Abstract
Background
Chronic stress affects many Americans. Stress management programs may be prohibitively expensive or have limited access.
Purpose
This study aims to determine feasibility of an 8-week Internet-based stress management program (ISM) based on mindfulness principles in reducing stress in a 12-week, parallel, randomized, controlled trial.
Methods
Participants were randomly allocated to ISM, ISM plus online message board (ISM+), or control groups. Perceived stress, mindfulness, self-transcendence, psychological well-being, vitality, and quality of life were measured at baseline, week 8, and week 12 using standard validated questionnaires.
Results
ISM and ISM+ groups demonstrated statistically significant improvements compared with control on all measures except vitality and physical health.
Conclusions
The ISM program effectively and sustainably reduced measures of stress. The magnitude of improvement is comparable to traditional mindfulness programs, although fewer participants were engaged. This feasibility study provides strong support for online stress management programs, which increase access at a fraction of cost of traditional programs.
Keywords: Mindfulness, Stress management, Internet, Web-based, Well-being, Quality of life, Randomized controlled trial
Stress is caused when an individual perceives environmental demands as beyond his/her adaptive capacity [1]. Severe psychological stress affects approximately 35 % of North Americans [2]; when chronic, it has a similar magnitude of risk as diabetes for development of acute myocardial infarction [2] and is associated with stroke [3], cardiovascular illness [1], hypertension [4], and depression [1, 5]. Prolonged or chronic stress impairs immunity [6] and shortens telomeres [7], a marker of accelerated aging and disease. Stress may be the single largest risk factor in North America for healthcare utilization and expenditures [8].
Psychological stress can be reduced by cultivating mindfulness, a state of consciousness that focuses an individual’s attention and awareness on the present moment and developing a nonjudgmental, conscious awareness of the moment-to-moment experience of one’s environment, thoughts, feelings, and actions [9–11]. One of the better-known mindfulness interventions is Jon Kabat-Zinn’s 8-week Mindfulness-Based Stress Reduction meditation workshop [12], demonstrating positive effects in patients with various chronic diseases [13–17]. However, the Mindfulness-Based Stress Reduction and similar programs require a skilled facilitator, have limited geographic availability, and may be cost prohibitive.
Internet-based stress management (ISM) programs may provide easy access, minimize stress-related diseases, and improve individuals’ resilience. Internet-based psychotherapeutic interventions using cognitive behavioral therapy or psychoeducation have demonstrated similar average effect sizes as traditional face-to-face therapy for a number of conditions including stress, anxiety, and depression [18]. Although mindfulness interventions have been successfully delivered online or remotely, they have been mainly geared toward conditions other than stress, such as depression [19, 20], irritable bowel syndrome [21], and pain [22]. The only two studies (to our knowledge) that have evaluated the effectiveness of virtual mindfulness-based programs for stress management have identified shortcomings, including the resource and practical limitations of videoconference delivery [23] and inconclusive results due to inherent study limitations including small sample size [24].
To facilitate broad access, an 8-week ISM program based on mindfulness principles was developed. In our conceptual framework, increased mindfulness, self acceptance of who you are and your past life, and self-transcendence work to reduce levels of stress that in turn improve vitality and quality of life. Prior to large-scale dissemination, a feasibility study was conducted to assess effectiveness of the program. The primary objective was to evaluate whether the ISM program effectively decreased stress and improved mindfulness, self-acceptance, self-transcendence, and vitality as measured by validated outcomes questionnaires. The secondary objectives were to assess: whether psycho-emotional improvement was accompanied by quality-of-life improvements, whether an online message board would be beneficial, and the relationship between program engagement and outcomes.
Methods
Internet-Based Stress Management Program
The online ISM program was designed to be self-directed and to be accessible and engaging to a wide audience by keeping practices and lessons short. At its core is the development of mindfulness, bringing attention to the present moment with an attitude of nonjudgmental acceptance of one’s experience [9]. The program introduces participants to a new meditation theme each week as described in Fig. 1. The themes and related guided meditation have been to great extent inspired from mindfulness traditions or other mindfulness programs [9] and were chosen to develop mindfulness skills or attitudes and traits that support mindfulness and well-being. The use of the breath as a reminder for present moment awareness is emphasized in all meditations. The program is delivered in four components (Fig. 1). (1) Weekly introductions to the concepts and meditation theme are delivered via Web page views or a 5- to 10-min audio clip. (2) Weekly guided meditations (20–25 min each) are available as embedded or downloadable mp3 format which participants are invited to practice five times each week and to record those practices. (3) Daily articles provide the scientific underpinnings and merits of each week’s theme or discuss various cognitive and behavioral strategies, activities, and concepts supporting or related to mindfulness. (4) Daily tips suggesting how to manage stress or incorporate mindfulness in daily activities and include motivational quotes. The program can be accessed via direct login to the Website or via a hyperlink sent in a twice-weekly e-mail introducing the theme and meditation of the week.
Fig. 1.
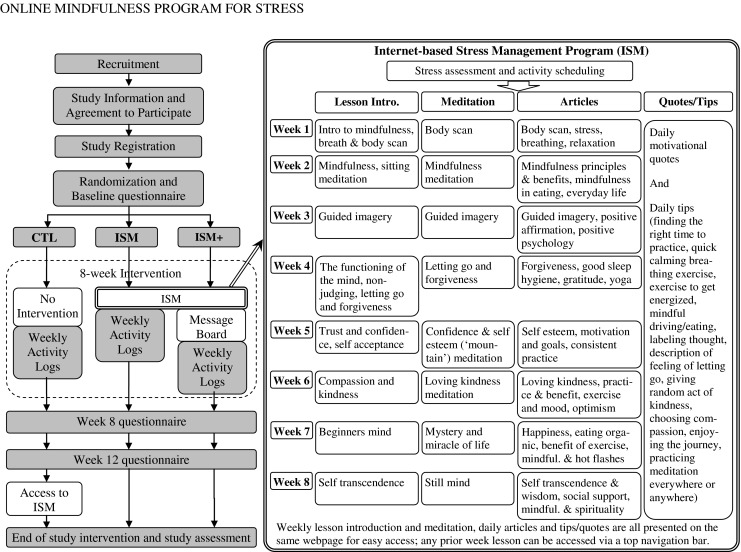
Intervention and study flow. CTL control, ISM Internet-based stress management, ISM+ Internet-based stress management + online message board
Study Population
Participants were recruited via flyers or posters in the clinics, by direct referrals from healthcare providers, or via e-newsletters, Websites, and daily e-mail tips sent to program subscribers. English-speaking participants 18 years or older who agreed to participate in the 8-week ISM and the 4-week follow-up were included. Participants with no regular Internet access were excluded, and for referrals, physicians were instructed to exclude patients with psychosis. The study was approved by an Institutional Review Board which waived formal signed consent. The study was registered at ClinicalTrials.gov (NCT01595555). Interested participants were e-mailed a description of the study and a registration link. All participants received a $15 coupon redeemable at the online wellness store of the host Website after each completed questionnaire. The control group received the ISM program for free after completing the study.
Study Design
The 12-week, randomized, parallel, controlled trial was administered entirely online at the program Website. Participants provided their name and e-mail address and were automatically randomized (using a computer-generated list with a block size of three) into one of three groups (1:1:1 ratio): ISM, ISM plus online message board (ISM+), or control (Fig. 1). All participants were asked to complete online questionnaires at 0 (baseline), 8, and 12 weeks and to fill out weekly activity logs for weeks 1–8. ISM and message board login activity was also monitored. Participants in the ISM and ISM+ groups were given instructions on how to access the ISM program. The ISM+ group was asked to participate in an online message board hosted by iVillage.com. The message board leader posted pre-specified discussion threads to generate interest and facilitated discussion while instructed not to give any advice.
Participants received an e-mail reminder if questionnaires were not completed within 1 week. Failure to complete the weeks 8 and 12 questionnaires within 2 weeks or the weekly log within 1 week resulted in missing data for that time point. At the end of the study, participants were asked to complete a questionnaire about reasons for early study or program termination and overall feedback about the ISM and message board.
Six valid and reliable patient-reported outcome measures were administered. Primary outcome measures were: the Perceived Stress Scale (PSS) [25] uses ten items to measure a person’s perception of and response to daily hassles and stress, resulting in a 0 (best) to 40 total score; the Mindfulness Attention Awareness Scale [26] uses 15 items to measure the frequency of mindful states over time and its mindfulness score of 1 to 6 (highest) predicts well-being and stress reduction; Adult Self-Transcendence Inventory [27] assesses individuals’ ability to separate themselves from external definitions of “self” and to dissolve rigid boundaries between “self” and others, yielding a score of 10 to 40 (highest); Psychological Well-being–Self-Acceptance Subscale [28] uses 14 items to assess a person’s acceptance of who they are now and who they were in the past, yielding a 14 (best) to 84 score; and the Subjective Vitality Scale [29] using seven items to measure the extent to which a person is alert, full of energy, and vital on a 7 to 49 (best) scale. The RAND 36-Item Short Form Health Survey (SF-36) [30] a commonly used generic measure of health status or health-related quality of life developed as part of the Medical Outcomes Study, was included as a secondary measure, with emphasis on two summary scores: Physical Component Score and Mental Component Score [31].
Statistical Analyses
The sample size estimate used data from previous studies to estimate the detectable difference and standard deviation of each of the six questionnaires (e.g., the PSS has detectable difference of 5 and standard deviation of 6) [32]. We determined 102 patients per group would provide 80 % power to detect between-group differences (using a two-side alpha level of 0.05).
Primary analyses used linear mixed-effects models to test outcome changes while accounting for individuals’ repeated measures; all three groups were analyzed simultaneously. The effect of each intervention (ISM and ISM+) compared with the control group at weeks 8 and 12 was estimated (controlling for age, gender, race, education, and income) for participants who responded to baseline and either weeks 8 or 12 questionnaires (i.e., available data).
Pairwise comparisons with a Student’s t test were used for other analyses. Subgroup analyses evaluated the effect of program activity on outcomes. First, analyses computed magnitude of outcome changes for ISM and ISM+ participants who remained engaged by showing some online activity beyond week 5. Second, Pearson correlation coefficients were used to measure association between meditation frequency (i.e., weekly meditation practices measured using activity logs and averaged over 8 weeks) and mean change in outcome during the 8 weeks. Linear model estimates of the magnitude of outcome change per unit increase of meditation frequency during the 8-week program were performed. Analyses were conducted using SAS software, version 9.2 (SAS Institute). Since multiple endpoints were tested individually (rather than a single significant finding among a family of outcomes used to draw study conclusions), there were no corrections for multiple comparisons [33].
Results
Since high dropout rates are expected for online studies [19, 34, 35], we enrolled approximately 700 people to obtain the target sample size; a few participants enrolled twice. Figure 2 shows that 1,204 people received the study description, and 684 (57 %) people enrolled in the study between September 2010 and August 2011. The study ended in November 2011. Of those enrolled, 133 (19 %) were lost prior to providing baseline data. Of the remaining (81 %) who enrolled and completed the baseline questionnaire (n = 551), more than half (57 %) also completed one or both follow-up questionnaires (n = 312). The 8- and 12-week completion rates differed across treatment groups: 41 and 33 % for ISM, 44 and 38 % for ISM+, and 67 and 65 % for the control group at weeks 8 and 12, respectively. No significant within-group differences in baseline characteristics were observed between those who completed questionnaires and those with missing follow-up data.
Fig. 2.

Participants’ progress through the study
As Table 1 shows, most participants were aged 40–59 (59.1 %) and were female (88.9 %) and Caucasian (88.8 %). Most participants had some college education (52.3 %) or post-graduate degree (36.8 %), and most reported an annual income of $40,000–100,000 (51.7 %). The majority (76.6 %) reported previous meditation experience a few times per year or less, and most (50.4 %) were recruited through healthcare referrals or posters. Statistically significant differences between treatment groups were observed at baseline for race and income variables.
Table 1.
Baseline characteristics of participants
| Characteristics | All | CTL | ISM | ISM+ |
|---|---|---|---|---|
| N | 551 | 184 | 183 | 184 |
| Age (%) | ||||
| 18–29 | 11.7 | 14.1 | 9.3 | 11.5 |
| 30–39 | 15.3 | 16.9 | 14.8 | 14.1 |
| 40–49 | 24.5 | 23.9 | 27.3 | 22.3 |
| 50–59 | 34.7 | 32.6 | 35.5 | 35.9 |
| 60–69 | 12.7 | 12.5 | 12.6 | 13.0 |
| 70–79 | 1.7 | 0 | 0.6 | 3.3 |
| ≥80 | 0 | 0 | 0 | 0 |
| Gender (%) | ||||
| Females | 88.9 | 87.5 | 90.7 | 88.6 |
| Race/ethnicity (%)* | ||||
| Caucasian | 88.8 | 88.6 | 89.1 | 88.6 |
| African-American | 5.8 | 6.0 | 5.5 | 6.0 |
| Hispanic | 1.8 | 3.3 | 2.2 | 0 |
| Asian | 2.5 | 0.5 | 2.2 | 4.9 |
| Other | 1.1 | 1.6 | 1.1 | 0.5 |
| Education level (%) | ||||
| Some high school education or less | 0.2 | 0 | 0 | 0.5 |
| High school graduation | 10.7 | 12.0 | 10.9 | 9.2 |
| College education or degree | 52.3 | 49.5 | 53.6 | 53.8 |
| Post-graduation education or higher | 36.8 | 38.6 | 35.5 | 36.4 |
| Family annual income level (%)* | ||||
| <$20 K | 7.8 | 7.1 | 8.2 | 8.2 |
| $20–40 K | 13.4 | 10.9 | 12.6 | 16.9 |
| $40–60 K | 20.7 | 25.5 | 22.4 | 14.1 |
| $60–100 K | 31.0 | 33.2 | 30.6 | 29.4 |
| $100–150 K | 15.3 | 11.4 | 15.9 | 18.5 |
| >$150 K | 11.8 | 12.0 | 10.4 | 13.0 |
| Prior meditation practice (%) | ||||
| Never meditated | 25.6 | 32.1 | 25.7 | 31.0 |
| Once or twice | 31.6 | 30.4 | 33.3 | 31.0 |
| A few times a year | 19.4 | 19.0 | 20.8 | 18.5 |
| A few times a month | 11.4 | 11.4 | 10.9 | 12.0 |
| A few times a week | 4.9 | 4.4 | 6.0 | 4.4 |
| Everyday | 3.1 | 2.7 | 3.3 | 3.3 |
| Recruitment method (%) | ||||
| Doctor | 2.2 | 3.3 | 1.6 | 1.6 |
| Poster or flier at clinic | 31.0 | 34.2 | 31.2 | 27.7 |
| Clinic employee (not referred by doctor) | 17.2 | 14.1 | 18.6 | 19.0 |
| Inner Pulse® (newspaper) | 3.5 | 6.0 | 2.7 | 1.6 |
| Newspaper/flyer/radio ad | 5.3 | 6.5 | 4.9 | 4.4 |
| Friend or family member | 9.1 | 7.6 | 8.7 | 10.9 |
| Othera | 31.8 | 28.3 | 32.2 | 34.8 |
Note. CTL control, ISM Internet-based stress management, ISM+ Internet-based stress management + online message board
*p = 0.01 for race/ethnicity and p = 0.03 for income between CTL and ISM; no other variables were significantly different
aThe main recruitment avenue for “other” is via wellness tips e-mails provided to subscribers
Table 2 indicates that the ISM and ISM+ groups demonstrated a statistically significant difference from control in changes from baseline scores on the PSS, Mindfulness Attention Awareness Scale, Adult Self-Transcendence Inventory, and Psychological Well-being–Self-Acceptance Subscale—indicating that the ISM program was effective in reducing perceived stress and improving mindfulness, transcendence, and self-acceptance compared with the control group at week 8. These improvements were sustained through week 12 and were also reflected in improved mental health as measured by the SF-36 Mental Component Score. The ISM+ versus control comparison for the Subjective Vitality Scale was statistically significant at both time points, whereas the comparisons for the ISM versus control were significant at week 12. Since the linear mixed-effects model results yielded very similar conclusions to the pairwise comparisons, additional analyses were conducted using the simpler pairwise approach. There were no statistically significant differences observed between the ISM and ISM+ groups (Table 2).
Table 2.
Univariate and multivariate comparisons of change from baseline scores between groups (weeks 8 and 12)
| Descriptive statistics using raw data | Change from baseline using linear mixed-effects modela | ||||||
|---|---|---|---|---|---|---|---|
| Baseline | Week 8 | Week 12 | Week 8 | Week 12 | |||
| Mean (SD) | Mean (SD) | Mean (SD) | Adj. mean (CI 95 %) | p value | Adj. mean (CI 95 %) | p value | |
| PSS | |||||||
| CTL | 22.3 (7.1) | 18.8 (7.6) | 18.9 (7.3) | −3.46 (−4.48, −2.43) | <0.0001 | −3.43 (−4.47, −2.40) | <0.0001 |
| ISM | 22.4 (7.1) | 17.2 (6.0)b | 16.0 (6.4)b | ||||
| ISM+ | 22.4 (6.1) | 15.4 (5.9)b | 15.1 (7.0)b | ||||
| ISM vs. CTL | −1.73 (−3.39, −0.06) | 0.043 | −2.92 (−4.68, −1.16) | 0.001 | |||
| ISM+ vs. CTL | −3.21 (−4.83, −1.58) | 0.0001 | −3.39 (−5.07, −1.70) | <0.0001 | |||
| MAAS | |||||||
| CTL | 3.29 (0.90) | 3.65 (0.89) | 3.68 (0.96) | 0.35 (0.24, 0.47) | <0.0001 | 0.40 (0.28, 0.52) | <0.0001 |
| ISM | 3.45 (0.89) | 4.03 (0.80)b | 4.02 (0.82)b | ||||
| ISM+ | 3.24 (0.80) | 3.86 (0.82)b | 3.98 (0.84)b | ||||
| ISM vs. CTL | 0.23 (0.03, 0.42) | 0.022 | 0.22 (0.01, 0.42) | 0.037 | |||
| ISM+ vs. CTL | 0.23 (0.05, 0.42) | 0.015 | 0.34 (0.14, 0.53) | 0.0007 | |||
| ASTI | |||||||
| CTL | 27.4 (4.6) | 29.0 (5.4) | 29.4 (4.8) | 1.57 (0.75, 2.38) | 0.0002 | 1.95 (1.12, 2.77) | <0.0001 |
| ISM | 27.7 (4.8) | 31.5 (4.3)b | 31.1 (4.8)b | ||||
| ISM+ | 27.2 (4.9) | 30.8 (4.7)b | 31.9 (5.8)b | ||||
| ISM vs. CTL | 2.21 (0.89, 3.54) | 0.001 | 1.50 (0.11, 2.90) | 0.035 | |||
| ISM+ vs. CTL | 2.07 (0.78, 3.37) | 0.002 | 2.79 (1.46, 4.13) | <0.0001 | |||
| PWB-SA | |||||||
| CTL | 57.9 (13.2) | 59.5 (12.9) | 59.5 (13.3) | 1.54 (0.12, 2.96) | 0.034 | 2.10 (0.66, 3.53) | 0.004 |
| ISM | 57.1 (14.0) | 62.3 (11.9)b | 61.2 (13.5)b | ||||
| ISM+ | 56.5 (11.7) | 62.4 (11.7) b | 63.7 (12.5)b | ||||
| ISM vs. CTL | 3.73 (1.42, 6.04) | 0.002 | 2.97 (0.53, 5.41) | 0.017 | |||
| ISM+ vs. CTL | 4.14 (1.88, 6.39) | 0.0004 | 4.57 (2.23, 6.91) | 0.0001 | |||
| SVS | |||||||
| CTL | 27.4 (9.1) | 29.1 (9.3) | 29.1 (9.7) | 1.73 (0.67, 2.79) | 0.001 | 1.70 (0.63, 2.77) | 0.002 |
| ISM | 28.0 (8.9) | 31.1 (8.2) | 31.7 (9.4) | ||||
| ISM+ | 28.1 (9.4) | 32.5 (9.1)b | 32.4 (9.3)b | ||||
| ISM vs. CTL | 1.41 (−0.31, 3.13) | 0.11 | 2.06 (0.24, 3.88) | 0.027 | |||
| ISM+ vs. CTL | 2.65 (0.97, 4.33) | 0.002 | 2.54 (0.80, 4.28) | 0.005 | |||
| SF-36 | |||||||
| Physical function | |||||||
| CTL | 83.5 (21.9) | 85.8 (18.5) | 87.1 (18.5) | 2.01 (−0.25, 4.27) | 0.082 | 2.40 (0.10, 4.69) | 0.041 |
| ISM | 81.7 (26.4) | 83.5 (23.0) | 84.5 (21.7) | ||||
| ISM+ | 84.1 (21.6) | 86.1 (16.9) | 85.9 (19.7) | ||||
| ISM vs. CTL | −0.50 (−4.18, 3.19) | 0.79 | −0.78 (−4.67, 3.11) | 0.70 | |||
| ISM+ vs. CTL | −0.02 (−3.61, 3.57) | 0.99 | −2.11 (−5.84, 1.61) | 0.27 | |||
| Role physical | |||||||
| CTL | 68.9 (39.7) | 73.1 (38.7) | 71.9 (39.5) | 4.17 (−2.41, 10.8) | 0.21 | 2.97 (−3.69, 9.63) | 0.38 |
| ISM | 70.5 (41.1) | 80.5 (32.2) | 80.8 (32.4) | ||||
| ISM+ | 73.2 (38.4) | 79.9 (36.2) | 79.9 (34.6) | ||||
| ISM vs. CTL | 5.82 (−4.89, 16.5) | 0.29 | 7.39 (−3.88, 18.7) | 0.20 | |||
| ISM+ vs. CTL | 2.46 (−7.98, 12.9) | 0.64 | 3.73 (−7.07, 14.5) | 0.50 | |||
| Bodily pain | |||||||
| CTL | 69.9 (24.6) | 73.6 (23.9) | 71.8 (24.8) | 3.26 (−0.08, 6.61) | 0.056 | 1.71 (−1.67, 5.09) | 0.32 |
| ISM | 70.1 (27.3) | 76.5 (20.9) | 78.9 (24.5) | ||||
| ISM+ | 69.6 (23.0) | 74.6 (22.6) | 74.5 (22.4) | ||||
| ISM vs. CTL | 3.04 (−2.40, 8.48) | 0.27 | 5.72 (−0.01, 11.5) | 0.051 | |||
| ISM+ vs. CTL | 1.58 (−3.73, 6.89) | 0.56 | 3.09 (−2.41, 8.59) | 0.27 | |||
| General health | |||||||
| CTL | 65.4 (21.3) | 67.1 (21.7) | 66.8 (22.9) | 1.51 (−0.69, 3.71) | 0.18 | 2.27 (0.04, 4.50) | 0.046 |
| ISM | 64.7 (24.8) | 69.2 (23.3) | 68.8 (24.5) | ||||
| ISM+ | 67.8 (21.2) | 73.2 (18.7)b | 74.6 (19.5) | ||||
| ISM vs. CTL | 2.97 (−0.61, 6.55) | 0.10 | 0.63 (−3.16, 4.41) | 0.75 | |||
| ISM+ vs. CTL | 3.18 (−0.32, 6.67) | 0.075 | 2.49 (−1.13, 6.12) | 0.18 | |||
| Vitality | |||||||
| CTL | 42.8 (22.8) | 46.8 (23.4) | 47.7 (24.0) | 4.05 (1.17, 6.94) | 0.006 | 4.92 (2.00, 7.84) | 0.001 |
| ISM | 44.7 (23.3) | 53.8 (22.2)b | 54.0 (24.6) | ||||
| ISM+ | 43.2 (22.8) | 57.7 (21.8)b | 56.9 (23.2)b | ||||
| ISM vs. CTL | 5.11 (0.42, 9.80) | 0.033 | 4.37 (−0.59, 9.33) | 0.085 | |||
| ISM+ vs. CTL | 10.4 (5.81, 15.0) | <0.0001 | 8.79 (4.04, 13.5) | 0.0003 | |||
| Social function | |||||||
| CTL | 67.4 (25.9) | 72.0 (25.9) | 73.1 (26.2) | 4.65 (0.69, 8.61) | 0.022 | 5.74 (1.73, 9.74) | 0.005 |
| ISM | 66.1 (28.6) | 79.0 (22.2)b | 79.3 (23.2) | ||||
| ISM+ | 70.5 (25.9) | 83.4 (22.9)b | 84.8 (19.1)b | ||||
| ISM vs. CTL | 8.21 (1.77, 14.7) | 0.013 | 7.44 (0.65, 14.2) | 0.032 | |||
| ISM+ vs. CTL | 8.27 (1.99, 14.6) | 0.010 | 8.59 (2.09, 15.1) | 0.010 | |||
| Role emotional | |||||||
| CTL | 49.5 (40.1) | 62.1 (40.4) | 59.2 (40.2) | 11.6 (4.42, 18.7) | 0.002 | 9.48 (2.24, 16.7) | 0.011 |
| ISM | 54.7 (42.6) | 68.0 (34.4) | 74.3 (34.6) | ||||
| ISM+ | 57.9 (40.9) | 73.8 (35.9) | 78.6 (35.0) | ||||
| ISM vs. CTL | 2.37 (−9.28, 14.0) | 0.69 | 11.5 (−0.73, 23.8) | 0.066 | |||
| ISM+ vs. CTL | 3.74 (−7.61, 15.1) | 0.52 | 7.70 (−4.04, 19.4) | 0.20 | |||
| Mental health | |||||||
| CTL | 56.7 (19.4) | 62.0 (19.8) | 61.2 (19.9) | 4.89 (2.16, 7.63) | 0.0005 | 4.69 (1.92, 7.45) | 0.001 |
| ISM | 57.1 (20.6) | 69.5 (16.8)b | 66.8 (19.5)b | ||||
| ISM+ | 58.1 (18.6) | 71.2 (18.3)b | 72.1 (20.2)b | ||||
| ISM vs. CTL | 7.43 (2.98, 11.9) | 0.001 | 5.63 (0.93, 10.3) | 0.019 | |||
| ISM+ vs. CTL | 7.47 (3.13, 11.8) | 0.0008 | 8.36 (3.86, 12.9) | 0.0003 | |||
| PCS | |||||||
| CTL | 50.8 (10.9) | 51.1 (9.9) | 51.0 (10.1) | 0.2 (−1.05, 1.45) | 0.76 | 0.14 (−1.12, 1.41) | 0.83 |
| ISM | 49.9 (12.8) | 50.6 (10.8) | 51.3 (10.6) | ||||
| ISM+ | 50.6 (10.8) | 50.7 (9.0) | 51.1 (9.6) | ||||
| ISM vs. CTL | 0.33 (−1.71, 2.36) | 0.75 | 0.17 (−1.98, 2.32) | 0.88 | |||
| ISM+ vs. CTL | −0.16 (−2.15, 1.82) | 0.87 | −0.57 (−2.63, 1.49) | 0.59 | |||
| MCS | |||||||
| CTL | 37.7 (12.1) | 41.3 (12.6) | 40.8 (12.4) | 3.36 (1.60, 5.13) | 0.0002 | 3.33 (1.54, 5.12) | 0.0003 |
| ISM | 38.8 (13.2) | 45.6 (10.9)b | 45.7 (11.4)b | ||||
| ISM+ | 39.1 (12.3) | 47.4 (11.2)b | 48.7 (11.2)b | ||||
| ISM vs. CTL | 3.56 (0.68, 6.43) | 0.016 | 4.00 (0.96, 7.03) | 0.010 | |||
| ISM+ vs. CTL | 4.53 (1.72, 7.34) | 0.002 | 5.14 (2.24, 8.05) | 0.0006 | |||
Available data used; there were no statistically significant differences between the ISM and ISM+ groups. Sample size, n = all participants (CTL, ISM, and ISM+); descriptive baseline, n = 551 (184, 183, and 184); descriptive week 8, n = 279 (124, 75, and 80); descriptive week 12, n = 251 (120, 61, and 70); linear mixed model, n = 313 (136, 83, and 94). Score ranges, PSS (0–40); MAAS (1–6); ASTI (10–40); PWB-SA (14–84); SVS (7–49); SF-36 (0–100). Higher scores are best with the exception of the PSS
CTL control, ISM Internet-based stress management, ISM+ Internet-based stress management + online message board, PSS Perceived Stress Scale, MAAS Mindfulness Attention Awareness Scale, ASTI Adult Self-transcendence Inventory, PWB-SA Psychological Well-being–Self-acceptance, SVS Subjective Vitality Scale, SF-36 Short Form 36, PCS Physical Component Score, MCS Mental Component Score
aLinear mixed-effects model controls for baseline age, gender, race, education, and income
bSignificantly different from control (CTL) using a p value of <0.05
Expected outcomes for those willing to complete most of the program are shown in Table 3. Participants active for 6–8 weeks displayed statistically significant improvements in the PSS, Mindfulness Attention Awareness Scale, Adult Self-Transcendence Inventory, Psychological Well-being—Self-Acceptance Subscale, Subjective Vitality Scale, and SF-36 Mental Component Score at week 8. Numerically, the change scores were larger for the more active participants compared with all participants. For example, relative to control, the more active participants demonstrated a substantial stress (PSS) score improvement of 4.04 (difference between −3.52 and −7.56 in Table 3), compared with 1.73 (ISM) or 3.21 (ISM+) for all participants (Table 2).
Table 3.
Impact of program activity levels on outcomes at week 8
| ISM Website activitya | Meditation frequencyb | |||||
|---|---|---|---|---|---|---|
| Change from baseline at week 8 for those active on ISM Website 6–8 weeks | Linear relationship between mean times meditation practiced over 8 weeks and outcomesc | |||||
| Control | ISM or ISM+ | p value | Pearson correlation coefficient | p value | Change per additional meditation/week | |
| N | 124 | 80 | 115 | |||
| PSS | −3.52 | −7.56 | <0.0001 | −0.20 | 0.03 | −1.53 |
| MAAS | 0.36 | 0.81 | <0.0001 | 0.26 | 0.005 | 0.15 |
| ASTI | 1.52 | 5.14 | <0.0001 | 0.19 | 0.04 | 1.00 |
| PWB-SA | 1.65 | 7.36 | <0.0001 | 0.14 | 0.13 | 1.51 |
| SVS | 1.79 | 5.64 | <0.0001 | 0.05 | 0.62 | 1.06 |
| SF-36 | ||||||
| Physical function | 2.26 | 1.25 | 0.60 | −0.00 | 0.97 | 0.34 |
| Role physical | 4.64 | 6.56 | 0.73 | −0.02 | 0.87 | 1.57 |
| Bodily pain | 3.71 | 5.41 | 0.56 | 0.01 | 0.90 | 1.33 |
| General health | 1.61 | 6.56 | 0.01 | 0.15 | 0.10 | 1.50 |
| Vitality | 4.35 | 15.88 | <0.0001 | 0.02 | 0.86 | 3.14 |
| Social function | 4.64 | 14.69 | 0.004 | 0.10 | 0.29 | 3.43 |
| Role emotional | 12.63 | 21.67 | 0.12 | 0.11 | 0.26 | 4.30 |
| Mental health | 5.29 | 17.45 | <0.0001 | 0.22 | 0.02 | 3.50 |
| PCS | 0.26 | −0.77 | 0.34 | −0.08 | 0.40 | −0.06 |
| MCS | 3.57 | 10.47 | <0.0001 | 0.18 | 0.06 | 2.12 |
Score ranges: PSS (0–40); MAAS (1–6); ASTI (10–40); PWB-SA (14–84); SVS (7–49); SF-36 (0–100). Higher scores are best with the exception of the PSS
CTL control, ISM Internet-based stress management, ISM+ Internet-based stress management + online message board, ASTI Adult Self-Transcendence Inventory, MAAS Mindfulness Attention Awareness Scale, PSS Perceived Stress Scale, PWB-SA Psychological Well-Being Self-Acceptance scale, SVS Subjective Vitality Scale, SF-36 Short Form 36, PCS Physical Component Score, MCS Mental Component Score
aWebsite activity is tracked by recording Website logins. Participants (n = 4) were excluded who started the program more than 1 week after completing the baseline questionnaires
bParticipants (n = 7) were excluded who started the program more than 1 week after completing the baseline questionnaires and because of a discrepancy between self-reported and actual program activity (n = 5)
cParticipants who completed four weekly activity logs (at least two during the last 4 weeks)
The relation between change in outcomes and amount of meditation practice was explored in a sub-analysis. For the 115 participants completing four or more weekly activity logs, meditation practice averaged 4.07 ± 1.59 times/week; the ISM group practiced meditation techniques significantly more often (4.55 ± 1.38) than the ISM+ group (3.68 ± 1.68; p = 0.003). As Table 3 shows, there was a weak yet statistically significant correlation between the mean number of meditation practices per week and stress (PSS, r = −0.20), mindfulness (Mindfulness Attention Awareness Scale, r = 0.26), and transcendence (Adult Self-Transcendence Inventory, r = 0.19) scores. Estimates of the effect on outcome scores per increased meditation practice per week yielded a change of −1.53 for the PSS, 0.15 for the Mindfulness Attention Awareness Scale, and 1.00 for the Adult Self-Transcendence Inventory, assuming the incremental effects are constant. This indicates, for example, that a person who practices meditation techniques an average of 5 times/week will experience a 6.12 decrease (1.53 times 4) in PSS score versus practicing once per week.
Feedback about the ISM program and message board was provided by 78 ISM and 68 ISM+ participants who practiced the relaxation exercise at least once. Of those respondents, 45 % found the overall program to be very or extremely helpful, 35 % somewhat helpful and 19 % little or not at all helpful. When asked about how helpful and beneficial specific components were, 53 % found the meditation techniques, 43 % the weekly audio lesson and 48 % the articles to be very or extremely helpful. Reasons most mentioned for “lack of benefit” were: not finding the time to practice or finding the program too demanding, ineffective or mode of delivery inconvenient. In contrast, of the 52 ISM+ participants who had responded to the feedback questionnaire and accessed the message board at least once, 85 % found the message board to be of little or no help. The main reasons given were lack of time or interest in message board participation, difficulty with accessing the Website, and lack of overall activity on the board.
Discussion
Stress is a major public health issue, and calls have been made for better access to stress management programs to prevent and manage chronic diseases [36]. To our knowledge, this is the first randomized, controlled study that demonstrates feasibility of a completely automated, online, mindfulness-based stress management program designed for broad public access.
This study demonstrates that ISM participants experienced significant reductions in stress. Four of the five primary patient-reported outcome comparisons demonstrated statistically significant differences from baseline scores for each of the ISM and ISM+ groups compared with control at week 8; these results were sustained through at least week 12, demonstrating that ISM program participation yielded improvements in perceived stress, mindfulness, transcendence, and self-acceptance. Vitality results were more variable.
These results appear to be clinically meaningful when using two common clinically important difference (CID) criteria: change of ≥10 % of the score range [37] and ≥0.5 baseline standard deviations [38]. In contrast to the control group, both the ISM and the ISM+ group achieved a clinically important change for the PSS, Mindfulness Attention Awareness, Adult Self-Transcendence Inventory, the SF-36 Mental Component Score, and the SF-36 mental health measures at each time point on both criteria. Furthermore, baseline stress measured by the PSS was 23.05 ± 6.61 points, much higher than the US norm (13.7 ± 6.6 for females; 12.1 ± 5.9 for males) [32]. ISM participation brought the stress levels to a more normal range of 15 or 16 points, on average. This reduction in mean score is similar to observed changes with more intensive mindfulness programs [23, 39] and may have clinical relevance. Similar findings were observed for mindfulness: the Mindfulness Attention Awareness Scale increased by approximately 0.6 or 0.7 points, which is similar to other studies suggesting an increase following the intervention [40, 41].
Despite a reduction in active participation in the online program, sustained outcome improvements persisted until week 12, 4 weeks after the intervention, consistent with other studies showing long lasting effects of mindfulness programs [21, 42]. Overall, the magnitude of improvement in outcome measures of the online ISM program was comparable to traditional face to face mindfulness programs [23, 39–41]. Benefits of the program were even greater for those who remained engaged for 6–8 weeks (Table 3). Future studies should evaluate whether increase in mindfulness is the direct result of the mindfulness concepts, skills learned, and/or the natural consequences of improved stress level and well-being.
Interventions designed to reduce stress have demonstrated health benefits [43, 44]. Although individual health status was not measured, the SF-36 Mental Component Score baseline value (37.0 ± 12.5) shows that our self-diagnosed “stress” study population’s mental health was well below the US average [45]. Statistically significant improvements from baseline Mental Component Score scores were observed for both treatment groups compared with the control group at weeks 8 and 12. These data imply mental health improvements; the magnitude of these changes was substantial (4 or 5 points; Table 2) and similar to other stress management programs [22, 40, 43, 44, 46].
Online message board was an important experimental feature. Some evidence from our study suggested that this component improved some participants’ therapeutic experience. These results and feedback from participants suggest that greater benefits may be achieved with more expansive and integrated social media component.
Approximately one third (35 %) of all ISM and ISM+ enrollees showed online program activity for 6–8 weeks, and 42 % completed the questionnaires at 8 weeks. Program and study retention may be lower than most small-sample-size studies of Web-based programs for psychological disorders, which range from 17 to 98 % with an average of about 70 % [34]; the rates are comparable to larger effectiveness studies [19, 35] and may be more reflective of real-world settings. Main reasons for the high attrition were technical or access problems and being too busy (Fig. 1). An easy online study enrollment process may have led to recruiting participants with no time or real motivation to do the program and may explain the differential dropout between the intervention groups and the control group. An ISM program that can reduce stress in one-third or more of participants suffering from stress would be a substantial contribution. Since the program does not require on-site instructional support, healthcare costs might be further reduced by delivering such programs online for $50 or less per person [47] (compared with facilitator-led workshops, which are in the $400–600 range/person) [48]. Thus, online therapeutic interventions have the potential to reach underserved populations in a cost-effective manner.
As with other studies, the control group reported improvements [23, 40] perhaps due to regression to the mean. Since the participants were self-selected as experiencing stress and seeking out programs, such as ISM, it is not surprising that their stress level decreased whether they received treatment or not. Comparing results to a control group, rather than focusing on within-group changes, minimized the possibility that the observed benefits were due to a transient stress event or positive effects by virtue of clinical trial participation. To further evaluate the role of mindfulness as the principal driver for the observed benefit, future study designs could include an online, attention-matched, educational or active control group.
To maximize generalizability, this feasibility study had broad inclusion criteria and was not limited to specific chronic diseases or conditions. However, this study population being primarily female, white, well educated, and Internet savvy may limit the generalizability of our results. Due to the logistic and resource challenges in collecting disease-specific or stress-related biomarker in an online study, outcomes were self-reported using validated measures. Several technical issues arose. For example, some participants’ failure to receive e-mail notifications may have reduced enrollment and completion rates. Some users experienced problems installing a plug-in software and were unable to complete study questionnaires after enrolling. Other participants (n = 31) did not start the program right after completing their baseline questionnaire, as instructed. Since these technical issues affected few participants, they are unlikely to have affected the results.
Further research is needed to evaluate the efficacy of the ISM program, such as: a longer follow-up period, the ideal program length, use of a treatment alternative control group, patient ratings of treatment and reasons for dropping out of the study, and/or measures of treatment fidelity. A study design that would enable an intent to treat population analysis and include analyses to determine the impact of baseline stress, level of medication and concurrent treatment, and prior meditation experience on outcomes should be evaluated. Considerations should be given to clinical outcome measures using physiological indices of stress, a more specific measure of different kinds of stress and the selection of the study population to focus on heterogeneous as well as disease-specific populations. Also, it will be important to determine whether the attrition rates observed pose a major threat to the internal validity or whether they impact the sustainability of the intervention. Additional efforts may be needed to reduce the dropout rate, such as: more frequent reminders, solving technical issues and selecting participants who can dedicate the time and effort to participate in the intervention and study. Ideas for program improvement should also be considered, such as a shorter program length, improved content, use of mobile apps, or integrating the message board with social networking platforms.
Conclusions
This study demonstrated an 8-week ISM program could feasibly and effectively reduce stress. Benefits were sustained through week 12 for a well-educated, mostly female and computer savvy self-selected population. Although the participant completion rate was low, the magnitude of improvement was significant for those who completed the online program. This study provides support for online stress management programs that are publicly accessible and not cost prohibitive.
Acknowledgments
We thank Michael F. Roizen, MD and Adam Bernstein MD from the Cleveland Clinic for providing valuable comments on the manuscript; Kristina Ceicys for serving as study coordinator providing technical support and managing the recruitment, and follow-up of study participants; and Kelley Friel, KRF Research, Writing and Editing Services for her careful editing of the manuscript.
Potential Conflict of Interest Statement
GE Healthcare and Cleveland Clinic provided funding for this study and both parties were involved in all aspects of the study. The ISM program is owned by the Cleveland Clinic, a nonprofit organization. Drs. Pham and Reese received consulting fees from GE Healthcare to assist with this project. Drs. Morledge and Fu, formerly employees at Cleveland Clinic, received consulting fees from Cleveland Clinic to complete the project.
Footnotes
Drs. Morledge and Allexandre contributed equally to this work. Dr. Morledge was the initial developer of the Internet-based stress management program and was the major contributor to the study design and concept.
References
- 1.Cohen S, Janicki-Deverts D, Miller GE. Psychological stress and disease. JAMA. 2007;298(14):1685–1687. doi: 10.1001/jama.298.14.1685. [DOI] [PubMed] [Google Scholar]
- 2.Yusuf S, Hawken S, Ounpuu S, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): Case–control study. Lancet. 2004;364(9438):937–952. doi: 10.1016/S0140-6736(04)17018-9. [DOI] [PubMed] [Google Scholar]
- 3.O’Donnell MJ, Xavier D, Liu L, et al. Risk factors for ischaemic and intracerebral haemorrhagic stroke in 22 countries (the INTERSTROKE study): A case–control study. Lancet. 2010;376(9735):112–123. doi: 10.1016/S0140-6736(10)60834-3. [DOI] [PubMed] [Google Scholar]
- 4.Lucini D, Di Fede G, Parati G, Pagani M. Impact of chronic psychosocial stress on autonomic cardiovascular regulation in otherwise healthy subjects. Hypertension. 2005;46:1201–1206. doi: 10.1161/01.HYP.0000185147.32385.4b. [DOI] [PubMed] [Google Scholar]
- 5.Siegrist J. Chronic psychosocial stress at work and risk of depression: Evidence from prospective studies. Eur Arch Psychiatr Clin Neurosci. 2008; 258 Suppl:115–9. doi:10.1007/s00406-008-5024-0. [DOI] [PubMed]
- 6.McEwen BS. Protection and damage from acute and chronic stress: Allostasis and allostatic overload and relevance to the pathophysiology of psychiatric disorders. Ann N Y Acad Sci. 2004;1032:1–7. doi: 10.1196/annals.1314.001. [DOI] [PubMed] [Google Scholar]
- 7.Epel ES, Blackburn EH, Lin J, Dhabhar FS, Adler NE, Morrow JD, Cawthon RM. Accelerated telomere shortening in response to life stress. Proc Natl Acad Sci U S A. 2004;101(49):17312–17315. doi: 10.1073/pnas.0407162101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Azagba S, Sharaf MF. Psychosocial working conditions and the utilization of health care services. BMC Publ Health. 2011;11:642. doi: 10.1186/1471-2458-11-642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Baer RA. Mindfulness training as a clinical intervention: A conceptual and empirical review. Clin Psychol Sci Pract. 2003;10(2):125–143. doi: 10.1093/clipsy.bpg015. [DOI] [Google Scholar]
- 10.Shapiro SL, Oman D, Thoresen CE, Plante TG, Flinders T. Cultivating mindfulness: Effects on well-being. J Clin Psychol. 2008;64(7):840–862. doi: 10.1002/jclp.20491. [DOI] [PubMed] [Google Scholar]
- 11.Chiesa A, Serretti A. Mindfulness-based stress reduction for stress management in healthy people: A review and meta-analysis. J Altern Complement Med. 2009;15(5):593–600. doi: 10.1089/acm.2008.0495. [DOI] [PubMed] [Google Scholar]
- 12.Kabat-Zinn J. Full catastrophe living: Using the wisdom of your body and mind to face stress, pain, and illness. New York, NY: Delta; 1990.
- 13.Grossman P, Tiefenthaler-Gilmer U, Raysz A, Kesper U. Mindfulness training as an intervention for fibromyalgia: Evidence of postintervention and 3-year follow-up benefits in well-being. Psychother Psychosom. 2007;25:226–233. doi: 10.1159/000101501. [DOI] [PubMed] [Google Scholar]
- 14.Veehof MM, Oskam MJ, Schreurs KMG, Bohlmeijer ET. Acceptance-based interventions for the treatment of chronic pain: A systematic review and meta-analysis. Pain. 2011;152(3):533–542. doi: 10.1016/j.pain.2010.11.002. [DOI] [PubMed] [Google Scholar]
- 15.Vøllestad J, Sivertsen B, Nielsen GH. Mindfulness-based stress reduction for patients with anxiety disorders: Evaluation in a randomized controlled trial. Behav Res Ther. 2011;49(4):281–288. doi: 10.1016/j.brat.2011.01.007. [DOI] [PubMed] [Google Scholar]
- 16.Sephton SE, Salmon P, Weissbecker I, Ulmer C, Floyd A, Hoover K, Studts JL. Mindfulness meditation alleviates depressive symptoms in women with fibromyalgia: Results of a randomized clinical trial. Arthritis Rheum. 2007;57(1):77–85. doi: 10.1002/art.22478. [DOI] [PubMed] [Google Scholar]
- 17.Gaylord S, Palsson OS, Garland EL, et al. Mindfulness Training reduces the severity of irritable bowel syndrome in women: Results of a randomized controlled trial. Am J Gastroenterol. 2011;106(9):1678–1688. doi: 10.1038/ajg.2011.184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Barak A, Hen L, Boniel-Nissim M, Shapira N. A comprehensive review and a meta-analysis of the effectiveness of internet-based psychotherapeutic interventions. J Technol Hum Serv. 2008;26:109–160. doi: 10.1080/15228830802094429. [DOI] [Google Scholar]
- 19.Meyer B, Berger T, Caspar F, Beevers CG, Andersson G, Weiss M. Effectiveness of a novel integrative online treatment for depression (Deprexis): Randomized controlled trial. J Med Internet Res. 2009;11(2):e15. doi: 10.2196/jmir.1151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Thompson NJ, Walker ER, Obolensky N, et al. Distance delivery of mindfulness-based cognitive therapy for depression: Project UPLIFT. Epilepsy Behav. 2010;19(3):247–254. doi: 10.1016/j.yebeh.2010.07.031. [DOI] [PubMed] [Google Scholar]
- 21.Ljotsson B, Hedman E, Lindfors P, et al. Long-term follow-up of internet-delivered exposure and mindfulness based treatment for irritable bowel syndrome. Behav Res Ther. 2011;49(1):58–61. doi: 10.1016/j.brat.2010.10.006. [DOI] [PubMed] [Google Scholar]
- 22.Gardner-Nix J, Backman S, Barbati J, Grummitt J. Evaluating distance education of a mindfulness-based meditation programme for chronic pain management. J Telemed Telecare. 2008;14(2):88–92. doi: 10.1258/jtt.2007.070811. [DOI] [PubMed] [Google Scholar]
- 23.Wolever RQ, Bobinet KJ, McCabe K, et al. Effective and viable mind-body stress reduction in the workplace: A randomized controlled trial. J Occup Heal Psychol. 2012;17(2):246–258. doi: 10.1037/a0027278. [DOI] [PubMed] [Google Scholar]
- 24.Gluck TM, Maercker A. A randomized controlled pilot study of a brief Web-based mindfulness training. BMC Psychiatry. 2011;11:175. doi: 10.1186/1471-244X-11-175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Heal Soc Behav. 1983;24:386–396. doi: 10.2307/2136404. [DOI] [PubMed] [Google Scholar]
- 26.Brown KW, Ryan RM. The benefits of being present: Mindfulness and its role in psychological well-being. J Personal Soc Psychol. 2003;84(4):822–848. doi: 10.1037/0022-3514.84.4.822. [DOI] [PubMed] [Google Scholar]
- 27.Levenson MR, Jennings PA, Aldwin CM, Shiraishi RW. Self-transcendence: Conceptualization and measurement. Int J Aging Hum Dev. 2005;60(2):127–143. doi: 10.2190/XRXM-FYRA-7U0X-GRC0. [DOI] [PubMed] [Google Scholar]
- 28.Ryff C. Happiness is everything, or is it? Explorations on the meaning of psychological well-being. J Pers Soc Psychol. 1989;57:1069–1081. doi: 10.1037/0022-3514.57.6.1069. [DOI] [Google Scholar]
- 29.Ryan RM, Frederick C. On energy, personality and health: Subjective vitality as a dynamic reflection of well-being. J Personal. 1997;65:529–565. doi: 10.1111/j.1467-6494.1997.tb00326.x. [DOI] [PubMed] [Google Scholar]
- 30.The RAND-36 measure of health-related quality of life. UCLA School of Medicine, Los Angeles, CA, USA. Santa Monica, CA, USA; 2001, Vol. 33, No. 5: Pages 350–357. [DOI] [PubMed]
- 31.Hays RD, Sherbourne CD, Mazel RM. The RAND 36-Item Health Survey 1.0. Health Econ. 1993;2(3):217–227. doi: 10.1002/hec.4730020305. [DOI] [PubMed] [Google Scholar]
- 32.Cohen S, Williamson G. Perceived stress in a probability sample of the U.S. In: Spacapam S, Oskamp S, editors. The social psychology of health: Claremont Symposium on Applied Social Psychology. Newbury Park, CA: Sage; 1988. [Google Scholar]
- 33.Rothman KJ. No adjustments are needed for multiple comparisons. Epidemiology. 1990;1(1):43–46. doi: 10.1097/00001648-199001000-00010. [DOI] [PubMed] [Google Scholar]
- 34.Melville KM, Casey LM, Kavanagh DJ. Dropout from Internet-based treatment for psychological disorders. Br J Clin Psychol. 2010;49(Pt 4):455–471. doi: 10.1348/014466509X472138. [DOI] [PubMed] [Google Scholar]
- 35.Verheijden MW, Jans MP, Hildebrandt VH, Hopman-Rock M. Rates and determinants of repeated participation in a Web-based behavior change program for healthy body weight and healthy lifestyle. J Med Internet Res. 2007;9(1):e1. doi: 10.2196/jmir.9.1.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.American Psychological Association. Latest APA Survey Reveals Deepening Concerns About Connection Between Chronic Disease and Stress; 11 January 2012
- 37.Ringash J, O’Sullivan B, Bezjak A, Relmeier DA. Interpreting clinically significant changes in patient-reported outcomes. Cancer. 2007;110(1):196–202. doi: 10.1002/cncr.22799. [DOI] [PubMed] [Google Scholar]
- 38.Norman GR, Sloan JA, Wyrwich KW. Interpretation of changes in health-related quality of life: The remarkable universality of half a standard deviation. Med Care. 2003;41:582–592. doi: 10.1097/01.MLR.0000062554.74615.4C. [DOI] [PubMed] [Google Scholar]
- 39.Carmody J, Baer RA. Relationships between mindfulness practice and levels of mindfulness, medical and psychological symptoms and well-being in a mindfulness-based stress reduction program. J Behav Med. 2008;31(1):23–33. doi: 10.1007/s10865-007-9130-7. [DOI] [PubMed] [Google Scholar]
- 40.Nyklicek I, Kuijpers KF. Effects of mindfulness-based stress reduction intervention on psychological well-being and quality of life: Is increased mindfulness indeed the mechanism? Ann Behav Med Publ Soc Behav Med. 2008;35(3):331–340. doi: 10.1007/s12160-008-9030-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Dobkin PL, Zhao Q. Increased mindfulness—the active component of the mindfulness-based stress reduction program? Complement Ther Clin Pract. 2011;17(1):22–27. doi: 10.1016/j.ctcp.2010.03.002. [DOI] [PubMed] [Google Scholar]
- 42.Bohlmeijer E, Prenger R, Taal E, Cuijpers P. The effects of mindfulness-based stress reduction therapy on mental health of adults with a chronic medical disease: A meta-analysis. J Psychosom Res. 2010;68(6):539–544. doi: 10.1016/j.jpsychores.2009.10.005. [DOI] [PubMed] [Google Scholar]
- 43.Grossman P, Niemann L, Schmidt S, Walach H. Mindfulness-based stress reduction and health benefits: A meta-analysis. J Psychosom Res. 2004;57:35–43. doi: 10.1016/S0022-3999(03)00573-7. [DOI] [PubMed] [Google Scholar]
- 44.Fang CY, Reibel DK, Longacre ML, Rosenzweig S, Campbell DE, Douglas SD. Enhanced psychosocial well-being following participation in a mindfulness-based stress reduction program is associated with increased natural killer cell activity. J Altern Complement Med. 2010;16(5):531–538. doi: 10.1089/acm.2009.0018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ware JE, Snow KK, Kosinski M, Gandek B. SF-36 health survey: Manual and interpretation guide. Boston, MA: Nimrod Press; 1993. [Google Scholar]
- 46.Moritz S, Quan H, Rickhi B, Liu M, et al. A home study-based spirituality education program decreases emotional distress and increases quality of life—a randomized, controlled trial. Altern Ther Health Med. 2006;12(6):26–35. [PubMed] [Google Scholar]
- 47.Cleveland Clinic Wellness Website. www.ClevelandClinicWellness.com/Relax. Accessed 14 March 2013.
- 48.University of Massachusetts Medical School. Center for Mindfulness in Medicine, Health Care, and Society. Stress Reduction Program, Tuition & Payment Plans. http://www.umassmed.edu/Content.aspx?id=41308. Accessed 14 March 2013


