Abstract
In this brief review we will discuss the reasoning and evolution of our current use of combined very high-fluence collagen crosslinking and laser in situ keratomileusis. Several presentations and pertinent publications are reviewed, along with the key steps of the enhanced LASIK procedure. Long term outcome data support the safety and efficacy of LASIK Xtra in stabilizing myopic but also hyperopic LASIK results. In conclusion, we have compelling evidence that LASIK Xtra is a safe and effective adjunct.
Keywords: Laser in situ keratomileusis surgery, very high fluence collagen cross-linking, corneal ectosia, LASIK ectosia prophylaxis
We started using collagen cross-linking as a means to stabilize post-refractive surgery ectasia and progressive keratoconus in younger patients back in 2002. At the time, we used the classic Dresden Protocol, which entailed 3 MW/cm2 ultraviolet radiation (UV) fluence of, at average wavelength 370 nm. It should be noted that this is not a laser treatment, this is a broader spectrum treatment and after instilling 0.1% riboflavin solution stabilized in 10% dextran solution for 30 min.
We had relative success and we have published several reports on stabilizing laser-assisted in situ keratomileusis (LASIK) ectasia and progressive keratoconus. In the years to come, we introduced several novel techniques of corneal collagen cross-linking (CXL).[1,2,3,4,5,6,7,8,9,10] In an attempt although to change the surgical technique and make it more patient friendly, we introduced at the European Society of Cataract and Refractive Surgeons (ESCRS) Meeting in 2007, the concept of creating a femtosecond laser pocket within the cornea, instilling within this pocket riboflavin solution and using higher fluence UV light to achieve collagen cross-linking within the corneal stroma. The advantages of this technique are obvious; there is no deepithelialization, no pain, and immediate rehabilitation. And in the first of its kind clinical study, which was published in 2009, we showed that this technique held relative success and promise as an alternate technique to the standard Dresden Protocol and at the same time, introduced the concept of higher fluence collagen CXL.
We employed a version of this technique and published that in 2009 as well, as a means of deturgescing very edematous corneas, such as in bullous keratopathy. And it was this work which brought the inception of the idea of using prophylactic collagen cross-linking within the flap in routine LASIK cases. We presented the first case series at the 2nd International CXL meeting in Zurich as well as the ESCRS meetings and the academy meetings over the next years, and published our results after we achieved long-term stability and had significant follow-up to determine the high level of safety of this technique.
Just to reiterate the key points in this prophylactic treatment, the whole purpose of the treatment is to avoid having riboflavin solution being absorbed by the LASIK flap. So after the laser ablation is completed and with the LASIK flap folded onto itself and being protected with a dry Wexel sponge, one drop of riboflavin 0.1% not diluted in Dextran but in saline (this is called VibeX Xtra, made by Avedro) is placed on the exposed stromal bed and carefully spread over the bed only with an irrigating cannula. Special attention is taken not to have that drop soak onto the folded flap and its hinge [Fig. 1]. The soaking continues for just 60 s and then the flap is repositioned into place, the residual riboflavin irrigated and the flap secured in place. In my particular technique, I use a Johnston applanator to iron out the little kinks that may be available and may have been produced in the flap and then very high fluence collagen cross-linking takes place [Fig. 2].
Figure 1.
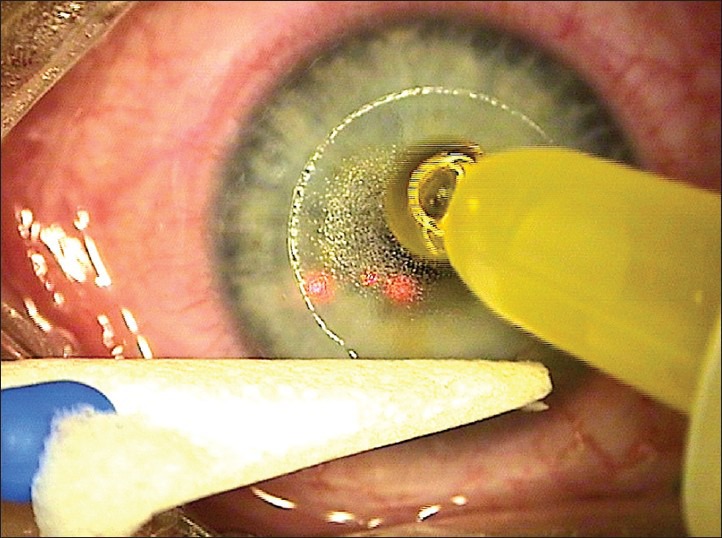
The riboflavin solution is applied over the bare stroma without contact with the laser in situ keratomileusis surgery (LASIK) flap for 60 s
Figure 2.
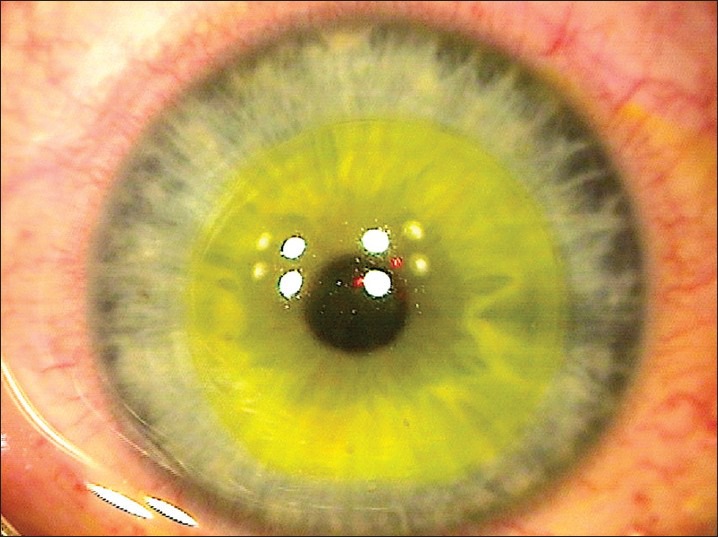
The flap is repositioned and prior to application of higher fluence ultraviolet (UV) light the riboflavin yellow-tinge is visualized in the corneal stroma
In our initial clinical work, we use 10 MW/cm2 for a total of 3 min duration and after the introduction of the Avedro KXL device, we took advantage of the even higher fluence of 30 MW/cm2, for a total of 80 s, in order to achieve collagen cross-linking. We have since performed thousands of successful LASIK Xtra procedures and we view this prophylactic treatment as a pivotal biomechanical enhancement of a LASIK procedure in a young adult, so any patient that is under 30, any patient we correct myopia over 6 D, and any patient that there is astigmatism over 1 D, and any patient that there is a difference in the amount of the astigmatism between the two eyes of over 0.5 D. This represents almost 70% of our routine myopic LASIK practice.
In closing, one of the interesting things with LASIK Xtra is that in our early clinical work, whether it be utilized in hyperopic LASIK, we are astounded by the tremendous stability that LASIK Xtra offered in hyperopia and we decided back in 2009 to start a contralateral eye study where one eye, which had hyperopic LASIK Xtra, received the routine that we described before, and the other eye was just hyperopic LASIK without any cross-linking. With following-up this significant number of cases for over 2 years, we were astounded to find a compelling difference in the amount of subsequent flattening that happened in the eyes that did not receive prophylactic cross-linking versus the eyes that had, therefore establishing LASIK Xtra as a possible mandatory adjunct to hyperopic LASIK.
Our theory, as we published, supports the fact that hyperopic LASIK has an intrinsic biomechanical response, which results in progressing flattening of the central cornea, which begins 6 months after the procedure and can be noted even 5 years after hyperopic LASIK procedure. Therefore, hyperopic LASIK Xtra, by reinforcing the biomechanical behavior of the cornea, counteracts this intrinsic progressive flattening of the hyperopic LASIK corneas and therefore offering higher stability and the ability to treat higher degrees of hyperopia with LASIK Xtra. In Fig. 3, the hyperreflectivity in corneal optical coherence tomography (OCT) is seen around the flap in hyperopic LASIK xtra. Of course, the future and longer follow-ups will establish these findings. These findings of very high fluence CXL used in manipulating corneal biomechanics and possibly refraction were also applied in our novel introduction of high fluence CXL in femtosecond laser astigmatic keratotomy, with great enhancement of the effect.
Figure 3.
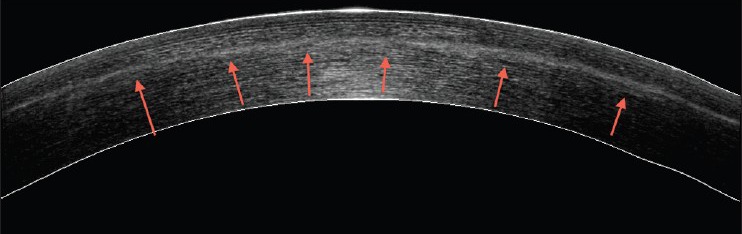
This is an anterior segment optical coherence tomography (AS-OCT) image of a treated cornea. There is evident hyperreflectivity visualized over and under the LASIK flap underlined by the red arrows
Although LASIK has established itself in the literature as being a safe and relatively stable procedure, when we studied keratometry in very large cohorts of LASIK patients, both from myopia and hyperopia, we did see long-term changes, which may not necessarily be reflected in refraction and visual acuities. So if one uses as a distinct biological marker, keratometry, the entity that possibly changes after LASIK, one may become convinced that LASIK Xtra can offer better results.
Finally, does LASIK Xtra cause any problems in visual quality? We are currently evaluating with the Oculus C-Quant device over the last 6 months and have studied routine LASIK cases and LASIK Xtra cases, and we have established that there is no additional scatter induced by the LASIK Xtra cases, which adds another point of safety for this procedure.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Kanellopoulos AJ. Geneva, Switzerland: Invited speaker at 8th International Congress of Corneal Cross-linking (CXL); 2012. Dec 8, Reduction of femtosecond astigmatic keratotomy (fsAK) regression with combined simultaneous high fluence CXL (hfCXL): A novel refractive procedure; pp. 52–9. [Google Scholar]
- 2.Kanellopoulos AJ, Binder PS. Collagen cross-linking (CCL) sequential topography-guided PRK: A temporizing alternative for keratoconus to penetrating keratoplasty. Cornea. 2007;26:891–5. doi: 10.1097/ICO.0b013e318074e424. [DOI] [PubMed] [Google Scholar]
- 3.Kanellopoulos AJ. Comparison of sequential vs same-day simultaneous collagen cross-linking and topography-guided PRK for treatment of keratoconus. J Refract Surg. 2009;25:S812–8. doi: 10.3928/1081597X-20090813-10. [DOI] [PubMed] [Google Scholar]
- 4.Kanellopoulos AJ. Collagen cross-linking in early keratoconus with riboflavin in a Femtosecond Laser-created pocket: Initial clinical results. J Refract Surg. 2009;25:1034–7. doi: 10.3928/1081597X-20090901-02. [DOI] [PubMed] [Google Scholar]
- 5.Krueger RR, Kanellopoulos A. Stability of simultaneous topography-guided photorefractive keratectomy and riboflavin/UVA cross-linking for progressive keratoconus: Case reports. J Refract Surg. 2010;26:S827–32. doi: 10.3928/1081597X-20100921-11. [DOI] [PubMed] [Google Scholar]
- 6.Kanellopoulos AJ, Binder PS. Management of corneal ectasia after LASIK with combined, same-day, topography-guided partial transepithelial PRK and collagen cross-linking: The Athens Protocol. J Refract Surg. 2011;27:323–31. doi: 10.3928/1081597X-20101105-01. [DOI] [PubMed] [Google Scholar]
- 7.Kanellopoulos AJ. Long term results of a prospective randomized bilateral eye comparison trial of higher fluence, shorter duration ultraviolet: A radiation, and riboflavin collagen cross linking for progressive keratoconus. Clin Ophthalmol. 2012;6:97–101. doi: 10.2147/OPTH.S27170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kanellopoulos AJ. Laboratory evaluation of selective in situ refractive cornea collagen shrinkage with continuous wave infrared laser combined with transepithelial collagen cross-linking: A novel refractive procedure. Clin Ophthalmol. 2012;6:645–52. doi: 10.2147/OPTH.S31250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kanellopoulos AJ. Long term safety and efficacy follow-up of prophylactic higher fluence collagen cross-linking in high myopic laser-assisted in situ keratomileusis. Clin Ophthalmol. 2012;6:1125–30. doi: 10.2147/OPTH.S31256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kanellopoulos AJ, Khan J. Topography-guided hyperopic LASIK with and without high irradiance collagen cross-linking: Initial comparative clinical findings in a contralateral eye study of 34 consecutive patients. J Refract Surg. 2012;28:S837–40. doi: 10.3928/1081597X-20121005-05. [DOI] [PubMed] [Google Scholar]


