Abstract
Corneal collagen cross-linking with riboflavin and UVA light (CXL) is the only method designed to arrest the progression of keratoconus. Visual improvement generally starts 3 months after treatment. Reduction is coma seen on aberrometry in early postoperative phase is also responsible for the improvement in visual acuity. In the light of currently available data we can thus say that CXL is a safe procedure that is successful in arresting keratoconus.
Keywords: Cornea collagen cross linking, keratoconus, long term results
Corneal collagen cross-linking with riboflavin and UVA light (CXL) is the only method designed to arrest the progression of keratoconus. Spoerl et al. were the first to report the use of cross-linking for stabilizing the cornea.[1] In recent years, it is a preferred method for targeting the stromal instability. It is popular treatment worldwide and is offered at various centers offering this option. The single most important outcome with CXL is the expected reduction in the need for donor keratoplasty. Our own study and several other studies have reported results upto 12 months after performing CXL.[2] However, studies for longer periods of follow-up are few. Even these report results on small cohorts followed up for 4 to 6 years after treatment.[3,4,5,6] The studies with long-term data have been performed with the corneal epithelium scraped off and thus, this discussion is restricted to studies performed with the epithelium-off method.
Visual improvement generally starts 3 months after treatment.[3] There is a temporary visual reduction seen in the early postoperative phase. This is due to stromal edema evident in 100% of eyes with confocal microscopy.[4] Average visual improvement has been between 1 and 2 Snellen lines from 1 to 4 years after treatment.[5,6] This is corroborated by our unpublished results over the last 5 years. We have also noted continuing minor changes in topography in patients over time [Fig. 1]. The improved uncorrected visual acuity can be partially explained by reduction in the sphere and the spherical equivalent reduction. Reduction is coma seen on aberrometry in early postoperative phase is also responsible for the improvement in visual acuity.[2] This reduction of values has been maintained up to 36 to 48 months.[5]
Figure 1.
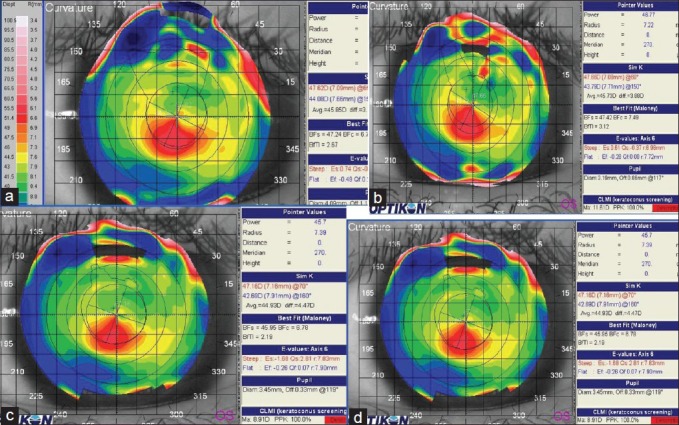
Sequential topography changes seen in one eye of a patient over 31 months. Note the generalized flattening of the cone and the shrinkage of the steepened areas. Also note the change in Best fit sphere as well as the Sim K values. (a) at baseline (b) at 8 months (c) at 20 months and (d) 31 months post-Cross Linking
In an uncontrolled retrospective study, Raiskup-Wolf et al.[6] showed that the flattening process continues over a period of years: They followed a large cohort of patients (480 eyes of 272 patients) for up to 6 years and reported arrested keratoconus progression and significant improvements in visual acuity. The long-term stabilization of keratoconic corneas without significant side-effects has also been demonstrated in 44 eyes for up to 48 months after CXL,[5] also accompanied by a reduction in the mean K value by 2 diopters and gradually increasing improvements in uncorrected visual acuity (UCVA) and best corrected visual acuity (BCVA) during the observation period. The statistical significance of these values was maintained after 36 and 48 months of follow up [Table 1].
Table 1.
Results from some clinical trials using the standard Cross-Linking procedure
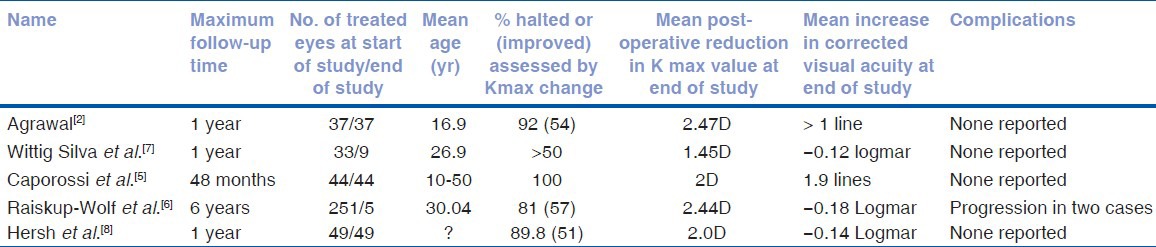
Randomized clinical trials (RCT), the holy grail of clinical evaluation, have reported data till one year of follow-up. These too have shown arrest of keratoconus along with improvement in visual acuity and keratometry values.[7,8]
In the Melbourne study,[7] which was conducted in 49 patients, statistically significant differences were observed between control and treatment groups in terms of BCVA and K values for up to 12 months after CXL. More recently, another group has published an RCT reporting on one-year results after CXL for the treatment of keratoconus and corneal ectasia.[8]
Risk factors for visual loss after CXL have been noted to be age over 35 years, pre-procedure corrected visual acuity of 20/25 or better, and a K value of more than 58D.[9] In our unpublished data, we observed in 3 patients the initial arrest of progression for 24 months after treatment and later had progression (increase in the Max K value by more than 0.5D). We are unable to find a cause to this specific situation. Repeat CXL performed in these 3 eyes prevented further progression over 24 months after repeat CXL.
The procedure is reported to be safe and without any severe complications. Infectious keratitis and corneal melt have been reported.[10] However, it is likely that the contact with the microbial agents causing infection or melt can occur during the epithelial healing phase and may not be directly attributable to the procedure itself.
In the light of currently available data, we can thus say that CXL is a safe procedure that is successful in arresting keratoconus. It is advisable to perform this procedure in patients with progressive keratoconus. Younger patients tend to have a more aggressive course, and thus should be offered this procedure too. It should no longer be considered as an elective procedure.[9]
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Spoerl E, Huble M, Kasper M, Sieler T. Increased rigidity of cornea caused by intrastromal cross-linking. Ophthalmologe. 1997;94:902–6. doi: 10.1007/s003470050219. [DOI] [PubMed] [Google Scholar]
- 2.Agrawal VB. Corneal collagen cross-linking with riboflavin and Ultra violet A light for keratoconus: Results in Indian eyes. Indian J Ophthalmol. 2009;57:111–4. doi: 10.4103/0301-4738.44515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mazotta C, Balestrazi A, Baiocchi S, Traversi C, Caporossi A. Stromal haze after combined riboflavin-UVA corneal collagen cross-linking in keratoconus: In vivo confocal microscopic evaluation. Clin Experiment Ophthalmol. 2007;35:580–2. doi: 10.1111/j.1442-9071.2007.01536.x. [DOI] [PubMed] [Google Scholar]
- 4.Mazotta C, Traversi C, Baiocchi S, Caporossi O, Bovone C, Sparano MC, et al. Corneal healing after riboflavin ultraviolet-A collagen cross-linking determined by confocal laser scanning microscopy in vivo early and late modifications. Am J Ophthalmol. 2008;146:527–33. doi: 10.1016/j.ajo.2008.05.042. [DOI] [PubMed] [Google Scholar]
- 5.Caporossi A, Mazzotta C, Baiocchi S, Caporossi T. Long-term results of riboflavin ultraviolet A corneal collagen cross-linking for keratoconus in Italy: The Seina eye cross study. Am J Ophthalmol. 2010;149:585–93. doi: 10.1016/j.ajo.2009.10.021. [DOI] [PubMed] [Google Scholar]
- 6.Raiskupf-Wolf R, Hoyer A, Spoerl E, Pillunat L. Collagen crosslinking with riboflavin and ultraviolet-A light in keratoconus: Long term results. J Cataract Refract Surg. 2008;34:796–801. doi: 10.1016/j.jcrs.2007.12.039. [DOI] [PubMed] [Google Scholar]
- 7.Wittig-Silva C, Whiting M, Lamoureux E, Lindsay LG, Sullivan LJ, Snibson GR. A randomized controlled trial of corneal collagen cross-linking in progressive keratoconus: Preliminary results. J Refract Surg. 2008;24:S720–5. doi: 10.3928/1081597X-20080901-15. [DOI] [PubMed] [Google Scholar]
- 8.Hersh PS, Greenstein A, Fry KL. Corneal collagen cross linking for keratoconus and corneal ectasia: One year results. J Cataract Refract Surg. 2011;37:149–60. doi: 10.1016/j.jcrs.2010.07.030. [DOI] [PubMed] [Google Scholar]
- 9.Koller T, Mrochen M, Seiler T. Complication and failure rates after corneal crosslinking. J Cataract Refract Surg. 2009;35:1358–62. doi: 10.1016/j.jcrs.2009.03.035. [DOI] [PubMed] [Google Scholar]
- 10.Sharma N, Maharana P, Singh G, Titiyal JS. Pseudomonas keratitis after collagen cross linking for keratoconus: Case report and review of literature. J Cataract Refract Surg. 2010;36:517–20. doi: 10.1016/j.jcrs.2009.08.041. [DOI] [PubMed] [Google Scholar]


