Abstract
Bacterial and viral infection of the intraparotideal and periparotideal lymph nodes, or of the glandular parenchyma, can lead to inflammatory and subsequently suppurative changes, which can result in abscess formation. Sonography allows a detailed morphological evaluation of the gland and has an important value, complementary to clinical examination, in the study of parotid inflammatory diseases. Specifically, sonography defines lesion’s characteristics and, in a large number of cases, also its nature and, among the various imaging techniques, it is considered first-line imaging for the evaluation of parotid abscesses, which are characterized by hypo-anechoic lesions, with irregular margins. Color Doppler signals are peripheral to the abscess. If combined with color Doppler, sonography is important not only in diagnosis, but also in the evaluation of therapeutic efficacy and as a guide to the aspiration and drainage of abscesses. The rarity of some of these lesions led us to publish this mini-pictorial essay.
Keywords: Salivary glands, Sonography, Abscess
Riassunto
Le infezioni batteriche e virali dei linfonodi intraparotidei e periparotiedei, o del parenchima ghiandolare, provocano una risposta infiammatoria e successivamente possono portare a suppurazione e a formazione di ascessi. L’ecografia consente di effetuare una valutazione morfologica dettagliata della ghiandola ed ha un valore importante, complementare all’esame clinico, nello studio delle malattie infiammatorie parotidee, poichè permette di definire le caratteristiche della lesione e, in un gran numero di casi, anche la loro natura; di conseguenza, tra le diverse metodiche di imaging, l’ecografia viene considerata quella di primo livello per lo studio degli ascessi parotidei, che si presentano come lesioni ipo-anecogene, con margini irregolari. La valutazione mediante color-Doppler mostra la presenza di segnali periferici alla lesione ascessuale. Oltre all’importanza per la diagnosi, l’ecografia, in combinazione con il color-Doppler, è utile nel follow-up e per guidare gli esami bioptici ed il drenaggio delle lesioni. Poichè alcune di queste lesioni sono rare, abbiamo deciso di pubblicare questo mini-pictorial essay.
Introduction
An infection of the parotid gland, a major salivary gland localized in the retromandibular fossa, can arise from ascending infection via Stensen’s duct, or from bacteraemia or viremia.
Bacterial and (more rarely) viral infection of the intraparotideal and periparotideal lymph nodes, or of the glandular parenchyma, can lead to suppurative changes, which can result in abscess formation. If the process continues pus penetrates the capsule and invades the surrounding tissue, and extends downward into the deep fascial planes of the neck, backward into the external auditory canal, or outward into the facial skin [1].
The most common pathogen associated with acute bacterial parotitis and head and neck abscesses is Staphylococcus aureus both in adults, and in pediatrics patients [2], while in infant recurrent parotitis, Streptococcus spp are the most recurrent isolated organisms [3]. Other infection-inducing pathogens reported in literature include Streptococcus, Hemophilus, Pseudomonas, Mycobacterium tuberculosis, anaerobic bacteria and others.
Even in the post-vaccine era, epidemic mumps caused by paramyxovirus is the most frequent viral cause of parotitis in childhood. Other viral agents associated with parotid infection are coxsackie viruses, Epstein Barr virus, influenza A virus, lymphocytic-choriomeningitis virus, para-influence viruses, herpes simplex virus, and cytomegalovirus [4].
The predisposing conditions and precipitating factors include: dehydration, poor oral hygiene, dental infection, oral trauma, xerostomia, ductal obstruction, certain drugs (anticholinergics and antihistamines), certain chronic diseases (Sjogren’s syndrome and diabetes mellitus), malnutrition, pre-existing parotid Warthin’s tumor, immunosuppression, and sialolithiasis [4].
An acute infection of the parotid gland is characterized by variety of symptoms such as the sudden onset of erythematous swelling in parotideal region, pain, fever, facial asymmetry, facial nerve palsy, and less frequently, pus/blood in the oral cavity and dysphagia.
Acute inflammation frequently evolves into abscesses, which are characterized by liquid or semiliquid content and sometimes gives rise to a fistula toward either the surface or the deepest layers of the gland.
A parotid abscess, in some cases, can be a life threatening disease, as the inflammation can spread to the head and neck causing the formation of abscesses in these zones [5].
Tuberculosis of the parotid gland is a rare clinical entity even in countries where the disease is endemic [6, 7]. Clinically, it generally presents as a localized, unilateral, slow-growing parotid mass with a certain degree of fixation indistinguishable from salivary gland tumors [8], in this cases the histopathological examination is characterized by tuberculoid granulomas, with caseous necrosis, Langhans giant cells and epithelioid cells.
US appearance
Among the various imaging modalities, sonography is considered first-line imaging for the evaluation of the parotid gland as, thanks to its superficial position, most parts are accessible by high-frequency linear probes (9–18 MHz) and only a little portion of the parotid gland may be hidden by the acoustic shadow of the mandible. Routine US examination is performed with the patient in the supine position, it include transverse and longitudinal scans over the mandibular angle covering the preauricular, infraauricular, retroauricular and cervical regions; it is crucial to examine the gland bilaterally because some diseases may occur bilaterally, or for comparison.
The parotid gland, which is localized in the retromandibular fossa, is divided into superficial and deep lobes by a plane at the level of the facial nerve, which is not normally visualized with ultrasound, although its position can be inferred as it lies just lateral to the main intraparotid vessels, which are readily identified. Usually, the normal intraglandular ducts and the main duct (Stenson’s duct) are rarely visualized even with high-frequency transducers in a non-dilated status. The echo structure of the gland is usually homogeneous and the echogenicity is similar to that of the thyroid gland. Very frequently in the parotid parenchyma can be observed normal lymph nodes, which appear elliptical and hypoechoic with a hyperechoic, fatty, central hilum.
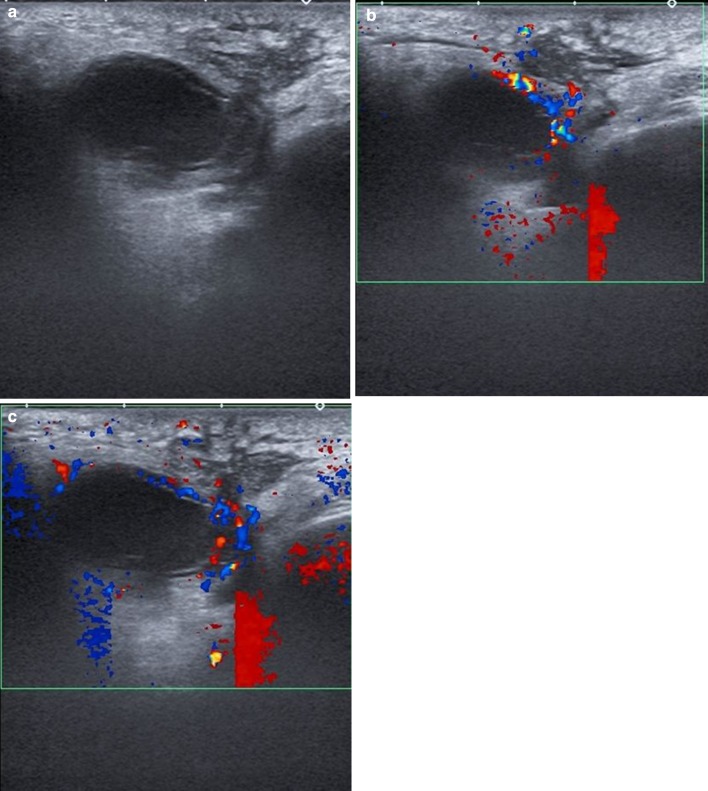
When a parotid inflammatory process is occurring, the gland sonographically appears increased in volume. The boundaries of the gland are slightly faded and the parenchyma is dishomogeneously hypoechoic due to the edematous state of the parenchyma. The abscessual evolution of the inflammation is characterized by hypo-anechoic lesion, with irregular margins (Fig. 1a).
Fig. 1.
Parotid abscess. Ultrasonography shows a hypo-anechoic lesion, with irregular margins (a) and peripheral hypervascularity was detected on color Doppler examination (b, c)
An important signal of the above-mentioned inflammatory state is the appearance of vessels with a linear and reasonably regular path which subsequently becomes more irregular and characterized by numerous anastomoses, which can be highlighted by the increase in intensity of the Color Doppler signal. In the abscessual forms, the Color Doppler signal have a peripheral typology, as in this case the vessels entwine in the area which is peripheral to the abcess (Fig. 1b, c).
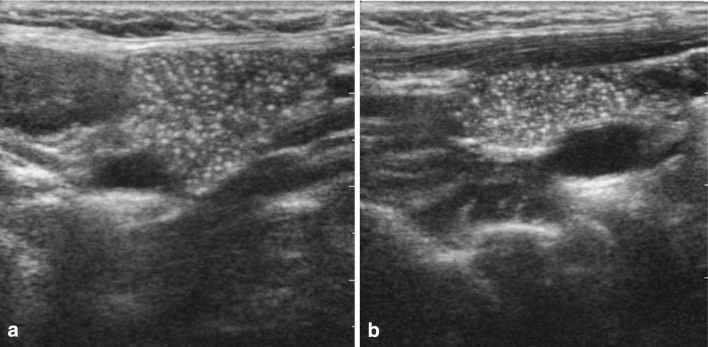
Another important aspect is the presence of enlarged lymph nodes with characters of reactivity; in advanced stages may appear areas of necrosis (Fig. 2).
Fig. 2.
Parotid abscess surrounded by lymph nodes, partially necrotic. Ultrasonography shows a hypo-anechoic lesion, with irregular margins (a, b), surrounded by lymph nodes with anechoic areas of necrosis. Color Doppler (c) examination detects hypervascularity in and around the lymph nodes
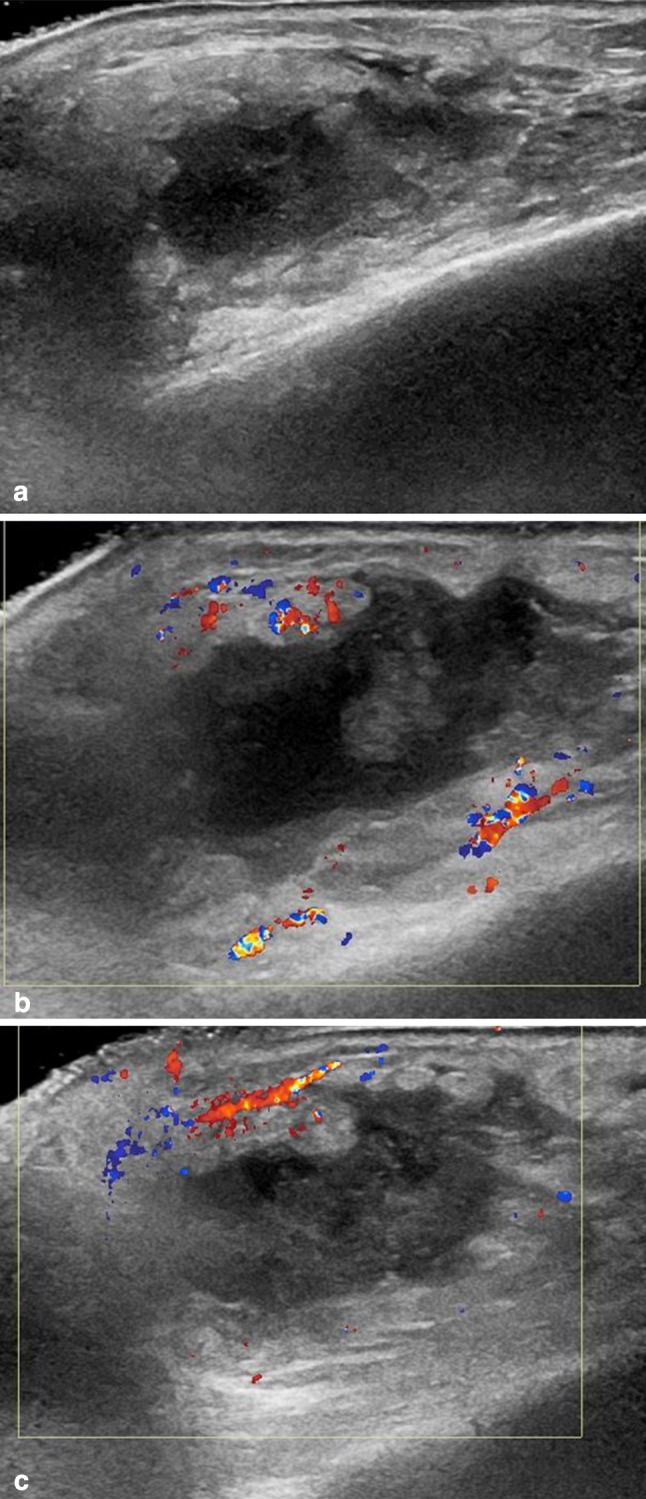
Frequently, the abscessual evolution gives rise to a fistula towards the surface (Fig. 3).
Fig. 3.
Abscess with fistula reaches the skin tissue. Ultrasonography showed a hypo-anechoic collection, with irregular margins of the parotid, with fistula reaches the skin tissue, surrounded by edema (a). Color Doppler examination detects perilesional hypervascularization and hypervascularization of the soft tissue surrounding the fistula (b, c)
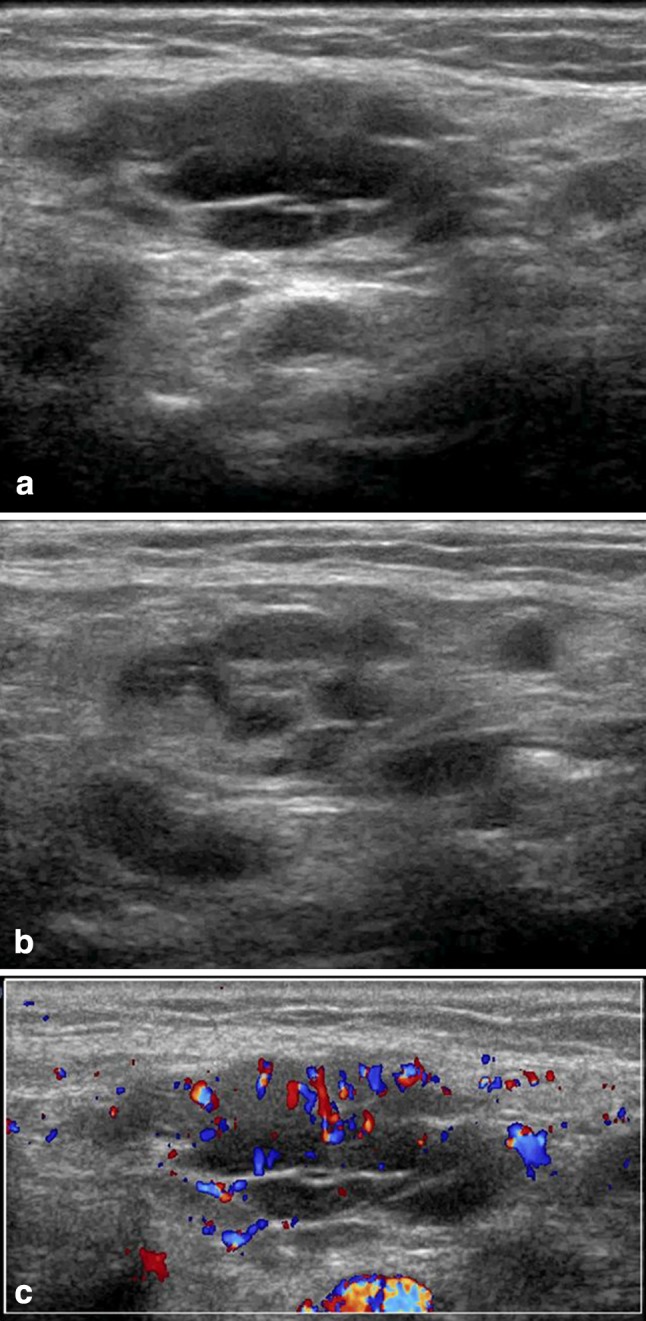
Sonographic findings, in case of tubercular abscess, are characterized by an enlarged parotid gland that shows a focal lesion, with pseudo-solid, inhomogeneous, appearance, and fairly regular margins (caseous necrosis) (Fig. 4).
Fig. 4.
Tubercular abscess. The ultrasound shows a lesion within the parotid parenchyma, with pseudo-solid, inhomogeneous appearance, and fairly regular margins (caseous necrosis)
Discussion and conclusions
Among the different imaging methods used for the study of the parotid gland, sonography represents the method of most frequent use, for its non-invasiveness, the wide distribution, rapid and easy to perform and the low cost. It allows a detailed morphological evaluation of the gland and has an important value, complementary to clinical examination, in the study of parotid inflammatory diseases, defining the characteristics of the lesion and, in a large number of cases, also its nature. In addition, ultrasound is also useful in the evaluation of treatment results and it is used to guide aspiration and drainage of abscesses.
Conflict of interest
None.
References
- 1.Krippaehne WW, Hunt TK, Dunphy JE. Acute suppurative parotitis: a study of 161 cases. Ann Surg. 1962;156:251–257. doi: 10.1097/00000658-196208000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nusem-Horowitz S, Wolf M, Coret A, Kronenberg J. Acute suppurative parotitis a parotid abscess in children. Int J Pediatr Otorhinolayngol. 1995;32:123–127. doi: 10.1016/0165-5876(94)01120-M. [DOI] [PubMed] [Google Scholar]
- 3.Giglio MS, Landaeta M, Pinto ME. Microbiology of recurrent parotitis. Pediatr Infect Dis J. 1997;16(4):386–390. doi: 10.1097/00006454-199704000-00010. [DOI] [PubMed] [Google Scholar]
- 4.Tan VE, Goh BS. Parotis abscess: a five-year review—clinical presentation, diagnosis and management. J Laryngol Otol. 2007;121:872–879. doi: 10.1017/S0022215106004166. [DOI] [PubMed] [Google Scholar]
- 5.Kishore R, Ramachandran K, Ngoma C, Morgan NJ. Unusual complication of parotid abscess. J Laryngol Otol. 2004;118:388–390. doi: 10.1258/002221504323086642. [DOI] [PubMed] [Google Scholar]
- 6.Prasad KC, Sreedharan S, Chakravarthy Y, Prasad SC. Tuberculosis in the head and neck: experience in India. J Laryngol Otol. 2007;121:979–985. doi: 10.1017/S0022215107006913. [DOI] [PubMed] [Google Scholar]
- 7.Oudidi A, Ridal M, Hachimi H, El Alami MN. Tuberculosis of the parotid gland. Rev Stomatol Chir Maxillofac. 2006;107:152–155. doi: 10.1016/S0035-1768(06)77010-3. [DOI] [PubMed] [Google Scholar]
- 8.Sethi A, Sareen D, Sabherwal A, Malhotra V. Primary parotid tuberculosis: varied clinical presentations. Oral Dis. 2006;12:213–215. doi: 10.1111/j.1601-0825.2005.01182.x. [DOI] [PubMed] [Google Scholar]