Abstract
We performed genetic immunization of outbred NMRI mice, using a cDNA encoding the human thyrotropin receptor (TSHr). All mice produced antibodies capable of recognizing the recombinant receptor expressed at the surface of stably transfected Chinese hamster ovary (CHO) cells, and sera from most of the immunized mice blocked TSH-dependent stimulation of cAMP accumulation in cells expressing the TSHr. Five out of 29 female mice showed sign of hyperthyroidism including elevated total T4 and suppressed TSH levels. The serum of these mice contained thyroid-stimulating activity, as measured in a classic assay using CHO cells expressing recombinant TSHr. In contrast, only 1 male out of 30 had moderately elevated serum total T4 with undetectable TSH values. The hyperthyroid animals had goiters with extensive lymphocytic infiltration, characteristic of a Th2 immune response. In addition, these animals displayed ocular signs reminiscent of Graves’ ophthalmopathy, including edema, deposit of amorphous material, and cellular infiltration of their extraocular muscles. Our results demonstrate that genetic immunization of outbred NMRI mice with the human TSHr provides the most convincing murine model of Graves’ disease available to date.
Introduction
Graves’ disease is an autoimmune condition characterized typically by hyperthyroidism, thyroid hyperplasia, and additional signs of ophthalmopathy, pretibial myxedema, or acropachy. The pathophysiological mechanisms responsible for thyrotoxicosis and thyroid hyperplasia are relatively well understood: autoantibodies directed against the thyrotropin receptor (TSHr) activate it, which results in cAMP-dependent stimulation of thyrocyte function and growth (1). The immediate causes of the additional peripheral signs, which can vary greatly in intensity, are less clear. One current hypothesis holds that the TSHr expressed in preadipocytes would be the antigen shared by thyrocytes and the affected peripheral tissues (2, 3), but the issue remains highly controversial (4–6).
The central roles of the TSHr as the main autoantigen and thyroid-stimulating autoantibodies (TSAbs) as the immediate cause of hyperthyroidism are not disputed. However, the mechanisms by which the TSAbs do activate the receptor and their relation with autoantibodies interfering with TSH binding (thyroid binding–inhibiting immunoglobulins [TBIIs]) or action (thyroid stimulation–blocking antibodies [TSBAbs]) are still unclear (7). An animal model would be an invaluable tool to explore the pathophysiology of Graves’ disease. Unfortunately, no natural model is available, and numerous attempts to create an experimental model have met with complete failure or resulted in imperfect phenocopies (7, 8). Immunization of inbred mice of various genetic backgrounds with TSHr preparations (9–13), TSHr peptides (14), or expression cDNA constructs (15) lead, in many cases, to the production of anti-TSHr antibodies with TBII and TSBAb activity. However, when observed, stimulatory effects on thyroid function were marginal (13, 14, 16). Recently, an original immunization protocol using transfected fibroblasts coexpressing the TSHr and class II antigen resulted in a proportion of the immunized mice displaying hyperthyroidism and goiter (17, 18). However, the hyperplastic glands were devoid of lymphocytic infiltration, a hallmark of Graves’ thyroids.
In an earlier experiment, we used genetic immunization of mice with a human TSHr cDNA construct in an expression vector (15). When immunized in this way, BALB/c mice mount a very strong response against the receptor. Anti-TSHr antibodies recognizing the native receptor at the surface of Chinese hamster ovary (CHO) cells are readily observed in all mice, and both TBII and TSBAb activities are present in their serum (15). However, in the only instance when it was observed, TSAb activity was not associated with hyperthyroidism (15). We reasoned that failure to develop hyperthyroidism might be related to an inadequate genetic background of the mice. Accordingly, in this study we used the same genetic immunization protocol with outbred NMRI mice. We show that 1 out of 5 female mice developed hyperthyroidism with circulating TSAb and thyroid hyperplasia. Their glands displayed a lymphocytic infiltration characteristic of a Th2 reaction, and, in addition, extraocular muscles were dissected by edema and a fibrotic amorphous material accompanied by macrophages and mast cells. To our knowledge, these mice constitute the closest model of human Graves’ disease presently available.
Methods
Animals used, immunization schedules, sampling.
Two groups of 6-week old NMRI mice [Ico:NMRI (IOPS:Han)] were used (29 females, 30 males). These mice were originally derived from Swiss mice (19) and were maintained as nonconsanguineous in the Central Institute for Laboratory of Animal Breeding (Hanover, Germany). According to available information, they do not tolerate cross-grafting of skin. On day 0 they were injected under Nembutal anesthesia in the anterior tibialis muscle with 100 μg of pcDNAIII-hTSHR in PBS. The muscle had been injected 5 days earlier with 100 μL cardiotoxin (10 mM, purified from the venom of Naja nigricollis; Calbiochem, La Jolla, California, USA). Injections were repeated 4 weeks and 8 weeks thereafter. Two groups of nonimmunized NMRI mice were used as controls (6 females, 6 males). Blood samples were obtained from the retro-ocular capillaries of the right eye between the 10th and the 12th week after the initial immunization, and all mice were sacrificed after 16 weeks. For all determinations sera were tested individually. Mice were handled and housed in accordance with procedures approved by the local committee for animal well-being.
Genotyping of NMRI mice.
The MHC haplotypes were determined by PCR amplification of selected portions of the Aα gene (exon α1, position 93 to 326 of Aαd allele) and Eβ gene (3′ intron 2, position 2161 to 2281 and 3′ intron 2 and 5′ exon β2, position 2161 to 2485, from Eβd allele) followed by restriction or DNA sequencing according to Saha and colleagues (20, 21) and Peng et al. (22). DNA was extracted from the liver of individual animals according to standard procedures (23). The microsatellite in intron 2 of Eβ gene, (TGGA)2-TAGA-TGGA-GGTA-(GGCA)8-TGCA-GACA-GCCTA, shows significant differences when compared with the canonical H2q haplotype.
Flow cytometry.
Flow cytometry analysis was performed as described previously (15) with 2 μL of serum on CHO cells expressing the hTSHR (JP19) (24) or control CHO cells. Results are expressed in arbitrary fluorescence units (AFU).
Total T4 and TSH assays.
Total T4 was measured with a commercial kit (TT4; INCSTAR, Diasorin, Zaventem, Belgium). TSH was measured using a sensitive, heterologous disequilibrium double-antibody precipitation radioimmunoassay. This assay uses rat antiserum, rat TSH labeled with 125I, and a standard of mouse serum TSH. The last named was derived from mice rendered hypothyroid and contained 20 mU/mL (1 ng rat TSH = 0.5 mU bovine TSH) (25).
Measurement of TSAb and TSBAb.
TSAb and TSBAb were measured using CHO cells stably expressing the TSHr (JP26, ref. 24), as described previously (15). Duplicate samples were assayed in all experiments; results are expressed as picomoles of cAMP per well.
Light microscopy and immunohistochemistry.
Mice were exsanguinated by cardiac puncture under Nembutal anesthesia. The extraocular muscle from the left eye (opposite from the side used for blood sampling) and the thyroid gland were removed and carefully dissected from the surrounding connective tissue under the microscope. The thyroid lobes were separated, dried on a filter paper, and weighed. The extraocular muscles and 1 thyroid lobe were processed for light microscopy. They were immersed for 2 hours in 2.5% glutaraldehyde in 0.1 M cacodylate buffer, postfixed for 1 hour in 1% osmium tetroxide, and embedded in LX 112 resin. Sections (0.5 μm thick) were stained with toluidine blue. The other thyroid lobe was handled for immunohistochemistry. It was inserted into a liver fragment, embedded in Tissue-Tek, and rapidly frozen in isopentane cooled in liquid nitrogen to generate cryostat sections. The frozen sections were subjected to immunoperoxidase staining using different rat mAb’s specific for CD4+ T cells, IL4-producing T cells, IFNγ-producing T cells, and B cells, as described previously (10). The number of labeled cells and follicular profiles were counted at a magnification of 250 in 10 microscope fields chosen at random.
Results
Previous studies have shown that virtually all BALB/c mice immunized by intramuscular injection of human TSHr cDNA constructs in an expression vector made antibodies recognizing the native receptor (15). Most displayed TSBAb and TBII activities in their serum, but hyperthyroidism was never observed, even in the only mouse with detectable TSAb (15). We reasoned that failure to produce effective stimulating autoantibodies in this inbred strain of mice might be related to their genetic background. Accordingly, we repeated the same genetic immunization protocol, but instead of using inbred animals, we used outbred NMRI mice. Fifty-nine mice (30 males and 29 females) were immunized (see Methods). They were individually analyzed (a) for the presence of antibodies recognizing the TSHr, (b) the levels of T4 and TSH in their sera, (c) the presence of TSAb and TSBAb activities in their blood, (d) the weight and histopathology of their thyroids, and (e) the histopathology of their eye orbits.
Virtually all immunized mice make anti-TSHr antibodies
When analyzed using flow cytometry with CHO cells expressing the human TSHr (JP19 cells; ref. 24), the sera from all immunized mice, except for 2 male mice (number 9 and 14, see Table 1), were shown to contain autoantibodies recognizing the native TSHr (Table 1).
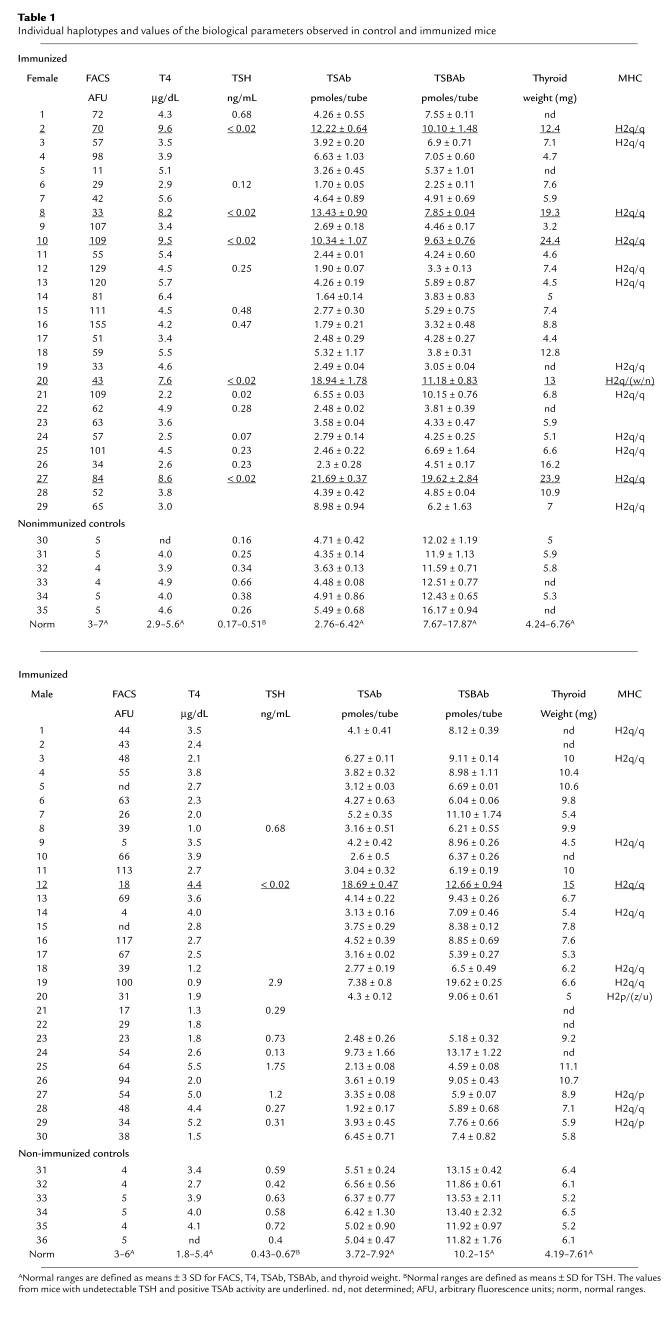
Table 1.
Individual haplotypes and values of the biological parameters observed in control and immunized mice
Twenty percent of immunized females are hyperthyroid and produce TSAb.
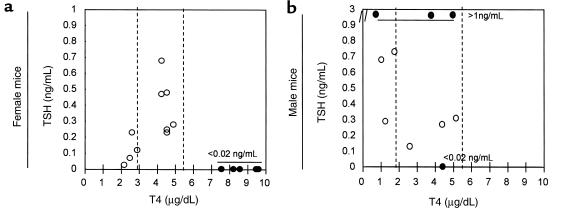
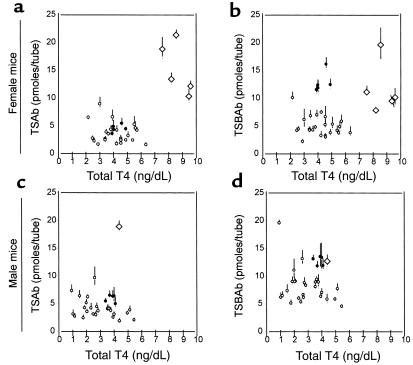
A striking difference was observed between total T4 levels measured in the serum of male and female mice immunized with TSHr cDNA (Table 1). Seven out of 29 female mice, but none of the 30 males, had levels above the upper limit of normal (normal range defined as mean ± 3 standard deviations in control, nonimmunized mice; see Table 1). This difference in incidence between sexes was statistically highly significant (P = 0.0046, Fisher exact test). Seven female animals, including 5 with a high T4, also displayed TSAb activity in their serum. Serum TSH levels measured in the 5 animals with both high T4 and TSAb activity (numbers 2, 8, 10, 20, 27) were undetectable, confirming their hyperthyroid state. In contrast, serum TSH concentrations were within the normal range in the 10 female animals with normal T4 in which sufficient amount of serum was available to perform the assay. Thus, it appears that the majority of these mice were euthyroid. The 2 female mice with the lowest T4 values (number 6 and 26, Table 1) had normal TSH, suggesting that these animals were not hypothyroid. In contrast, only a single male mouse (number 12) displayed clear TSAb activity, and, although the serum T4 concentration was in the normal range, TSH was fully suppressed, suggesting subclinical hyperthyroidism. Another male mouse (number 19) was overtly hypothyroid, with low T4 and high TSH levels (Table 1 and Figure 1b). Plotting of individual T4 values against TSH (Figure 1) or TSAb (Figure 2) led to the clear identification of a subpopulation of mice that became hyperthyroid upon immunization. The relation was particularly striking in females (Figures 1a and 2a).
Figure 1.
Relation between total T4 and TSH in sera from female (a) or male (b) mice immunized with cDNA coding for human TSHr. T4 levels are expressed in micrograms per deciliter, and TSH is expressed in nanograms per milliliter. Dotted lines show the limits of normal values. Filled circles correspond to sera with an undetectable level of TSH (< 0.02 ng/mL). Open circles correspond to sera with a TSH level above 1.5 ng/mL.
Figure 2.
Relation between total T4 and TSAb (a and c) or TSBAb (b and d) in sera from female (a and b) or male (c and d) mice. Nonimmunized or immunized animals are indicated by filled or open symbols, respectively. Open diamonds correspond to sera with a undetectable TSH levels. TSAb and TSBAb activities were measured using CHO cells expressing the human TSHr as described in Methods. Results are expressed as picomoles of cAMP produced per well (mean ± range of duplicates).
Whereas only the hyperthyroid mice had TSAb (Table 1 and Figure 2, a and c), a great proportion (> 75%), whether male or female, had TSBAb in their serum (Table 1 and Figure 2, b and d). It must be stressed that TSAb and TSBAb measurements are not independent of each other; each activity is potentially affected by the presence of the other. Female mouse number 8, for instance, displayed both TSAb and TSBAb activities. It is the balance between the two activities that likely determines the hormonal status of the animals. Female mouse number 27 was an example of almost “pure” TSAb activity leading to hyperthyroidism, whereas mouse number 6 had low T4 and displayed almost “pure” blocking activity.
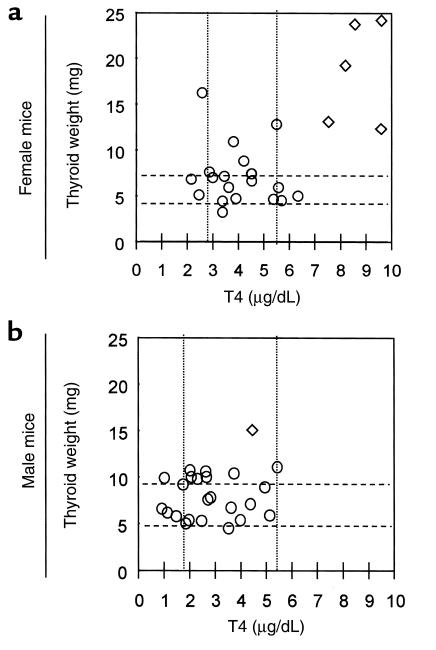
Hyperthyroid mice have a goiter with a lymphocytic infiltration.
The weight of the thyroid glands of the 5 hyperthyroid females was 18.6 ± 5.6 mg (mean ± SD) as compared with 5.6 ± 0.4 in control nonimmunized animals (P < 0.001; Figure 3a). Plotting of the individual T4 values against thyroid weight led again to the clear identification of a subpopulation of hyperthyroid animals. Again, this observation could be made only in females (compare Figure 3a and 3b). In these hyperthyroid mice, the thyroid morphology was considerably modified as compared with control mice (Figure 4a).
Figure 3.
Relation between total T4 and thyroid weight for female (a) or male mice (b) immunized with cDNA coding for the human TSHr. Open diamonds correspond to the glands from animals with undetectable TSH levels. Dotted lines show the limits of normal values.
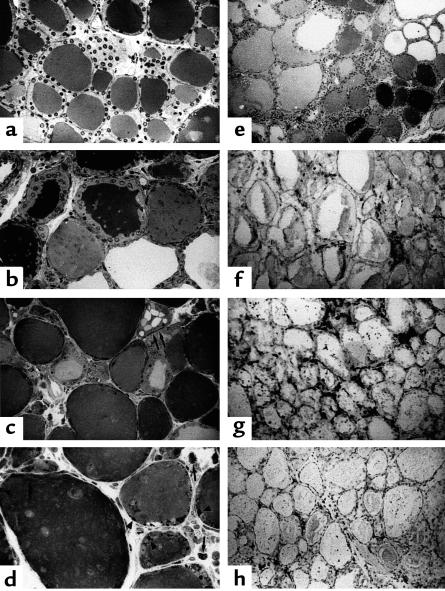
Figure 4.
(a) Semi-thin section of the thyroid from a control NMRI mouse. ×160. The follicles have a regular cuboidal epithelial layer limiting a lumen homogeneously filled with colloid. (b–e) Semi-thin sections of the thyroids from immunized hyperthyroid NMRI mice. (b) The follicles are heterogeneous. Some have a thickened irregular epithelial layer limiting a dense lumen, whereas others have a flat epithelium and an empty lumen. ×130. (c) Cloverleaf-shaped follicles (arrows) are indicative of an active neofolliculo-genesis. ×320. (d) Dense colloid droplets are frequently observed in the thyroid cells (arrowheads). Mast cells (arrows) are numerous in the interstitium. ×320. (e) The inflammatory infiltrate is very extended among the heterogenous follicles. ×320. (e–h) Frozen sections of thyroids from immunized hyperthyroid mice. (f) CD4+ T cells are clustered between the heterogenous follicles. ×130. (g) Numerous B220+ B cells are observed. ×130. (h) IL4+-producing T cells are also scattered around the follicles. ×130.
A first feature was the follicular heterogeneity. Some follicular lumina looked empty, whereas others were filled with dense colloid. The epithelia were either made of very flat cells or of cylindrical cells with irregular apical poles protruding into the colloid space (Figure 4b). Signs of new follicle formation, with typical cloverleaf-shaped follicles, were frequently observed (Figure 4c), and the epithelial cells, whatever their thickness, contained numerous and dense colloid droplets, a sign of active endocytosis (Figure 4d).
A second important morphological feature was an extended inflammatory infiltrate present throughout the gland (Figure 4e). It was made mostly of mononuclear cells, among which numerous mast cells were observed (Figure 4d). The infiltrate was constituted mainly of CD4+ T lymphocytes (Figure 4f) and B cells (Figure 4g), which is indicative of a Th2 humoral response. This was confirmed by the presence of numerous IL4-producing T cells (Figure 4h).
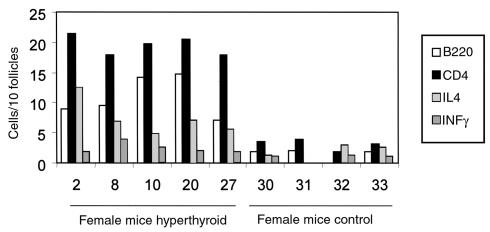
In the thyroid glands of the 5 hyperthyroid female mice, the mean number (± SD) of B cells per 10 follicular profiles (10.5 ± 0.7) was 5 times higher than in controls (1.9 ± 0.15; P < 0.001). The mean number of IL4-producing T cells (7.2 ± 0.5) was also significantly increased as compared with the controls (2.26 ± 0.85; P < 0.001). On the contrary, the number of IFNγ-producing cells remained low (2.63 ± 0.90) and not different from the controls (1.33 ± 0.04; P > 0.05) (Figure 5).
Figure 5.
Number of infiltrating cells in the thyroid glands of the 5 hyperthyroid mice (mice 2, 8, 10, 20, 27) in comparison with control mice (mice 30, 31, 32, 33): B cells (B220), CD4 T cells, IL4-producing cells, INFγ-producing cells. Results are expressed as number of cells per 10 follicles.
Histopathology of the extraocular muscle.
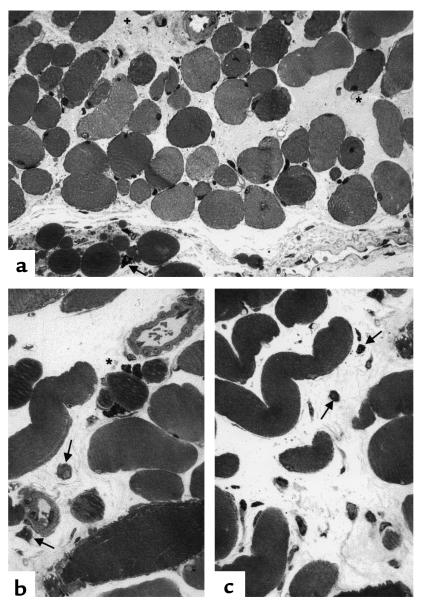
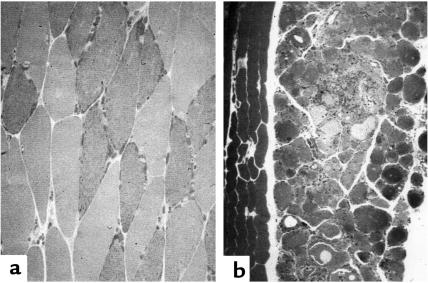
When compared with control mice, extraocular muscles from hyperthyroid animals displayed histological modifications with some characteristics of Graves’ ophthalmopathy (Figure 6). Muscular fibers were dissociated by edema and accumulation of a lightly stained amorphous material, probably made of glycosaminoglycans and, in some places, by fibrous tissue. A cellular infiltrate was present, made essentially of mast cells and macrophages, in close vicinity to adipocytes. Immune T and B cells were rare. These modifications were specific for the extraocular muscles. Other skeletal muscle from immunized animals were strictly normal (Figure 7).
Figure 6.
Semi-thin sections of extraocular muscles from immunized hyperthyroid NMRI mice. (a) The muscular cells, in transverse section, are dissociated by an edema and a deposit of an amorphous material (*) or by fibrous tissue (+). ×250. The adipous tissue infiltrating the muscle is made of cells of various size, often in association with mast cells (arrows). (b) Higher magnification of the closed association of adipocytes and mast cells (*) infiltrating the muscular cells, with macrophages (arrows). ×380. (c) Higher magnification of the fibrous tissue made of elongated fibroblasts and collagen fibers, among which mast cells (arrows) and macrophages are scattered. ×380.
Figure 7.
(a) Semi-thin section of extraocular muscle from a control NMRI mouse. The muscular cells are tightly associated to form a cylindrical bundle. ×250. (b) Semi-thin section of a thyroid from an immunized hyperthyroid NMRI mouse. The muscular cells along the thyroid do not show any modifications and form a regular bundle. ×130.
Determination of MHC haplotypes.
The MHC haplotypes of 24 mice, developing hyperthyroidism or not hyperthyroid, were determined by PCR amplification of selected portions of the Aα and Eβ genes followed by restriction or DNA sequencing (Table 1, and see Methods) (20–22). A total of 4 different haplotypes were identified. The most frequent haplotype (ν = 0.895) resembles closely H2q, with an α1 segment displaying minor variation in the coding sequence, when compared with published H2q sequence (H2-Iαq, Genbank accession number K01925) (C→T at position 212, changing a phenylalanine for a serine). In addition, the microsatellite in intron 2 of the Eβ gene, also shows significant differences when compared with the canonical H2q haplotype (see Methods). The other haplotypes resembled H2p (ν = 0.063), H2w (or H2n) (ν = 0.021), and H2z (or H2u) (ν = 0.021), according to published criteria (20–22). In females, 4 out of the 5 hyperthyroid animals were homozygous H2q/q, the fifth being heterozygous 112q/w or 112q/n). All immunized females that did not develop hyperthyroidism were H2q/q homozygotes. In males, the single immunized mouse with a suppressed TSH value was also H2q/q.
Discussion
Genetic immunization of outbred NMRI mice with the human TSHr cDNA led to a strong humoral response in both sexes: virtually all mice displayed antibodies capable of recognizing the native receptor in flow cytometry, and most had detectable levels of TSBAb activity in their serum (Figure 2, b and d). These results parallel those obtained previously with BALB/c mice (15) and confirm the efficiency of genetic immunization as a means to obtain antibodies recognizing the native structure of the receptor. With some exceptions (26, 27), immunization with recombinant protein preparations or peptides have yielded antibodies recognizing only (or preferentially) the denatured molecule (7). A proportion of these antibodies were endowed with TBII or TSBAb activities, which indicates that linear epitopes exposed at the surface of the native TSHr molecule are directly or indirectly implicated in the recognition of TSH. A constant frustration regarding all these experiments has been the absence of effective TSAb among the antibodies generated and the paucity of symptoms suggestive of thyroid dysfunction in the immunized animals.
There is evidence in humans that Graves’ disease is a multigenic/multifactorial disease (28). The observation that the concordance rate is higher in monozygotic than in dizygotic twins is a strong indication for a role of the genetic background (29). The relatively low concordance rate in monozygotic twins (20–50%), however, indicates that environment also plays an important role (29). Except for association with certain MHC class II alleles, the genetic makeup required for the development of Graves’ disease in humans remains unknown. We reasoned that a TSAb response in mice might be incompatible with the genetic background of the inbred strains that had been used up to now. Together with the previous negative results, our present observation that 1 out of 5 female NMRI mice immunized with TSHr cDNA constructs produced TSAbs, developed a goiter, and became thyrotoxic, suggests that the genetic background is indeed a major determinant of the ability to generate TSAbs. In addition, it indicates that the immune response triggered against the human receptor initially generated antibodies capable of recognizing the mouse receptor and interfering with its normal function. This seems to be the case both for stimulating antibodies (Figure 2a) and for blocking antibodies (Figure 2, b and d). Interestingly, there was no correlation between the amount of anti-TSHr antibodies produced, as judged by flow immunocytometry, and their TSAb or TSBAb activity (Table 1), indicating that it is the quality of the response that matters for generation of TSAb.
The cause for the higher prevalence of Graves’ disease in females is unknown in humans. When association of high T4, undetectable TSH, presence of TSAb’s and goiter were used as diagnostic criterion for Graves’ disease, a statistically different prevalence was observed between sexes in the present study (5/29 in females versus 0/30 in males, P = 0.0237). This constitutes an additional argument in favor of the relevance of our model in relation to the human disease. It will allow experimental exploration of the putative role of male/female hormones in this phenomenon.
Our model presents similarities and differences to that developed initially by Shimojo et al. (17, 18). In this case, immunization involved injection of the AKR/N mouse strain with syngeneic fibroblasts coexpressing the human TSHr and MHC class II antigen. The result was that about 1 out of 5 mice developed goiter and hyperthyroidism and had TSAb activity in their serum. An important difference wirh our model was the complete absence of lymphocytic infiltration in the thyroid glands. The reasons for this difference are not clear. They may reflect the different genetic background of the mice and/or the immunization protocol itself. Mice in the Shimojo model behave as if a purely humoral response was involved, with its origin outside of the thyroid gland. On the contrary, in the present study histopathology of the thyroid glands displayed signs of active thyroiditis with many of the characteristics found in human Graves’ disease. The thyroid interstitium was extensively infiltrated by immune cells. These include CD4+ T cells, but mainly cells characteristic of a Th2 humoral response, namely B cells, IL4-producing T cells, and mast cells. Besides the immune infiltration, thyroid follicles showed highly heterogeneous signs of activity. In addition, preliminary experiments indicate that the immunized mice show variation over time of the relative proportion of TSAb and TSBAb activities (not shown), a characteristic also found in the human disease (1). Finally, clear extrathyroidal manifestations were observed in the eye orbits of the mice immunized according to the present protocol. The ocular muscle displayed edema, accumulation of amorphous material, and signs of fibrosis in their interstitium. Cellular infiltration included mast cells and macrophages in the vicinity of adipocytes, with few B or T lymphocytes. Interestingly, eye signs have also been observed in experiments where BALB/c mice were immunized by passive transfer of T cells from animals immunized according to a protocol similar to the present one (30). This suggests that the genetic determinants required to develop TSAb and hyperthyroidism and the extrathyroidal signs of Graves’ disease may be different. It is an argument in favor of the pathophysiological relevance of the present experiments as a model for the human disease and strengthens the link between immunization against the TSHr and thyroid ophthalmopathy. An open question is whether the TSH receptor gene needs to be expressed within the eye orbit to trigger development of Graves’ ophthalmopathy.
It is puzzling that both in our model and that of Shimojo et al., only 1 out of 5 female mice developed hyperthyroidism after immunization. In this study, the outbred nature of NMRI mice would provide a logical explanation. However, our results demonstrate that the genetic diversity of the NMRI strain at the MHC locus is limited and does not correlate with the ability to develop hyperthyroidism (Table 1). The majority of mice, whether becoming hyperthyroid or not, were homozygous for a haplotype resembling closely H2q. Except, if genetic diversity at other non-MHC loci were involved, it is thus equally tenable that all NMRI mice would bear the susceptibility gene(s) and that the heterogeneity of the immunological response of individual mice would reflect differences in their personal immunological history. In this respect it would be interesting to explore the immunological response of H2q/q homozygotes with a homogenous genetic background, as in DBA or SWR mice. If one excludes the possibility of experimental causes, differences in the environment and/or individual experiences of the mice must be invoked in the case of the Shimojo model in which inbred mice were used. It would be of interest to replicate both our study and that of Shimojo with animals housed under pathogen-free conditions.
The immunization protocol described in this study constitutes, in our opinion, the closest animal model presently available for Graves’ disease. It opens the way to a series experiments that may help our understanding of the pathophysiology of the human disease, among these, generation of mAb’s with TSAb activity, identification of susceptibility genes by segregation analyses, study of the determinants responsible for the bias in sex ratio, and tracking of the antigen(s) or mechanisms responsible for the eye disease.
While this study was being evaluated for publication, Kaithamana et al. reported generation of hyperthyroidism in BALB/c mice after immunization with syngeneic M12 cells expressing TSHr or soluble purified extracellular domain of TSHr (31). Despite some similarities to the present study, there was no mention of eye signs.
Acknowledgments
We thank Marian Ludgate (University of Cardiff) and Christine Gervy (Erasme Hospital) for discussions and performance of the TSAb/TSBAb assays, respectively. This study was supported by the Belgian State, Prime Minister’s office, Service for Sciences, Technology and Culture. This work was also supported by grants from the Fonds de la Recherche Scientifique Médicale, the Fonds National de la Recherche Scientifique, the European Union (Biomed), and the Francqui Foundation. It was also supported by BRAHMS Diagnostica, Euroscreen S.A., and a grant from the National Institutes of Health (DK 15,070).
References
- 1.McKenzie, J.M., and Zakarija, M. 1995. Hyperthyroidism. In Endocrinology. L.J. DeGroot, editor. W.B. Saunders Co. Philadelphia, PA. 676–711.
- 2.Ludgate M, et al. The thyrotropin receptor in thyroid eye disease. Thyroid. 1998;8:411–413. doi: 10.1089/thy.1998.8.411. [DOI] [PubMed] [Google Scholar]
- 3.Bahn RS, et al. Thyrotropin receptor expression in Graves’ orbital adipose/connective tissues: potential autoantigen in Graves’ ophthalmopathy. J Clin Endocrinol Metab. 1998;83:998–1002. doi: 10.1210/jcem.83.3.4676. [DOI] [PubMed] [Google Scholar]
- 4.Gunji K, et al. Role of the eye muscles in thyroid eye disease: identification of the principal autoantigens [erratum 1998, 8:1079] Thyroid. 1998;8:553–556. doi: 10.1089/thy.1998.8.553. [DOI] [PubMed] [Google Scholar]
- 5.Heufelder AE. Retro-orbital autoimmunity. Baillieres Clin Endocrinol Metab. 1997;11:499–520. doi: 10.1016/s0950-351x(97)80723-9. [DOI] [PubMed] [Google Scholar]
- 6.Weetman AP. Eyeing up Graves’ ophthalmopathy. Mol Cell Endocrinol. 1997;126:113–116. doi: 10.1016/s0303-7207(96)03986-x. [DOI] [PubMed] [Google Scholar]
- 7.Rapoport B, Chazenbalk GD, Jaume JC, McLachlan SM. The thyrotropin (TSH) receptor: interaction with TSH and autoantibodies [erratum 1999, 20:100] Endocr Rev. 1998;19:673–716. doi: 10.1210/edrv.19.6.0352. [DOI] [PubMed] [Google Scholar]
- 8.Prabhakar BS, Fan JL, Seetharamaiah GS. Thyrotropin-receptor-mediated diseases: a paradigm for receptor autoimmunity. Immunol Today. 1997;18:437–442. doi: 10.1016/s0167-5699(97)01089-x. [DOI] [PubMed] [Google Scholar]
- 9.Wagle NM, Patibandla SA, Dallas JS, Morris JC, Prabhakar BS. Thyrotropin receptor-specific antibodies in BALB/cJ mice with experimental hyperthyroxinemia show a restricted binding specificity and belong to the immunoglobulin G1 subclass. Endocrinology. 1995;136:3461–3469. doi: 10.1210/endo.136.8.7628382. [DOI] [PubMed] [Google Scholar]
- 10.Costagliola S, et al. Recombinant thyrotropin receptor and the induction of autoimmune thyroid disease in BALB/c mice: a new animal model. Endocrinology. 1994;135:2150–2159. doi: 10.1210/endo.135.5.7956939. [DOI] [PubMed] [Google Scholar]
- 11.Carayanniotis G, et al. Unaltered thyroid function in mice responding to a highly immunogenic thyrotropin receptor: implications for the establishment of a mouse model for Graves’ disease. Clin Exp Immunol. 1995;99:294–302. doi: 10.1111/j.1365-2249.1995.tb05548.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang SH, et al. Induction of thyroiditis in mice with thyrotropin receptor lacking serologically dominant regions. Clin Exp Immunol. 1998;113:119–125. doi: 10.1046/j.1365-2249.1998.00627.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Marion S, Braun JM, Ropars A, Kohn LD, Charreire J. Induction of autoimmunity by immunization of mice with human thyrotropin receptor. Cell Immunol. 1994;158:329–341. doi: 10.1006/cimm.1994.1280. [DOI] [PubMed] [Google Scholar]
- 14.Hidaka Y, et al. Production of thyroid-stimulating antibodies in mice by immunization with T-cell epitopes of human thyrotropin receptor. Endocrinology. 1995;136:1642–1647. doi: 10.1210/endo.136.4.7534706. [DOI] [PubMed] [Google Scholar]
- 15.Costagliola S, Rodien P, Many MC, Ludgate M, Vassart G. Genetic immunization against the human thyrotropin receptor causes thyroiditis and allows production of monoclonal antibodies recognizing the native receptor. J Immunol. 1998;160:1458–1465. [PubMed] [Google Scholar]
- 16.Wagle NM, et al. Induction of hyperthyroxinemia in BALB/C but not in several other strains of mice. Autoimmunity. 1994;18:103–112. doi: 10.3109/08916939409007983. [DOI] [PubMed] [Google Scholar]
- 17.Kita M, et al. Regulation and transfer of a murine model of thyrotropin receptor antibody mediated Graves’ disease. Endocrinology. 1999;140:1392–1398. doi: 10.1210/endo.140.3.6599. [DOI] [PubMed] [Google Scholar]
- 18.Shimojo N, et al. Induction of Graves-like disease in mice by immunization with fibroblasts transfected with the thyrotropin receptor and a class II molecule. Proc Natl Acad Sci USA. 1996;93:11074–11079. doi: 10.1073/pnas.93.20.11074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Salamone MF, Mavournin KH. Bone marrow micronucleus assay: a review of the mouse stocks used and their published mean spontaneous micronucleus frequencies. Environ Mol Mutagen. 1994;23:239–273. doi: 10.1002/em.2850230402. [DOI] [PubMed] [Google Scholar]
- 20.Saha BK. Typing of murine major histocompatibility complex with a microsatellite in the class II Eb gene. J Immunol Methods. 1996;194:77–83. doi: 10.1016/0022-1759(96)00065-8. [DOI] [PubMed] [Google Scholar]
- 21.Saha BK, Shields JJ, Miller RD, Hansen TH, Shreffler DC. A highly polymorphic microsatellite in the class II Eb gene allows tracing of major histocompatibility complex evolution in mouse [erratum 1993, 90:8757] Proc Natl Acad Sci USA. 1993;90:5312–5316. doi: 10.1073/pnas.90.11.5312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Peng SL, Craft J. PCR-RFLP genotyping of murine MHC haplotypes. Biotechniques. 1996;21:362, 366–362, 368. doi: 10.2144/96213bm03. [DOI] [PubMed] [Google Scholar]
- 23.Sambrook, J., Fritsch, E.F., and Maniatis, T. 1989. Molecular cloning: a laboratory manual. Cold Spring Harbor Laboratory Press. Cold Spring Harbor, NY.
- 24.Perret J, et al. Stable expression of the human TSH receptor in CHO cells and characterization of differentially expressing clones. Biochem Biophys Res Commun. 1990;171:1044–1050. doi: 10.1016/0006-291x(90)90789-p. [DOI] [PubMed] [Google Scholar]
- 25.Weiss RE, et al. Thyrotropin regulation by thyroid hormone in thyroid hormone receptor beta-deficient mice. Endocrinology. 1997;138:3624–3629. doi: 10.1210/endo.138.9.5412. [DOI] [PubMed] [Google Scholar]
- 26.Johnstone AP, Cridland JC, DaCosta CR, Harfst E, Shepherd PS. Monoclonal antibodies that recognize the native human thyrotropin receptor. Mol Cell Endocrinol. 1994;105:R1–R9. doi: 10.1016/0303-7207(94)90175-9. [DOI] [PubMed] [Google Scholar]
- 27.Harfst E, Ross MS, Nussey SS, Johnstone AP. Production of antibodies to the human thyrotropin receptor and their use in characterising eukaryotically expressed functional receptor. Mol Cell Endocrinol. 1994;102:77–84. doi: 10.1016/0303-7207(94)90100-7. [DOI] [PubMed] [Google Scholar]
- 28.Tomer Y, Davies TF. The genetic susceptibility to Graves’ disease. Baillieres Clin Endocrinol Metab. 1997;11:431–450. doi: 10.1016/s0950-351x(97)80678-7. [DOI] [PubMed] [Google Scholar]
- 29.Brix TH, Kyvik KO, Hegedus L. What is the evidence of genetic factors in the etiology of Graves’ disease? A brief review [erratum 1998, 8:1079] Thyroid. 1998;8:727–734. doi: 10.1089/thy.1998.8.727. [DOI] [PubMed] [Google Scholar]
- 30.Many MC, et al. Development of an animal model of autoimmune thyroid eye disease. J Immunol. 1999;162:4966–4974. [PubMed] [Google Scholar]
- 31.Kaithamana S, Fan J, Osuga Y, Liang SG, Prabhakar BS. Induction of experimental autoimmune Graves’ Disease in BALB/c mice. J Immunol. 1999;163:5157–5164. [PubMed] [Google Scholar]