:6. doi: 10.1186/1471-2318-9-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Waelde LC, Thompson L, Gallagher-Thompson D. A pilot study of a yoga and meditation intervention for dementia caregiver stress. J Clin Psychol. 2004;60(6):677–687. doi: 10.1002/jclp.10259. [DOI] [PubMed] [Google Scholar]
- 46.McCurry SM, Gibbons LE, Logsdon RG, et al. Nighttime insomnia treatment and education for Alzheimer’s disease: a randomized, controlled trial. J Am Geriatr Soc. 2005;53(5):793–802. doi: 10.1111/j.1532-5415.2005.53252.x. [DOI] [PubMed] [Google Scholar]
- 47.Bruce ML, Ten Have TR, Reynolds Reynolds CF, III, et al. Reducing suicidal ideation and depressive symptoms in depressed older primary care patients: a randomized controlled trial. JAMA. 2004;291(9):1081–1091. doi: 10.1001/jama.291.9.1081. [DOI] [PubMed] [Google Scholar]
- 48.Callahan CM, Boustani MA, Unverzagt FW, et al. Effectiveness of collaborative care for older adults with Alzheimer disease in primary care: a randomized controlled trial. JAMA. 2006;295(18):2148–2157. doi: 10.1001/jama.295.18.2148. [DOI] [PubMed] [Google Scholar]
- 49.Droes RM, Meiland F, Schmitz M, et al. Effect of combined support for people with dementia and carers versus regular day care on behaviour and mood of persons with dementia: results from a multi-centre implementation study. Int J Geriatr Psychiatry. 2004;19(7):673–684. doi: 10.1002/gps.1142. [DOI] [PubMed] [Google Scholar]
- 50.Zarit SH, Femia EE, Watson J, et al. Memory club: a group intervention for people with early-stage dementia and their care partners. Gerontologist. 2004;44(2):262–269. doi: 10.1093/geront/44.2.262. [DOI] [PubMed] [Google Scholar]