Abstract
Background
A few studies focused on open reduction and internal fixation (ORIF) or nonoperative treatment of displaced 3-part or 4-part proximal humeral fractures in elderly patients have been published, all of whom had a low number of patients. In this meta-analysis of randomized controlled trials (RCTs), we aimed to assess the effect of ORIF or nonoperative treatment of displaced 3-part or 4-part proximal humeral fractures in elderly patients on the clinical outcomes and re-evaluate of the potential benefits of conservative treatment.
Methods
We searched PubMed and the Cochrane Central Register of Controlled Trials databases for randomized controlled trials comparing ORIF and nonoperative treatment of displaced 3-part or 4-part proximal humeral fractures in elderly patients. Our outcome measures were the Constant scores.
Results: Three randomized controlled trials with a total of 130 patients were identified and analyzed. The overall results based on fixed-effect model did not support the treatment of open reduction and internal fixation to improve the functional outcome when compared with nonoperative treatment for treating elderly patients with displaced 3-part or 4-part proximal humeral fractures (WMD −0.51, 95% CI: −7.25 to 6.22, P = 0.88, I2 = 0%).
Conclusions
Although our meta-analysis did not support the treatment of open reduction and internal fixation to improve the functional outcome when compared with nonoperative treatment for treating elderly patients with displaced 3-part or 4-part proximal humeral fractures, this result must be considered in the context of variable patient demographics. Only a limited recommendation can be made based on current data. Considering the limitations of included studies, a large, well designed trial that incorporates the evaluation of clinically relevant outcomes in participants with different underlying risks of shoulder function is required to more adequately assess the role for ORIF or nonoperative treatment.
Introduction
Proximal humeral fracture is one of the most frequent osteoporotic fractures in the elderly people, accounting for 6% of all fractures seen in accident and emergency departments[1]–[3]. Most proximal humeral fractures are undisplaced or minimally displaced[4] and can be treated successfully nonoperatively[5]. The most frequently used classification for proximal humeral fractures is the Neer classification[6], [7] which is based on the 4 anatomical segments of the proximal humerus (the humeral head, shaft, greater and lesser tubercles) and whether these segments are fractured and displaced.
According to Neer classification, 3-part and 4-part proximal humeral fractures are comminuted displaced fractures which represent 13% to 16% of all proximal humeral fractures[1]. Operative treatment of these fractures in younger patients is not controversial. The main controversy pertains to elderly patients with varying degrees of osteoporosis and 3-part or 4-part proximal humeral fractures after low-energy trauma. Whether these fractures need surgery or not, remains controversial.
A few studies[8]–[10] focused on open reduction and internal fixation (ORIF) or nonoperative treatment of displaced 3-part or 4-part proximal humeral fractures in elderly patients have been published, all of whom had a low number of patients. In this meta-analysis of randomized controlled trials (RCTs), we aimed to assess the effect of ORIF or nonoperative treatment of displaced 3-part or 4-part proximal humeral fractures in elderly patients on the clinical outcomes and re-evaluate of the potential benefits of conservative treatment.
Materials and Methods
Search strategy
The literature search was performed on PubMed (1966- October 2012), and the Cochrane Central Register of Controlled Trials (1996 to October 2012). We used the following search terms in different combinations as MeSH (Medical Subject Heading) terms and as text words: Proximal humeral fracture, internal fixation, treatment outcome, surgery and comparative study. We did not restrict by language or type of article. To identify other relevant studies, we manually scanned reference lists from identified trials and review articles, and we also searched conference proceedings. We requested original data by directly contacting authors.
Study selection
We included studies when the following criteria were met: (1) randomized, controlled trials assessing treatment for displaced 3-part or 4-part proximal humeral fractures in elderly patients; (2) the intervention was open reduction and internal fixation versus nonoperative treatment; (3) studies reported the the outcome measure of the Constant score in both arms. The primary outcome measure was the Constant score, which is the most often used functional score as an outcome measure in studies of proximal humeral fractures[11]. Secondary outcome measures were nonunion, avascular necrosis (AVN) of humeral head and osteoarthritis.
Data extraction and quality assessment
Data were collected independently by 2 reviewers. Extracted data included patient characteristics (mean age, female rate); inclusion criteria; protocol for the treatment of fractures; Constant score and complications. Quality assessment was judged on concealment of treatment allocation; similarity of both groups at baseline regarding prognostic factors; eligibility criteria; blinding of outcome assessors, care providers, and patients; completeness of follow-up; and intention-to-treat analysis[12]. We quantified study quality by using the Jadad score[13]. A third reviewer adjudicated any disagreement about extracted data. Then data were checked and entered into the Review Manager (Version 5.0. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2008) database for further analysis.
Statistical analysis
Continuous variable (the Constant Score) was analysed using the weighted mean differences (WMD) with its 95% CI, whereas dichotomous data (nonunion, avascular necrosis of humeral head, and osteoarthritis) were analyzed using the risk ratio (RR) measure and its 95% confidence interval (CI). Moreover, heterogeneity across trials was evaluated with I2 statistic, which defined as I2>50%. If heterogeneity existed, a random-effect model was used to assess the overall estimate. Otherwise, a fixed-effect model was chosen. Sensitivity analyses (exclusion of one study at a time) were conducted to assess heterogeneity and robustness of pooled results. We assessed for potential publication bias by using the Begg adjusted-rank correlation test[14] and Egger regression asymmetry test[15]. All tests were two-tailed and a P value less than 0.05 was regarded as significant in this meta-analysis.
Results
Selected studies and characteristics
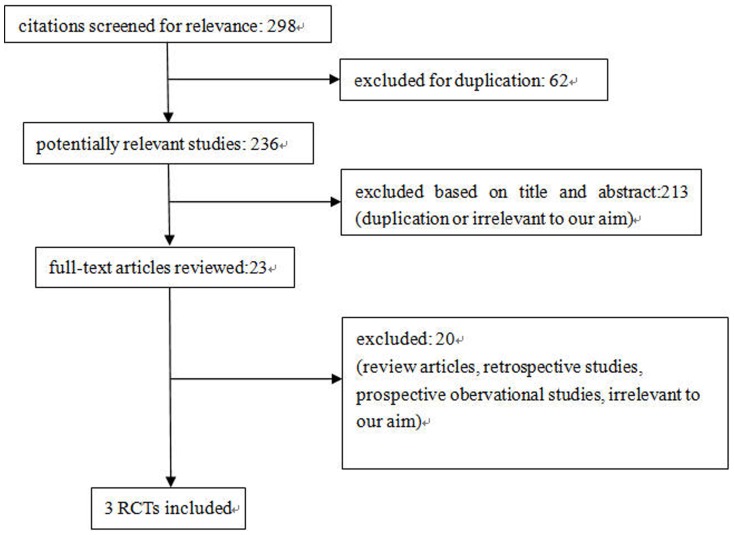
We identified 298 potentially relevant citations from the initial literature search. After independently reviewing the title and abstract of all potential articles, 23 articles were considered of interest and reviewed in full-text. Of these, 19 were excluded from the meta-analysis (review articles, retrospective studies, prospective obervational studies, irrelevant to our aim). Although the study carried out by Fjalestad Tore et al[9] did not provide data on the Standard Deviation (SD) of Constant score, we requested it by directly contacting the author. Therefore, three randomized controlled studies with a total of 130 elderly patients with displaced 3-part or 4-part proximal humeral fractures were identified and analyzed[8]–[10]. Our search strategy is outlined in Figure 1 .
Figure 1. Study selection diagram.
Table 1 and table 2 summarizes the characteristics of the included studies. One of them[8] was reported in 1997 and others[9], [10] were reported in the past two years. 64 subjects were assigned to open reduction and internal fixation group and 66 subjects were assigned to nonoperative treatment group. All studies involved patients with displaced 3-part or 4-part proximal humeral fractures who were aged 55 years or older. Most subjects were females. Open reduction and internal fixation in one study[8] was treated by tension-band and in other two studies[9], [10] were treated by locking plate. Nonoperative treatment in three studies were almost same. The proportion of patients lost to follow-up was very high (27.5%) in the study carried out by Zyto Karol et al[8] and less than 10% in other two studies[9], [10]. Constant score was calculated in each study as the shoulder function outcome measure. Although the study carried out by Fjalestad Tore et al[9] did not provide data on the SD of Constant score, we requested it by directly contacting the author. The quality characteristics of the studies were shown in table 3 .
Table 1. Characteristics of included studies.
| Author, year | Patients,n | Female proportion in each group,% | Mean age,y | Three-part | Inclusion criteria | ||||
| Surgical | Conservative | Surgical | Conservative | Surgical | Conservative | Surgical | Conservative | ||
| Zyto K, 1997 | 14 | 15 | 90 | 85 | 73 | 75 | 19 | 18 | A displaced three- or four-part fracture of the humerus not caused by high-energy trauma and not pathological; at least 30% contact between the humeral head and the humeral shaft; no other fractures elsewhere in the upper limbs; no concomitant disease likely to influence the end result; and ability of the patient to co-operate |
| Fjalestad T, 2011 | 23 | 25 | 80 | 96 | 72.2 | 73.1 | \ | \ | Patients aged 60+ years with a displaced, unstable three- or four-part proximal humerus fracture of OTA group 11-B2 or 11-C2 (displaced fracture of extra-articular or articular, bifocal type) were included in this study |
| Olerud P, 2011 | 27 | 26 | 80 | 83 | 72.9 | 74.9 | 30 | 30 | A displaced 3-part fracture of the proximal humerus in elderly patients. The patient inclusion criteria were age 55 or older, a fracture sustained after a low-energy trauma (ie, simple fall), no previous shoulder problems, independent living conditions (ie, not institutionalized), and no severe cognitive dysfunction (ie, 3 correct answers on a 10-item Short Portable Mental Status Questionnaire [SPMSQ]). |
Table 2. Characteristics of included studies-continued.
| Surgical treatment | Conservative treatment | Constant score | Complications | Follow-up time | ||
| Surgical | Conservative | Surgical | Conservative | |||
| Tension-band surgery | Conservative treatment | 60±19 | 65±15 | AVN 1, nonunion 1, osteoarthritis 4 | osteoarthritis 2 | 50 months |
| Open reduction and internal fixation using an angular stable plate and cerclages | Standardized nonoperative treatment | 52.3±20.9 | 52.2±18.3 | AVN 8, nonunion 0 | AVN 13, nonunion 2 | 1 year |
| ORIF with a locking plate | Nonoperative treatment | 61±19.2 | 58.4±23.1 | AVN 3, nonunion 1, osteoarthritis 0 | nonunion 1, AVN 2, osteoarthritis 1 | 2 years |
Table 3. Quality of included RCTs.
| Author, year | Jadad Score | Allocation Concealment | Similarity of Baseline Characteristics | Eligibility Criteria | Blinding | Completeness of Follow-up | Intention-to-Treat Analysis | ||
| Outcome Assessor | Care Provider | Patient | |||||||
| Zyto K, 1997 | 1+0+1 | YES | YES | YES | YES | NS | NS | YES | NS |
| Fjalestad T, 2011 | 2+0+1 | YES | YES | YES | NO | NS | NS | YES | YES |
| Olerud P, 2011 | 1+0+1 | NS | YES | YES | YES | NS | NS | YES | YES |
NS = not specified or available.
Effects of ORIF vs nonoperative treatment
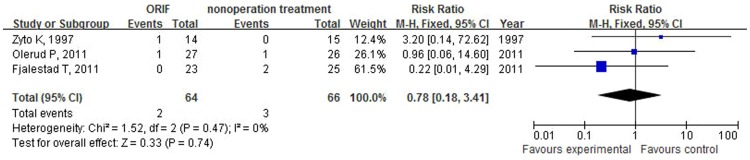
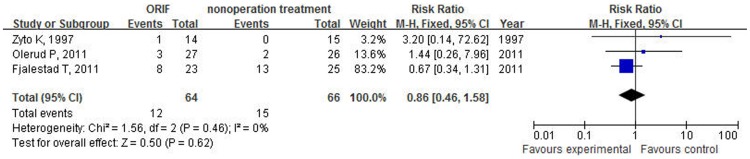
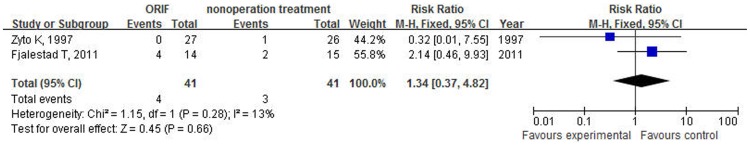
Three studies[8]–[10] that included 130 cases provided data on Constant score. The overall results based on fixed-effect model did not support the treatment of open reduction and internal fixation to improve the functional outcome when compared with nonoperative treatment for treating elderly patients with displaced 3-part or 4-part proximal humeral fractures (WMD −0.51, 95% CI: −7.25 to 6.22, P = 0.88, I2 = 0%, figure 2 ). Incidence of nonunion was low in both arms and there was not significant different after the use of ORIF compared with nonoperative treatment (RR = 0.78; 95% CI: 0.18–3.41, P = 0.74, I2 = 0%, figure 3 ). Nonoperative treatment was not associated with a significant reduction in risk of avascular necrosis of humeral head (RR = 0.86; 95% CI: 0.46–1.58, P = 0.62, I2 = 0%, figure 4 ). Two studies reported data on osteoarthritis, including 82 patients. Fractures receiving ORIF did not show more osteoarthritis than those receiving nonoperative treatment (RR = 1.34; 95% CI: 0.37–4.82, P = 0.66, I2 = 0%, figure 5 ).
Figure 2. Forest plot of mean difference and 95% confidence intervals (CI) for constant scores among patients assigned to ORIF versus nonoperative treatment.
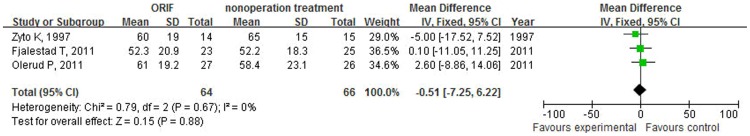
Figure 3. Forest plot of risk ratios and 95% confidence intervals (CI) for the incidence of nonunion among patients assigned to ORIF versus nonoperative treatment.
Figure 4. Forest plot of risk ratios and 95% confidence intervals (CI) for the incidence of AVN among patients assigned to ORIF versus nonoperative treatment.
Figure 5. Forest plot of risk ratios and 95% confidence intervals (CI) for the incidence of osteoarthritis among patients assigned to ORIF versus nonoperative treatment.
Assessment of publication bias using Egger's and Begg's tests showed that no potential publication bias existed among the included trials (Egger's test: p>0.05; Begg's test: p>0.05).
Discussion
To our knowledge, this is the first meta-analysis of randomized controlled trials comparing open reduction and internal fixation and nonoperative in the treatment of displaced 3-part or 4-part proximal humeral fractures in elderly patients. This meta-analysis was based on 3 randomized controlled trials that included 64 fractures treated with ORIF and 66 fractures treated with nonoperative. The outcomes investigated were shoulder function (Constant Score), nonunion, avascular necrosis and osteoarthritis. Our results failed to show beneficial effects of ORIF on the shoulder function measured by Constant score, on the risk of nonunion, avascular necrosis of humeral head or osteoarthritis, compared with nonoperative treatment. Because of poor number included among these studies, a large definitive RCT is needed.
Almost 40 years ago, early mobilisation was attentioned by orthopedic doctors. With the development of better fixation devices, open reduction and internal fixation in treating elderly patients with displaced 3-part or 4-part proximal humeral fractures is increasingly popular. There are several predictors of success with surgical treatment of a proximal humeral fracture such as careful soft tissue management, anatomic reduction, and proper plate placement. However, we surgeons can not controll everything. For instance, primary devascularization of the head fragments resulting from the injury itself, particularly in severely displaced Type B fractures and in most displaced C fractures, is an important problem that cannot be controlled[16]. In this meta-analysis, open reduction and internal fixation in one study[8] was treated by tension-band and in other two studies[9], [10] were treated by locking plate. We did not find better shoulder function, lower rate nonunion, higher rate avascular necrosis of humeral head and higher rate osteoarthritis, compared with nonoperative treatment. This may be explained partly by above predictors.
In addition to open reduction and internal fixation, shoulder arthroplasty might be an alternative surgical method for treating elderly patients with displaced 3-part or 4-part proximal humeral fractures. Three different arthroplasty are available: hemiarthroplasty (HAS), total shoulder arthroplasty (TSA) and reverse shoulder arthroplasty (RSA). HAS and TSA are indicated for patients with intact rotator cuffs. RSA is indicated for elderly patients with massive irreparable rotator cuff tears and is usually considered as a ‘‘last chance’’ possible surgery for a functional shoulder[17], [18]. For these elderly displaced 3-part or 4-part proximal humeral fracture patients with seriously rotator cuff tears, RSA should be a suitable method instead of ORIF which might have been used in these patients with poor shoulder function. Although RSA shoulders have showed better functional improvement in a limited number of studies, they have also demonstrated higher complication rates[19]–[21]. Moreover, the RSA shoulder implant is also markedly more expensive than other methods'. Because of these, cost-effectiveness analysis can be used to evaluate the decision about which arthroplasty or ORIF is preferred and related study is needed to be carried out.
Recent studies have shown the significant complication rate associated with operative treatment of above injuries[22], [23]. As such, nonoperative treatment has been re-emphasized these days. Yuksel HY et al[24] carried out a study to evaluate the results of nonoperative treatment of three- and four-part fractures of the proximal humerus in patients who refused surgery or could not undergo surgery because of medical conditions and found satisfactor results either in younger or elderly patients. Iyengar JJ et al[25] did a systematic review of nonoperative management of proximal humerus fractures which demonstrated high rates of radiographic healing, good functional outcomes, and a modest complication rate. Patients with nonoperative treatment in the studies included in our meta-analysis all received standardized treatment. We did not found a significant difference compared with ORIF treatment, which is in line with previous studies.
The updated Cochrane meta-analysis published in 2012 was unable to provide guidelines for treating proximal humerus fractures due to a lack of solid evidence. Indeed, meta-analysis of Handoll et al published in 2012 is a detailed, wide and good paper. In this paper, the authors gave us lots of data about interventions for treating proximal humeral fractures in adults, such as comparison of early mobilisation versus immobilisation for 3 weeks, comparison of surgery versus conservative treatment, comparison of locking plate versus locking intramedullary nail and comparison of hemi-arthroplasty versus tension band wiring and so on. However, our meta-analysis is specifically focused on the problem of ORIF vs non operative treatment for treating elderly patients with displaced 3-part or 4-part proximal humeral fractures. We analyzed the data and made the recommendation and this may be a reference for our clinical doctors that we can consider conservative treatment instead of ORIF.
There are several potential limitations in this meta-analysis. Firstly, one prominent drawback pertinent to this study is that only three RCTs with 130 subjects were included in this meta-analysis; the results of pooled analysis might therefore be accompanied with bias. Secondly, although all included studies reported the Constant score, few trials designed to investigate the effect of ORIF on some clinical outcomes such as malunion, osteoarthritis, axillary nerve injury and infections. Finally, we did not have access to patient-level data to determine whether the risk factors (eg, gender and age) could influence the effect of open reduction and internal fixation on the shoulder function.
In conclusion, although our meta-analysis did not support the treatment of open reduction and internal fixation to improve the functional outcome when compared with nonoperative treatment for treating elderly patients with displaced 3-part or 4-part proximal humeral fractures, this result must be considered in the context of variable patient demographics. Only a limited recommendation can be made based on current data. Considering the limitations of included studies, a large, well designed trial that incorporates the evaluation of clinically relevant outcomes in participants with different underlying risks of shoulder function is required to more adequately assess the role for ORIF or nonoperative treatment.
Supporting Information
PRISMA Checklist
(DOC)
PRISMA Flow Diagram
(DOC)
Acknowledgments
We thank Fjalestad Tore who provided additional data to conduct this analysis.
Funding Statement
This work was supported by grants from the National Natural Science Foundation of China (30973054, 81171161). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Horak J, Nilsson BE (1975) Epidemiology of fracture of the upper end of the humerus. Clin Orthop Relat Res (112): 250–3. [PubMed] [Google Scholar]
- 2. Bengner U, Johnell O, Redlund-Johnell I (1988) Changes in the incidence of fracture of the upper end of the humerus during a 30-year period. A study of 2125 fractures. Clin Orthop Relat Res (231): 179–82. [PubMed] [Google Scholar]
- 3. Court-Brown CM, Caesar B (2006) Epidemiology of adult fractures: A review. Injury 37(8): 691–7. [DOI] [PubMed] [Google Scholar]
- 4. Court-Brown CM, Garg A, McQueen MM (2001) The epidemiology of proximal humeral fractures. Acta Orthop Scand 72(4): 365–71. [DOI] [PubMed] [Google Scholar]
- 5. Gaebler C, McQueen MM, Court-Brown CM (2003) Minimally displaced proximal humeral fractures: epidemiology and outcome in 507 cases. Acta Orthop Scand 74(5): 580–5. [DOI] [PubMed] [Google Scholar]
- 6. 2nd NCS (1970) Displaced proximal humeral fractures. I. Classification and evaluation. J Bone Joint Surg Am 52(6): 1077–89. [PubMed] [Google Scholar]
- 7. 2nd NCS (1970) Displaced proximal humeral fractures. II. Treatment of three-part and four-part displacement. J Bone Joint Surg Am 52(6): 1090–103. [PubMed] [Google Scholar]
- 8. Zyto K, Ahrengart L, Sperber A, Tornkvist H (1997) Treatment of displaced proximal humeral fractures in elderly patients. J Bone Joint Surg Br 79(3): 412–7. [DOI] [PubMed] [Google Scholar]
- 9. Fjalestad T, Hole MO, Hovden IA, Blucher J, Stromsoe K (2012) Surgical treatment with an angular stable plate for complex displaced proximal humeral fractures in elderly patients: a randomized controlled trial. J Orthop Trauma 26(2): 98–106. [DOI] [PubMed] [Google Scholar]
- 10. Olerud P, Ahrengart L, Ponzer S, Saving J, Tidermark J (2011) Internal fixation versus nonoperative treatment of displaced 3-part proximal humeral fractures in elderly patients: a randomized controlled trial. J Shoulder Elbow Surg 20(5): 747–55. [DOI] [PubMed] [Google Scholar]
- 11. Kontakis G, Koutras C, Tosounidis T, Giannoudis P (2008) Early management of proximal humeral fractures with hemiarthroplasty: a systematic review. J Bone Joint Surg Br 90(11): 1407–13. [DOI] [PubMed] [Google Scholar]
- 12. Verhagen AP, de Vet HC, de Bie RA, Kessels AG, Boers M, et al. (1998) The Delphi list: a criteria list for quality assessment of randomized clinical trials for conducting systematic reviews developed by Delphi consensus. J Clin Epidemiol 51(12): 1235–41. [DOI] [PubMed] [Google Scholar]
- 13. Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, et al. (1996) Assessing the quality of reports of randomized clinical trials: is blinding necessary. Control Clin Trials 17(1): 1–12. [DOI] [PubMed] [Google Scholar]
- 14. Begg CB, Mazumdar M (1994) Operating characteristics of a rank correlation test for publication bias. Biometrics 50(4): 1088–101. [PubMed] [Google Scholar]
- 15. Egger M, Davey SG, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315(7109): 629–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hertel R, Hempfing A, Stiehler M, Leunig M (2004) Predictors of humeral head ischemia after intracapsular fracture of the proximal humerus. J Shoulder Elbow Surg 13(4): 427–33. [DOI] [PubMed] [Google Scholar]
- 17. Boileau P, Watkinson D, Hatzidakis AM, Hovorka I (2006) Neer Award 2005: The Grammont reverse shoulder prosthesis: results in cuff tear arthritis, fracture sequelae, and revision arthroplasty. J Shoulder Elbow Surg 15(5): 527–40. [DOI] [PubMed] [Google Scholar]
- 18. Grammont PM, Baulot E (1993) Delta shoulder prosthesis for rotator cuff rupture. Orthopedics 16(1): 65–8. [DOI] [PubMed] [Google Scholar]
- 19.Boileau P, Watkinson DJ, Hatzidakis AM, Balg F (2005) Grammont reverse prosthesis: design, rationale, and biomechanics. J Shoulder Elbow Surg 14(1 Suppl S): 147S–161S. [DOI] [PubMed]
- 20. Frankle M, Siegal S, Pupello D, Saleem A, Mighell M, et al. (2005) The Reverse Shoulder Prosthesis for glenohumeral arthritis associated with severe rotator cuff deficiency. A minimum two-year follow-up study of sixty patients. J Bone Joint Surg Am 87(8): 1697–705. [DOI] [PubMed] [Google Scholar]
- 21. Sirveaux F, Favard L, Oudet D, Huquet D, Walch G, et al. (2004) Grammont inverted total shoulder arthroplasty in the treatment of glenohumeral osteoarthritis with massive rupture of the cuff. Results of a multicentre study of 80 shoulders. J Bone Joint Surg Br 86(3): 388–95. [DOI] [PubMed] [Google Scholar]
- 22. Thalhammer G, Platzer P, Oberleitner G, Fialka C, Greitbauer M, et al. (2009) Angular stable fixation of proximal humeral fractures. J Trauma 66(1): 204–10. [DOI] [PubMed] [Google Scholar]
- 23. Südkamp N, Bayer J, Hepp P, Voigt C, Oestern H (2009) Open reduction and internal fixation of proximal humeral fractures with use of the locking proximal humerus plate. Results of a prospective, multicenter, observational study. J Bone Joint Surg Am 91(6): 1320–8. [DOI] [PubMed] [Google Scholar]
- 24. Yuksel HY, Yimaz S, Aksahin E, Celebi L, Muratli HH, et al. (2011) The results of nonoperative treatment for three- and four-part fractures of the proximal humerus in low-demand patients. J Orthop Trauma 25(10): 588–95. [DOI] [PubMed] [Google Scholar]
- 25. Iyengar JJ, Devcic Z, Sproul RC, Feeley BT (2011) Nonoperative treatment of proximal humerus fractures: a systematic review. J Orthop Trauma 25(10): 612–7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
PRISMA Checklist
(DOC)
PRISMA Flow Diagram
(DOC)