Abstract
Keratoconus is a progressive ectatic disorder of the cornea which often presents with fluctuating refraction and high irregular astigmatism. Correcting the vision of these patients is often a challenge because glasses are unable to correct the irregular astigmatism and regular contact lenses may not fit them very well. Topography-guided custom ablation treatment (T-CAT) is a procedure of limited ablation of the cornea using excimer laser with the aim of regularizing the cornea, improving the quality of vision and possibly contact lens fit. The aim of the procedure is not to give a complete refractive correction. It has been tried with a lot of success by various groups of refractive surgeons around the world but a meticulous and methodical planning of the procedure is essential to ensure optimum results. In this paper, we attempt to elucidate the planning for a T-CAT procedure for various types of cones and asphericities.
Keywords: Keratoconus, topography-guided custom ablation treatment, treatment
The major problem with keratoconus and other corneal ectatic disorders is progressive, asymmetrical corneal steepening associated with an increase in myopic and astigmatic refractive errors, combined with midperipheral and/or peripheral corneal thinning. High irregular astigmatism is typically seen with keratoconus, which is difficult to treat with spectacles and/or contact lenses. In the past, treatment of corneas with keratoconus using excimer laser was difficult as well as considered inappropriate, as the laser treatment results in further thinning of the cornea, and possible destabilization of the corneal structure. This could lead to progressive deterioration of the corneal shape and worsening of ectasia. Further, options for correcting irregular astigmatism induced by these ectatic disorders were few in the past, with limited and unpredictable anatomical and functional outcomes.[1] Recently, however, improvements in laser technology have led to several options for dealing with irregular astigmatism.[2,3,4,5,6,7,8,9,10,11,12]
There are two customized approaches for treatment of irregular astigmatism: Wavefront-guided[3,4,5,6,7,8,9] and corneal topography-guided treatments.[10,11,12,13,14] Wavefront-guided treatment was used in the past for aberrated corneas, but the difficulty remained in capturing satisfactory and repeatable images especially in highly irregular corneas, thereby, not allowing for satisfactory treatment in severely aberrated eyes.
Topography-guided excimer laser ablation was introduced more than 10 years ago, primarily for the treatment of highly aberrated and irregular corneas. The concept of topography-guided laser ablation is to modify the cornea by treating anatomical rather than physiological changes, and consequently is less influenced by intraocular factors than wavefront-guided laser ablation. The topography-guided custom ablation treatment (T-CAT) is designed to improve the central corneal symmetry, without attempting to correct other spherical, or regular astigmatic, optical defects. By not attempting to correct the whole optical defect of the eye, the T-CAT treatment can be kept to a small degree of ablation with the maximum depth of tissue loss typically being less than 50 μm. Since the procedure is done after removing the epithelium, similar to a photorefractive keratectomy (PRK) the terminology of topography-guided-PRK (TPRK) can be used interchangeably with T-CAT. However, while a topography-guided correction can improve the topography and corrected distance visual acuity (CDVA), the refraction is not always predictable. The custom topographical neutralization technique (TNT) was developed[15] to provide a neutralizing refractive effect to compensate for refractive changes in a single treatment. Although the article elaborately explains the technique for zone enlargement and neutralization of irregular cornea, the effectiveness of the procedure in keratoconus eyes has not been as clearly elucidated by the authors.
The use of topical riboflavin combined with ultraviolet A (UVA) irradiation in collagen cross-linking (CXL) has demonstrated the potential for retarding the progression of keratoconus. Kanellopoulos et al.,[16] first reported CXL to stabilize keratoconus progression followed by customized PRK to normalize the corneal surface by reducing irregular astigmatism and potentially reducing the refractive error as well as providing improved visual outcomes in addition to stabilizing the disease process.[17,18]
We present our technique in patients with keratoconus who underwent combined same-day T-CAT followed by accelerated CXL (Avedro Inc., Waltham, USA) to achieve stabilization of corneal ectasia and enhance visual rehabilitation.
Materials and Methods
Our protocol to define progression of keratoconus is an increase of 0.5 diopter (D) or more in two or more keratometry values in the steep meridian between two sagittal curve maps or a decrease in corneal thickness of 10% or more at the thinnest point between two pachymetry maps on Pentacam (Oculus, Wetzlar, Germany) in the last 6 months. Pre-operative thinnest pachymetry of 450 μm or a predicted post-operative thinnest pachymetry of at least 400 μm after T-CAT is a prerequisite.
Pre-operative assessment
Each patient undergoes assessment of uncorrected visual acuity (UCVA) and best corrected visual acuity (BCVA) on the Snellen's chart, which was converted into decimal values for reporting and analysis. Corneal topography was performed using Pentacam (Oculus) and Topolyzer, (WaveLight Laser Technologie AG, Erlangen, Germany). Corneal thickness was measured using the Pentacam. Five readings, one central and four from each of the four quadrants acquired from the Pentacam were used for the T-CAT treatment planning. Corneal asphericity (Q) was measured using the Topolyser.
Inclusion criteria
Mild-to-moderate grade Keratoconus
Thinnest pachmetry >450 μm
Poor contact lens fit/unhappy with glasses or contact lenses
No active allergic eye disease.
No active ocular inflammation
No central scarring of the cornea
Surgical procedure
After instilling a topical anesthetic solution (proparacaine 0.5%), an 8-mm diameter zone of corneal epithelium is mechanically removed and the customized ablation performed. T-CAT is performed by linking the Topolyzer with the WaveLightAllegretto Wave™ Excimer Laser System (WaveLight Laser Technologie AG). The software uses data from eight topographies and averages the data. “No tilt” option is chosen in all cases. In order to remove the minimum possible tissue, the optical zone diameter is kept between 5.5 and 6.5 mm in all cases. The maximum ablation we perform is 40 μm in the thinnest region of the cornea. Zernike optimization is done in all patients to match defocus (C4) and spherical aberration (C12) keeping the refractive correction as zero. The aim of the procedure is to topographically neutralize the cornea, making it more regular, and is not necessarily a reduction in the spherical equivalent of the eye. Therefore, the procedure is targeted to make the cornea more aspheric, improve contact lens fitting post-operatively and assure better BCVA to the patient by reducing the corneal aberrations and is therefore not a ‘refractive correction’ such as LASIK or photorefractive keratectomy (PRK) Figs. 1 and 2.
Figure 1.
Simulated visual acuity in a keratoconus patient before treatment showing blurred vision with aberrations on the iTrace Visual Function Analyzer
Figure 2.
Simulated improved visual acuity post-TCAT treatment showing reduced aberrations and clearer ‘E’ on the iTrace Visual Function Analyzer
The bed is washed after ablation and riboflavin (0.1% solution: 10 mg riboflavin in 10 ml dextran-T-500 20% solution) is applied every 2 minutes for the first 20 minutes. Ultraviolet A (UVA) (365 nm), 30 mW/cm2 surface irradiation is then performed for the next 4 minutes. A thorough irrigation with balanced salt solution is done, following which a bandage contact lens (BCL) is applied for 3 days or until complete healing of the epithelium. The patient was put on a tapering dose of prednisolone acetate 1% eye drops, topical antibiotic, and a lubricating eye drop.
Patients are followed up on day 1, day 7, and then at 1, 3, and 6 months. UCVA, BCVA, corneal biomechanics using CorvisST (Oculus Inc) and corneal topography on Pentacam and Topolyzer are evaluated at each visit.
Concept of T-PRK (Our Protocol)
Corneal asphericity (Q) depends on the location of the cone in keratoconus. Topographic neutralization will induce a change in the Q value and refractive error. While planning a T-CAT, we can choose to manipulate the Q or the refractive correction to achieve the desired post-operative corneal asphericity.
A cornea with a central cone (in which > 50% of the cone is within the 3-mm zone on pentacam posterior elevation map) will have a high negative Q value and a high myopic refractive error. In such eyes, if no refractive correction is performed, then the ablation for topography-guided ablation will induce a small change in refraction and Q but will not achieve the desired outcome.
In this case, we have an option of reducing the Q to a less negative value or applying a partial refractive correction, both of which will achieve a more neutral cornea. The decision to plan a partial refractive treatment is based on the spherical equivalent and the pachymetry. Corneas with spherical equivalent <6D and with thinnest pachymetry of >475 μm can be planned for partial refractive treatment, but in corneas with thinnest pachymetry between 450 and 475 μms and higher spherical equivalent, refractive treatment is not done in order to avoid excessive tissue ablation. The refractive correction results in some reduction of myopia and a reduction of Q induced by the ablation.
If refraction is not touched, the Q value alone can be reduced by 20-30% pre-operatively to preserve the asphericity of the cornea post-operatively.
Similarly, a cornea with a decentered cone (in which > 50% of the cone is outside the central 3 mm on the pentacam posterior elevation map) has a less negative Q or even a positive Q value and lower corneal myopia. In these cases, the topography-guided ablation will attempt to regularize the cornea and in effect cause a more negative Q post-operatively and a myopic shift of the refraction. We need to anticipate this change and adjust the Q and refractive correction pre-operatively to compensate for the post-operative change. If no refractive correction is performed, Q can be changed to zero pre-operatively, to prevent too much overshoot of Q post-operatively. If refractive correction is performed, then Q can be left unchanged. Refractive correction was performed for up to 50% of patient's refractive error, simultaneously manipulating to keep the maximum ablation on thinnest point <40 μms.
Based on this concept, we would like to present two case examples:
Case examples
Case 1
A 22-year-old male patient presented to us with keratoconus both eyes, intolerant to contact lens. His right eye UCVA was 6/18 and BCVA was 6/9 with a spectacle correction of −1.0 DS/−3.5DC@70°. His pre-operative pentacam map is shown in Fig. 3 which shows an early keratoconus with a partially inferiorly decentred cone. The pre-operative Q measured by Topolyser was −0.67 which also suggests a mild decentration of the cone and it was retained unchanged.
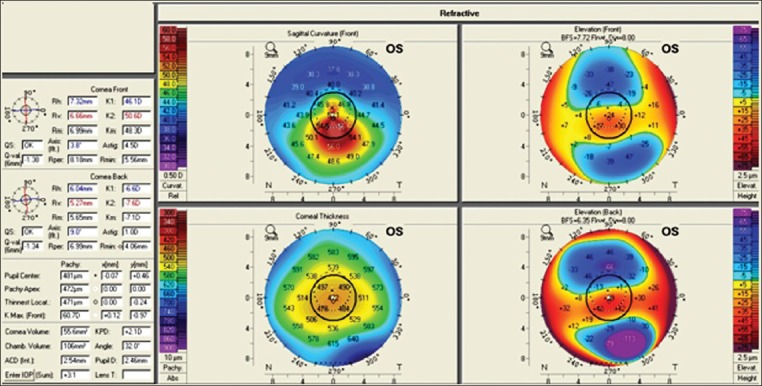
Figure 3.
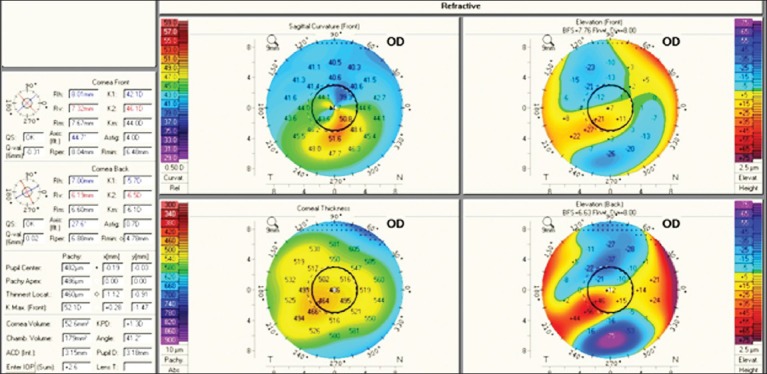
Case 1 pre-operative pentacam 4 map showing a slightly decentred cone in keratoconus
He underwent T-CAT with CXL for his right eye. T-CAT was performed with a refractive correction-1.25DS/-2DC@70° after Zernike optimization, maintaining the maximum central ablation to be less than 40 microns.
Post-operatively his UCVA was 6/12, BCVA was 6/6 with a spectacle correction of +1.00DS/−1.50DC@20°. His pentacam post-operatively [Fig. 4] revealed regularization of the cornea with flattening of the K-values at various points on the sagittal curvature map.
Figure 4.
Case 1 post-TCAT pentacam 4 map showing better centration of the cone with flattening in the sagittal curvature
Case 2
A 28 year-old male patient with keratoconus presented with UCVA of 6/60 and BCVA of 6/9 with a spectacle correction −5.5DC@30°. His pre-operative pentacam [Fig. 5] revealed grade 2 keratoconus. His pre-operative Q as measured by Topolyzer was −0.54 which suggests a more decentred cone. The Q value was retained unchanged during the planning for T-CAT. The refractive power treated was +0.75DS/−3DC@6° after Zernike optimization.
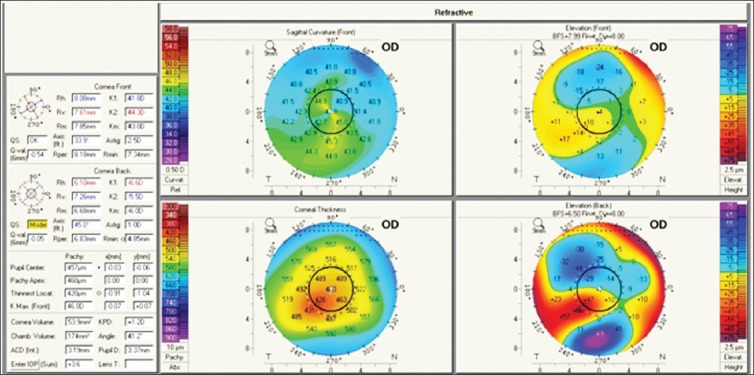
Figure 5.
Case 2 pre-operative pentacam showing a steep cornea in keratoconus
Post-operatively his UCVA improved to 6/24p and BCVA TO 6/6p with a spectacle correction of −1DS/−2.25DC@30°. His pentacam revealed good centration of the cone post-operatively, with relative flattening of the cornea [Fig. 6].
Figure 6.
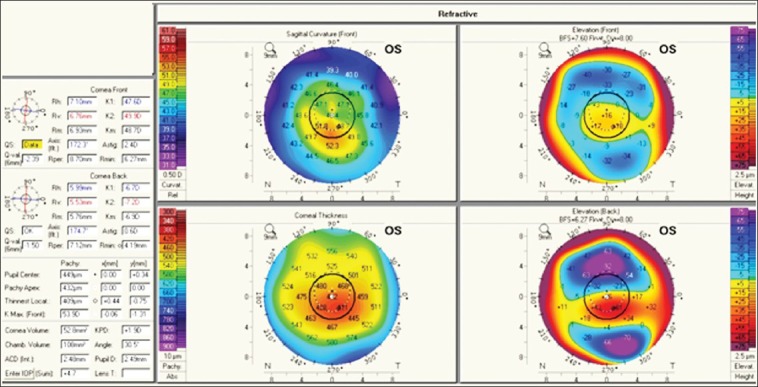
Case 2 post-TCAT pentacam showing flattening of the cone with better centration of the cone
Discussion
The treatment of progressive keratoconus involves multiple approaches, taking into account several factors, the primary ones being corneal biomechanical stability and irregular astigmatism leading to visual deterioration.[19] Simultaneous TPRK with CXL offers the unique advantage of tackling both parameters at one sitting.[20]
TPRK flattens some of the cone apex (in a fashion similar to an eccentric partial myopic PRK but simultaneously flattens an arcuate, broader area of the cornea away from the cone, usually in the superior nasal periphery; this ablation pattern resembles part of a hyperopic treatment and thus will cause some amount of steepening or elevation adjacent to the cone, effectively normalizing the cornea. This treatment offers an effective tissue sparing ablation pattern in highly irregular corneas such as ectasia in keratoconus.
Kymionis et al., recently reported a series of 31 keratoconus eyes treated with simultaneous T-CAT and C3R.[20] Their study showed a decrease in mean SE of only 1.22D (95% C.I., 2.5-0.1). In terms of visual acuity, there was a loss of 1 Snellen's line in 10% of the patients while 48% showed a gain of 1 line or more.[20] In another study comparing sequential and same-day TPRK and C3R for treatment of keratoconus, Kanellopoulos noted a SE reduction of 3.20 ± 1.4 D in the simultaneous group.[21] Kanellopoulos aimed to achieve a maximum ablation of 50 μ while we had aimed to achieve about 40 μ of ablation.
The decrease in the steep keratometry (K) readings on topography has been variable across studies; 2.35 D (95% C.I., 0.2-4.75) (Kymionis et al., 2011), 3.07 D (95% C.I., 0.99-5.21) (Kymionis et al., 2009), and 3.50 ± 1.3 D (Kanellopoulos).[19,20,21] Krueger et al., described two case reports of simultaneous TPRK and C3R in which the steep K reading reduced by 3.3 D at the end of 36 months in one eye in the first case but increased by 0.9 D in the fellow eye at the end of 3 years.[22] The second case showed a decrease of 4.1 D in one eye at the end of 3 years while the fellow eye demonstrated no change in the steep K reading at 30 months. The same authors also reported an improvement in UCVA at 3 months, which remained stable up to 30 months post-operatively in their second case report.[22]
The combination of T-CAT and CXL has been described in the recent past as a two-step procedure with CXL being done first, followed by PRK after a 1 year interval,[18] as well as a simultaneous procedure.[19,20,21,22] The simultaneous method has a number of advantages over the sequential technique, such as less post-operative haze,[21,23,24] more predictable refractive results and visual outcome due to ablation of normal non-crosslinked tissue, and less post-surgical recovery period.[22]
Conclusions
Various studies have evaluated the efficacy of T-CAT with CXL in keratoconus[19,20,21,22] and the procedure appears to be alternative efficient modality of treatment. Future studies can be aimed at evaluating the biomechanical and topographical stability of the procedure. This is necessary to determine the safety of this treatment and standardize its efficacy in keratoconus management.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Lindstrom RL. The surgical correction of astigmatism: A clinician's perspective. Refract Corneal Surg. 1990;6:441–54. [PubMed] [Google Scholar]
- 2.Alió JL, Belda JI, Shalaby AM. Correction of irregular astigmatism with excimer laser assisted by sodium hyaluronate. Ophthalmology. 2001;108:1246–60. doi: 10.1016/s0161-6420(01)00602-9. [DOI] [PubMed] [Google Scholar]
- 3.Kanjani N, Jacob S, Agarwal A, Agarwal A, Agarwal S, Agarwal T, et al. Wavefront- and topography-guided ablation in myopic eyes using Zyoptix. J Cataract Refract Surg. 2004;30:398–402. doi: 10.1016/j.jcrs.2003.07.004. [DOI] [PubMed] [Google Scholar]
- 4.Gimbel HV, Sofinski SJ, Mahler OS, van Westenbrugge JA, Ferensowicz MI, Triebwasser RW. Wavefront-guided multipoint (segmental) custom ablation enhancement using the Nidek NAVEX platform. J Refract Surg. 2003;19:S209–16. doi: 10.3928/1081-597X-20030302-07. [DOI] [PubMed] [Google Scholar]
- 5.Mrochen M, Krueger RR, Bueeler M, Seiler T. Aberration-sensing and wavefront-guided laser in situ keratomileusis: Management of decentered ablation. J Refract Surg. 2002;18:418–29. doi: 10.3928/1081-597X-20020701-01. [DOI] [PubMed] [Google Scholar]
- 6.Carones F, Vigo L, Scandola E. Wavefront-guided treatment of abnormal eyes using the LADARVision platform. J Refract Surg. 2003;19:S703–8. doi: 10.3928/1081-597X-20031101-17. [DOI] [PubMed] [Google Scholar]
- 7.Salz JJ. Wavefront-guided treatment for previous laser in situ keratomileusis and photorefractive keratectomy: Case reports. J Refract Surg. 2003;19:S697–702. doi: 10.3928/1081-597X-20031101-16. [DOI] [PubMed] [Google Scholar]
- 8.Castanera J, Serra A, Rios C. Wavefront-guided ablation with Bausch and Lomb Zyoptix for retreatments after laser in situ keratomileusis for myopia. J Refract Surg. 2004;20:439–43. doi: 10.3928/1081-597X-20040901-05. [DOI] [PubMed] [Google Scholar]
- 9.Chalita MR, Xu M, Krueger RR. Alcon CustomCornea wavefront-guided retreatments after laser in situ keratomileusis. J Refract Surg. 2004;20:S624–30. [PubMed] [Google Scholar]
- 10.Knorz MC, Jendritza B. Topographically-guided laser in situ keratomileusis to treat corneal irregularities. Ophthalmology. 2000;107:1138–43. doi: 10.1016/s0161-6420(00)00094-4. [DOI] [PubMed] [Google Scholar]
- 11.Kymionis GD, Panagopoulou SI, Aslanides IM, Plainis S, Astyrakakis N, Pallikaris IG. Topographically supported customized ablation for the management of decentered laser in situ keratomileusis. Am J Ophthalmol. 2004;137:806–11. doi: 10.1016/j.ajo.2003.11.077. [DOI] [PubMed] [Google Scholar]
- 12.Alió JL, Belda JI, Osman AA, Shalaby AM. Topography-guided laser in situ keratomileusis (TOPOLINK) to correct irregular astigmatism after previous refractive surgery. J Refract Surg. 2003;19:516–27. doi: 10.3928/1081-597X-20030901-06. [DOI] [PubMed] [Google Scholar]
- 13.Alessio G, Boscia F, La Tegola MG, Sborgia C. Topography-driven excimer laser for the retreatment of decentralized myopic photorefractive keratectomy. Ophthalmology. 2001;108:1695–703. doi: 10.1016/s0161-6420(01)00706-0. [DOI] [PubMed] [Google Scholar]
- 14.Alessio G, Boscia F, La Tegola MG, Sborgia C. Corneal interactive programmed topographic ablation customized photorefractive keratectomy for correction of postkeratoplasty astigmatism. Ophthalmology. 2001;108:2029–37. doi: 10.1016/s0161-6420(01)00807-7. [DOI] [PubMed] [Google Scholar]
- 15.Lin DT, Holland SR, Rocha KM, Krueger RR. Method for optimizing topography-guided ablation of highly aberrated eyes with the ALLEGRETTO WAVE excimer laser. J Refract Surg. 2008;24:S439–45. doi: 10.3928/1081597X-20080401-22. [DOI] [PubMed] [Google Scholar]
- 16.Kanellopoulos AJ, Binder PS. Management of corneal ectasia after LASIK With combined, same-day, topography-guided partial transepithelial PRK and Collagen Cross-linking: The athens protocol. J Refract Surg. 2010;27:323–31. doi: 10.3928/1081597X-20101105-01. [DOI] [PubMed] [Google Scholar]
- 17.Kanellopoulos AJ. Post LASIK ectasia. Ophthalmology. 2007;114:1230. doi: 10.1016/j.ophtha.2007.03.041. [DOI] [PubMed] [Google Scholar]
- 18.Kanellopoulos AJ, Binder PS. Collagen cross-linking (CCL) with sequential topography-guided PRK: A temporizing alternative for keratoconus to penetrating keratoplasty. Cornea. 2007;26:891–5. doi: 10.1097/ICO.0b013e318074e424. [DOI] [PubMed] [Google Scholar]
- 19.Kymionis GD, Kontadakis GA, Kounis GA, Portaliou DM, Karavitaki AE, Magarakis M, et al. Simultaneous topography-guided PRK followed by corneal collagen cross-linking for keratoconus. J Refract Surg. 2009;25:S807–11. doi: 10.3928/1081597X-20090813-09. [DOI] [PubMed] [Google Scholar]
- 20.Kymionis GD, Portaliou DM, Kounis GA, Limnopoulou AN, Kontadakis GA, Grentzelos MA. Simultaneous topography-guided photorefractive keratectomy followed by corneal collagen cross-linking for keratoconus. Am J Ophthalmol. 2011;152:748–55. doi: 10.1016/j.ajo.2011.04.033. [DOI] [PubMed] [Google Scholar]
- 21.Kanellopoulos AJ. Comparison of sequential vs same-day simultaneous collagen cross-linking and topography-guided PRK for treatment of keratoconus. J Refract Surg. 2009;25:S812–8. doi: 10.3928/1081597X-20090813-10. [DOI] [PubMed] [Google Scholar]
- 22.Krueger RR, Kanellopoulos AJ. Stability of simultaneous topography-guided photorefractive keratectomy and riboflavin/UVA cross-linking for progressive keratoconus: Case Reports. J Refract Surg. 2010;26:S827–32. doi: 10.3928/1081597X-20100921-11. [DOI] [PubMed] [Google Scholar]
- 23.Wollensak G, Spoerl E, Reber F, Seiler T. Keratocyte cytotoxicity of riboflavin/UVA treatment in vitro. Eye (Lond) 2004;18:718–22. doi: 10.1038/sj.eye.6700751. [DOI] [PubMed] [Google Scholar]
- 24.Xu H, Liu S, Xia X, Huang P, Wang P, Wu X. Mitomycin C reduces haze formation in rabbits after excimer laser photorefractive keratectomy. J Refract Surg. 2001;17:342–9. doi: 10.3928/1081-597X-20010501-08. [DOI] [PubMed] [Google Scholar]


