Abstract
The keratocystic odontogenic tumor (KCOT) is a relatively common oral and maxillofacial lesion with specific characteristics such us rapid growth, extension into the surrounding tissues and high rates of recurrence. Various treatment modalities have been reported. Due to the very thin and friable lining characteristic of the tumor, enucleation can be difficult undertaken and for this reason it is associated with the highest recurrence rates. A 22-year-old male referred to our clinic due to a slight expansion in the right mandible from 2 years ago. He has a history of occurrence of KCOT in this region that was treated surgically by enucleation and curettage 5 years ago. Cone beam computed tomography showed a multilocular radiolucent lesion that extended from the angle of the mandible to the symphysis. Incisional biopsy showed a KCOT recurrence that surgically treated with resection of the right mandible by continuity preservation. Selection of the best treatment modality and also a periodical lifelong follow-up is very important to reduce the rate of recurrence and morbidity of the patient.
Keywords: Keratocyst odontogenic tumor, mandible, recurrence
INTRODUCTION
The keratocystic odontogenic tumor (KCOT) is defined as a benign, intraosseous tumor of odontogenic origin with a potential for aggressive, infiltrative behavior. This tumor shows specific histopathological features and has a high recurrence rate.[1,2,3] in 2005 in the revised World Health Organization classification, the odontogenic keratocysts (OKCs) was recognized as a benign odontogenic tumor and the new terminology is “KCOT.” The range of occurrence is wide from the first to the ninth decade of life.[4] But the more frequency is in the second and third decades. The tumor usually is found more frequently in men than in women.[5,6] Mandible is involved more frequently with a higher incidence in the posterior area of mandibular body and ramus.[3,5,6,7,8] Some of the patients are unaware of the lesion. But symptoms such as swelling, pain and discharge are rather common.[9] In the cases that patients are unaware of their pathological lesion, pathological fractures can occur because of the tendency of the tumor to extend into the medullary cavity. Clinically observable expansion of the bone occurs late.[5]
Penetration of the tumor into the soft tissues, orbit, infratemporal fossa and skull base may occur in aggressive forms.[9,10,11]
The basal cell nevus syndrome is a syndrome with multiple KCOTs.[12]
Radiographically, KCOT appears as a unilocular or multilocular radiolucency with a scalloped contour.[3] The effect on surrounding structures is displacement of unerupted teeth and displacement of the mandibular canal inferiorly or superiorly.[8]
Histopathologically, the KCOT include a thin, uniform layer of epithelium with little or no evidence of rete ridges, a well-defined basal cell layer with palisading cuboidal or columnar cells, and a corrugated, keratinizing luminal surface that is primarily parakeratinized. The presence of small “daughter” or “satellite” cysts may be observed in the connective tissue wall of the KCOT.[13] The tumors linings are thin and fragile, being difficult to enucleate in one piece.[5,14]
The treatment of KCOT is of controversy: Some surgeons advocate conservative therapies, whereas others are in favor of an aggressive treatment.[15,16] Choose of the best treatment modality to lower risk of possible recurrence and also the least morbidity is of importance.[4]
This article presents a case of recurrence of KCOT in the right mandibular body of a male patient after 5 years.
CASE REPORT
A 22-year-old male presented to the clinic of oral and maxillofacial radiology of Isfahan dental school for evaluation of a gradually enlarging hard mass in the right mandible on January, 2013. He reported that the swelling had gradually increased in size over a period of 2 years. He has not any other symptoms such as pain, drainage and neurosensory deficit associated with right inferior alveolar nerve. He has a history of surgery on the right side of the mandible at molar region due to the KCOT in this region 5 years ago with the size of 2.5 × 2.5 cm. Unfortunately, all the patient previous documents except the pathological report were lost.
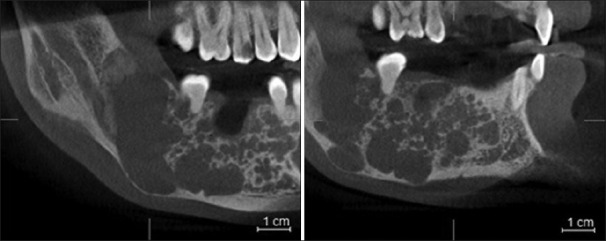
Clinical evaluation showed a slight swelling along all the right mandibular body, second premolar and first molar teeth in this region were extracted. The cone beam computed tomography was performed by Gallileos unit (Sirona dental systems GmbH, Germany, Hessen, Bensheim) with slice thickness and slice interval of 2 mm. Evaluation of coronal, axial and cross-sectional views exhibits a large multilocular radiolucency from the angle of mandible to the symphysis [Figure 1].
Figure 1.

Cone beam computed tomography, panoramic view, extension of a multilocular radiolucent lesion from the angle of the mandible to the symphysis
The lesion expands the inferior border of the mandible and displaced the inferior alveolar canal inferiorly [Figure 2].
Figure 2.
Cone beam computed tomography, tangential view, note to the expansion of the inferior border of the mandible and inferior displacement of the infrior alveolar canal nerve
In the right parasymphis region, the buccal cortical plate of the mandible was perforated in some regions [Figure 3].
Figure 3.

Cone beam computed tomography, axial view, mandibular buccal cortex perforation
Finally, due to the patient's past history and radiological findings, the temporary diagnosis was recurrence of KCOT that was proved by incisional biopsy and the patient referred for surgical treatment. Surgical resection of the right side of the mandible from an angle to the right parasymphis region was done under the general anesthesia and reconstruction with autologous graft was done. The histhopathologic examination confirmed the diagnosis of recurrent KCOT [Figure 4.
Figure 4.

Histopathologic view, H and E,×40
DISCUSSION
KCOT is the second most prevalent cysts of odontogenic origin. The majority of patients are in age from 20 to 29.[9] Males are more involved.[17] Our presented case was a 22-year-old man. The most common site of occurrence of KCOT is posterior mandibular body and angle as we see in this case.[18,19] Radiographically, OKC present as a unilocular or multilocular radiolucency with sclerotic borders.[9] OKCs are significant clinical entities due to their tendency for recurrence and aggressive behavior. Characteristic thin and friable lining of the KCOT that makes removal of the tumor as a single piece difficult.[13,15] The range of recurrence is 13-60%.[20]
The treatment of KCOT remains controversial and various surgical modalities have developed to decrease the rate of recurrence, including enucleation, curettage, marsupialization,[21,22] decompression,[3] enucleation and treatment of the bony defect with Carnoy's solution (a cauterizing mild penetrating agent that is used to the elimination of possible vital cells left behind in the defect),[20,23] liquid nitrogen cryotherapy[22,24] and resection (with or without loss of jaw continuity).[15] Patient characteristics are very important determinants, including the general health status, age, reliability for follow-up, and whether the patient has basal cell nevus syndrome.[15]
Resection has proved to be the most predictable treatment, but the morbidity associated with reconstructing continuity defects seems unwarranted in most instances for a disease with no real metastatic potential, although it is aggressive nature. It is advised to use resection for the more aggressive cysts with perforation of buccal and lingual plates.[14] in the presented case we have a tumor of large size with buccal plate perforation so the surgery decision was resection. As long as more conservative treatment is used, recurrences should be anticipated.[14] In a systematic review[25] the authors stated that for a routine KCOT in a cooperated person who is likely to return for follow-up treatment, Carnoy's solution appeared to be the least invasive procedure with the lowest recurrence rate as was stated by the studies of Stoelinga et al. and Voorsmit et al.[23,26] for very large tumors, decompression followed by enucleation will also have a low recurrence rate. For patients who are unlikely to return for follow-up, the authors recommend resection of the lesion.[21]
The highest rate of recurrence is in cases that treated only by enucleation. So the minimal surgical treatment must be adequate curettage after tumor removal.[23] Recently for the voluminous KCOT of the mandible, endoscopy has been used to assist the surgeon to explore accurately the operative field and areas of difficult access.[16] As was mentioned, choose of the best treatment modality extremely depends on the patient assistance for periodical follow-up. Recurrence can occur many years after treatment, so long-term follow-up is mandatory. Some authors suggest a lifelong follow-up schedule, regardless of the treatment given, every year for the first 5 years and every 2 years thereafter because the recurrence can occur after 40 years.[23] the present case did not refer for the periodical follow-up that allows the tumor to reach to the large size that makes the surgery more difficult and also increases the morbidity of the patient after surgical treatment.
Footnotes
Source of Support: This study was under the support of Isfahan university of medical sciences,school of dentistry and Torabinejad research center
Conflict of Interest: None declared
REFERENCES
- 1.Sanchez-Siles M, Camacho-Alonso F, Lopez-Jornet P, Salazar-Sanchez N. Keratocystic odontogenic tumor. Case report and review of the literature. N Y State Dent J. 2013;79:44–7. [PubMed] [Google Scholar]
- 2.González-Alva P, Tanaka A, Oku Y, Yoshizawa D, Itoh S, Sakashita H, et al. Keratocystic odontogenic tumor: A retrospective study of 183 cases. J Oral Sci. 2008;50:205–12. doi: 10.2334/josnusd.50.205. [DOI] [PubMed] [Google Scholar]
- 3.Maurette PE, Jorge J, de Moraes M. Conservative treatment protocol of odontogenic keratocyst: A preliminary study. J Oral Maxillofac Surg. 2006;64:379–83. doi: 10.1016/j.joms.2005.11.007. [DOI] [PubMed] [Google Scholar]
- 4.Naveen F, Tippu SR, Girish K, Kalra M, Desai V. Maxillary keratocystic odontogenic tumor with calcifications: A review and case report. J Oral Maxillofac Pathol. 2011;15:295–8. doi: 10.4103/0973-029X.86692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shear M. Odontogenic keratocysts: Clinical features. Oral Maxillofac Surg Clin North Am. 2003;15:335–45. doi: 10.1016/S1042-3699(03)00035-9. [DOI] [PubMed] [Google Scholar]
- 6.Oda D, Rivera V, Ghanee N, Kenny EA, Dawson KH. Odontogenic keratocyst: The northwestern USA experience. J Contemp Dent Pract. 2000;1:60–74. [PubMed] [Google Scholar]
- 7.Ali M, Baughman RA. Maxillary odontogenic keratocyst: A common and serious clinical misdiagnosis. J Am Dent Assoc. 2003;134:877–83. doi: 10.14219/jada.archive.2003.0286. [DOI] [PubMed] [Google Scholar]
- 8.van Rensburg LJ, Paquette M, Morkel JA, Nortjé CJ. Correlative MRI and CT imaging of the odontogenic keratocyst: A review of twenty-one cases. Oral Maxillofac Surg Clin North Am. 2003;15:363–82. doi: 10.1016/S1042-3699(03)00037-2. [DOI] [PubMed] [Google Scholar]
- 9.White SC, Pharoah MJ. 6th ed. St. Louis: Mosby Elsevier; 2009. Oral Radiology; pp. 506–12. [Google Scholar]
- 10.Emerson TG, Whitlock RI, Jones JH. Involvement of soft tissue by odontogenic keratocysts (primordial cysts) Br J Oral Surg. 1972;9:181–5. doi: 10.1016/s0007-117x(71)80032-x. [DOI] [PubMed] [Google Scholar]
- 11.Jackson IT, Potparic Z, Fasching M, Schievink WI, Tidstrom K, Hussain K. Penetration of the skull base by dissecting keratocyst. J Craniomaxillofac Surg. 1993;21:319–25. doi: 10.1016/s1010-5182(05)80490-1. [DOI] [PubMed] [Google Scholar]
- 12.Worrall SF. Recurrent odontogenic keratocyst within the temporalis muscle. Br J Oral Maxillofac Surg. 1992;30:59–62. doi: 10.1016/0266-4356(92)90139-a. [DOI] [PubMed] [Google Scholar]
- 13.Eryilmaz T, Ozmen S, Findikcioglu K, Kandal S, Aral M. Odontogenic keratocyst: An unusual location and review of the literature. Ann Plast Surg. 2009;62:210–2. doi: 10.1097/SAP.0b013e31817dad9c. [DOI] [PubMed] [Google Scholar]
- 14.Bell RB, Dierks EJ. Treatment options for the recurrent odontogenic keratocyst. Oral Maxillofac Surg Clin North Am. 2003;15:429–46. doi: 10.1016/S1042-3699(03)00043-8. [DOI] [PubMed] [Google Scholar]
- 15.Ghali GE, Connor MS. Surgical management of the odontogenic keratocyst. Oral Maxillofac Surg Clin North Am. 2003;15:383–92. doi: 10.1016/S1042-3699(03)00042-6. [DOI] [PubMed] [Google Scholar]
- 16.Sembronio S, Albiero AM, Zerman N, Costa F, Politi M. Endoscopically assisted enucleation and curettage of large mandibular odontogenic keratocyst. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107:193–6. doi: 10.1016/j.tripleo.2008.07.020. [DOI] [PubMed] [Google Scholar]
- 17.el-Hajj G, Anneroth G. Odontogenic keratocysts: A retrospective clinical and histologic study. Int J Oral Maxillofac Surg. 1996;25:124–9. doi: 10.1016/s0901-5027(96)80057-9. [DOI] [PubMed] [Google Scholar]
- 18.Forssell K. The primordial cyst. A clinical and radiographic study. Proc Finn Dent Soc. 1980;76:129–74. [PubMed] [Google Scholar]
- 19.Karandikar S, Nilesh K, Dadhich A. Large odontogenic keratocyst of mandible. A case report. J Indian Dent Assoc. 2011;7:822–4. [Google Scholar]
- 20.Browne RM. The odontogenic keratocyst. Clinical aspects. Br Dent J. 1970;128:225–31. doi: 10.1038/sj.bdj.4802449. [DOI] [PubMed] [Google Scholar]
- 21.Giuliani M, Grossi GB, Lajolo C, Bisceglia M, Herb KE. Conservative management of a large odontogenic keratocyst: Report of a case and review of the literature. J Oral Maxillofac Surg. 2006;64:308–16. doi: 10.1016/j.joms.2005.10.013. [DOI] [PubMed] [Google Scholar]
- 22.Pogrel MA. Decompression and marsupialization as a treatment for the odontogenic keratocyst. Oral Maxillofac Surg Clin North Am. 2003;15:415–27. doi: 10.1016/S1042-3699(03)00038-4. [DOI] [PubMed] [Google Scholar]
- 23.Stoelinga PJ. The treatment of odontogenic keratocysts by excision of the overlying, attached mucosa, enucleation, and treatment of the bony defect with Carnoy solution. J Oral Maxillofac Surg. 2005;63:1662–6. doi: 10.1016/j.joms.2005.08.007. [DOI] [PubMed] [Google Scholar]
- 24.Schmidt BL. The use of liquid nitrogen cryotherapy in the management of the odontogenic keratocyst. Oral Maxillofac Surg Clin North Am. 2003;15:393–405. doi: 10.1016/S1042-3699(03)00041-4. [DOI] [PubMed] [Google Scholar]
- 25.Blanas N, Freund B, Schwartz M, Furst IM. Systematic review of the treatment and prognosis of the odontogenic keratocyst. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;90:553–8. doi: 10.1067/moe.2000.110814. [DOI] [PubMed] [Google Scholar]
- 26.Voorsmit RA, Stoelinga PJ, van Haelst UJ. The management of keratocysts. J Maxillofac Surg. 1981;9:228–36. doi: 10.1016/s0301-0503(81)80049-5. [DOI] [PubMed] [Google Scholar]


