Abstract
A baby with the complete form of pentalogy of Cantrell was delivered at 33 weeks of gestation. The hallmark of this syndrome is ectopia cordis (EC) with omphalocele. Even though a fetal diagnosis was made at 14 weeks, parents have decided to continue with the pregnancy. Early antenatal ultrasonographic diagnosis is essential as survival depends mostly on the EC, associated cardiac anomalies and degree of thoraco-abdominal defect. Fetal diagnosis of this lethal anomaly before viability gives the parents an option of termination.
Keywords: Diaphragmatic defects, ectopia cordis, omphalocele, pentalogy of Cantrell, thoraco-abdominal wall defect
INTRODUCTION
Cantrell in 1958 first described the full spectrum of PC.[1] The PC is an extremely rare and usually lethal anomaly. The full spectrum consists of five anomalies: A deficiency of the anterior diaphragm, a midline supraumbilical abdominal wall defect, a defect in the diaphragmatic pericardium, various congenital intracardiac abnormalities, and a defect of the lower sternum.[1] Complete PC is rarely reported. We report a case of complete PC.
CASE REPORT
A baby boy weighing 2,390 gm was born to a 39-year-old primigravida mother at 33 weeks of gestation. The maternal antenatal care was transferred to a tertiary setting following the detection of multiple fetal anomalies at 14 weeks of gestation in a polyclinic. Her medical and obstetric histories were unremarkable. Parents were non-consanguineous. A detailed anomaly scan showed a live fetus with EC [Figure 1] and omphalocele. Fetal echocardiography revealed atrial and ventricular septal defects. The pericardium was not visualized.
Figure 1.
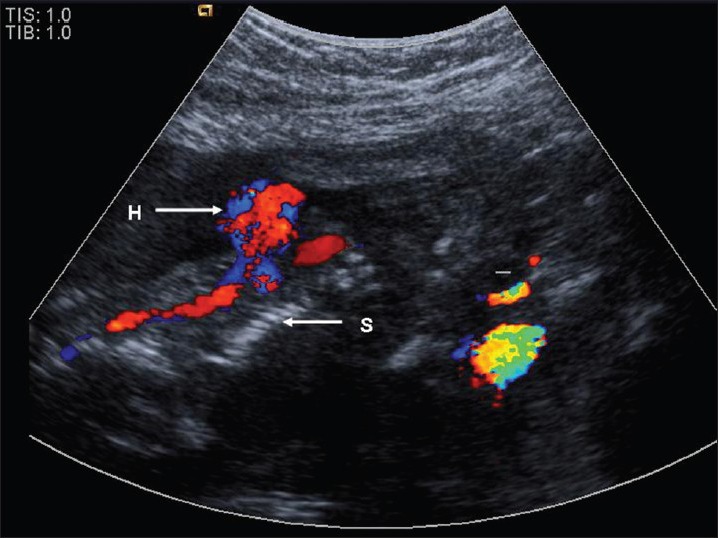
Fetal ultrasounds scan showing the ectopia cordis. H – heart; S – spine
Parents were counseled regarding the fetus possibly having a severe form of PC and an amniocentesis was offered. However, they denied amniocentesis and decided to continue with the pregnancy due to religious beliefs. At parental request the perinatal team agreed to deliver the baby at term with a standby multidisciplinary team for surgical intervention, if feasible after assessment.
While on follow-up, mother was admitted with preterm labor at 33 weeks of pregnancy. At parental request, cesarean section was done. A live male infant was born with poor Apgar scores requiring intubation at two minutes of life. On examination there was a large anterior thoraco-abdominal wall defect, ectopic contractile heart and an edematous liver with loops of small intestine and colon outside the abdominal cavity [Figure 2]. Spleen and splenunculi were seen. The face was dysmorphic with bilateral cleft lip. The thoraco-abdominal wall defect was extending from the umbilicus to the upper third of the body of the sternum. The cord was distorted at the umbilicus due to omphalocele. The liver was enlarged with a prominent caudate lobe and the gall bladder appeared normal. A large defect in the diaphragm extending from the sternum to the spine posteriorly was noted. Lungs could be visualized through the defect. Lower half of the body of the sternum and the xiphisternum were absent. The spine was showing severe scoliosis and the abdominal cavity was contracted. All the four limbs were normal. Both kidneys were small and were noted in the pelvis. The external genitalia showed a normal male phenotype. Birth weight, length and head circumference were in the 10-50th percentile.
Figure 2.
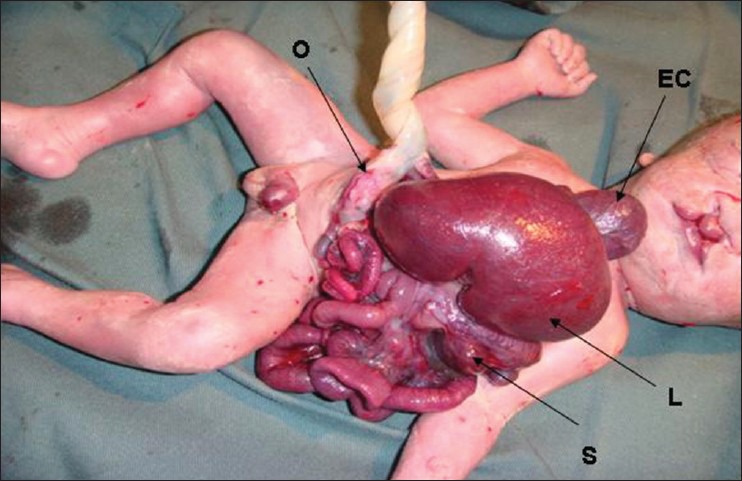
The baby at birth with the pentalogy of Cantrell. EC – ectopia cordis; L – liver; S – spleen; O – omphalocele
An echocardiogram confirmed the atrial and ventricular septal defects and patent ductus arteriosus. The pericardium was absent. Cranial ultrasonographic scan was unremarkable.
Parents were updated and they requested for comfort care. The ventilatory support was withdrawn and the baby died at three hours of life. The parents consented only for partial autopsy. The biopsy of the skin surrounding the anterior abdominal wall defect was done to rule out amniotic bands and was reported as normal. A biopsy was obtained from the base of the heart and confirmed the absence of the pericardium. Karyotyping showed a normal male infant.
DISCUSSION
Toyama suggested the following classification for the PC:[2] Class 1, definite diagnosis, with all five defects present; Class 2, probable diagnosis, with four defects present, including intracardiac and ventral wall abnormalities; and Class 3, incomplete expression, with various combinations of defects present, including a sternal abnormality. Our case fits into Class 1 or complete PC.
Incidence of the PC varies from 5.5 to 7.9 per million live births.[3] The constellation of defects observed in PC is thought to result from the abnormalities in the differentiation of the intraembryonic mesoderm at approximately 14 to 18 days after conception. The diaphragmatic and pericardial defects result from abnormal development of the septum transversum whereas the sternum and abdominal wall defects are probably related to impaired migration of mesodermal structures.[4]
The etiology of PC is unknown. Most cases are sporadic and no recurrences have been reported. There is male dominance with a male to female ratio of 2.7:1. This syndrome has also been reported occasionally in association with sirenomelia, anencephaly and amniotic band syndrome.[5] Familial occurrence of both isolated EC and pentalogy of Cantrell has been reported.[6]
An associated intracardiac anomaly is the rule, such as septal defects, Ebstein's anomaly, Fallot's tetralogy or single atrium. In 75% of the cases pericardium may be absent. Extracardiac abnormalities in PC include craniofacial anomalies such as cleft lip and/or palate; central nervous system anomalies such as hydrocephalus; skeletal malformations such as clubfoot, absence of tibia or radius and abdominal abnormalities such as polysplenia and gallbladder agenesis.[7,8] Sternal defects include bifid sternum (26%), absent xiphoid (10%) and absent lower 2/3 of sternum (9%). Anterior abdominal wall defect is mostly an omphalocele (63%). A ventral retrosternal defect of the diaphragm occurs in 91% of the cases.[8] Omphalocele, cardiac septal defects, absent pericardium, cleft lip and defects in the sternum and diaphragm were noted in the reported case as well.
With prenatal ultrasonography, PC can usually be diagnosed as early as 10 weeks of pregnancy. It has been suggested that magnetic resonance imaging and prenatal fetal echocardiography provide optimal assessment of fetuses with PC. Using 2D ultrasound in the first trimester, and the adjunctive use of the 3D ultrasound may help to enhance the visualization of the fetal anomalies in different orthogonal planes, even in unfavorable fetal positions.[9] If a diagnosis is made by ultrasound, fetal chromosomal analysis is recommended as associations with Trisomies and Turner syndrome have been reported.[4]
The treatment strategy and prognosis depends on the size of the abdominal wall defect, the type of EC, and the associated anomalies.[7] Following prenatal diagnosis, termination of pregnancy may be offered in severe cases, when amniocentesis shows an abnormal karyotype. A multidisciplinary team should follow-up milder forms in order to determine the best time for delivery. After delivery, repair of the omphalocele should not be delayed. Repair of the sternal, diaphragmatic, and pericardial defects can be attempted at the same time.[10,11] Surgical correction is often difficult due to the hypoplasia of the thoraco-abdominal cavity and inability to enclose the ectopic heart as seen in our case. Some of the affected infants have respiratory insufficiency secondary to pulmonary hypoplasia. Norma et al., reported the outcome of 22 patients surgically treated for PC where the babies without EC had a favorable outcome.[11] Hornberger and colleagues published the outcome of surgically repaired cases of EC. Ten out the 13 cases (4 thoracic and 9 thoraco-abdominal EC) were treated in the neonatal period. Three of the infants with major extracardiac defects died before surgical intervention. Five of the seven infants were alive at 3.5 to 9.5 years after successful surgical intervention. The authors concluded that the infants with thoracic and thoraco-abdominal EC with significant intracardiac defects, in the absence of significant extracardiac anomalies, could survive beyond early infancy and undergo successful cardiac repair.[12] In 2008 Hoorn et al., published the results of a PubMed search for outcome of infants with PC. Fifty-eight infants were reported with PC, of which 33 were complete and 23 were incomplete forms. Two patients were incompletely defined. Fourteen infants had EC with structurally normal heart, 16 had normal cardiac situs with intracardiac defects and 23 infants had both. Twenty-nine infants had other associated anomalies. Thirty-seven of 58 infants died within days of birth, including the fetuses terminated following diagnosis of PC. Mortality was higher in infants with complete form of PC and associated extracardiac anomalies. The infants with EC who survived were those who had intracardiac defects.[13]
Increasing awareness of this rare condition among the obstetricians and ultrasonologists will help them in making a diagnosis before viability and thereby an option of termination of the pregnancy if parents wish to do so.
ACKNOWLEDGMENTS
The authors thank Dr. Hjh Rohayati Taib, Specialist Pediatric Cardiologist, for her contributions in fetal and neonatal cardiac screening. We also thank Dr. Ravi Agarwal, Consultant Neonatologist, Hope Hospital, and Greater Manchester, UK for his valuable suggestions after going through the manuscript.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Cantrell JR, Haller JA, Ravitch MM. A syndrome of congenital defects involving the abdominal wall, sternum, diaphragm, pericardium, and heart. Surg Gynecol Obstet. 1958;107:602–14. [PubMed] [Google Scholar]
- 2.Toyama WM. Combined congenital defects of the anterior abdominal wall, sternum, diaphragm, pericardium, and heart: A case report and review of the syndrome. Pediatrics. 1972;50:778–92. [PubMed] [Google Scholar]
- 3.Carmi R, Boughman JA. Pentalogy of Cantrell and associated midline anomalies: A possible ventral midline developmental field. Am J Med Genet. 1992;42:90–5. doi: 10.1002/ajmg.1320420118. [DOI] [PubMed] [Google Scholar]
- 4.Morales JM, Patel SG, Duff JA, Villareal RL, Simpson JW. Ectopia cordis and other midline defects. Ann Thorac Surg. 2000;70:111–4. doi: 10.1016/s0003-4975(00)01388-6. [DOI] [PubMed] [Google Scholar]
- 5.Bittmann S, Ulus H, Springer A. Combined pentalogy of Cantrell with Tetralogy of Fallot, gall bladder agenesis, and polyspleenia: A case report. J Pediatric Surg. 2004;39:107–9. doi: 10.1016/j.jpedsurg.2003.09.030. [DOI] [PubMed] [Google Scholar]
- 6.Assaqat MA, Al-Fayyadh MI, Bulbul ZR. Exteriorisation of the heart in two siblings. Cardiol Young. 2003;13:98–100. doi: 10.1017/s1047951103000155. [DOI] [PubMed] [Google Scholar]
- 7.Morales JM, Patel SG, Duff JA, Villareal RL, Simpson JW. Ectopia cordis and other midline defects. Ann Thorac Surg. 2000;70:111–4. doi: 10.1016/s0003-4975(00)01388-6. [DOI] [PubMed] [Google Scholar]
- 8.Vazquez-Jimenez JF, Muehler EG, Daebritz S, Keutel J, Nishigaki K, Huegel W, et al. Cantrell's syndrome: A challenge to the surgeon. Ann Thoracic Surg. 1998;65:1178–85. doi: 10.1016/s0003-4975(98)00089-7. [DOI] [PubMed] [Google Scholar]
- 9.Rodgers EB, Monteagudo A, Santos R, Greco A, Timor-Tritsch IE. Diagnosis of pentalogy of Cantrell using 2- and 3-dimensional sonography. J Ultrasound Med. 2010;29:1825–8. doi: 10.7863/jum.2010.29.12.1825. [DOI] [PubMed] [Google Scholar]
- 10.Fernandez MS, Lopez A, Vila JJ, Lluna J, Miranda J. Cantrell's pentalogy: Report of four cases and their management. Pediatr Surg Int. 1997;12:428–31. doi: 10.1007/BF01076959. [DOI] [PubMed] [Google Scholar]
- 11.Norma BS, Alfredo VA, Erika SS, Begona SS, Luis AA, Lorenzo RC, et al. Pentalogy of Cantrell. Forty- two years of Experience in the Hospital Infantil de Mexico Federico Gomez. World J Pediatr Congenital Heart Surg. 2011;2:211–8. doi: 10.1177/2150135110390528. [DOI] [PubMed] [Google Scholar]
- 12.Hornberger LK, Colan SD, Lock JE, Wessel DL, Mayer JE., Jr Outcome of patients with ectopia cordis and significant intracardiac defects. Circulation. 1996;94:32–7. [PubMed] [Google Scholar]
- 13.van Hoorn JH, Moonen RM, Huysentruyt CJ, van Heurn LW, Offermans JP, Mulder AL. Pentalogy of Cantrell: Two patients and a review to determine prognostic factors for optimal approach. Eur J Pediatr. 2008;167:29–35. doi: 10.1007/s00431-007-0578-9. [DOI] [PMC free article] [PubMed] [Google Scholar]


