Abstract
Background:
Mental illness have been largely ignored or neglected because of a community's perception and attached social stigma.
Materials and Methods:
A community based cross-sectional study was conducted in an urban community in South Delhi to study perception and attitude of the community about towards mental illness. An adult member in household selected by systematic random sampling was interviewed using semi-structured interview schedule for perception about mental illness and 34 item Opinion about Mental Illness for Chinese Community (OMICC) scale
Results:
A total of 100 adults were interviewed. Mean age of the participants was 35.8 (SD: 12.6) years. Living without tension and satisfaction in routine life were identified as indicators of healthy mental status. Change in the behavior was perceived as the most common symptom of mental illness. Although mental stress was identified as the most common cause of mental illness, 25% attributed it to evil spirits. Keeping surroundings friendly and sharing problems with others were identified as - important preventive measures against mental illness. Mental illness was perceived as treatable; 12% preferred treatment from Tantric/Ojha. Community showed negative attitude for stereotyping, restrictiveness, and pessimistic prediction domains of OMICC scale with mean score of 4.5 (SD: 0.2), 3.9 (SD: 0.9), and 3.8 (SD: 0.4), respectively, with no statistically significant difference across age, sex, and literacy.
Conclusion:
Study observed lack of awareness regarding bio-medical concept of mental illness with socially restrictive, stereotyping, pessimistic, and non-stigmatizing attitude toward mental illness in the capital city.
Keywords: Attitude about mental illness, India, opinion about mental illness for chinese community scale, perception, urban community
INTRODUCTION
Mental health is an indicator of the social life of a population. The rising level of morbidity and mortality is a sign of social as well as individual malaise.[1] In most parts of the world, mental health and mental illness are largely ignored or neglected, resulting in increasing burden of mental disorders in the community and a widening of “treatment gap.”[2]
Meta-analysis of epidemiological studies reported prevalence of mental illness as 58.2[3] and 73[4] per 1000 population in India. However, even after three decades of its launch, National Mental Health Programme is restricted only to 123 districts, that too in the rural region.[5] Urban community in the country, which is exposed to stress of migration, change in family and social dynamics, widening inequalities in economic status, widespread poverty, poor living conditions, and insecurity, hardly gets due attention in the program. Lack of organised public health infrastructure and expensive treatment at private settings add to the problem.
Patients with mental illness have been stigmatised since long back in any community, and this stigmatisation is beyond just “labelling” the patients.[6] The condition is perceived as frightening, shameful, imaginary, feigned, and incurable, while the patients are characterised as dangerous, unpredictable, untrustworthy, unstable, lazy, weak, worthless, and/or helpless in the community.[7,8,9]
Furthermore, it is important to study the perception, attitude, and health-seeking behavior in the community regarding mental illness, which will help in providing mental healthcare services for the community.
MATERIALS AND METHODS
This was a community based cross-sectional study conducted from August 2009 to November 2009 in an urban community, South Delhi, in northern India. Six blocks of area were included in Intensive Field Practice Area under Urban Health Programme of Centre for Community Medicine of All India Institute of Medical Sciences, New Delhi. Out of which, one block was randomly selected for the study by lottery method.
In the selected block, list of all households was prepared to provide the sampling frame. Individual household was selected by systematic random sampling. Any adult member (≥18 years) residing in a selected household for more than 6 months and volunteering for interview was recruited in the study to complete a predetermined sample size of 100 participants.
Focus group discussion (FGD) guide was prepared after extensive review of literature and discussion with experts in this field to identify various domains related with mental illness. Focus group discussion was carried out among males and females separately in the two different blocks of the study area other than block selected for the study. On the basis of FGD, semi-structured interview schedule was designed to collect information about mental illness including causative factors, preventive measures, identifying features, treatment seeking places, and related practices in the community. This interview schedule was translated into Hindi language, pretested, and then modified before use. Attitude about mental illness was studied by using Opinion about Mental Illness for Chinese Community (OMICC) scale. English version of OMICC scale was translated into Hindi language. Hindi version was again back translated into English for checking integrity of concepts of various domains. Hindi version was pretested in the community.
OMICC scale
OMICC scale was developed by Ng et al.,[10] on the basis of face validity; building on the scale of Opinion about Mental Illness (OMI) developed by Cohen and Strunning[11] and small scale survey with mental health professionals. Six factors were studied as follows:
Benevolence—Items related to kind orientation towards people with mental illness
Separatism—Items emphasize the distinctiveness of people with mental illness and to keep them away at a safe distance
Stereotyping—Items that fixed people with mental illness in a particular behavioral pattern, mental ability, and mannerism
Restrictiveness—Items that held a doubtful view on the right of people with mental illness
Pessimistic prediction—Items that held the view that people with mental illness are unlikely to improve and that how society treats them, is not optimistic
Stigmatization—Items that perceived mental illness as shameful, that sufferers should be kept from being known to others
Factor analysis of the OMICC scale with 34 questions in “six” domains has been reported to yield a Cronbach's Alpha of 0.866.[10]
Data analysis
For perception about mental illness, frequency distribution of the responses was calculated.
Analysis of OMICC attitude scale was done like any other likert scale with five point responses. All responses under each domain were coded from one to five and reverse coded for benevolence domain. Analysis was performed in the form of mean and standard deviation. Attitude in each domain was determined on the basis of pooled mean values for the respective domain. Values higher than “two” were consider as negative attitude in the respective domain.
Difference in attitude across age, sex, and literacy in six domains was assessed by independent sample t test. P<0.05 was considered statistically significant. Data analysis was done with SPSS version 13 for windows.
Ethical issues
Written informed consent was obtained from the participants. Ethical clearance for the study was obtained from Institute's ethical committee of All India Institute of Medical Sciences, New Delhi.
RESULTS
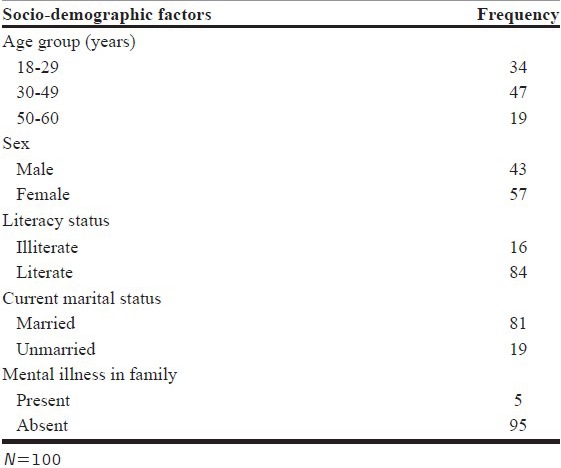
A total of 100 participants were recruited in the study. Mean age of the participants was 35.8 (SD: 12.6) years with almost half (47%) belonging to the 30–49 years age group. Majority of the participants were female (57%), literate (84%), currently married (81%), and did not report mental illness in the family (95%) [Table 1].
Table 1.
Socio-demographic profile of the study participants
Perception about mental illness
Most of the participants (32%) perceived that living without tension, living happily, and satisfied in routine life as indicators of a healthy mental status. Almost one-fourth (24%) of the participants did not know the meaning of being mentally healthy. Sudden change in behavior like remaining quite or over talkativeness (59%) and abusing or fighting with others (53%) were among the most common symptoms/signs of mental illness identified by the participants. Almost one-third of the participants perceived that symptoms of mental illness were overt, which makes a person with mental illness easily identifiable. Only few (3%) of them perceived that it would require expert to diagnose the mental illness.
Tension/mental stress in routine day to day life were perceived as the most common cause of mental illness (79%). Importantly, one-fourth of the participants perceived the role of Uppari chakkar/evil spirits in the development of mental illness.
Almost one-fourth of the participants perceived that mental illness is transmitted from person to person (21%) and from the mother to her child (27%) like any other communicable disease. Most of the participants perceived that mental illness could be curable, but one-fifth of them (20%) perceived that these are not completely curable. Almost one-third (29%) perceived that these disorders can be prevented by keeping friendly home environment and sharing problems, thoughts with others. Stress relieving activities like yoga and meditations were perceived as one of the important preventive measures for development of mental illness. However, 11% felt that mental illness is non-preventable.
Almost half of the participant felt that patient with mental illness can get specialised care at a mental hospital only; 21% of the participants perceived the role of faith healers (Tantrik, Ojha) in the treatment of mental illness.
According to the participants, community (39%) as well they themselves will prefer mental hospital over general physician for seeking care for mental illness. Faith healers (Tantric, Ojha) were identified as health seeking places both for the community as well as for them by (12%). Most of the participant felt that community (80%) ignores mentally ill patients and their families. Almost one-fourth (27%) of the participants felt that people from the community tease and make fun of a person with mental illness instead of getting them treated.
Attitude of community towards mental illness
Analysis of OMICC scale showed higher (mean) scores for stereotyping (4.5), restrictiveness (3.9), and pessimistic prediction (3.8) domains and lower values for separatism (2.6), benevolence (1.8), and stigmatisation (2.3) domains [Figure 1]. Community showed kind, non-stigmatising but pessimistic attitude toward the future of the people with mental illness. At the same time, participants also felt that social relationship with these people should be restricted.
Figure 1.
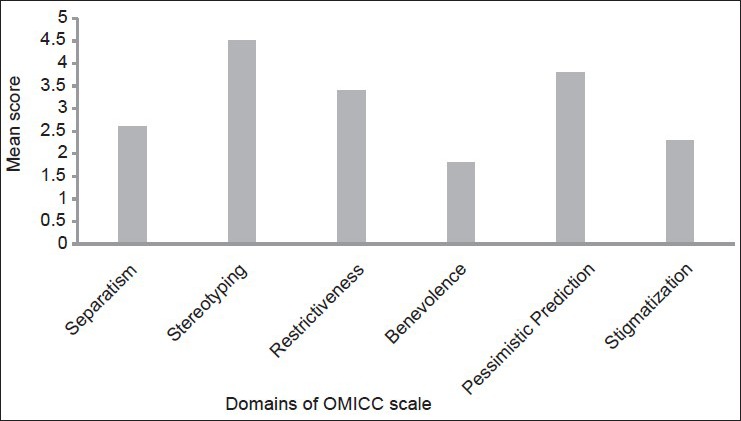
Representation of attitude of the participants toward patients with mental illness by analysing OMICC scale
Difference in attitude towards mental illness across age, sex, and literacy status was found statistically non-significant (P > 0.05).
DISCUSSION
This study describes the perception of the community regarding mental health and derangement of mental health, similar to WHO definition of mental health as a positive sense of well-being and not merely the absence of a illness.[1]
Awareness of the community about symptoms/signs of mental illness is limited to symptoms that manifest in severe mental illness or in later stage of the illness. The reason could be either lack of awareness of participants about other common symptoms like sense of hopelessness, aloofness, and anxiety or may be that these symptoms are too common to be recognised as abnormal. This fact is supported by the observation that only few of the participants agreed that mental illness could be present in a person with normal behavior and it is not possible to diagnose it by mere observation (3%).
Singh et al.,[12] reported stressful conditions as a cause for development of mental illness similar to the observations in the present study. Attribution of mental illness to upari chakkar/evil spirit/black magic was present in a substantial proportion (25%) and shows the lack of awareness of the community about bio-medical concept of causation of these disorders. Similar findings have been reported in various studies.[13,14,15,16] The knowledge of the participant has been reflected in the health-seeking behavior of the community as tantric and ojha were reflected among health-seeking places for mental illness to get rid of evil spirits. Similar findings have been reported by Chadda et al.,[17] This fact is also supported by observation that participants do regard transmission of the mental illness from person to person (21%) and from mother to child (27%).
This lack of knowledge in the study population from the capital city that has a well-known institute for care for mentally ill is serious because the ignorance could possibly be more in other regions of the country.
Community showed positive perception regarding treatment outcome of mental illness. Mental hospital has been identified as a preferred place by the participants for treatment. This indicates preference for specialised care for patients with mental illness. Similar findings have been reported in previous studies.[12,18]
Community identified stress relieving activities like Yoga and Satsang, supportive family environment, and sharing thoughts with others as preventive measures against mental illness. These findings are in coherence with the knowledge of the community about causality of mental illness. Similar findings were reported in study by Singh et al.[12]
Community attitude toward patient with mental illness was kind and non-stigmatising, which was similar to the attitude of the community reported in various studies.[12,13] Although participants did not support isolating person with mental illness from the society, restrictive attitude was observed with regards to marriage or child bearing. Socially desirable responses hiding the true stigmatizing attitude of the community is possible.
This finding corroborates with findings of the study by Singh et al.,[12] and Kermode et al.,[14] Also, participants are pessimistic when it comes to career or job opportunity for a person with mental illness.
This socially restrictive attitude is reflected in the practices of community toward psychiatric ill patients in the form of restricting visits to patient's home and ignoring the patients.
In the era of economic and social development, community still approaches Tantric/Ojha in the capital city. Community reported restrictive, stereotyping, pessimistic, and non-stigmatizing attitude toward patient with mental illness that can be the barrier in health-seeking behavior for mental illnesses.[18]
CONCLUSION
This study reported lack of awareness about bio-medical concepts of mental illness in a community in the capital city.
There is a need for creating awareness regarding biomedical concepts, availability of effective treatment for mental illness, for identification and better care for these disorders in a community as a part of National Mental Health Programme.
Health education and increase in public awareness regarding factual information about mental illness can decrease the stigma attached with mental illness and improve help-seeking behavior of the community.[19,20] This will also help in reducing burden of psychiatric morbidity in the community.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.World Health Organization. The World Health Report 2001-Mental Health: New Understanding, New Hope. 2001 [Google Scholar]
- 2.Kumar A. District mental health programme in India: A case study. J Health Dev. 2005;1:24–35. [Google Scholar]
- 3.Math SB, Chandrashekar CR, Bhugra D. Psychiatric epidemiology in India. Indian J Med Res. 2007;126:183–92. [PubMed] [Google Scholar]
- 4.Reddy MV, Chandrasekar CR. Prevalence of mental and behavioural disorders in India: A meta-analysis. Indian J Psychiatry. 1998;40:149–57. [PMC free article] [PubMed] [Google Scholar]
- 5.Annual Report (2009-10). Ministry of Health and Family Welfare. Government of India. 2010 [Google Scholar]
- 6.Lawrie SM. Stigmatisation of psychiatric disorder. Psychiatric Bull. 1999;23:129–31. [Google Scholar]
- 7.Raguram R, Weiss MG, Channabasavanna SM, Devins GM. Stigma, depression, and somatization in South India. Am J Psychiatry. 1996;153:1043–9. doi: 10.1176/ajp.153.8.1043. [DOI] [PubMed] [Google Scholar]
- 8.Charles H, Manoranjitham SD, Jacob KS. Stigma and explanatory models among people with schizophrenia and their relatives in Vellore, south India. Int J Soc Psychiatry. 2007;53:325–32. doi: 10.1177/0020764006074538. [DOI] [PubMed] [Google Scholar]
- 9.Crisp AH, Gelder MG, Rix S, Meltzer HI, Rowlands OJ. Stigmatisation of people with mental illness. Br J Psychiatry. 2000;177:4–7. doi: 10.1192/bjp.177.1.4. [DOI] [PubMed] [Google Scholar]
- 10.Ng P, Chan KF. Sex differences in opinion towards mental illness of secondary school students in Hong Kong. Int J Soc Psychiatry. 2000;46:79–88. doi: 10.1177/002076400004600201. [DOI] [PubMed] [Google Scholar]
- 11.Cohen J, Struening EL. Opinions about mental illness in the personnel of two large mental hospitals. J Abnorm Soc Psychol. 1962;64:349–60. doi: 10.1037/h0045526. [DOI] [PubMed] [Google Scholar]
- 12.Singh AJ, Shukla GD, Verma BL, Kumar A, Srivastava RN. Attitude of Indian urban adults towards mental illnesses. Indian J Public Health. 1992;36:51–4. [PubMed] [Google Scholar]
- 13.Chong SA, Verma S, Vaingankar JA, Chan YH, Wong LY, Heng BH. Perception of the public towards the mentally ill in a developed Asian country. Soc Psychiatry Psychiatr Epidemiol. 2007;42:734–9. doi: 10.1007/s00127-007-0213-0. [DOI] [PubMed] [Google Scholar]
- 14.Kermode M, Bowen K, Arole S, Pathare S, Jorm AF. Attitudes to people with mental disorders: A mental health literacy survey in a rural area of Maharashtra, India. Soc Psychiatry Psychiatr Epidemiol. 2009;44:1087–96. doi: 10.1007/s00127-009-0031-7. [DOI] [PubMed] [Google Scholar]
- 15.Verghese A, Beig A. Public attitude towards mental illness- The Vellore study. Indian J Psychiatry. 1984;16:8–18. [Google Scholar]
- 16.Boral GC, Bagchi R, Nandi DN. An opinion survey about the causes and treatment of mental illness and social acceptance of the mentally ill patients. Indian J Psychiatry. 1980;22:235–8. [PMC free article] [PubMed] [Google Scholar]
- 17.Chadda RK, Agarwal V, Singh MC, Raheja D. Help seeking behaviour of psychiatric patients before seeking care at a mental hospital. Int J Soc Psychiatry. 2001;47:71–8. doi: 10.1177/002076400104700406. [DOI] [PubMed] [Google Scholar]
- 18.Hugo CJ, Boshoff DE, Traut A, Zungu-Dirwayi N, Stein DJ. Community attitudes toward and knowledge of mental illness in South Africa. Soc Psychiatry Psychiatr Epidemiol. 2003;38:715–9. doi: 10.1007/s00127-003-0695-3. [DOI] [PubMed] [Google Scholar]
- 19.Pothen M, Kuruvilla A, Philip K, Joseph A, Jacob KS. Common mental disorders among primary care attendees in Vellore, South India: Nature, prevalence and risk factors. Int J Soc Psychiatry. 2003;49:119–25. doi: 10.1177/0020764003049002005. [DOI] [PubMed] [Google Scholar]
- 20.Rose D, Thornicroft G, Pinfold V, Kassam A. 250 labels used to stigmatise people with mental illness. BMC Health Serv Res. 2007;7:97. doi: 10.1186/1472-6963-7-97. [DOI] [PMC free article] [PubMed] [Google Scholar]


