Abstract
Uterine arteriovenous vascular malformations (UAVM) are uncommon vascular diseases, occurring during reproductive age. Patients affected by UAMVs usually present with recurrent pregnancy loss or menorrhagia. Initial evaluation of UAVMs is made with ultrasonography (US) and US-Doppler. Magnetic resonance is used when a UAMV is suspected at US. Treatment can be surgical (hysterectomy or surgical removal of AVM), or with selective uterine arterial embolization. We report a case of UAMV, from its clinical signs to diagnostic confirmation and subsequent treatment.
Keywords: Uterine arteriovenous malformation, US-Doppler, MRI, Uterine artery, Embolization
Riassunto
Le malformazioni arterovenose dell’utero (MAVU) sono disordini vascolari poco comuni, che spesso si presentano in donne in età fertile; si manifestano come aborti ricorrenti o con menorragia. La valutazione iniziale viene eseguita con l’ecografia e eco colour-Doppler. La risonanza magnetica è utilizzata in caso di sospetto ecografico di MAVU. Il trattamento può essere chirurgico o mediante embolizzazione delle arterie uterine. In questo articolo è riportato un caso di MAVU, dal sospetto clinico alla conferma diagnostica e al trattamento effettivo.
Introduction
Uterine arteriovenous vascular malformations (UAVM) are uncommon vascular disease, which usually occur during reproductive age [1]. They consist of high-flow heterogeneous-sized vessels. Initial diagnosis can be made with US-Doppler, and can be confirmed with angiography. UAVM are treated with uterine artery embolization (UAE). Surgery is reserved for selected cases [2, 3].
The authors report a case of UAMV, from its clinical signs to its diagnostic confirmation and subsequent treatment.
Case report
A multiparous 39-year-old woman with a history of previous gynaecological surgery for three caesarean sections came to our attention for the evaluation of a uterine mass. The patient was hospitalized for an abundant metrorrhagia, with haemoglobin (Hb) levels dropping from 11 to 8 g/dl.
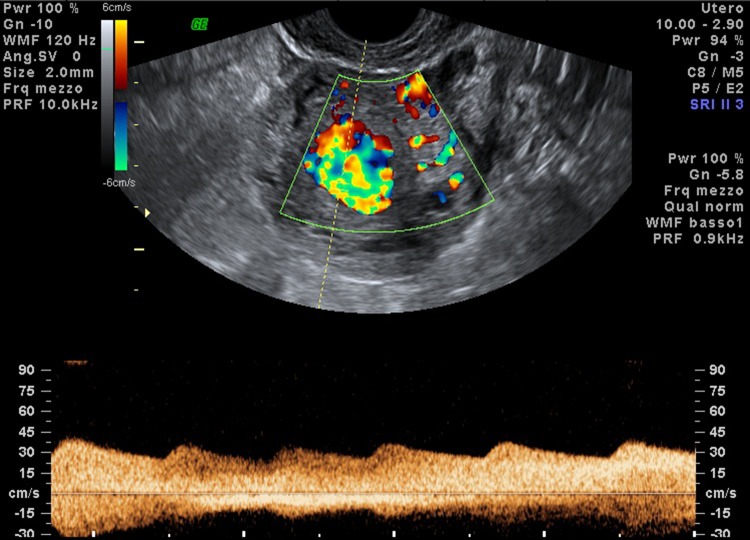
Transvaginal-US was performed showing a uterine mass bulking the anterior-left part of the myometrium with non-pulsatile high flow vessels within the lesion (Fig. 1). The patient was sent to the radiology department for the evaluation of a suspected UAMV and scheduled for a MR. MR showed a focal myometrial thickening with peripheral spots of signal voids which after contrast media administration proved to be dilated high flow vessels. MR-angiography was performed subsequently showing that the UAMV was supplied by both the uterine arteries (UA), mainly from the left UA, with some vessels proceeding from the contralateral UA (Fig. 2).
Fig. 1.
US-Doppler shows high flow vessels within the uterine lesions
Fig. 2.
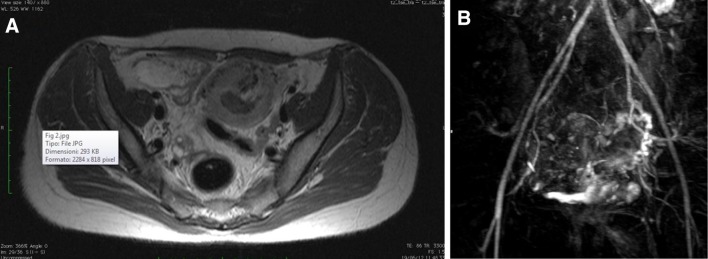
MR shows a uterine lesion within myometrium. a In axial scans it appears as a focal thickening of anterior uterine wall. b MR-angiography shows that the UAMV is supplied by uterine arteries and drains directly into parauterine veins
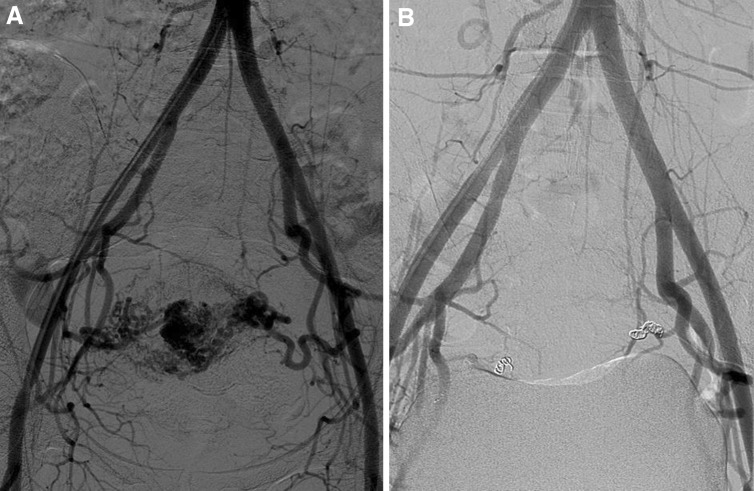
Patient then gave informed consent to undergo UAE, which was carried out with Gelfoam 1,200 nm particles and releasing of metallic coils after embolization. An internal iliac angiogram after the procedure helped confirm obliteration of the mass (Fig. 3).
Fig. 3.
Conventional angiography before (a) and after (b) uterine artery embolization
Discussion
Uterine arteriovenous malformations (UAVM) are an uncommon vascular disease and represent 2 % of all genital and intraperitoneal haemorrhages [1]. Dubreil and Loubat first described them in 1926 as cirsoid aneurisms, and since then they had been referred as arteriovenous aneurysm or arteriovenous malformations [3, 4].
UAMV can be congenital or acquired. Congenital lesions are rare. Acquired lesions are related to previous surgery on the uterus and rare causes as endometrial adenocarcinoma, maternal diethylstilbestrol exposure, miscarriage, uterine infections, myomas, endometriosis, intrauterine devices and trophoblastic disease.
An AVM consists of a proliferation of heterogeneous-sized vascular channels with an arteriovenous fistula formation [1].
Congenital UAVMs tend to have multiple vascular connections and to invade the surrounding structures, while acquired UAVMs are confined within the myometrium and/or the endometrium showing direct communication between the intramural branches of the uterine artery and the myometrial veins [2].
UAMV usually occurs during reproductive age. Common clinical signs are bleeding (metrorrhagia), which is typically intermittent and abundant, pelvic pain and signs of anaemia [5]. Congestive heart failure, due to a large arteriovenous shunting, and the incidental finding of a pelvic mass occurs rarely [1]. Clinical Examination can be unremarkable or showing a palpable mass at vaginal examination [6].
Initial evaluation of UAVMs is made with ultrasonography (US), at which they appear either as masses with multiple hypo/anechoic tubular like structures of varying sizes or as focal endometrial and myometrial thickenings. US-Doppler adds the possibility of recognizing vessels within malformations. Spectral analysis permits evaluating the flow within vessels, recognizing high flow and low resistive index within arteries and veins [2, 3].
In case of suspected UAVM at US, Serum b-hCG is recommended to exclude a gestational trophoblastic disease (GTD), since US findings in UAMV may mimic those of GTD [1].
Magnetic resonance (MR) is used when a UAMV is suspected at US. The best soft tissue characterization, its multiplanar imaging capabilities and the use of gadolinium based contrast media, permits characterization of uterine vascular anomalies. Typical MR findings are a bulky uterus with absence of a defined mass and the presence of serpiginous and dilated vessels within myometrium or parametrium. MR-angiography demonstrates a nidus of high-flow vessels in the uterus fed by uterine arteries and draining into parauterine veins [1, 7].
Conventional angiography remains the gold standard imaging technique, although MRA has proven to be comparable to conventional angiography in evaluation of AMV in other districts, due to the presence of a 3D data set, allowing maximum intensity projections (MIP) and multiplanar reconstructions and a precise depiction of AMV feeding and draining vessels [1, 8].
Arteriography shows dilated irregular vascular spaces supplied by enlarged uterine arteries, with high flow vascular dynamics [2].
Treatment can be surgical (Hysterectomy or surgical removal of AVM), or with selective uterine arterial embolization (UAE) [2, 5, 9]. Preferred treatment is selective UAE [9]. Surgery should be reserved for those cases in which UAE is not feasible or is contraindicated. Medical treatment with combined oral contraceptive pill has been reported in literature [7].
In the case reported above, the natural history of the lesion, its clinical and imaging characteristics, and the effectiveness of treatment are all features of UAVM. In fact, our patient showed a previous history of Caesarean sections, consistent with acquired type UAMV. Imaging aspects were compatible with UAVM and treatment with UAE proved to be effective.
Conflict of interest
The authors have no conflict of interest to disclose.
References
- 1.Cura M, Martinez N, Cura A, Dalsaso TJ, Elmerhi F. Arteriovenous malformations of the uterus. Acta Radiol. 2009;50(7):823–829. doi: 10.1080/02841850903008792. [DOI] [PubMed] [Google Scholar]
- 2.Nicholson AA, Turnbull LW, Coady AM, Guthrie K. Diagnosis and management of uterine arterio-venous malformations. Clin Radiol. 1999;54:265–269. doi: 10.1016/S0009-9260(99)91165-0. [DOI] [PubMed] [Google Scholar]
- 3.Polat P, Suma S, Kantarcý M, Alper F, Levent A. Color Doppler US in the evaluation of uterine vascular abnormalities. Radiographics. 2002;22(1):47–53. doi: 10.1148/radiographics.22.1.g02ja0947. [DOI] [PubMed] [Google Scholar]
- 4.Dubreuil G, Loubat E. Aneurysme cirsoide de l’uterus. Ann Anat Pathol. 1926;3:697–718. [Google Scholar]
- 5.Brown JV, 3rd, Asrat T, Epstein HD, Oglevie S, Goldstein BH. Contemporary diagnosis and management of a uterine arteriovenous malformation. Obstet Gynecol. 2008;112(2 Pt 2):467–470. doi: 10.1097/AOG.0b013e3181719f7d. [DOI] [PubMed] [Google Scholar]
- 6.Sanguin S, Lanta-Delmas S, Le Blanche A, Grardel-Chambenoit E, Merviel P, Gondry J, et al. Uterine arteriovenous malformations: diagnosis and treatment in. Gynecol Obstet Fertil. 2011;39(12):722–727. doi: 10.1016/j.gyobfe.2011.08.013. [DOI] [PubMed] [Google Scholar]
- 7.Grivell RM, Reid KM, Mellor A. Uterine arteriovenous malformations: a review of the current literature. Obstet Gynecol Surv. 2005;60:761–767. doi: 10.1097/01.ogx.0000183684.67656.ba. [DOI] [PubMed] [Google Scholar]
- 8.Díaz Candamio MJ, Lee VS, Rofsky NM, Krinsky GA, Weinreb JC (2000) Pelvic arteriovenous malformation: gadolinium-enhanced three-dimensional MR angiography findings. Eur Radiol 10:1257–1260 [DOI] [PubMed]
- 9.Vogelzang RL, Nemcek AA, Jr, Skrtic Z, Gorrell J, Lurain JR. Uterine arteriovenous malformations: primary treatment with therapeutic embolization. J Vasc Interv Radiol. 1991;2:517–522. doi: 10.1016/S1051-0443(91)72234-3. [DOI] [PubMed] [Google Scholar]