Abstract
PURPOSE
This study evaluated the effectiveness of various methods for removing provisional cement from implant abutments, and what effect these methods have on the retention of prosthesis during the definitive cementation.
MATERIALS AND METHODS
Forty implant fixture analogues and abutments were embedded in resin blocks. Forty cast crowns were fabricated and divided into 4 groups each containing 10 implants. Group A was cemented directly with the definitive cement (Cem-Implant). The remainder were cemented with provisional cement (Temp-Bond NE), and classified according to the method for cleaning the abutments. Group B used a plastic curette and wet gauze, Group C used a rubber cup and pumice, and Group D used an airborne particle abrasion technique. The abutments were observed using a stereomicroscope after removing the provisional cement. The tensile bond strength was measured after the definitive cementation. Statistical analysis was performed using one-way analysis of variance test (α=.05).
RESULTS
Group B clearly showed provisional cement remaining, whereas the other groups showed almost no cement. Groups A and B showed a relatively smooth surface. More roughness was observed in Group C, and apparent roughness was noted in Group D. The tensile bond strength tests revealed Group D to have significantly the highest tensile bond strength followed in order by Groups C, A and B.
CONCLUSION
A plastic curette and wet gauze alone cannot effectively remove the residual provisional cement on the abutment. The definitive retention increased when the abutments were treated with rubber cup/pumice or airborne particle abraded to remove the provisional cement.
Keywords: Retentive strength, Implant cement, Provisional cement, Implant abutment
INTRODUCTION
Dental implants have been used as a successful restoration treatment for tooth replacement over the last few decades. Nevertheless, there is some controversy regarding the clinical procedures or materials. The method for connecting the prosthesis to an implant is one of the most important topics.1-6
Screw-retained prostheses have the advantage of being retrievable, thereby allowing periodic replacement of the prosthodontic components. Furthermore, they are easy to replace if the abutments or screws are fractured, and easy to modify the prostheses after implant loss. However, they are associated with non-passive superstructures. Moreover, loosening and fracture of the screws occur frequently.1,7
On the other hand, cement-retained prostheses allow a passive fit, and have the advantage of simplicity in fabrication, better esthetics and occlusion. In addition, reduced chair time is needed compared to screw-retained prostheses. Therefore, cement-retained prostheses are more economical and effective.1-3 Such advantages account for the recent increase in clinical use but clinicians often face difficulties due to the inconvenient retrieval.1,4,8,9
When permanent cement is used to cement cement-retained prostheses, the removal, if necessary, can be very difficult because of its excessive retention. Therefore, rather than trying to enhance the retention of all circumstances as in natural teeth, the retention in cement-retained prostheses should be adjusted according to the individual situation. The factors that affect the retention of the cementretained prostheses include the taper or parallelism, surface area and height, surface treatment or roughness of abutments, and the type of cement. They are basically the same as those for natural teeth.4
The taper significantly affects the retention of a cement-retained prosthesis. In a study on the retention of implant prostheses, Schneider10 reported that the retention decreases with increasing taper of the abutment. It was reported that a 6 degree taper is ideal for tooth preparation.11 This is the reason why in implant industry, most manufacturers machine their abutments to a 6 degree taper.
In a study of the CeraOne implant system, Covey et al.12 reported that the relationship between the height and width of the abutment is more important than the tooth surface area of the abutment in determining crown retention. Moreover, the total surface area and width of the abutment did not increase the retention value significantly. Others showed that the level of retention increases with increasing vertical height of the abutments.13
Surface roughness and luting agents are factors that can be controlled by the clinician. Other authors reported that the retention values of cements increased with increasing surface roughness of the restoration or abutment.14-18
With regard to selecting cement, Akça et al.13 encouraged the use of permanent cement because provisional cement showed long-term instability. On the other hand, Ramp et al.19 recommended the use of provisional cement for the benefit of retrievability in implant prostheses. However, the use of low-retention cement at the initial phase with a gradual change to higher-retention cement until adequate retention is achieved has been suggested.1
Unfortunately, selecting the correct cement in a clinic is not very simple. When permanent cement is used, its removal when necessary can be quite difficult due to excessive retention. However, the use of provisional cement instead of permanent cement just for retrievability can result in dissolution of cement due to its physical and mechanical instability. This can create a gap between the abutment margin and restoration causing inflammation by plaque accumulation. In addition, the implants may exhibit excessive loading because the functional load is concentrated on the remaining cemented region of the abutment.8
Therefore, the use of provisional cement is recommended only for a short time and a cement with adequate retention is needed for definitive cementation. For this reason, despite the few clinical studies, implant cement is now commercially available because of its convenient removal.
On the other hand, some studies have suggested that residual provisional cement can have a deleterious effect during the definitive cementation in natural teeth if provisional cement is used before the definitive cement. Residual provisional cement inside the prostheses can act as a contamination source and decrease the retention of the definitive cementation.20,21 It can also prevent microroughness on the internal surface of the restoration and make it smooth, thereby decreasing the retention of the definitive cement.22 In addition, a provisional cement containing eugenol disturbs the bonding of the resin cement because eugenol reduces the free radicals and restrains polymerization of the resin.23,24 Kanakuri et al.25 asserted that one cause of the problems associated with ill-fitting restorations would be remaining provisional cement on the abutment surface. Therefore, the complete removal of provisional cement before the definitive cementation of the restorations is recommended.
However, provisional cement is quite difficult to remove completely. Consequently, when implant cement is planned for better retention during the definitive setting, previous provisional cementation and inadequate removal of the provisional cement can affect the retention of the prosthesis.
This study evaluated the effectiveness of a range of methods for removing provisional cement from implant abutments, and the influence these methods on the retention of the prosthesis during definitive cementation. The null hypothesis of this study was that there are no significant differences in retention when using different various methods of removing provisional cement from implant abutment.
MATERIALS AND METHODS
Forty prefabricated implant abutments (GS Rigid Abutment, Osstem Implant Co., Seoul, Korea) with a diameter of 5.0 mm, a length of 5.5 mm and a taper of 6° were used (Fig. 1A). Autopolymerizing acrylic resin (Ortho-Jet, Lang Dental Mfg Co., Wheeling, IL, USA) blocks, approximately 6 mm × 10 mm × 20 mm in size, were fabricated, allowing the implant fixture analogues (Osstem Implant Co., Seoul, Korea) (Fig. 1B) to be placed perpendicular to the 6 mm × 10 mm face of the resin blocks (Fig. 2). The perpendicular placement of the implant fixture analogues into the resin blocks was confirmed using a dental surveyor (Ney surveyor, Ney Dental Intl., Bloomfield, CT, USA). The abutments were connected to the implant fixture analogues to a torque of 30 Ncm.
Fig. 1.
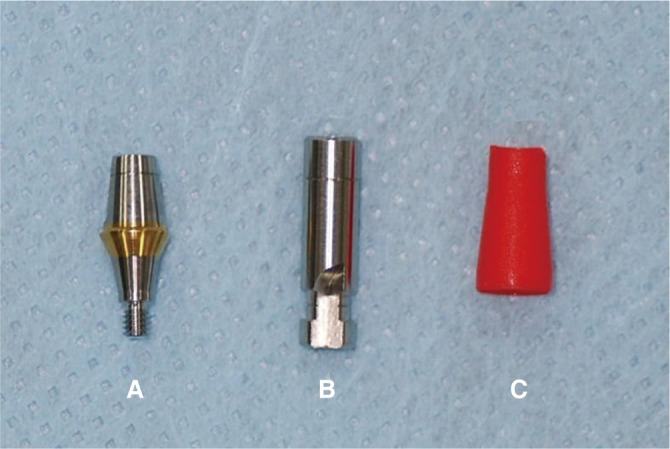
Prefabricated implant abutment (A), implant fixture analogue (B), and prefabricated plastic coping (C) used in this study.
Fig. 2.

Abutment and fixture analogue embedded in acrylic resin.
A prefabricated plastic coping (Fig. 1C) was placed on each abutment. Each plastic burnout coping was attached to a randomly selected implant abutment and complete seating was confirmed by an audible click sound as a "snapon mechanism". A loop of wax was added to the occlusal surface of the coping to allow subsequent retention testing (Fig. 3). All plastic copings were sprued, invested with a phosphate bonded investment (Univest Non-precious, Shofu Dental Co., Kyoto, Japan) and cast with a noble alloy (V-Supragold, Metalor Technologies SA, Neuchâtel, Switzerland) by a single dental technician. Castings were devested, desprued and airborne particle abraded with 50 µm aluminum oxide particles to remove the residual investment materials. The fitting surface nodules were removed using rotary instruments under a microscope with ×10 magnification. A silicone disclosing medium (Fit Checker, GC Corp., Tokyo, Japan) was used to achieve the best possible fit.
Fig. 3.

Crown coping with a loop for retention testing.
All abutment screw access holes were filled with gutta-percha before cementation. Ten specimens were used in the control group (Group A), and cemented finally without provisional cementation.
Temp-Bond NE (Kerr Corp., Orange, CA, USA) was used for the provisional cementation of the remaining 30 specimens. Provisional cement was used to completely cover all the internal walls of the castings, which were then seated onto the abutments by firm finger pressure for 10 seconds, followed by a 5 kg axial compressive load for 10 minutes. Excess cement was removed using a plastic curette. Mixing and cementing procedures were carried out at room temperature by one investigator. After cementation, the specimens were subjected to 500 thermocycling cycles between 5℃ and 55℃ with a 20 second dwell time in each water bath, and 10 second interlude between water baths.
The castings were then separated with the abutments using a universal testing machine (Instron 8871, Instron Co., Norwood, MA, USA). To remove the residual cement, the inner surfaces of all copings were cleaned with an excavator, air abraded with 50 µm aluminum oxide particles for 10 seconds, cleaned with steam for 10 seconds, and cleaned ultrasonically with distilled water for 30 minutes.
Thirty specimens were divided into three groups according to the method used to clean the abutments, as listed in Table 1. In Group B, the abutments were cleaned with a plastic curette (Premier Implant scaler, Premier Dental Products Co., Plymouth Meeting, PA, USA) for 30 seconds, wiped with wet gauze. In Group C, the abutments were cleaned with a rubber cup and pumice for 30 seconds. Group D was treated with an air-powder system (MicroEtcher IIA, Danville Materials, San Ramon, CA, USA) with 50 µm aluminum oxide for 10 seconds. The air-powder system had a 60 psi pressure at the opening of the syringe tip, which was held at a distance of 10 mm from the abutment surface. Each abutment was rinsed with an air/water spray for 10 seconds, and then air dried. At this point, the abutment surface was observed using a stereomicroscope (SZ-PT, Olympus Corp., Tokyo, Japan).
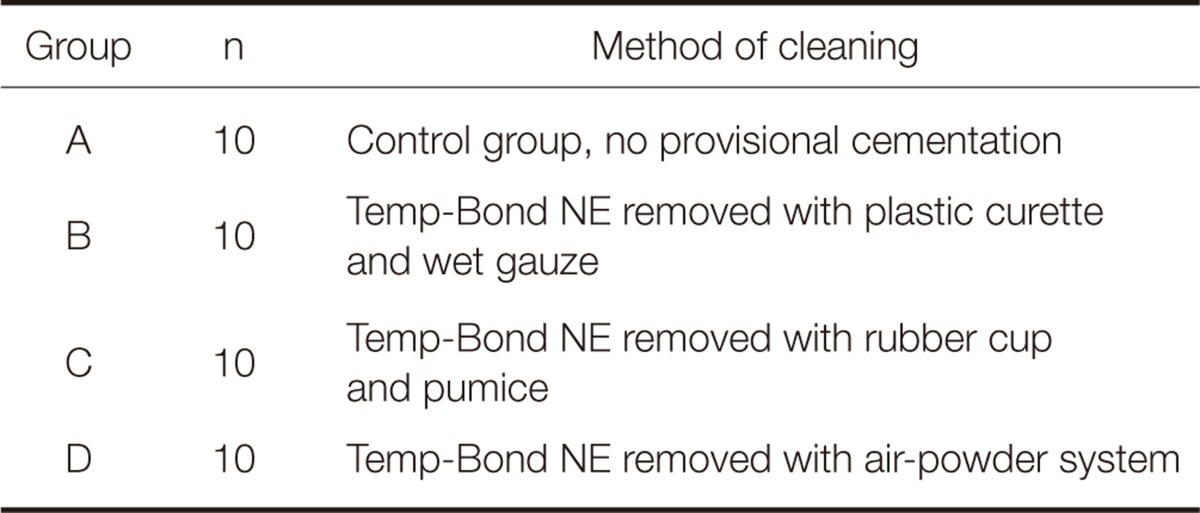
Table 1.
Classification of experimental groups
The old gutta-percha in the abutment screw access holes was removed, and access holes were filled with new gutta-percha. The castings were then cemented onto the abutments with a 5 kg load maintained for 10 minutes using resin cement (Cem-Implant, BJM Laboratories Ltd., Or-Yehuda, Israel). An excess of cement was removed using a plastic curette, followed by thermocycling in the same manner as that after provisional cementation.
The specimens were fixed rigidly to the lower member of the universal testing machine, and stainless steel wire, 10 mm in diameter, was fixed to the upper member (Fig. 4). The machine was set to apply a uniaxial tensile force to the copings with a cross-head speed of 0.5 mm/min, and the force at which cement failure occurred was recorded in Newtons.
Fig. 4.
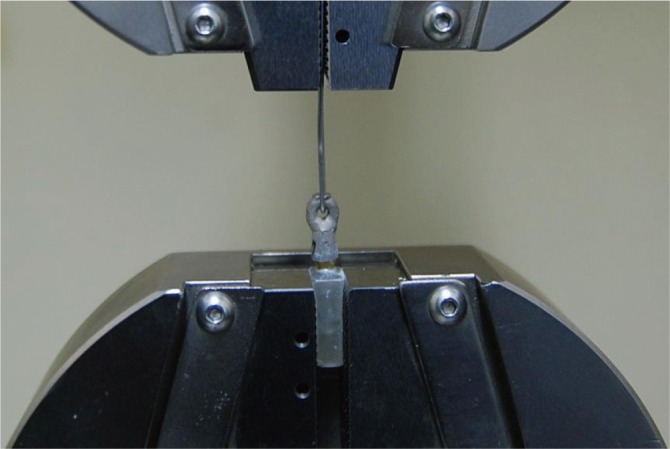
Specimen fixed to the universal testing machine (Instron 8871, Instron Co., Norwood, MA, USA) for tensile testing.
The mean value and standard deviation of each group were calculated. The data were analyzed using one-way analysis of variance (ANOVA). The post hoc tests were carried out using a Duncan's test. 'SPSS for Windows' (Version 12.0, SPSS Inc., Chicago, IL, USA) was used for statistical analysis. It was considered statistically significant for P value <.05.
RESULTS
The abutment surfaces were observed under a stereomicroscope. Group A was the control group with no treatment and representing a smooth surface (Fig. 5). Group B also showed a smooth surface, but a small amount of provisional cement remnant remained (Fig. 6). Group C lost some reflection of light or gloss and showed a slightly roughened surface (Fig. 7), whereas Group D lost almost all the reflection or gloss and showed a significantly roughened surface (Fig. 8). Almost no cement remained in Group C and D.
Fig. 5.
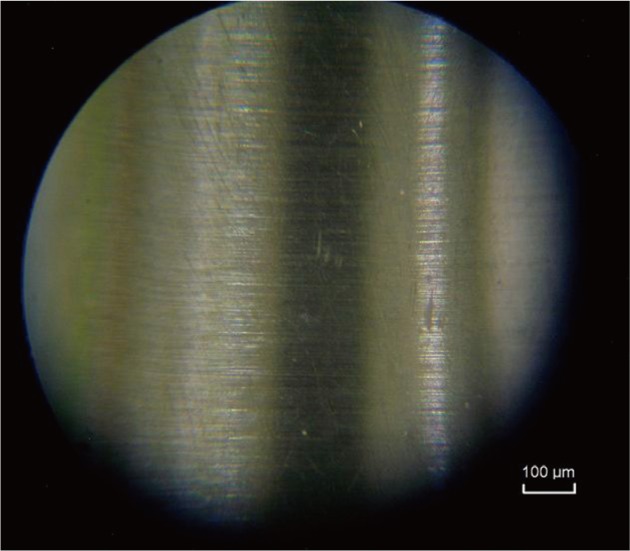
Abutment surface in Group A (original magnification ×330).
Fig. 6.
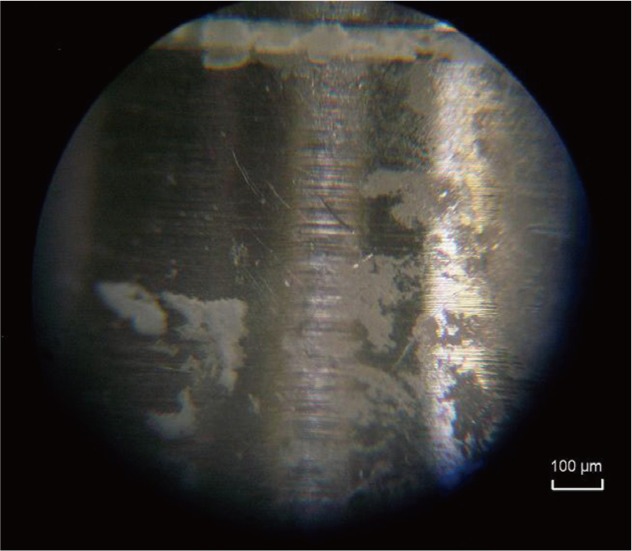
Abutment surface in Group B (original magnification ×330).
Fig. 7.
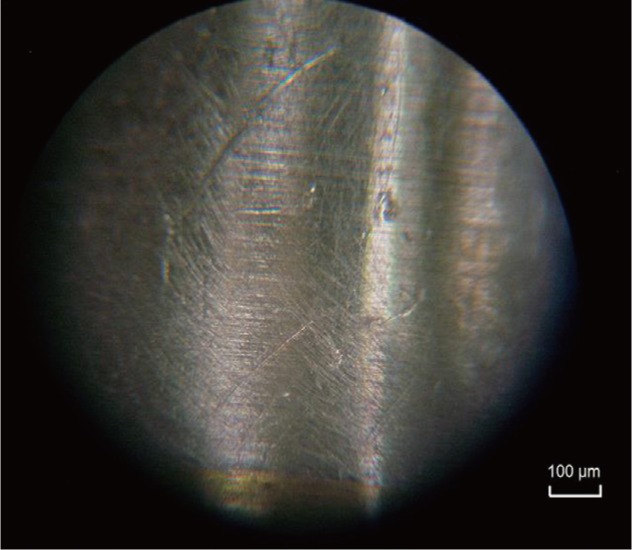
Abutment surface in Group C (original magnification ×330).
Fig. 8.
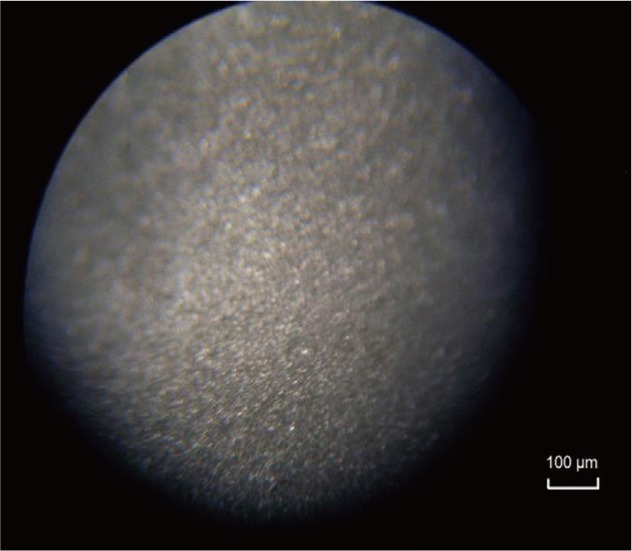
Abutment surface in Group A (original magnification ×330).
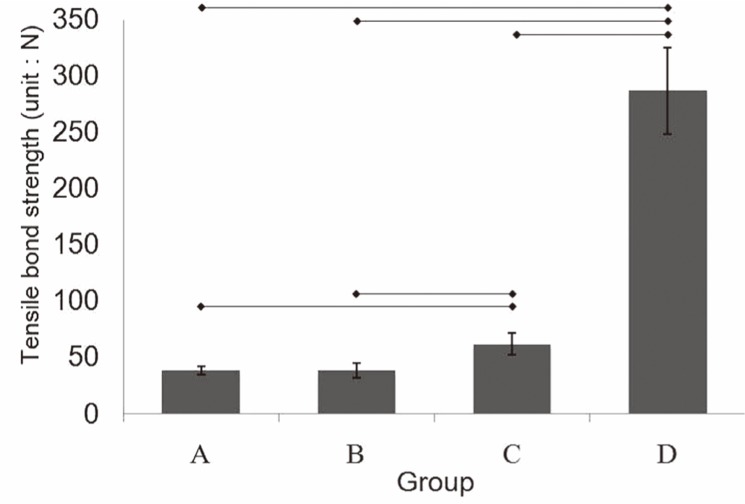
Group D showed the highest tensile bond strength (286.73 N), followed in order by Group C (61.99 N), A (38.65 N) and B (38.45 N) (Fig. 9). The retention value increased as the abutment surfaces became rougher. Significant differences in retention were observed between the 4 groups (P<.05) using the one-way ANOVA test.
Fig. 9.
Average tensile bond strength of each group (unit: N). Horizontal lines indicate significant differences (P<.05).
Tensile bond strength was similar in Group A and B. The tensile bond strength in Group C was higher than that in Group A and B. Group D showed an apparently higher tensile bond strength than the other groups (P<.05).
DISCUSSION
In this study, prefabricated 1-piece implant abutments were used and all factors except for the method for removing the residual cement were standardized. All clinical procedures were reflected in the experiment as much as possible. In addition, implant cement, which has gained more attention recently, was selected as the definitive cement.
The plastic burn-out coping system that has been used in this study offers easy and predictable procedures to laboratory technicians. A space between the abutment and the plastic cap is manufactured, which eliminates the need for a die spacer. This built-in cement space is from 5 µm to 10 µm. The presence of this uniform cement space also decreases the need for casting adjustments.
There is no consensus as to whether an abutment screw access hole should be filled or not, and if filled, with what type of material. Composite resin, wax, polyvinylsiloxane impression material, gutta percha, and cotton pellets have been used to seal the abutment screw access holes. There is potential for chemical bonding between the abutment screw access hole filling material and compatible luting cement that may aid in crown coping retention.26,27 In the present study, the abutment screw access holes were filled with gutta percha, which can be repaired easily. In this manner, there is no possibility of a potential chemical bond between the material used to fill the abutment screw access hole and cement.
While every effort was made to manage all the specimens identically, inadvertent unequal treatment of the specimens should be recognized and may be responsible for some of the observed variations and results. During crown coping construction, variations in individual copings may be introduced at any point of the construction process. On the other hand, the abutments were proposed to be identical due to their high precision computer-aided machining. Thermocycling aims to thermally stress the cements but may not realistically represent the in vivo behavior. If in vitro thermocycling is assumed to be an accurate representation of the in vivo conditions, then its effect on luting cement may be more pronounced than under in vivo conditions due to different crown coping thicknesses. The crown copings in the current study were thin compared to in vivo crowns because no additional wax was added to the plastic burnout coping and porcelain was not layered. Additional material thicknesses may further insulate the cement from thermal stress. Therefore, the cements in this experiment may have been exposed to more severe temperature extremes than that in vivo. Uniaxial tensile testing was used to minimize the lateral forces. When a specimen was tested, there was the potential for incorrect positioning, resulting in a non-uniaxial tensile force. The resulting cement failure force may not be a true indication of the uniaxial force required to remove the copings.
In the control group, the machined abutment surface was not modified with any preparation and was relatively smooth. This can have less cement-abutment micromechanical interlocking, leading to lower cement retention values. The rough, airborne particle abraded internal surface of the coping provided greater micromechanical retention than the smooth machined titanium abutment surface; hence the cement adhered to the coping. Different methods for removing the residual cement from the internal surface of coping are known.28-31 In this study, airborne particle abrasion, steam cleaning and ultrasonic cleaning were used.
A number of techniques have been introduced to clean implant abutments, and some proven to be efficient were used in this study.32-38 Group B showed that a small amount of residual provisional cement remained on the abutment, and there was no change in retention compared to the control group. Group C showed some surface roughness and slightly higher retention than the control group, whereas Group D demonstrated significant roughness and increased retention. This suggests that a surface treatment on a smooth implant abutment surface can create roughness, which in turn increases the retention. However, a small amount of residual provisional cement is unlikely to have a significant effect on retention.
When removing the provisional cement, the appropriate removal method should be determined considering the condition of each abutment. Dario39 suggested that cement-retained prostheses can be retrieved properly by selecting cement with the retention required by the individual restoration. A restoration on multiple long abutments would require a cement of less retention compared to a restoration on a few short abutments. Therefore, an abutment where small retention is expected should be treated with airborne particle abrasion to ensure higher retention. On the other hand, abutments that do not require an increase in retention or require only small increase, can be treated with a plastic curette or rubber cup and pumice. An air-powder system carries the risk of trauma to the periimplant tissue or emphysema if used inappropriately, and caution must be taken when spraying towards the cervical region.35,40
One of the limitations of this study was that only the tensile force was assessed, as in previous studies. In an oral environment, retention failure of fixed partial denture occurs because various mastication forces work in a complex manner for a long time. The same applies to the implants, and mastication forces include direct compressive forces, complex lateral forces and small tensile forces. In most retention experiments, only a direct tensile force is applied. This is quite different from an actual oral environment, which means that it cannot be applied clinically. However, the relative tensile bond strength could be compared because all other factors were controlled in this study. Moreover, an objective comparison can be made because most studies measured the tensile bond strength.
The other limitations of this study were that only one type of adhesive resin cement and provisional cement was used. Different results could have been obtained if a different adhesive resin or different provisional cement had been used. These topics should be investigated in a further study.
CONCLUSION
Within the limitations of the in vitro conditions used in this study, the following conclusions were made. A plastic curette and wet gauze alone could not effectively remove the residual provisional cement on an abutment. And the retention of the prosthesis increased when the abutments were treated with rubber cup/pumice or airborne particle abraded, to remove provisional cement.
Clinically, when the retention of a cement-retained implant prosthesis is insufficient or more retention is needed, retention of the definitive cementation can be regulated by applying different methods to remove the residual provisional cement from the abutment.
References
- 1.Hebel KS, Gajjar RC. Cement-retained versus screw-retained implant restorations: achieving optimal occlusion and esthetics in implant dentistry. J Prosthet Dent. 1997;77:28–35. doi: 10.1016/s0022-3913(97)70203-8. [DOI] [PubMed] [Google Scholar]
- 2.Chee W, Felton DA, Johnson PF, Sullivan DY. Cemented versus screw-retained implant prostheses: which is better? Int J Oral Maxillofac Implants. 1999;14:137–141. [PubMed] [Google Scholar]
- 3.Taylor TD, Agar JR, Vogiatzi T. Implant prosthodontics: current perspective and future directions. Int J Oral Maxillofac Implants. 2000;15:66–75. [PubMed] [Google Scholar]
- 4.Michalakis KX, Hirayama H, Garefis PD. Cement-retained versus screw-retained implant restorations: a critical review. Int J Oral Maxillofac Implants. 2003;18:719–728. [PubMed] [Google Scholar]
- 5.Vigolo P, Givani A, Majzoub Z, Cordioli G. Cemented versus screw-retained implant-supported single-tooth crowns: a 4-year prospective clinical study. Int J Oral Maxillofac Implants. 2004;19:260–265. [PubMed] [Google Scholar]
- 6.Weber HP, Sukotjo C. Does the type of implant prosthesis affect outcomes in the partially edentulous patient? Int J Oral Maxillofac Implants. 2007;22:140–172. [PubMed] [Google Scholar]
- 7.Michalakis KX, Pissiotis AL, Hirayama H. Cement failure loads of 4 provisional luting agents used for the cementation of implant-supported fixed partial dentures. Int J Oral Maxillofac Implants. 2000;15:545–549. [PubMed] [Google Scholar]
- 8.Breeding LC, Dixon DL, Bogacki MT, Tietge JD. Use of luting agents with an implant system: Part I. J Prosthet Dent. 1992;68:737–741. doi: 10.1016/0022-3913(92)90194-f. [DOI] [PubMed] [Google Scholar]
- 9.Mehl C, Harder S, Wolfart M, Kern M, Wolfart S. Retrievability of implant-retained crowns following cementation. Clin Oral Implants Res. 2008;19:1304–1311. doi: 10.1111/j.1600-0501.2008.01587.x. [DOI] [PubMed] [Google Scholar]
- 10.Schneider RL. Evaluation of the retention of castings to endosseous dental implants. J Prosthet Dent. 1987;58:73–78. doi: 10.1016/s0022-3913(87)80147-6. [DOI] [PubMed] [Google Scholar]
- 11.Rosenstiel SF, Land MF, Fujimoto J. Contemporary fixed prosthodontics. 4th ed. St. Louis: Mosby; 2006. p. 229. [Google Scholar]
- 12.Covey DA, Kent DK, St Germain HA, Jr, Koka S. Effects of abutment size and luting cement type on the uniaxial retention force of implant-supported crowns. J Prosthet Dent. 2000;83:344–348. doi: 10.1016/s0022-3913(00)70138-7. [DOI] [PubMed] [Google Scholar]
- 13.Akça K, Iplikçioğlu H, Cehreli MC. Comparison of uniaxial resistance forces of cements used with implant-supported crowns. Int J Oral Maxillofac Implants. 2002;17:536–542. [PubMed] [Google Scholar]
- 14.Juntavee N, Millstein PL. Effect of surface roughness and cement space on crown retention. J Prosthet Dent. 1992;68:482–486. doi: 10.1016/0022-3913(92)90415-7. [DOI] [PubMed] [Google Scholar]
- 15.Tuntiprawon M. Effect of tooth surface roughness on marginal seating and retention of complete metal crowns. J Prosthet Dent. 1999;81:142–147. doi: 10.1016/s0022-3913(99)70241-6. [DOI] [PubMed] [Google Scholar]
- 16.Oilo G, Jørgensen KD. The influence of surface roughness on the retentive ability of two dental luting cements. J Oral Rehabil. 1978;5:377–389. doi: 10.1111/j.1365-2842.1978.tb01257.x. [DOI] [PubMed] [Google Scholar]
- 17.Felton DA, Kanoy BE, White JT. The effect of surface roughness of crown preparations on retention of cemented castings. J Prosthet Dent. 1987;58:292–296. doi: 10.1016/0022-3913(87)90043-6. [DOI] [PubMed] [Google Scholar]
- 18.Ayad MF, Rosenstiel SF, Salama M. Influence of tooth surface roughness and type of cement on retention of complete cast crowns. J Prosthet Dent. 1997;77:116–121. doi: 10.1016/s0022-3913(97)70223-3. [DOI] [PubMed] [Google Scholar]
- 19.Ramp MH, Dixon DL, Ramp LC, Breeding LC, Barber LL. Tensile bond strengths of provisional luting agents used with an implant system. J Prosthet Dent. 1999;81:510–514. doi: 10.1016/s0022-3913(99)70203-9. [DOI] [PubMed] [Google Scholar]
- 20.Grasso CA, Caluori DM, Goldstein GR, Hittelman E. In vivo evaluation of three cleansing techniques for prepared abutment teeth. J Prosthet Dent. 2002;88:437–441. doi: 10.1067/mpr.2002.128123. [DOI] [PubMed] [Google Scholar]
- 21.Erkut S, Küçükesmen HC, Eminkahyagil N, Imirzalioglu P, Karabulut E. Influence of previous provisional cementation on the bond strength between two definitive resin-based luting and dentin bonding agents and human dentin. Oper Dent. 2007;32:84–93. doi: 10.2341/06-27. [DOI] [PubMed] [Google Scholar]
- 22.Peutzfeldt A, Asmussen E. Influence of eugenol-containing temporary cement on efficacy of dentin-bonding systems. Eur J Oral Sci. 1999;107:65–69. doi: 10.1046/j.0909-8836.1999.eos107110.x. [DOI] [PubMed] [Google Scholar]
- 23.Lingard GL, Davies EH, von Fraunhofer JA. The interaction between lining materials and composite resin restorative materials. J Oral Rehabil. 1981;8:121–129. doi: 10.1111/j.1365-2842.1981.tb00485.x. [DOI] [PubMed] [Google Scholar]
- 24.Marshall SJ, Marshall GW, Jr, Harcourt JK. The influence of various cavity bases on the micro-hardness of composites. Aust Dent J. 1982;27:291–295. doi: 10.1111/j.1834-7819.1982.tb05249.x. [DOI] [PubMed] [Google Scholar]
- 25.Kanakuri K, Kawamoto Y, Matsumura H. Influence of temporary cement remnant and surface cleaning method on bond strength to dentin of a composite luting system. J Oral Sci. 2005;47:9–13. doi: 10.2334/josnusd.47.9. [DOI] [PubMed] [Google Scholar]
- 26.Koka S, Ewoldsen NO, Dana CL, Beatty MW. The effect of cementing agent and technique on the retention of a CeraOne gold cylinder: a pilot study. Implant Dent. 1995;4:32–35. doi: 10.1097/00008505-199504000-00005. [DOI] [PubMed] [Google Scholar]
- 27.Dudley JE, Richards LC, Abbott JR. Retention of cast crown copings cemented to implant abutments. Aust Dent J. 2008;53:332–339. doi: 10.1111/j.1834-7819.2008.00075.x. [DOI] [PubMed] [Google Scholar]
- 28.Button GL, Barnes RF, Moon PC. Surface preparation and shear bond strength of the casting-cement interface. J Prosthet Dent. 1985;53:34–38. doi: 10.1016/0022-3913(85)90060-5. [DOI] [PubMed] [Google Scholar]
- 29.Cobb DS, Vargas MA, Fridrich TA, Bouschlicher MR. Metal surface treatment: characterization and effect on compositeto-metal bond strength. Oper Dent. 2000;25:427–433. [PubMed] [Google Scholar]
- 30.Al-Zain SA. The effect of different metal cleaning methods on retention of cast crowns. Egypt Dent J. 2006;52:2087–2092. [Google Scholar]
- 31.Mosharraf R. A simple method for cleaning zinc oxide-eugenol provisional cement residues from the intaglio surface of casting restorations. J Prosthet Dent. 2004;91:200. doi: 10.1016/j.prosdent.2003.12.001. [DOI] [PubMed] [Google Scholar]
- 32.Homiak AW, Cook PA, DeBoer J. Effect of hygiene instrumentation on titanium abutments: a scanning electron microscopy study. J Prosthet Dent. 1992;67:364–369. doi: 10.1016/0022-3913(92)90248-9. [DOI] [PubMed] [Google Scholar]
- 33.Speelman JA, Collaert B, Klinge B. Evaluation of different methods to clean titanium abutments. A scanning electron microscopic study. Clin Oral Implants Res. 1992;3:120–127. doi: 10.1034/j.1600-0501.1992.030304.x. [DOI] [PubMed] [Google Scholar]
- 34.Brookshire FV, Nagy WW, Dhuru VB, Ziebert GJ, Chada S. The qualitative effects of various types of hygiene instrumentation on commercially pure titanium and titanium alloy implant abutments: an in vitro and scanning electron microscope study. J Prosthet Dent. 1997;78:286–294. doi: 10.1016/s0022-3913(97)70028-3. [DOI] [PubMed] [Google Scholar]
- 35.Mengel R, Buns CE, Mengel C, Flores-de-Jacoby L. An in vitro study of the treatment of implant surfaces with different instruments. Int J Oral Maxillofac Implants. 1998;13:91–96. [PubMed] [Google Scholar]
- 36.Bain CA. An in vitro and in vivo evaluation of various implant-cleaning instruments. Quintessence Int. 1998;29:423–427. [PubMed] [Google Scholar]
- 37.Razzoog ME, Koka S. In vitro analysis of the effects of two air-abrasive prophylaxis systems and inlet air pressure on the surface of titanium abutment cylinders. J Prosthodont. 1994;3:103–107. doi: 10.1111/j.1532-849x.1994.tb00136.x. [DOI] [PubMed] [Google Scholar]
- 38.Augthun M, Tinschert J, Huber A. In vitro studies on the effect of cleaning methods on different implant surfaces. J Periodontol. 1998;69:857–864. doi: 10.1902/jop.1998.69.8.857. [DOI] [PubMed] [Google Scholar]
- 39.Dario LJ. Implant angulation and position and screw or cement retention: clinical guidelines. Implant Dent. 1996;5:101–104. [PubMed] [Google Scholar]
- 40.Kreisler M, Kohnen W, Christoffers AB, Götz H, Jansen B, Duschner H, d'Hoedt B. In vitro evaluation of the biocompatibility of contaminated implant surfaces treated with an Er : YAG laser and an air powder system. Clin Oral Implants Res. 2005;16:36–43. doi: 10.1111/j.1600-0501.2004.01056.x. [DOI] [PubMed] [Google Scholar]