Abstract
Contact lenses are required for the visual improvement in patients with keratoconus. Various contact lens options, such as rigid gas permeable (RGP) lenses, soft and soft toric lenses, piggy back contact lenses (PBCL), hybrid lenses and scleral lenses are availble. This article discusses about selection of a lens depending on the type of keratoconus and the fitting philosophies of various contact lenses including the starting trial lens. A Medline search was carried out for articles in the English language with the keywords keratoconus and various contact lenses such as Rose k lens, RGP lens, hybrid lens, scleral lens and PBCL.
Keywords: Contact lens, keratoconus, piggy back contact lenses, rigid gas permeable, scleral lens, SynergEyes, toric soft contact lens
Keratoconus is a non-inflammatory ectatic thinning disorder of the cornea that results in poor vision because of irregular astigmatism.[1] Spectacles are useful in the early stages of keratoconus when the astigmatism is mild. With advanced keratoconus, spectacles play a very limited role and contact lenses become necessary for improving the vision and play a major role. Various options for contact lenses are available and one can use any one of these as a starting lens, depending on the severity of the cone and associated conditions.[2,3,4,5] To fit contact lenses is a challenge in patients with keratoconus; this article attempts to simplify the selection of a right contact lens to obtain an acceptable fit with improved vision.
Methods of literature search: A Medline search was carried out for articles in the English language, with the keywords keratoconus and various contact lenses such as Rose k lens, rigid gas permeable (RGP) lens, hybrid lens, scleral lens, piggy back contact lenses (PBCL) and the relevant references are mentioned here.
Pre-requisite for the Fitting
Keratometry and corneal topography are important tools in the management of keratoconus and a guide in selecting the parameter for the initial trial lens indices.[6,7] A trial lens (diagnostic) approach is necessary to achieve an acceptable contact lens fit in keratoconus patients.[8] But as the severity of keratoconus increases, the corneal apex become steeper and fitting the contact lens becomes more challenging. Ultimately, the fitting of contact lens in keratoconus patients becomes complex, necessitating longer chair time and multiple diagnostic fitting trials. The parameters obtained on corneal topography help in reducing the chair time and in getting an acceptable fitting with RGP or Rose k lenses in keratoconus patients.[2]
Buxton et al., have classified keratoconus based on the keratometry values at the apex of the cone: Mild if less than 45.00 D, moderate if >45.00 D and <52.00 D, advanced if > 52.00 D and < 62 D, and severe if > 62.00 D. Their classification extends to categorizing as round or oval cones based on the morphological shape of the cone.[9] Most keratometers are in the range of 36 to 52 D and the range of keratometry measurement can be increased with a spherical lens of +1.25 in front of the central aperture of keratometer mire to 61 D. This helps in measuring the curvature in cases of advanced disease.
Corneal topography helps in assessing the severity and in knowing the morphology of the cone i.e., nipple cone (small, paracentral, steeper, located inferiorly or inferonasally), oval cone (inferiorly or inferotemporally steeper cornea) and globus cone (overall steeper cornea). The globus cone is much larger and involves more than three fourth of the cornea up to the limbus.[10]
Which Lens to Choose?
The main goal of fitting contact lenses is to improve visual acuity with comfort without compromising the health of the cornea. Barr et al., had shown that corneal scarring can be reduced by modifying the contact lens fit.[11]
A lens is selected based on the manifest refraction if possible and the degree of the keratoconus. For mild keratoconus, a soft or soft toric contact lens can be selected but as the degree of keratoconus advances, RGP is the lens of choice. Soft contact lenses (SCL) are known for comfort.[12] Once the patient starts using SCL, then with the progression of the disease, it becomes difficult for the patient to tolerate RGP. So preferably RGP trial should be conducted as a first lens whenever possible.
The three important parameters in the fitting of any contact lens are diameter of the contact lens, the base curve and the power. A low minus power lens is to be used for mild keratoconus and a high minus trial lenses should be used in advanced to severe cone even when refraction is not possible and with steeper base curves.
The diameter is based on the location of the cone, its size, and steepness. In general, it is good to start with a lens of small diameter such as 8.7 mm. Nipple cone has a small diameter, making the fitting of contact lens easy. The oval or sagging cone is located inferotemporally and needs larger diameter lenses and it is difficult to fit these patients.
Soft Spherical/Soft Toric Lenses
Soft spherical or toric contact lenses have a very limited role and are indicated in early keratoconus. These lenses can be prescribed with glasses over contact lens. Sometimes high myopia is associated with keratoconus and SCL are useful in these patients. The other indications for SCL include intolerance to RGP lenses and discomfort with RGP lenses.
While selecting SCL, thicker lenses with low water content should be used to neutralize the irregular astigmatism. For severe apical displacement or a globus cone, or a cone with a large diameter, lenses with a large diameter should be selected.[13]
The various soft toric lenses, which are available, include HydroKone (Medlens Innovations), Soft K (Advanced Vision Technologies), Solus Soft K (Strategic Lens Innovations), SpecialEyes 59/54 Toric (SpecialEyes), and Ocu-Flex Toric (Ocu-Ease). These lenses are available with steeper base curves.[13,14]
Kerasoft lenses (UltraVision, UK) are available as either conventional hydrogel or silicone hydrogel lenses. These are similar to soft toric lenses with a single laser marking at the 6 O′clock position [Fig. 1] to assess the rotation. The rotation should be minimal. As the lens stabilizes on the ocular surface, the lens steepens after a while and one needs to re-assess these patients after a longer duration of wear. The fitting of these lenses can be immediately assessed after 5 minutes of lens application as per company guidelines. However, these lenses may tighten on the eye and fits should be reassessed after 30 minutes before placing final order. The fitting assessment of the lens includes the lens fitting on the eye along with the assessment of visual acuity with the lens. Poor visual acuity indicates a poor lens fit. A movement of 1-2 mm is acceptable and sometimes even a movement of 3 mm is acceptable if the visual acuity is good and the patient is comfortable.
Figure 1.
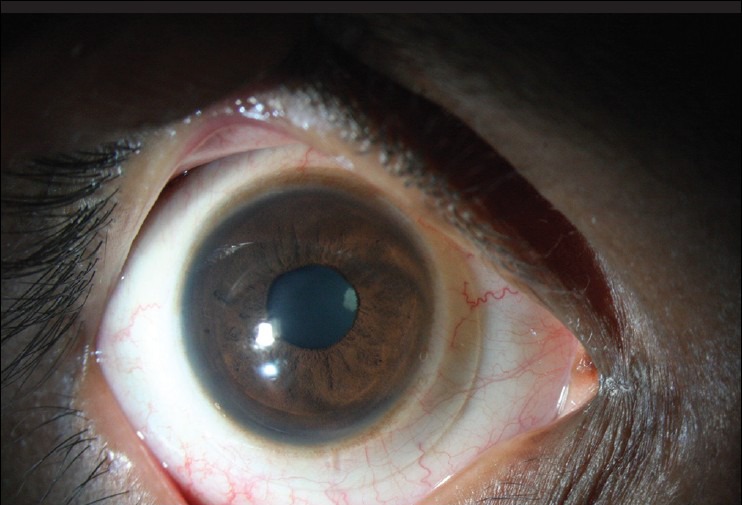
Kerasoft – A single laser mark towards the right of 6 O’ clock position
These are indicated for RGP intolerance, prior to wearing PBCL. In a retrospective study comparing the Rose K2 and Kerasoft IC contact lenses, the best corrected visual acuity was similar in both groups in cases of mild and moderate keratoconus but the corneal staining was more with Rose K as compared to Kerasoft lenses.[15] Our experience too is similar, with mild and moderate keratoconus. It is often difficult to fit Kerasoft lenses in advanced or severe keratoconus.
Rigid gas permeable lenses
Corneal RGP lens is the first lens of choice for visual improvement. Diameter, base curve and power of the contact lens are important criteria in selecting the first lens, as stated earlier. In keratoconus, the cone is steeper and the cornea beyond the cone is flatter. RGP lenses usually rest on the apex of the cone; so to fit RGP lenses in keratoconus, lenses that have a tri-curve or more peripheral curves are used, hence special trial lenses are required. In early or mild keratoconus, traditional RGP lenses can be used and it is possible to obtain an ideal fit but as the cone advances, it becomes difficult to get an optimal or ideal fit and one may have to accept a compromised fit, provided it does not cause any damage to the ocular surface.
There are various materials and designs available for fitting these lenses such as traditional or customized lenses that are made locally (e.g., Material - Flouroperm 90, CLASSIC company, Bangalore, India), or Rose k lenses (Menicon Z material from Menicon Co., Ltd, Nagoya, Japan). Materials with high oxygen transmissibility should be selected to prevent hypoxia related corneal changes.
After allowing for an adaptation period of 30 min for the lens on the eye after insertion, both the dynamic and static fit should be assessed. As the name suggests, in dynamic fit, the lens fit is considered to be acceptable when the lens is centered on the cornea adequately during post-blink movements, good stability in different gazes and the patient is comfortable during all these movements. The movement should be not more than 1mm with every blink and the lens should not cross the limbus.
The static fit is assessed after instilling fluorescein in the eye with cobalt blue filter with or without the Wratten filter. (One can use the yellow gelatine paper if Wratten filter is not available for fitting assessment).
Fitting the contact Lens
Fitting philosophies
The three different types of contact lens fitting philosophies in keratoconus include apical clearance, apical bearing or three point touch; the three point touch being the most widely accepted one.[16]
Apical clearance
This is where there is no bearing or touch in the apical area i.e., the apical area is clear (vault is present) and the lens bearing is directed towards the periphery [Fig. 2]. This reduces the risk of scarring, whorl keratopathy and erosions but the tightening at the periphery may result in sealing of tear exchange.[16] These are usually smaller diameter steeper lenses, centered over the cone which is usually decentered in keratoconus. This can sometimes result in lens edge in the visual axis or optic zone bifurcating the pupil and flare or fluctuating vision.
Figure 2.
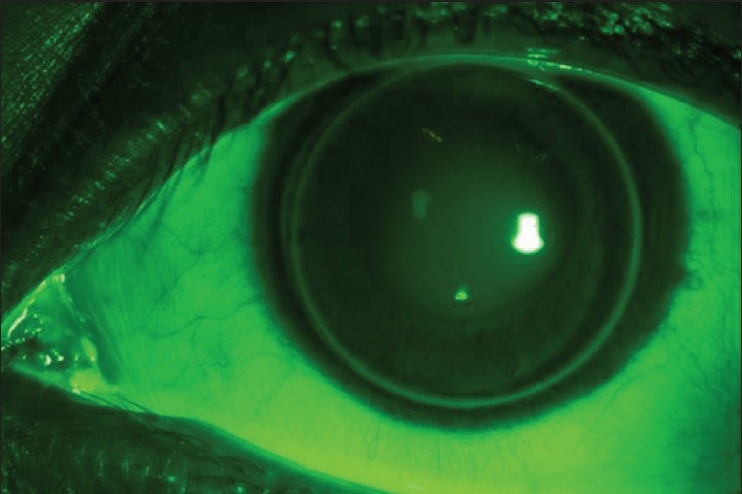
Apical clearance - Central fluorescein pooling and thin edge clearance is visible. The fit should be modified using a flatter base curve
Apical bearing
The optic zone of the contact lens touches or bears on the apex of the cone resulting in good visual acuity [Fig. 3]. Because of the flatter fitting of the lens on the cornea, there can be heavy bearing on the cornea. This can result in corneal scarring and intolerance over long term use. The quality of vision is better with apical bearing.
Figure 3.
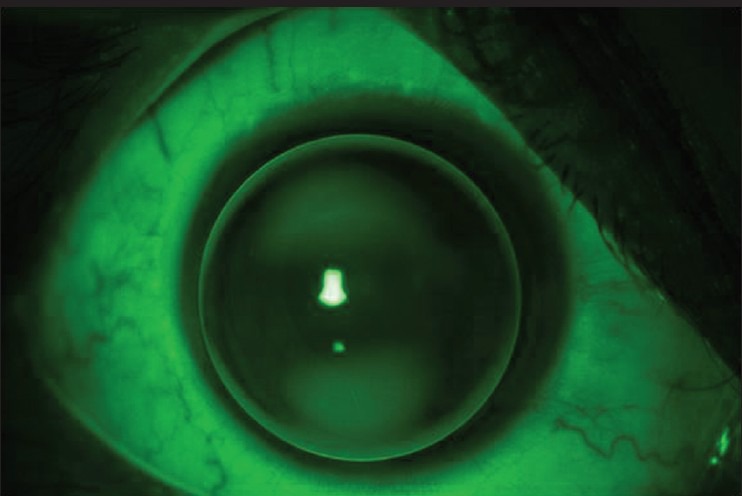
Apical bearing - Central bearing, seen as dark area because of lack of fluorescein in this area with thin edge clearance at 3 O’ Clock position, this can result in staining in the same area
Three point touch or divided support
Here, the lens bearing is shared between the apex and the midperipheral c ornea. This helps in minimizing the risk of apical scarring as well as facilitates the tear exchange [Fig. 4]. This is the most preferred type of lens fitting. It provides good vision, better comfort and prolonged wearing time.
Figure 4.
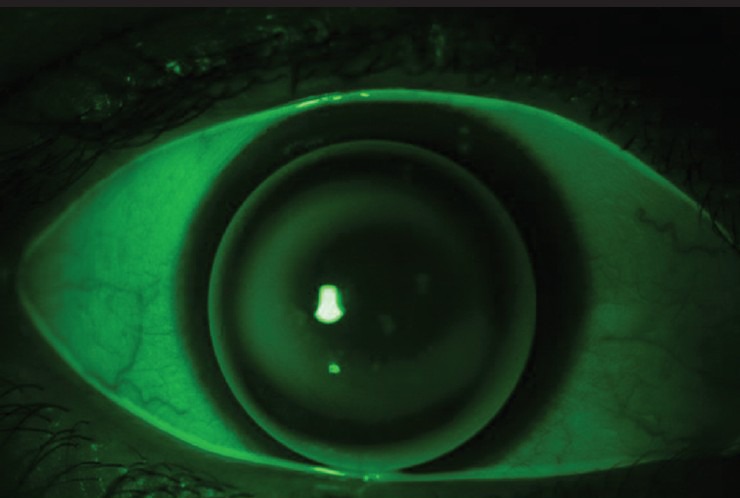
Diffuse fluorescein in the centre and midperiphery on either side depicting the divided touch or three point touch
The trial should be repeated until an acceptable dynamic and static fit is achieved. An ideal fit will show a central feather touch, a peripheral edge lift of 0.5-0.7 mm. But, as the cone advances, the lens edge may stand off with pooling and air bubbles under the peripheral edge. These peripheral edges can be steepened in meridians according to the area of clearance and edge lift sectorally as per company guidelines.
Rose K lenses
When the cone is a central nipple cone, a Rose K lens (Menicon Co., Ltd, Nagoya, Japan) can be selected. These lenses are multicurve lenses with a small optical zone which snugly fits the cone, for the so called ‘feather touch’ to the cornea. The company recommends the selection of first trial lenses to be 0.2 mm steeper than the average K for mild to moderate K values (average k reading is flatter than 6.00 mm). For advanced (average k values are between 5.1-6.00 mm) the first lens to be applied should be same as average k value and 0.3 mm flatter than the average k in severe cases (average k values are steeper than 5.00 mm).
Mandathara et al., had shown that selecting the initial trial lens BC based on the 5-mm average K will reduce the number of trial lenses and shorten the chair time in fitting Rose K lenses in keratoconic eyes.[2]
The success rate of fitting Rose K lens in keratoconus was reported to be more than 90%.[2,4,17] Mandathara et al., have shown similar results in 95% patients with an average number of trials being 1.73 (range: 1-5) and in 95% of the cases, the final fit was achieved within the first three trials.[2]
Once the optimal lens fit is achieved, the final power should be calculated after performing a spherical over refraction over the trial lens.
Rose K2 XL semi-scleral contact lens (Menicon Co. Ltd., Nagoya, Japan) is shown to improve visual acuity and comfort and can avoid the need for PBCL in the management of the irregular cornea.[18]
Intralimbal lenses
These are large diameter lenses ranging between 10.5-12 mm and are used for patients with moderate keratoconus, low sagging cones.[5] The large diameter helps in improving the lens centration and also reduces the movements of the lens. Standard lenses from local companies or Rose K2IC or Dyna Z intralimbal lenses (Lens Dynamics, Inc., Golden, CO) can be used for large cones or oval cones. A three point touch is preferred but the fitting with these lenses sometimes may not show the ideal fluorescein pattern.
As these are large lenses, patients may find it difficult to handle lenses of large diameters if they are using the lenses for the first time.[5]
Piggyback contact lenses
Piggyback contact lenses (PBCL) include two lenses on one eye; the RGP lens piggybacks i.e., is placed on a soft contact lens[13,19] [Fig. 5]. The indications are irregular corneas where RGP lenses fitting are not possible such as keratoconus, PMCD, post graft and post lasik ectasia. PBCL is indicated in patients with RGP discomfort or intolerance, unstable RGP on the eye, popping out of lens, 3 and 9 O’ clock staining with RGP fit and presence of scar.[19,20] A PBCL system is also indicated in some patients to improve comfort.
Figure 5.
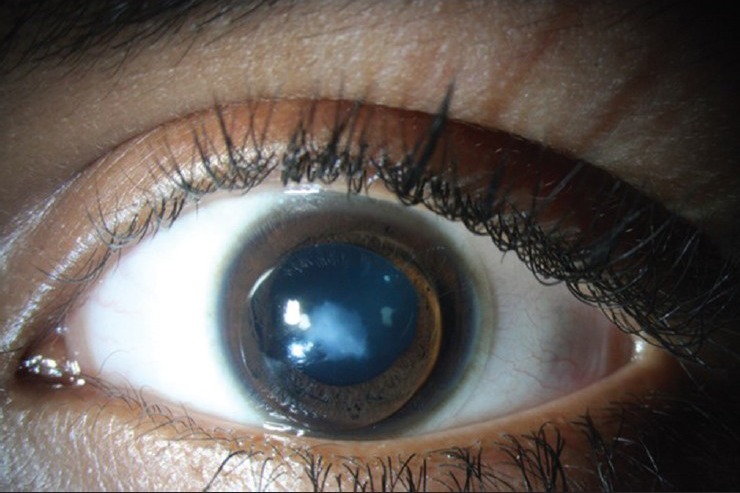
Piggy back contact lens in advanced keratoconus with corneal scar
Fitting of PBCL
A diagnostic soft contact lens is fitted first. As two lenses are to be used on the cornea, a silicone hydrogel lens is preferred - usually a minus power lens.[21] Once an optimal fit with the soft contact lens is obtained, either keratometry or corneal topography is performed over the lens surface to select the base curve of the RGP lens. Base curve of RGP is selected on a flat k value with a diameter ranging between 9 to 9.5 mm. Assessment of both the dynamic and static fit should be performed for RGP. The movements of the SCL and RGP lenses are independent of each other. After attaining optimal fits for both the SCL and RGP lens, over refraction is performed and the final subjective acceptance is added to the RGP power. Both lenses should be of high Dk material to minimize the risk of hypoxia.
One can modify the final fit of the RGP lens by modifying the power of the soft contact lens; a plus power SCL can be used to flatten the RGP and a minus power SCL can be used to steepen the RGP.[13]
Custom piggyback lenses (Flex lenses piggyback lens, X-Cel Contacts) are lathe cut lenses wherein a groove is present in the soft contact lens. In this groove, RGP lens which is 1mm smaller than the groove diameter is selected that remains in the groove. This allows the RGP to center well on the surface. In addition, the presence of RGP with a less thick lens edge in the groove improves the comfort because of minimal interaction with the lids. The reduced thickness compared to the SCL with no groove, reduces the recurrence of hypoxia related complications as compared to the thickness of the traditional PBCL system.
Though PBCL can improve vision and comfort, the disadvantages include lost RGP, giant papillary conjunctivitis (GPC), the difficulty in the care regimen of handling and maintaining two lenses and high risk of hypoxia changes because of two lenses on the corneal surface.[3,13,19]
Hybrid lenses
These lenses have a rigid lens in the centre and a soft skirt in the periphery. The most recent introduction in hybrid lenses is the SynergEyes lens (SynergEyes, Inc, Carlsbad, CA) with various designs. The Synergeyes lens has a central rigid gas permeable portion made of Paragon HDS100 material (Paflufocon D) bonded to the nonionic hydrophilic skirt material of 27% water (PolyHEMA hem-iberfilcon A). Indications include RGP intolerance or inability to obtain an optimal RGP fitting,[22] poor lens centering and reduced wearing time with the RGP lenses.[13]
The overall diameter of the lens is 14.5 mm. These lenses are fitted with no or minimal apical touch in the central cornea. The vault can be between 100-600 microns. The soft skirt should exhibit 0.25 mm blink induced movements. Abdalla et al., had found that 36.1% (22/61 eyes) needed refitting.[22] To avoid the tightening of the lenses over a period of time, now the lens is fitted towards a flatter side.[22] The RGP and soft skirt can be changed individually with different lenses. The lenses can be fitted on cones of any severity. The complications (31.1% - 19/61 eyes) noted with these lenses are GPC, tear in the soft skirt and not the junction, infection and discomfort.[22] The SynergEyes lens allows significantly more oxygen to reach the cornea during wear than the SoftPerm lens at the central cornea, or the 2.0 mm and 4.5 mm temporal to the central cornea.[23]
The other complications with SynergEyes include hypoxia related changes such as vascularisation and central corneal clouding.[24] The cornea should be examined for corneal oedema after 5 hours of ClearKone lens wear.[24]
Scleral contact lenses
True scleral lenses rest on the sclera and do not touch the cornea and limbus, leaving a clear area between the contact lens and the cornea. There is renewed interest over the last few years because of the availability of high Dk material and newer designs.[13,25,26,27] These lenses are indicated when all other contact lenses fail to improve the vision or because of inability to get an optimal fit with RGP, RGP intolerance, 3 and 9 O’ clock staining of the cornea, vascularisation with PBCL, advanced keratoconus or scarring in the cornea[25,26,27,28] [Fig. 6]. Even associated diseases such as VKC should not deter one from trying these lenses. The contraindications are presence of corneal oedema, acute hydrops and post filtration surgery. The fitting of the lens can be resumed after the hydrops heals.[29] The other indication for these lenses is prior to penetrating keratoplasty. The lenses can be non fenestrated or fenestrated. We describe the fitting of nonfenestrated scleral contact lens (PROSE, Prosthetic Replacement of the Ocular Surface Ecosystem, Boston Foundation for Sight, Needham Heights, Boston, MA, USA) that are filled with fluid prior to insertion in the eye.
Figure 6.
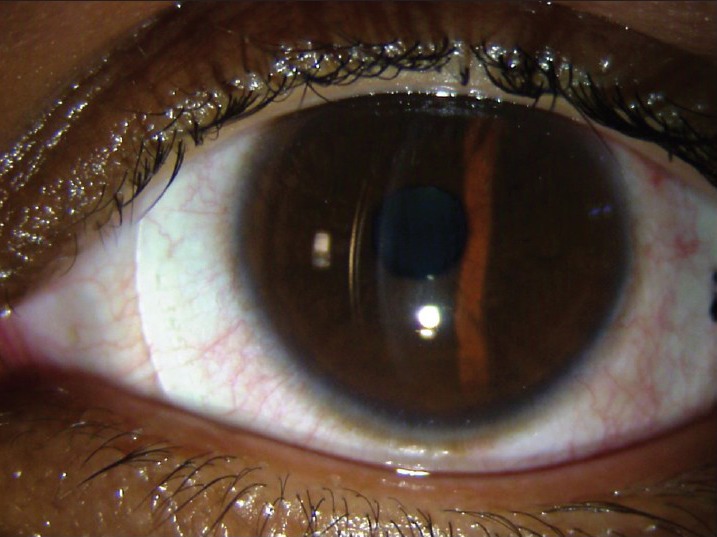
Haptic resting on sclera and the corneal clearance indicating adequate vault
Scleral lens fitting procedure
PROSE is lathe cut lens manufactured from dedicated software to customize the lens design for haptic bearing or the scleral portion of the lens and vaulting for corneal clearance of individual cornea.[27,30]
Slit lamp biomicroscopy aids in assessing the two main parameters: Haptic and vault. An acceptable fit is characterized by an adequate corneal clearance (no touch) with no air bubble in the fluid, and no impingement i.e. no compression of conjunctival vessels or edge lift. If the fit is acceptable, the lens can be left in the eye so that the patient experiences both comfort and improved vision during trial.
Either the trial can be continued on the same day or the patient can be called later for an extended trial of 4-6 h of continuous lens wear. This is required as the lens settles on the ocular surface.
The corneal clearance is assessed by noting the distance between the cornea and the back surface of the lens in the central area and this is compared with the peripheral corneal thickness or can be compared to the known lens thickness. A corneal clearance of 400-600 microns is acceptable. In a study conducted by us (unpublished data), we found that the corneal clearance reduces significantly after 4 h of lens wear and this needs to be increased before placing the final order for the lens. The vault can be kept in excess in patients with keratoconus considering the progression of keratoconus over follow-up.
Also, the presence of suction while removing the lens from the eye, aids in assessing the haptic portion of the lens. Fluorescein staining of the conjunctiva after lens removal aids in changing the haptic portion. If no suction is felt while removing the lens and no conjunctival staining and no debris collects in the vault after 4 h of lens wear, the lens can be ordered with power adjustment after performing subjective refraction. However, if suction is noted while removing the lens indicating a tighter lens on the ocular surface, a flatter haptic is required. It should be noted that, a flatter haptic will settle more on the surface and hence the vault should be increased.
Lenses are custom made depending on the stain pattern of the conjunctiva. If an overall stain pattern of 360 degree is noted, then the overall haptic is designed flatter and the vault is increased by 0.1 to 0.2. If the stain pattern is seen in one or two quadrants, indicating toric sclera, then the haptic can be designed with toricity.[27] Patients should be re-examined for final assessment of their lens fit three to four weeks after dispensing the lens. Unisol or normal saline is used to fill these lenses prior to the insertion in the eye. In keratoconus, the cornea clearance is between (150-600 microns) in fluid filled lenses with no air bubble. With fenestrated scleral lenses, the corneal clearance can be 40-80 microns.
The disadvantage is the care regimen of the scleral lenses, different insertion and removal technique using plungers and the frequent change of saline bottles. The fenestrated lenses are removed by applying the plunger at the centre. With non- fenestrated lenses, the plunger is applied at the junction of vault and haptic and lenses are removed. The advantage of scleral lenses, apart from the provision of improved comfort and stable visual acuity, is that it delays or obviates the need for keratoplasty.
Practical tips
For early cones (<50 D) – Start with traditional RGP or Rose k contact lens
For advanced cones – Start with lenses of small diameter - 8.7 mm - with a steeper base curve (start with 0.2 mm steeper than average k value).
Proud nebulae – With the corneal scar at the apex of the cone or proud nebulae, the patient may complain of irritation, watering and pain. The lens fit may not be acceptable because of the popping out of the lens. In such cases, both the raised surface can be treated with superficial keratectomy or excimer laser and the patients can restart contact lens wear,[31,32] or the patient can be given PBCL to improve the comfort. In addition, hybrid and scleral lenses can be fitted in such situations.
After Collagen cross linking - Once the defect heals, the patient can resume wearing contact lenses. Usually, the patients are asked to continue with their own lenses and later on when the topography and power changes, they can be asked to change the lenses accordingly. In our practice, we found that the fitting pattern of contact lens changed after cross linking, but the patient could nevertheless continue using the same lenses in 50% cases. Pre-surgery, 3-point-touch fit was in 24 eyes and central fluorescein pooling in 10 eyes. Post- surgery, 30 eyes had 3-point-touch and central fluorescein pooling was in 4 eyes. (Unpublished observation)
After keratoplasty - The patient may have either high astigmatism after keratoplasty or may have recurrence of keratoconus in the graft. The fitting philosophies are the same, but one may have to use large diameter lenses such as intralimbal lenses.
After intracorneal rings – Intracorneal rings improve the corneal surface topography and aid in fitting the RGP lenses in keratoconus. Also, all other lenses can be tried.
Keratoconus with corneal dystrophy – If the visual acuity is not explained by the opacities in a patient with corneal dystrophy, one should consider keratoconus and perform corneal topography and contact lens trial as the association of keratoconus and corneal dystrophy is well known.[32] The fitting philosophy remains the same.
Summary
Fitting contact lens in keratoconus can improve the vision and delay or obviate the need for keratoplasty. Though the fitting takes longer chair time, with the availability of newer materials and designs in the market, it is possible to fit many keratoconic patients. The lens of choice is RGP lens and if the patient develops discomfort or intolerance, then one can go in for customized soft toric lenses or PBCL and later on, if required, hybrid lenses can be considered. Scleral lenses are used when all other options fail or the patient has associated ocular disease such as vernal keratoconjunctivitis.
Footnotes
Source of Support: Hyderabad Eye Institute, Hyderabad, India.
Conflict of Interest: None declared.
References
- 1.Rabinowitz YS. Keratoconus. Surv Ophthalmol. 1998;42:297–319. doi: 10.1016/s0039-6257(97)00119-7. [DOI] [PubMed] [Google Scholar]
- 2.Mandathara Sudharman P, Rathi V, Dumapati S. Rose K lenses for keratoconus-An Indian experience. Eye Contact Lens. 2010;36:220–2. doi: 10.1097/ICL.0b013e3181e5cd0b. [DOI] [PubMed] [Google Scholar]
- 3.Kok JH, van Mil C. Piggyback lenses in keratoconus. Cornea. 1993;12:60–4. doi: 10.1097/00003226-199301000-00010. [DOI] [PubMed] [Google Scholar]
- 4.Jain AK, Sukhija J. Rose-K contact lens for keratoconus. Indian J Ophthalmol. 2007;55:121–5. doi: 10.4103/0301-4738.30706. [DOI] [PubMed] [Google Scholar]
- 5.Ozbek Z, Cohen EJ. Use of intralimbal rigid gas-permeable lenses for pellucid marginal degeneration, keratoconus, and after penetrating keratoplasty. Eye Contact Lens. 2006;32:33–6. doi: 10.1097/01.icl.0000174759.91179.30. [DOI] [PubMed] [Google Scholar]
- 6.Nosch DS, Ong GL, Mavrikakis I, Morris J. The application of a computerised videokeratography (CVK) based contact lens fitting software programme on irregularly shaped corneal surfaces. Cont Lens Anterior Eye. 2007;30:239–48. doi: 10.1016/j.clae.2007.06.003. [DOI] [PubMed] [Google Scholar]
- 7.Sorbara L, Dalton K. The use of video-keratoscopy in predicting contact lens parameters for keratoconic fitting. Cont Lens Anterior Eye. 2010;33:112–8. doi: 10.1016/j.clae.2010.01.002. [DOI] [PubMed] [Google Scholar]
- 8.Edrington TB, Szczotka LB, Barr JT, Achtenberg JF, Burger DS, Janoff AM, et al. Rigid contact lens fitting relationships in keratoconus. Collaborative Longitudinal Evaluation of Keratoconus (CLEK) Study Group. Optom Vis Sci. 1999;76:692–9. [PubMed] [Google Scholar]
- 9.Buxton JN, Buxton DF, Dias AK, Scorsetti DH. The CLAO Guide to Basic Science and Clinical Practice. 3rd ed. Vol. 3. Iowa: Kendall/Hunt; 1995. Keratoconus Basic and Clinical Features; pp. 101–22. [Google Scholar]
- 10.Perry HD, Buxton JN, Fine BS. Round and oval cones in keratoconus. Ophthalmology. 1980;87:905–9. doi: 10.1016/s0161-6420(80)35145-2. [DOI] [PubMed] [Google Scholar]
- 11.Barr JT, Zadnik K, Wilson BS, Edrington TB, Everett DF, Fink BA, et al. Factors associated with corneal scarring in the Collaborative Longitudinal Evaluation of Keratoconus (CLEK) Study. Cornea. 2000;19:501–7. doi: 10.1097/00003226-200007000-00020. [DOI] [PubMed] [Google Scholar]
- 12.Jinabhai A, Radhakrishnan H, Tromans C, O’Donnell C. Visual performance and optical quality with soft lenses in keratoconus patients. Ophthalmic Physiol Opt. 2012;32:100–16. doi: 10.1111/j.1475-1313.2011.00889.x. [DOI] [PubMed] [Google Scholar]
- 13.Barnett M, Mannis MJ. Contact lenses in the management of keratoconus. Cornea. 2011;30:1510–6. doi: 10.1097/ICO.0b013e318211401f. [DOI] [PubMed] [Google Scholar]
- 14.Gonzalez-Meijome JM, Jorge J, de Almeida JB, Parafita MA. Soft contact lenses for keratoconus: Case report. Eye Contact Lens. 2006;32:143–7. doi: 10.1097/01.icl.0000179707.85290.f4. [DOI] [PubMed] [Google Scholar]
- 15.Fernandez-Velazquez FJ. Kerasoft IC compared to Rose-K in the management of corneal ectasias. Cont Lens Anterior Eye. 2012;35:175–9. doi: 10.1016/j.clae.2012.02.005. [DOI] [PubMed] [Google Scholar]
- 16.Leung KK. RGP fitting philosophies for keratoconus. Clin Exp Optom. 1999;82:230–5. doi: 10.1111/j.1444-0938.1999.tb06653.x. [DOI] [PubMed] [Google Scholar]
- 17.Betts AM, Mitchell GL, Zadnik K. Visual performance and comfort with the Rose K lens for keratoconus. Optom Vis Sci. 2002;79:493–501. doi: 10.1097/00006324-200208000-00011. [DOI] [PubMed] [Google Scholar]
- 18.Romero-Jimenez M, Flores-Rodriguez P. Utility of a semi-scleral contact lens design in the management of the irregular cornea. Cont Lens Anterior Eye. 2013;36:146–50. doi: 10.1016/j.clae.2012.12.006. [DOI] [PubMed] [Google Scholar]
- 19.Yeung K, Eghbali F, Weissman BA. Clinical experience with piggyback contact lens systems on keratoconic eyes. J Am Optom Assoc. 1995;66:539–43. [PubMed] [Google Scholar]
- 20.Sengor T, Kurna SA, Aki S, Ozkurt Y. High Dk piggyback contact lens system for contact lens-intolerant keratoconus patients. Clin Ophthalmol. 2011;5:331–5. doi: 10.2147/OPTH.S16727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Romero-Jimenez M, Santodomingo-Rubido J, Flores-Rodriguez P, Gonzalez-Meijome JM. Which soft contact lens power is better for piggyback fitting in keratoconus? Cont Lens Anterior Eye. 2013;36:45–8. doi: 10.1016/j.clae.2012.10.070. [DOI] [PubMed] [Google Scholar]
- 22.Abdalla YF, Elsahn AF, Hammersmith KM, Cohen EJ. SynergEyes lenses for keratoconus. Cornea. 2010;29:5–8. doi: 10.1097/ICO.0b013e3181a9d090. [DOI] [PubMed] [Google Scholar]
- 23.Pilskalns B, Fink BA, Hill RM. Oxygen demands with hybrid contact lenses. Optom Vis Sci. 2007;84:334–42. doi: 10.1097/OPX.0b013e3180421748. [DOI] [PubMed] [Google Scholar]
- 24.Fernandez-Velazquez FJ. Severe epithelial edema in Clearkone SynergEyes contact lens wear for keratoconus. Eye Contact Lens. 2011;37:381–5. doi: 10.1097/ICL.0b013e31822a33a6. [DOI] [PubMed] [Google Scholar]
- 25.Pullum KW, Buckley RJ. A study of 530 patients referred for rigid gas permeable scleral contact lens assessment. Cornea. 1997;16:612–22. [PubMed] [Google Scholar]
- 26.Schornack MM, Patel SV. Scleral lenses in the management of keratoconus. Eye Contact Lens. 2010;36:39–44. doi: 10.1097/ICL.0b013e3181c786a6. [DOI] [PubMed] [Google Scholar]
- 27.Rathi VM, Mandathara PS, Dumpati S, Vaddavalli PK, Sangwan VS. Boston ocular surface prosthesis: An Indian experience. Indian J Ophthalmol. 2011;59:279–81. doi: 10.4103/0301-4738.81994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Segal O, Barkana Y, Hourovitz D, Behrman S, Kamun Y, Avni I, et al. Scleral contact lenses may help where other modalities fail. Cornea. 2003;22:308–10. doi: 10.1097/00003226-200305000-00006. [DOI] [PubMed] [Google Scholar]
- 29.Rathi VM, Sudharman Mandathara P, Vaddavalli PK, Dumpati S, Chakrabarti T, Sangwan VS. Fluid-filled scleral contact lenses in vernal keratoconjunctivitis. Eye Contact Lens. 2012;38:203–6. doi: 10.1097/ICL.0b013e3182482eb5. [DOI] [PubMed] [Google Scholar]
- 30.Rosenthal P, Croteau A. Fluid-ventilated, gas-permeable scleral contact lens is an effective option for managing severe ocular surface disease and many corneal disorders that would otherwise require penetrating keratoplasty. Eye Contact Lens. 2005;31:130–4. doi: 10.1097/01.icl.0000152492.98553.8d. [DOI] [PubMed] [Google Scholar]
- 31.Moodaley L, Liu C, Woodward EG, O’Brart D, Muir MK, Buckley R. Excimer laser superficial keratectomy for proud nebulae in keratoconus. Br J Ophthalmol. 1994;78:454–7. doi: 10.1136/bjo.78.6.454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Moodaley L, Buckley RJ, Woodward EG. Surgery to improve contact lens wear in keratoconus. CLAO J. 1991;17:129–31. [PubMed] [Google Scholar]


