Abstract
Keratoconus is a progressive non-inflammatory thinning of the cornea that induces myopia and irregular astigmatism and decreases the quality of vision due to monocular diplopia, halos, or ghost images. Keratoconus patients unfit for corneal procedures and intolerant to refractive correction by spectacles or contact lenses have been implanted toric posterior chamber phakic intraocular lenses (PC pIOLs) alone or combined with other surgical procedures to correct the refractive errors associated with keratoconus as an off label procedure with special informed consent from the patients. Several reports attest to the safety and efficacy of the procedure, though the associated corneal higher order aberrations would have an impact on the final visual quality.
Keywords: Implantable collamer lens, intra corneal ring implants, keratoconous, toric implantable collamer lens
Keratoconus (Greek: kerato: Cornea; konos: Cone) is a progressive noninflammatory thinning of the cornea that is usually bilateral and involves the central two-thirds of the cornea resulting in a cone-shaped protrusion of the cornea. It induces myopia and irregular astigmatism and may decrease the quality of vision[1,2] due to monocular diplopia, halos, or ghost images.
The Visian implantable collamer lens (Staar Surgical AG, Nidau, Switzerland), is a monoblock single-piece plate haptic lens made of collamer (an extremely hydrophilic and highly biocompatible flexible collagen copolymer with a refractive index of 1.452 that is permeable to oxygen and nutrients). It is designed to be implanted in the posterior chamber, behind the iris with an aqueous humor layer separating it from the lens and with the haptics resting on the ciliary sulcus. Keratoconus patients unfit for corneal procedures and intolerant to refractive correction by spectacles or contact lenses have been implanted toric posterior chamber phakic intraocular lenses alone[3] or combined with other surgical procedures[4,5,6] to correct the refractive errors associated with keratoconus.
The toric implantable collamer lens (TICL) is conventionally indicated for the correction of myopia in adults aged 21-40 years with myopia ranging from −3.0 to 23.0 diopters (D) and up to 6 D of astigmatism at the spectacle plane, with anterior chamber depth (ACD) ³ 2.8 mm and a stable refraction within 0.5 D for 1 year prior to implantation. The patients should have a best corrected distance visual acuity (CDVA) of at least 20/50 with no previous ocular surgery, normal intraocular pressure and open anterior chamber angles (Shaffer grade 3 and 4 or Scheie grade 0 and 1). The peripheral retina should be normal or treated with laser photocoagulation when necessary.
It is contraindicated in patients with ocular comorbidity that includes corneal degeneration or dystrophy, low endothelial count, lens opacity, pseudoexfoliation, pigment dispersion, glaucoma, intraocular inflammation, macular pathology, and neovascularization.
Correcting the refractive error in keratoconus using the TICL is an off label use of the lens. Particular care should be taken to ensure that the refractive error is stable or stabilized in these patients.[7] Stable keratoconus may be defined as stable refraction in the eye with no surgical intervention for 2 years. Eyes having riboflavin-ultraviolet-A collagen cross linking (CXL) may tend to have a fluctuation in refraction in the initial posttreatment period that stabilizes over time. Once the patient has attained stable refraction for 3 consecutive months after CXL, the keratoconus may be considered stable. Additionally, keratoconus cases should have a clear central cornea, keratometric values ≤52.00 D and a central or centralized cone [Fig. 1]. A decentered cone may be defined as the location of the highest point of elevation away from the central 3.0 mm and/or more than 50% of the cone outside the central 3.0 mm zone on topography, which may be centralized by the use of adjunct intracorneal ring segments (ICRS).[7,8]
Figure 1.
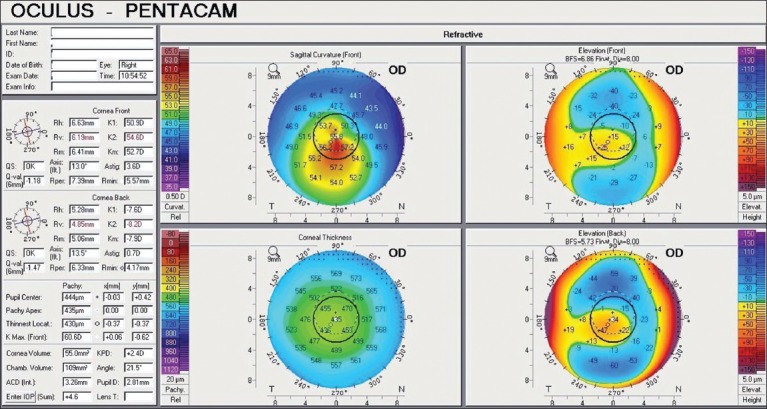
Pentacam quad maps showing inferiorly skewed regular bow tie pattern on sagital curvature map taken after implantation of intra stromal corneal rings before implantation of TICL
If these criteria are not met, penetrating keratoplasty or other management options may provide better visual outcomes. Table 1 summarizes the currently available peer reviewed literature.
Table 1.
Peer reviewed publications on the use of collamer posterior chamber intraocular lenses for refractive correction in keratoconus
My Personal Experience
Preoperative evaluation consists of a comprehensive ophthalmic evaluation including gonioscopy for peripheral iris configuration and a dilated fundus evaluation followed by measurement of manifest and cycloplegic refraction, corneal curvature (Pentacam and Orbscan), intraocular pressure, ACD (anterior segment ocular coherence tomography (AS-OCT)), white-to-white (Orbscan and Digital Calliper), pupil size, specular count of the corneal endothelium, and direct measurement of the horizontal sulcus diameter using the ultrasound biomicroscope (UBM).
The lens power, size based on the horizontal white-to-white distance and the axis placement for the TICL are calculated using software provided by the manufacturer. The postoperative target in all cases is as close to emmetropia as possible.
Each TICL comes with a diagram demonstrating the amount and direction of rotation from the horizontal axis required to align the cylinder axis of the TICL to the patient's required cylinder correction. To control for cyclotorsion with the patient supine, the reference marker is used preoperatively for the 0-180 degree horizontal axis with the patient sitting upright. Intraoperatively, an axis marker is used to measure the required rotation from horizontal during the surgical procedure.
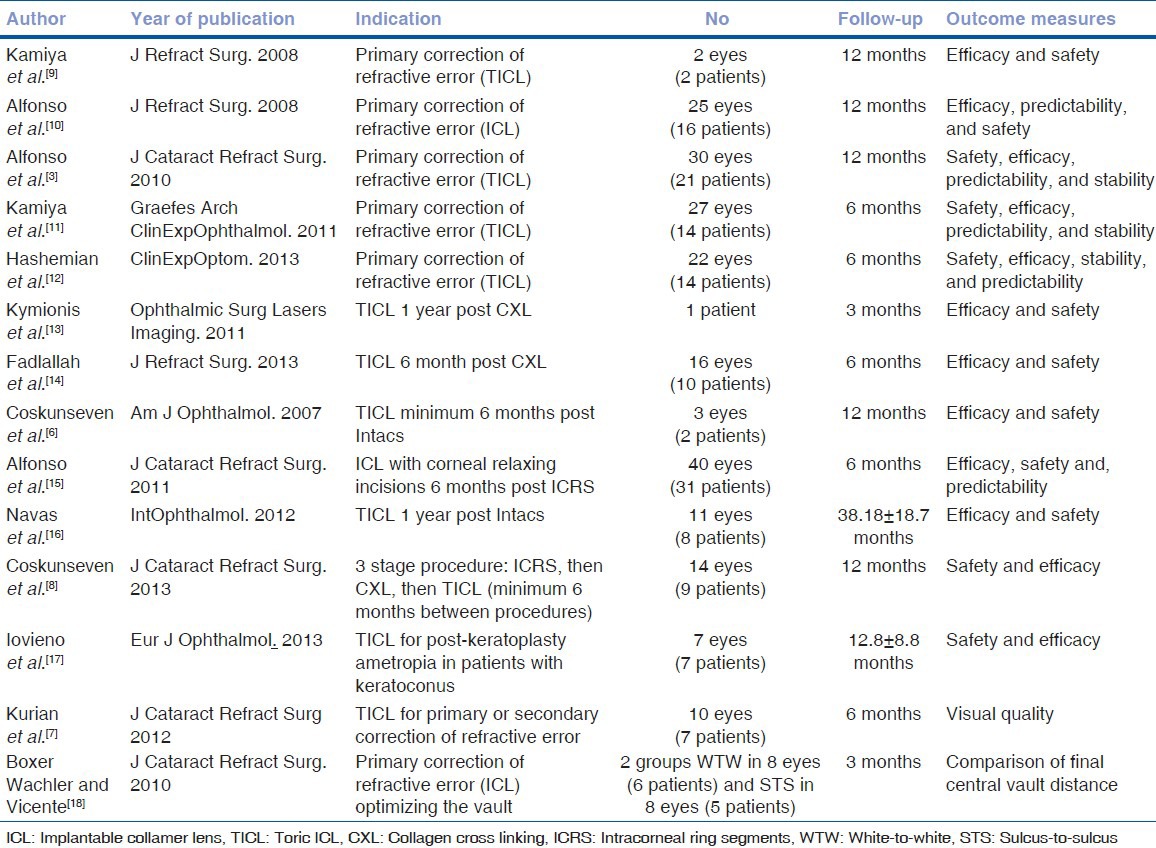
In all cases, the lens implantation is performed through a 3.0 mm temporal clear corneal tunnel incision under hydroxypropyl methylcellulose that is removed at the end of surgery. After the lens is injected into the anterior chamber, the haptics are tucked under the iris and the TICL is aligned to the desired axis [Fig. 2] using a Vukich manipulator (Rhein MedicalInc.). Preoperatively, two laser iridotomies are recommended. However, due to the thick brown irides in our patient population, a surgical iridectomy is performed using the vitrectomy cutter at high vacuum (250 mmHg) with a minimum cut rate (10 cuts per min) after the pupil is constricted with preservative-free intracameral pilocarpine 0.13 mg/mL.
Figure 2.
Intraoperative snapshot of the TICL haptic being tucked into the ciliary sulcus. The intrastromal corneal rings can be seen in situ in the cornea
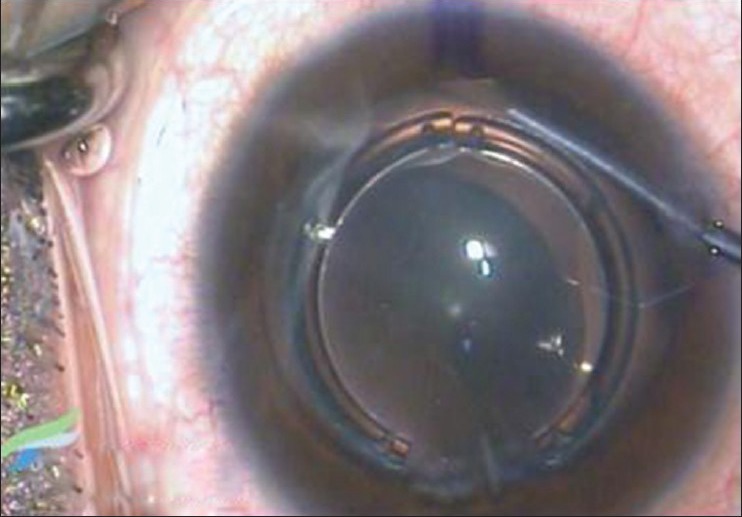
The postoperative topical regimen comprises moxifloxacin 0.3% eye drops four times a day for 2 weeks, prednisolone acetate eye drops 1.0% one drop every 6 h in a weekly tapering schedule, and nepafenac 0.1% eye drops twice daily over 6 weeks. Postoperative visits are on day 1, 1 and 6 weeks, 6 months, and annually thereafter. At each visit, symptoms are elicited and uncorrected distance visual acuity (UDVA), CDVA, slit-lamp, and dilated fundus examinations are performed. AS-OCT for vault measurement [Fig. 3], specular endothelial count, iTrace for axis alignment and neutralization of the corneal cylinder, tonometry, and visual quality evaluations are performed at each visit from the 6 week review.
Figure 3.

Fourier domain high resolution anterior segment ocular coherence tomography image showing the cross section of the intra stromal corneal rings within the cornea. The ICL can be seen with the vault measured at 0.488 mm
Ten eyes of seven patients with a mean age of 25.43 ± 3.95 years underwent lens implantation. One patient had stage 1, six patients had stage 2, and three patients had stage 3 keratoconus according to the Amsler-Krumeich classification. Of the seven eyes with central cones, four had stable keratoconus while the remaining three needed to be stabilized with CXL. The three patients with eccentric cones underwent ICRS implantation for cone centration and reduction of the irregular astigmatism and two of them required supplemental CXL to improve the biomechanical stability.
The preoperative mean refractive spherical equivalent (MRSE) of –7.21 ± 2.25 D decreased to −0.55 ± 1.53 D at 6 weeks and −0.44 ± 1.21 D at 6 months. The predictability of the procedure was 70% with seven of 10 eyes within 1.00 D and three eyes within 0.50 D of the intended MRSE 6 months after surgery. The efficacy of the procedure was 60% defined as the number and percentage of eyes (six of 10 eyes) achieving UDVA 6/12 (20/40). The efficacy index defined as the mean postoperative UDVA/mean preoperative CDVA was 0.72 at 6 months, indicating that at 6 months after implantation, patients could achieve 72% of the preoperative CDVA without correction. Nine eyes (90%) had a stable MRSE defined as the number and percentage of eyes with change in MRSE less than 1 D from the 6 weeks postoperative baseline to the 6 month postoperative visit. The safety index, defined as mean postoperative CDVA divided by mean preoperative CDVA was 1.13 at 6 months and the procedure was 100% safe as none of the eyes lost more than two lines of CDVA. There were no intraoperative or postoperative complications or adverse events. The modulation transfer function correlated inversely with secondary coma (P = 0.026), negative vertical coma (P = 0.014), and the root mean square (RMS) of total aberrations (P = 0.010), and higher order aberrations (HOAs; P = 0.015). The objective scatter index was directly correlated with secondary coma (P = 0.021), secondary trefoil (P = 0.016), the RMS of total aberrations (P = 0.032), and HOAs (P = 0.050).
Discussion
Multiple studies have documented the use of TICLs for the primary correction of the refractive error in stable keratoconus and demonstrated the safety and stability of to be on par with that for the correction of myopia or myopic astigmatism.[3,9,10,11,12] All studies document 100% safety because none of the patients lost more than two lines of best spectacle corrected visual acuity (BSCVA) on the Snellen chart after surgery. The safety index, defined as mean postoperative BSCVA divided by mean preoperative BSCVA, ranges from 1.12 to 1.4, indicating a net gain in visual acuity of 12-40%. Efficacy is defined as the number and percentage of eyes achieving UDVA 6/12 (20/40). The efficacy index defined as the mean postoperative uncorrected visual acuity/mean preoperative BSCVA ranged from 1.01 to 1.24 indicating that the studies reported a net gain in postoperative uncorrected vision compared to the preoperative BSCVA. These safety and efficacy results are comparable to that reported for the use of TICL in moderate to high myopic astigmatism[19] and are achieved despite the greater challenge of getting accurate refractions in keratoconic eyes.
Secondary use of TICLs have focused on the correction of the residual refractive error after progressive keratoconus was stabilized by CXL[13,14] or after management of the irregular astigmatism induced by an eccentric cone with or without adjunct CXL.[6,8,15,16] These results demonstrate the complementary goals of each treatment modality. Corneal ring implantation in keratoconic eyes reshapes the abnormal cornea, thus reducing the topographic abnormalities. Corneal CXL is performed 6-12 months later to stabilize the normalized corneal shape. Finally, after another delay to allow resolution of post-CXL corneal changes, correction of the residual spherocylindrical refractive error is performed with a toric pIOL. However, the visual quality metrics after correction of the refractive error by TICLs may be affected by the inherent corneal aberrations in keratoconus [Figs. 4 and 5].[7] One possible method of predicting the eyes with significant irregular corneal astigmatism and higher order aberrations that are likely to interfere with the postoperative visual quality is to evaluate the preoperative spectacle CDVA and compare it to the rigid gas permeable CDVA.[16] Eyes with significant difference between the two are likely to have poor postoperative visual quality metrics.
Figure 4.
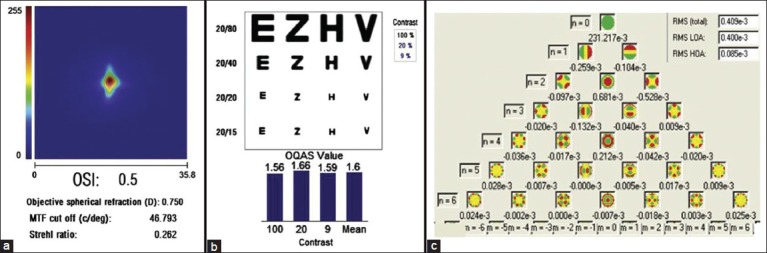
(a) Double-pass image of the PSF of a patient with a central cone on topography after pIOL implantation. (b) Good functional outcome illustrated by the good double-pass (OQAS) values and a good extrapolated contrast level. (c) Zernike analysis of the corneal wavefront aberrations with low RMS total and HOAs (c/deg = cycles per degree; HOA = higher-order aberration; LOA = lower-order aberration; MTF = modulation transfer function; OQAS = Optical Quality Analysis System; OSI = optical scatter index; RMS = root mean square)
Figure 5.
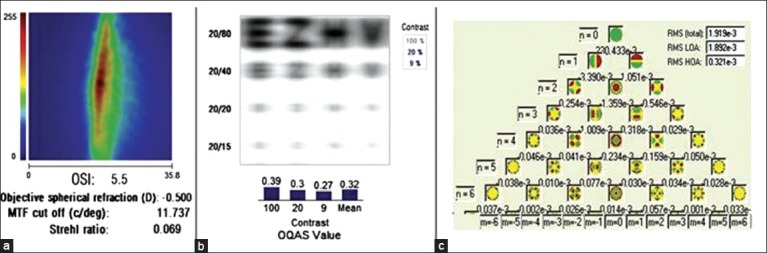
(a) Vertically spread double-pass image of the PSF of a patient with dysphotopsia post-toric pIOL despite UDVA of 6/9. (b) The doublepass (OQAS) values at different levels of contrast and visual acuity chart show poor optical quality. (C) Corresponding high values for corneal aberrations, specifically vertical coma (nZ3,mZ_1), seen in the pyramidal representation of the Zernike analysis (c/deg=cycles per degree;HOA=higher-order aberration; LOA=lower-order aberration; MTF=modulation transfer function; OQAS=Optical quality Analysis System; OSI = optical scatter index; RMS = root mean square).
The safety and efficacy of TICL for post-keratoplasty ametropia in patients with keratoconus has also found to be satisfactory.[17]
One comparative study has attempted to optimize the postoperative vault by using a sulcus-to-sulcus based sizing nomogram using UBM that was associated with higher vault predictability; however the difference between the two methods was not statistically significant.[18]
More prospective, randomized controlled trials with adequate sample sizes and long term follow-up are required to convert the proof of concept generated by these studies into appropriate practice guidelines.
Conclusion
The results of peer-reviewed, published articles outline the role of each treatment modality in addressing the different optical manifestations of keratoconus. ICRS reduce irregular corneal astigmatism and help to centralize eccentric cones. Corneal CXL is performed once the corneal shape normalizes to stabilize the biomechanically unstable cornea. Intraocular correction of the residual spherocylindrical refractive error with a toric pIOL gives good refractive outcomes though the visual quality is limited in those eyes with associated high corneal total and higher order aberrations.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Davis LJ, Schechtman KB, Wilson BS, Rosenstiel CE, Riley CH, Libassi DP, et al. Collaborative Longitudinal Evaluation of Keratoconus (CLEK) Study Group. Longitudinal changes in visual acuity in keratoconus. Invest Ophthalmol Vis Sci. 2006;47:489–500. doi: 10.1167/iovs.05-0381. [DOI] [PubMed] [Google Scholar]
- 2.Zadnik K, Barr JT, Edrington TB, Nichols JJ, Wilson BS, Siegmund K, et al. Corneal scarring and vision in keratoconus: A baseline report from the Collaborative Longitudinal Evaluation of Keratoconus (CLEK) Study. Cornea. 2000;19:804–12. doi: 10.1097/00003226-200011000-00009. [DOI] [PubMed] [Google Scholar]
- 3.Alfonso JF, Fernandez-Vega L, Lisa C, Fernandes P, Gonzalez-Meijome JM, Montes-Mico R. Collagen copolymer toric posterior chamber phakic intraocular lens in eyes with keratoconus. J Cataract Refract Surg. 2010;36:906–16. doi: 10.1016/j.jcrs.2009.11.032. [DOI] [PubMed] [Google Scholar]
- 4.Colin J, Velou S. Implantation of Intacs and a refractive intraocular lens to correct keratoconus. J Cataract Refract Surg. 2003;29:832–4. doi: 10.1016/s0886-3350(02)01618-8. [DOI] [PubMed] [Google Scholar]
- 5.Kamburoglu G, Ertan A, Bahadır M. Implantation of Artisan toricphakic intraocular lens following Intacs in a patient with keratoconus. J Cataract Refract Surg. 2007;33:528–30. doi: 10.1016/j.jcrs.2006.10.047. [DOI] [PubMed] [Google Scholar]
- 6.Coskunseven E, Onder M, Kymionis GD, Diakonis VF, Arslan E, Tsiklis N, et al. Combined Intacs and posterior chamber toric implantable Collamer lens implantation forkeratoconic patients with extreme myopia. Am J Ophthalmol. 2007;144:387–9. doi: 10.1016/j.ajo.2007.05.035. [DOI] [PubMed] [Google Scholar]
- 7.Kurian M, Nagappa S, Bhagali R, Shetty R, Shetty BK. Visual quality after posterior chamber phakic intraocular lens implantation in keratoconus. J Cataract Refract Surg. 2012;38:1050–7. doi: 10.1016/j.jcrs.2011.12.035. [DOI] [PubMed] [Google Scholar]
- 8.Coºkunseven E, Sharma DP, Jankov MR, 2nd, Kymionis GD, Richoz O, Hafezi F. Collagen copolymer toric phakic intraocular lens for residual myopic astigmatism after intrastromal corneal ring segment implantation and corneal collagen crosslinking in a 3-stage procedure for keratoconus. J Cataract Refract Surg. 2013;39:722–9. doi: 10.1016/j.jcrs.2012.11.027. [DOI] [PubMed] [Google Scholar]
- 9.Kamiya K, Shimizu K, Ando W, Asato Y, Fujisawa T. Phakic toric Implantable Collamer Lens implantation for the correction of high myopic astigmatism in eyes with keratoconus. J Refract Surg. 2008;24:840–2. doi: 10.3928/1081597X-20081001-12. [DOI] [PubMed] [Google Scholar]
- 10.Alfonso JF, Palacios A, Montés-Micó R. Myopic phakic STAAR collamer posterior chamber intraocular lenses for keratoconus. J Refract Surg. 2008;24:867–74. doi: 10.3928/1081597X-20081101-03. [DOI] [PubMed] [Google Scholar]
- 11.Kamiya K, Shimizu K, Kobashi H, Komatsu M, Nakamura A, Nakamura T, et al. Clinical outcomes of posterior chamber toric phakic intraocular lens implantation for the correction of high myopic astigmatism in eyes with keratoconus: 6–month follow-up. Graefes Arch Clin Exp Ophthalmol. 2011;249:1073–80. doi: 10.1007/s00417-010-1540-5. [DOI] [PubMed] [Google Scholar]
- 12.Hashemian SJ, Soleimani M, Foroutan A, Joshaghani M, Ghaempanah J, Jafari ME. Toric implantable collamer lens for high myopic astigmatism in keratoconic patients after six months. Clin Exp Optom. 2013;96:225–32. doi: 10.1111/j.1444-0938.2012.00800.x. [DOI] [PubMed] [Google Scholar]
- 13.Kymionis GD, Grentzelos MA, Karavitaki AE, Zotta P, Yoo SH, Pallikaris IG. Combined corneal collagen cross-linking and posterior chamber toric implantable collamer lens implantation for keratoconus. Ophthalmic Surg Lasers Imaging. 2011;42:e22–5. doi: 10.3928/15428877-20110210-05. [DOI] [PubMed] [Google Scholar]
- 14.Fadlallah A, Dirani A, El Rami H, Cherfane G, Jarade E. Safety and visual outcome of Visian toric ICL implantation after corneal collagen cross-linking in keratoconus. J Refract Surg. 2013;29:84–9. doi: 10.3928/1081597X-20130117-01. [DOI] [PubMed] [Google Scholar]
- 15.Alfonso JF, Lisa C, Fernández-Vega L, Madrid-Costa D, Poo-López A, Montés-Micó R. Intrastromal corneal ring segments and posterior chamber phakic intraocular lens implantation for keratoconus correction. J Cataract Refract Surg. 2011;37:706–13. doi: 10.1016/j.jcrs.2010.10.060. [DOI] [PubMed] [Google Scholar]
- 16.Navas A, Tapia-Herrera G, Jaimes M, Graue-Hernández EO, Gomez-Bastar A, Ramirez-Luquín T, et al. Implantable collamer lenses after intracorneal ring segments for keratoconus. Int Ophthalmol. 2012;32:423–9. doi: 10.1007/s10792-012-9582-9. [DOI] [PubMed] [Google Scholar]
- 17.Iovieno A, Guglielmetti S, Capuano V, Allan BD, Maurino V. Correction of postkeratoplasty ametropia in keratoconus patients using a toric implantable Collamer lens. Eur J Ophthalmol. 2013;23:361–7. doi: 10.5301/ejo.5000232. [DOI] [PubMed] [Google Scholar]
- 18.Boxer Wachler BS, Vicente LL. Optimizing the vault of collagen copolymer phakic intraocular lenses in eyes with keratoconus and myopia: Comparison of 2 methods. J Cataract Refract Surg. 2010;36:1741–4. doi: 10.1016/j.jcrs.2010.04.032. [DOI] [PubMed] [Google Scholar]
- 19.Kamiya K, Shimizu K, Kobashi H, Igarashi A, Komatsu M. Three-year follow-up of posterior chamber toric phakic intraocular lens implantation for moderate to high myopic astigmatism. PLoS One. 2013;8:e56453. doi: 10.1371/journal.pone.0056453. [DOI] [PMC free article] [PubMed] [Google Scholar]


