Abstract
Background:
Persistent pulmonary hypertension of the newborn (PPHN) result from the failure of the normal fetal-to-neonatal circulatory transition is associated with substantial infant mortality and morbidity.
Objective:
To estimate the possible risk factors and assess the outcome of these cases.
Materials and Methods:
Prospective study was performed enrolling all full-term and post-term newborn admitted to the NICU from January 2009 to April 2012, All neonates were subjected to complete history and physical examination, laboratory data including a complete blood count, arterial blood gases, blood glucose, serum electrolytes, and blood culture to exclude sepsis. Cases with PPHN had a continuous pulse oximeter, blood pressure and electrocardiography monitoring. Chest X-ray and echocardiogarphy were carried out to verify shunt and exclude structural congenital heart disease.
Results:
Out of the studied 640 infants, 32 infants (5%) developed PPHN, Meconium aspiration, birth asphyxia, hyaline membrane diseases, neonatal septicemia, post-term birth being large for gestational age, cesarean section, maternal overweight, and diabetes mellitus were associated with an elevated risk for PPHN. All neonates treated with O2, 10 neonates with Mg sulphate, 16 with oral sildenafil and 12 with mechanical ventilation. After 6 months follow-up, 12 (37.54%) improved and followed-up without sequelae, 4 (12.5%) developed some neurodevelopmental impairment, 8 (25%) died, 3 (9.3%) developed chronic lungs diseases, 2 (6.2%) developed hearing defects and another 3 (9.3%) missed follow-up.
Conclusion:
PPHN was found in 5% of the studied population. Meconium aspiration, birth asphyxia, neonatal septicemia, post-term were associated with an elevated risk for PPHN. As this is a unit based study, a comprehensive countrywide survey on PPHN in Egypt is recommended to determine any regional differences in disease incidence.
Keywords: Mg sulphate, persistent pulmonary hypertension of the newborn, risk factors, sildenafil, mechanical ventilation
INTRODUCTION
Persistent pulmonary hypertension of the newborn (PPHN) is a serious neonatal illness, which in the past was associated with high mortality and morbidity. It results from failure of the neonate to make a postnatal transition from a high resistance fetal pulmonary circulatory state to a low resistance pulmonary circulation.[1] This increased pulmonary vascular resistance and decreased pulmonary blood flow prevents adequate gas exchange in the lungs resulting in severe respiratory distress and hypoxemia in the neonate.[2] Data suggested that PPHN occurs in 1-2 infants/1000 live births.[3] The affected newborn usually term or late-preterm infant was not associated congenital anomalies and develop within hours after birth with severe respiratory distress that requires the mechanical ventilation.[4,5] The mortality rate about 10-20% of affected infants despite of treatments such as nitric oxide, extracorporeal membrane oxygenation (ECMO) and advanced modes of mechanical ventilation.[6] In addition, infants who survive PPHN at increased risks for long-term sequelae including chronic lung disease, seizures, and neurological developmental problems as a result of hypoxemia and/or the aggressive treatments that PPHN often requires.[7,8] The main goals of treatment of PPHN are to decrease pulmonary vascular resistance and increase pulmonary blood flow. This is carried out by correcting the underlying disease, good supportive care, and selective pulmonary vasodilators such as inhaled nitric oxide (iNO), Magnesium sulphate (MgSO4) and Oral sildenafil.[9]
The aim of this study was to estimate the incidence of PPHN at NICU of Al-Minya university pediatric hospital, to identify the risk factors and to assess the outcome of these cases.
MATERIALS AND METHODS
This data were prospectively collected from NICU of Al-Minya University Hospital (a tertiary referral hospital) in cooperation between the Departments of Neonatology and cardiology. A total of 640 neonates greater than 36 weeks of gestation and admitted to the NICU, from January 2009 to April 2012 were studied a written informed consent was obtained from the legal guardians of each patient the study was approved by the scientific ethical committee of Al-minya university hospital. Patients with a major congenital anomalies, congenital diaphragmatic hernia, congenital heart disease and pre-term were excluded.
Study protocol
All neonates in the study were subjected to complete history, and the physical examination was performed and blood drawn to obtain the baseline laboratory data including a complete blood count, arterial blood gases, blood glucose, serum electrolytes and blood culture to exclude sepsis. All patients had a continuous pulse oximeter, blood pressure and electrocardiography monitoring. Chest X-ray and echocardiogarphy were carried out to verify shunt and exclude structural congenital heart disease.
Medications and protocols for managements
A neonate with acidosis was given sodium bicarbonate slow bolus infusion: 2-3 mEq/kg IV for neonates with acidosis and guided by improvement of arterial blood gases. Drugs that decrease pulmonary vascular resistance and increase pulmonary blood flow were given for selected neonates 1st group (16 neonates) was given Oral Sildenafil citrate 1 mg/kg every 6 h and the dose could be doubled if the oxygenation did not improve and blood pressure remained stable and the treatment was discontinued if there was no significant change in oxygenation after 36 h, or patient has received eight doses. This strategy according to previous study[10] and 2nd group (10 neonates) was given MgSO4, a loading dose of 250 mg/kg of MgSO4 IV over 10-15 min. a clinical response is obtained once the serum magnesium level exceeds 3-5 mmol/L give between 20 and 75 mg/kg/h for 2-5 days while maintaining a blood level of between (3.5 and 5.5 mmol/L).[11] Mechanical ventilation was used in 12 neonates with extreme acidosis (pH<7.10) resistance to treatment, severe neonatal pneumonia, and massive lung collapse.[12] Other drugs; anti-infective, positive inotropic drugs (dopamine), sedatives and skeletal muscle relaxants according to the clinical condition of the infant.
Follow-up of these neonates for 6 months for evaluation of neurological injury by performing complete neurological examination by a pediatric neurologist and in some of them by doing cranial ultrasound, electroencephalography, brain computed tomography and or magnetic resonance imaging hearing test and fundus examination were also performed for neonates suspected with complications.
RESULTS
The study population included 640 neonates during the duration from January 2009 to April 2012. Only 32 (5%) were diagnosed as PPHN. It was higher for those who were born by cesarean section, male, post-term, large for gestational age, meconium stained amniotic fluid, perinatal asphyxia, sepsis, hyaline membrane disease, pneumonia, and down-syndrome. Maternal diseases including, diabetes mellitus, hypertension, and anemia [Tables 1 and 2].
Table 1.
Demographic and clinical data of cases with PPHN
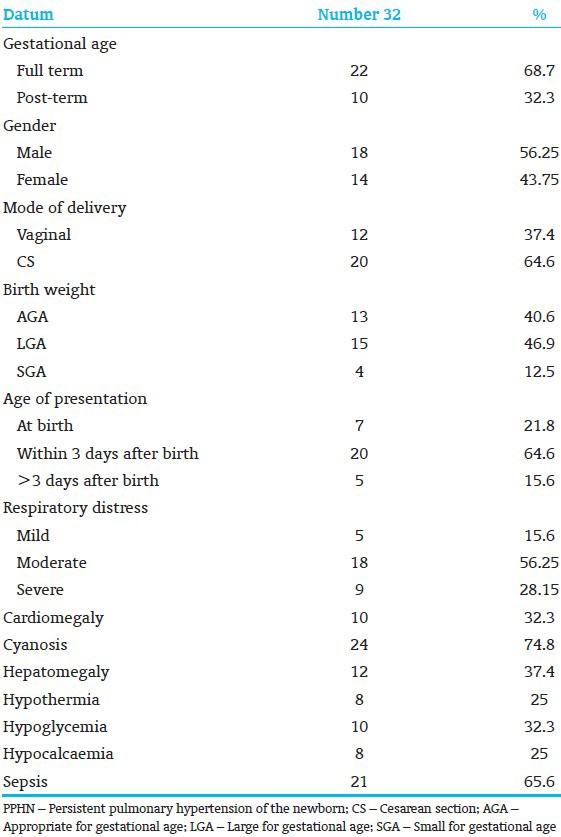
Table 2.
Risk factors and causes of PPHN
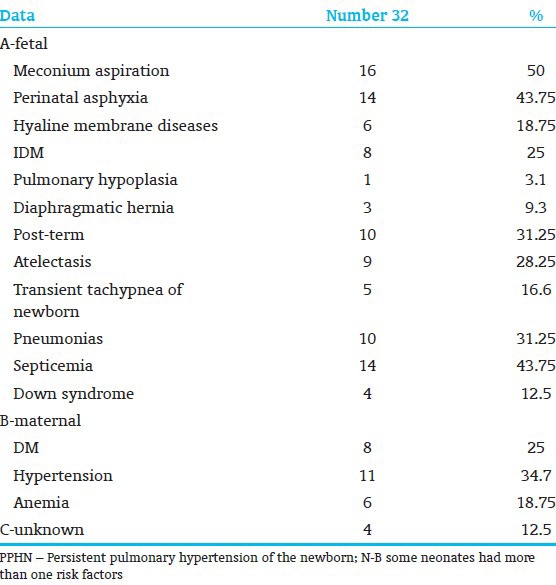
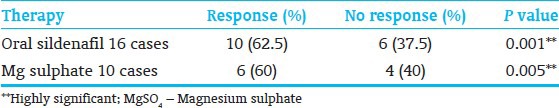
Table 3, showed the different therapeutic modalities, which were available in NICU units for management of PPHN included oxygen administration to all neonates for short duration (6-9 days). Oral sildenafil was administered to 16 neonates with PPHN and the outcome was satisfactory and there was a significant difference between responsive (10 cases) and unresponsive neonates (6 cases); (P = 0.001) [Table 4]. Infusion of magnesium sulfate was administered to 10 neonates with PPHN the outcome was satisfactory and there was a significant difference between responsive and unresponsive neonates. We did not give any neonate the two agents simultaneously. 12 (37.5%) neonates with extreme acidosis (pH<7.10) resistance to treatment, severe neonatal pneumonia, and massive lung collapse were treated by mechanical ventilation. 8 neonates (25%) were died from respiratory failure.
Table 3.
Therapy used for treatment of newborns with PPHN
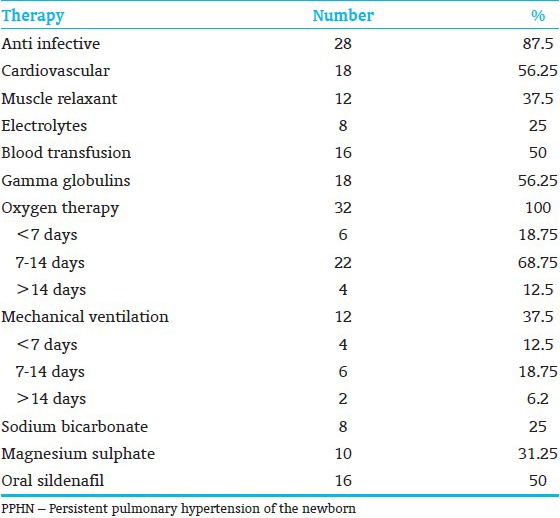
Table 4.
Comparison of improvement of cases received oral sildenafil and MgSO4
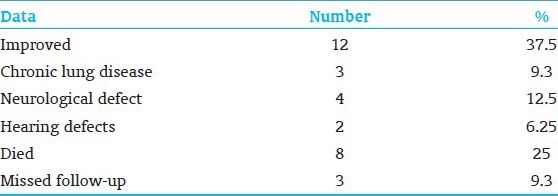
The outcome of the neonates with PPHN was mentioned in [Table 5], it showed that after 6 months of closed follow-up, 12 neonates (37.54%) improved without sequelae, 4 neonates (12.5%) developed some neurodevelopmental impairment, 3 neonates (9.3%) developed chronic lungs diseases, 2 neonates (6.2%) developed hearing (deficits) and another 3 neonates (9.3%) missed follow-up.
Table 5.
Outcome of the newborn after 6 months follow-up
DISCUSSION
Persistence of pulmonary hypertension leading to respiratory failure in the neonate has been recognized for 40 years since its original description by Gersony et al. in 1969.[13] The mortality rate of infants with PPHN was estimated to be around 10-20% even with the use of high-frequency ventilation, surfactant, iNO, and ECMO but is much higher when these therapies are not available.[14]
A total of 32 neonates (18 male and 14 females) were diagnosed as having persistent neonatal pulmonary hypertension prospectively evaluated.
PPHN represented nearly 5% (32/640 cases) of total neonatal care units’ admissions and it was considered the sixth leading cause of death in our NICU units in year 2010. The diagnosis of our cases depends on high clinical suspicion, echocardiography, and pulse oximetry and blood gas analysis. The most common cause of PPHN in this study was mainly meconium aspiration syndrome, representing 50% of PPHN in this series.[15] Meconium cause mechanical obstruction to the airways, resulting in air trapping, hyperinflation, and increased risk for pneumothorax. Meconium components also inactivate surfactant,[16] trigger an inflammatory response with the release of cytokines, and increase the production of the vasoconstrictors endothelin and thromboxane.[17]
The second cause of PPHN in this study was congenital pneumonia and sepsis. PPHN can be a complication of pneumonia or sepsis secondary to common neonatal pathogens.[18] Bacterial endotoxin causes pulmonary hypertension from several mechanisms, including the release of thromboxane, endothelin, and several cytokines.[19] In this study, PPHN occurred as a complication of hyaline membrane disease and transient tachypnea of the newborn in five cases (16.6%) delivered by C-section. The increasing reactivity of pulmonary arteries at this gestation period predisposes these neonates to pulmonary hypertension when gas exchange is impaired because of surfactant deficiency.[20] Four cases (12.5%) of PPHN of unknown etiology in this series were transient forms with a good outcome, suggesting transient maladaptation to extrauterine life. Down-syndrome21] was diagnosed in 12.5% of cases.
The majority of neonates were delivered by cesarean section (62.5% of cases) due to prenatal problems in agreement with Previous studies had reported cesarean section delivery was associated with a high incidence of respiratory distress syndrome and PPHN.[22] Maternal diseases such as uncontrolled diabetes mellitus, hypertension, and anemia represented maternal risk factors in our neonates. Uncontrolled diabetes Mellitus associated is with high incidence of hyaline membrane disease, hypoglycemia, marcosmia, and fetal distress. This was in agreement with many previous studies that maternal diseases play a role in occurrence of PPHN especially DM, hypertension and maternal anemia.[23]
iNO has been one of the latest measures to successfully treat PPHN and significantly reduce the need for ECMO,[24] but both were not available in our NICU. Hence we used other modalities as pulmonary vasodilator drugs, which are available like oral Sildenafil and MgSO4 infusion.
MgSO4 was tried in 10 cases (31.25%), 6 (60%) of cases showed improvement of PO2, decrease in total oxygen depending time, and infants survive without sequelae. Two expired as a sequalae of severe birth asphyxia and neonatal septicemia. We discontinued infusion in 2 cases due to hypotension and unresponsiveness to therapy, and shifted to mechanical ventilation. Previous studies by Abu-osba et al.[25] and Tolsa et al.[26] showed that intravenous MgSO4 has been used extensively in developing countries for the treatment of PPHN. It is cheap and easily available and has a potential neuroprotective effect; its main disadvantage is that it can cause systemic hypotension.
Oral sildenatil was used in 16 cases (50%) who were randomly selected, all of them were full-term with moderate respiratory distress syndrome, 10 of them (62.5%) neonates showed improvement and 6 (37.5%) cases discontinued medication due to unresponsiveness and shifted to another line of available therapeutic modalities. Baquero et al.[10] stated that oral sildenafil was administered easily and was tolerated as well as placebo and improved oxygenation index in infants with severe PPHN, which suggests that oral sildenafil, may be effective in the treatment of PPHN and underscores the need for a large, controlled trial. Khorana et al.[27] in a retrospective study concluded that results confirm that sildenafil may be a useful adjuvant therapy for term infants with pulmonary hypertension in centers lacking iNO and ECMO, Mechanical ventilation was performed in 12 (37.5%) neonates with PPHT, extreme acidosis (pH<7.1) severe neonatal pneumonia, massive lung collapse, and whom unresponsiveness to other therapeutic modalities was recorded. 8 cases (66, 7%) improved and gradually weaned from ventilation. Three of our cases were subjected to high-frequency oscillatory ventilation mode due to severe condition from the start and one of them after failure of other alternative therapy. All showed air leak as a complication and expired.
After meticulous follow-up (6 months) of these neonates, the outcome was: 12 cases (37.5%) improved and showed normal development and were followed-up in pediatric neurology, ophthalmology, otolaryngology clinics without sequelae 8 cases (25%) died (four of them from severe sequelae of birth asphyxia and myocardial failure, three from severe neonatal septicemia, one from massive air leak syndrome). Four cases (12.5%) developed some neurodevelopmental impairment. three cases (9.3%) developed chronic lung disease, two (6.2%) develop hearing defects and another 3 (9.3%) missed follow-up.
The mortality and morbidity rates in our neonate were high and may be attributed to late presentation, delayed diagnosis and unavailability of other highly effective therapeutic modalities such as iNO, ECMO and more recent vasodilators agents like tolazoline.
CONCLUSION
PPHN was diagnosed in 5% of the studied neonates in our NICU, Meconium aspiration, birth asphyxia, hyaline membrane diseases, neonatal septicemia, post-term, cesarean section, maternal hypertension, and diabetes mellitus were the most encountered risk factors for PPHN. MgSO4 and oral sildenafil were effective in treatment of PPHN. This study is limited by the fact of being a single center analysis, Prospective studies with the objective of evaluating the different therapies including a significant number of patients, will give much more information regarding therapeutic efficacy and survival.
ACKNOWLEDGMENTS
We are appreciated to all members of Pediatric and Cardiology Department and also the patients for their patience and compliance.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Thérèse P. Persistent pulmonary hypertension of the newborn. Paediatr Respir Rev. 2006;7:S175–6. doi: 10.1016/j.prrv.2006.04.211. [DOI] [PubMed] [Google Scholar]
- 2.Ostrea EM, Villanueva-Uy ET, Natarajan G, Uy HG. Persistent pulmonary hypertension of the newborn: Pathogenesis, etiology, and management. Paediatr Drugs. 2006;8:179–88. doi: 10.2165/00148581-200608030-00004. [DOI] [PubMed] [Google Scholar]
- 3.Abman SH. Recent advances in the pathogenesis and treatment of persistent pulmonary hypertension of the newborn. Neonatology. 2007;91:283–90. doi: 10.1159/000101343. [DOI] [PubMed] [Google Scholar]
- 4.Suesaowalak M, Cleary JP, Chang AC. Advances in diagnosis and treatment of pulmonary arterial hypertension in neonates and children with congenital heart disease. World J Pediatr. 2010;6:13–31. doi: 10.1007/s12519-010-0002-9. [DOI] [PubMed] [Google Scholar]
- 5.Walsh-Sukys MC, Tyson JE, Wright LL, Bauer CR, Korones SB, Stevenson DK, et al. Persistent pulmonary hypertension of the newborn in the era before nitric oxide: Practice variation and outcomes. Pediatrics. 2000;105:14–20. doi: 10.1542/peds.105.1.14. [DOI] [PubMed] [Google Scholar]
- 6.Greenough A, Khetriwal B. Pulmonary hypertension in the newborn. Paediatr Respir Rev. 2005;6:111–6. doi: 10.1016/j.prrv.2005.03.005. [DOI] [PubMed] [Google Scholar]
- 7.Abman SH. Neonatal pulmonary hypertension: A physiologic approach to treatment. Pediatr Pulmonol Suppl. 2004;26:127–8. doi: 10.1002/ppul.70080. [DOI] [PubMed] [Google Scholar]
- 8.Latini G, Del Vecchio A, De Felice C, Verrotti A, Bossone E. Persistent pulmonary hypertension of the newborn: Therapeutical approach. Mini Rev Med Chem. 2008;8:1507–13. doi: 10.2174/138955708786786507. [DOI] [PubMed] [Google Scholar]
- 9.Vargas-Origel A, Gómez-Rodríguez G, Aldana-Valenzuela C, Vela-Huerta MM, Alarcón-Santos SB, Amador-Licona N. The use of sildenafil in persistent pulmonary hypertension of the newborn. Am J Perinatol. 2010;27:225–30. doi: 10.1055/s-0029-1239496. [DOI] [PubMed] [Google Scholar]
- 10.Baquero H, Soliz A, Neira F, Venegas ME, Sola A. Oral sildenafil in infants with persistent pulmonary hypertension of the newborn: A pilot randomized blinded study. Pediatrics. 2006;117:1077–83. doi: 10.1542/peds.2005-0523. [DOI] [PubMed] [Google Scholar]
- 11.Grimes DA, Nanda K. Magnesium sulfate tocolysis: Time to quit. Obstet Gynecol. 2006;108:986–9. doi: 10.1097/01.AOG.0000236445.18265.93. [DOI] [PubMed] [Google Scholar]
- 12.Clark RH. High-frequency ventilation. J Pediatr. 1994;124:661–70. doi: 10.1016/s0022-3476(05)81352-6. [DOI] [PubMed] [Google Scholar]
- 13.Gersony WM, Duc GV, Sinclair JC. PFC syndrome. Circulation. 1969;40(suppl):3–87. [Google Scholar]
- 14.Rocha G, Baptista MJ, Guimarães H. Persistent pulmonary hypertension of non cardiac cause in a neonatal intensive care unit. Pulm Med 2012. 2012 doi: 10.1155/2012/818971. 818971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yoder BA, Kirsch EA, Barth WH, Gordon MC. Changing obstetric practices associated with decreasing incidence of meconium aspiration syndrome. Obstet Gynecol. 2002;99:731–9. doi: 10.1016/s0029-7844(02)01942-7. [DOI] [PubMed] [Google Scholar]
- 16.Dargaville PA, South M, McDougall PN. Surfactant and surfactant inhibitors in meconium aspiration syndrome. J Pediatr. 2001;138:113–5. doi: 10.1067/mpd.2001.109602. [DOI] [PubMed] [Google Scholar]
- 17.Soukka H, Jalonen J, Kero P, Kääpä P. Endothelin-1, atrial natriuretic peptide and pathophysiology of pulmonary hypertension in porcine meconium aspiration. Acta Paediatr. 1998;87:424–8. doi: 10.1080/08035259850157039. [DOI] [PubMed] [Google Scholar]
- 18.Navarrete CT, Devia C, Lessa AC, Hehre D, Young K, Martinez O, et al. The role of endothelin converting enzyme inhibition during group B streptococcus-induced pulmonary hypertension in newborn piglets. Pediatr Res. 2003;54:387–92. doi: 10.1203/01.PDR.0000078272.77816.1E. [DOI] [PubMed] [Google Scholar]
- 19.Verma B, Daga SR, Mahapankar A. Persistent pulmonary hypertension among neonates with sepsis. Indian J Pediatr. 2006;73:250–1. doi: 10.1007/BF02825496. [DOI] [PubMed] [Google Scholar]
- 20.Konduri GG, Kim UO. Advances in the diagnosis and management of persistent pulmonary hypertension of the newborn. Pediatr Clin North Am. 2009;56:579–600. doi: 10.1016/j.pcl.2009.04.004. Table of Contents. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cua CL, Blankenship A, North AL, Hayes J, Nelin LD. Increased incidence of idiopathic persistent pulmonary hypertension in Down syndrome neonates. Pediatr Cardiol. 2007;28:250–4. doi: 10.1007/s00246-006-0011-6. [DOI] [PubMed] [Google Scholar]
- 22.de Araujo OR, Andrea de Cdssia Stefano, Vanessa Aparecida. Cesarean deliveries and other risks for persistent pulmonary hypertension of the newborn. Bras Ter lntensiva. 2008;20:394–7. [PubMed] [Google Scholar]
- 23.Hernández-Díaz S, Van Marter LJ, Werler MM, Louik C, Mitchell AA. Risk factors for persistent pulmonary hypertension of the newborn. Pediatrics. 2007;120:e272–82. doi: 10.1542/peds.2006-3037. [DOI] [PubMed] [Google Scholar]
- 24.Rao S, Bartle D, Patole S. Current and future therapeutic options for persistent pulmonary hypertension in the newborn. Expert Rev Cardiovasc Ther. 2010;8:845–62. doi: 10.1586/erc.09.186. [DOI] [PubMed] [Google Scholar]
- 25.Abu-Osba YK, Galal O, Manasra K, Rejjal A. Treatment of severe persistent pulmonary hypertension of the newborn with magnesium sulphate. Arch Dis Child. 1992;67:31–5. doi: 10.1136/adc.67.1_spec_no.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tolsa JF, Cotting J, Sekarski N, Payot M, Micheli JL, Calame A. Magnesium sulphate as an alternative and safe treatment for severe persistent pulmonary hypertension of the newborn. Arch Dis Child Fetal Neonatal Ed. 1995;72:F184–7. doi: 10.1136/fn.72.3.f184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Khorana M, Yookaseam T, Layangool T, Kanjanapattanakul W, Paradeevisut H. Outcome of oral sildenafil therapy on persistent pulmonary hypertension of the newborn at Queen Sirikit National Institute of Child Health. J Med Assoc Thai. 2011;94(Suppl 3):S64–73. [PubMed] [Google Scholar]