Abstract
Background:
Chronic arsenic poisoning is an important public health problem and most notable in West Bengal and Bangladesh. In this study different systemic manifestations in chronic arsenic poisoning were evaluated.
Methods:
A nonrandomized, controlled, cross-sectional, observational study was carried out in Arsenic Clinic, Institute of Postgraduate Medical Education and Research, Kolkata, West Bengal, over a period of 1 year 4 months. Seventy-three cases diagnosed clinically, consuming water containing arsenic ≥50 μg/L and having hair and nail arsenic level >0.6 μg/L, were included. Special investigations included routine parameters and organ-specific tests. Arsenic levels in the drinking water, hair, and nail were measured in all. Twenty-five nonsmoker healthy controls were evaluated.
Results:
Murshidabad and districts adjacent to Kolkata, West Bengal, were mostly affected. Middle-aged males were the common sufferers. Skin involvement was the commonest manifestation (100%), followed by hepatomegaly [23 (31.5%)] with or without transaminitis [7 (9.58%)]/portal hypertension [9 (12.33%)]. Restrictive abnormality in spirometry [11 (15.06%)], bronchiectasis [4 (5.47%)], interstitial fibrosis [2 (2.73%)], bronchogenic carcinoma [2 (2.73%)], oromucosal plaque [7 (9.58%)], nail hypertrophy [10 (13.69%)], alopecia [8 (10.95%)], neuropathy [5 (6.84%)], and Electrocardiography abnormalities [5 (6.84%)] were also observed.
Conclusions:
Mucocutaneous and nail lesions, hepatomegaly, and restrictive change in spirometry were the common and significant findings. Other manifestations were characteristic but insignificant.
Keywords: Arsenic poisoning, ground water, India, West Bengal
INTRODUCTION
Chronic arsenic poisoning results mostly from consumption of contaminated ground water. Areas maximally affected are in Asia, i.e., Bangladesh, West Bengal, Inner Mongolia, China, and Taiwan.[1,2] But the largest reported population exposed to inorganic arsenic is in West Bengal, India, and neighboring Bangladesh. In 1994, it was estimated that over 8,00,000 people in West Bengal were exposed to elevated inorganic arsenic level through drinking water retrieved from tube wells installed in late 1960s.[3,4] WHO guideline permits arsenic level in drinking water up to 10 μg/L. Groundwater arsenic problems result both from natural sources and anthropogenic activities, e.g., mining. Arsenic is derived from reductive dissolution of ferric oxyhydroxide (FeOOH) and release of adsorbed arsenic ferric oxyhydroxide occurs in the aquifer as dispersed phases, such as coatings on sedimentary grains. Once absorbed after consumption of contaminated water, arsenic initially binds to globulin in blood and within 48 h it is redistributed to different organs.
Chronic arsenic poisoning commonly presents as skin lesions. Other common manifestations are chronic liver disease, noncirrhotic portal fibrosis and portal hypertension, chronic sensorimotor polyneuropathy, peripheral vasospastic disease, and diabetes.[5] Arsenic is carcinogenic and its poisoning may manifest as basal cell carcinoma and squamous cell carcinoma of skin, brochogenic carcinoma, angiosarcoma bladder, and colonic cancer. Pulmonary manifestations in chronic arsenic poisoning have been less well studied.[6,7,8,9] Objective of this study was to re-explore different systemic manifestations in chronic arsenic poisoning resulting from consumption of contaminated ground water.
METHODS
This was a nonrandomized, case–control, observational study carried out between April 2008 and July 2009 in the Arsenic Clinic, Institute of Postgraduate Medical Education and Research (IPGMER), Kolkata, West Bengal.
Inclusion criteria
Presence of raindrop mottled skin pigmentation (trunk/limbs)/palmoplantar hyperkeratosis
Arsenic level in the consumed water ≥50 μg/L
Hair or nail arsenic level >0.6 μg/g
Exclusion criteria
Any organ system involvement due to causes other than chronic arsenicosis
Smoking
Occupational lung disease
Diffuse lung parenchymal or pleural disease of other known causes like collagen vascular disease
Cardiac/vascular disease
Control was defined as: 1. Coming from same geographic area; 2. healthy; 3. no past history of pulmonary or cardiovascular disease; 4. arsenic level in the consumed water <50 μg/L; 5. nonsmoker.
Detailed history was taken and thorough physical examination was done. Apart from routine tests, the special investigations done included measurement of arsenic level in the drinking water, hair, and nail, prothrombin time, Ultrasonography (USG) of abdomen, Electrocardiography (ECG), Chest X Ray (CXR), Echocardiography, and spirometry. Arsenic was measured in water samples, hair, and nail in School of Tropical Medicine, Kolkata, using Gudzet apparatus by colorimetric method. High-resultation Computerized Tomography (HRCT) chest, flexible bronchoscopy, and bronchial lung biopsy/bronchial biopsy were done in selected cases where any lesion was suspected by screening tests and none of these was tested in controls. Electromyography (EMG) and Nerve Conduction Velocity (NCV) were also done to evaluate neural/muscular involvement.
Data were analyzed in SPSS statistical software version 15.0. Sample t-test and Pearson chi-squire test were applied for continuous and discrete data, respectively, to find out statistical significance.
The study was approved by the Institute Ethical Committee. There was no conflict of interest.
The study was funded by the hospital authority.
RESULTS
During April 2008 to July 2009, 104 subjects attending Arsenic Clinic, Department of Medicine, IPGMER, Kolkata, were screened. Eighty patients satisfied the inclusion criteria. Seven patients were eliminated following the exclusion criteria and finally 73 cases were enrolled. Twenty-five subjects were considered as controls who were selected consecutively from the same geographic areas. Average age was 42.3±11.24 years. Male:Female ratio was 4.5:1. All the subjects came from within West Bengal, India. Maximum number of cases was from Murshidabad district. Mean arsenic level in the water consumed by the cases was much higher, i.e., 0.25±0.16 mg/L in cases versus 0.018±0.007 mg/L in controls. The levels in hair and nail of cases were also higher as compared to those of controls, i.e., 2.95±1.47 versus 0.59±0.30 mg/g and 5.31±3.33 versus 0.58±0.37 mg/g, respectively. Cases were observed to consume water from older tube wells and controls used to consume the same from newer ones having lower arsenic concentration.
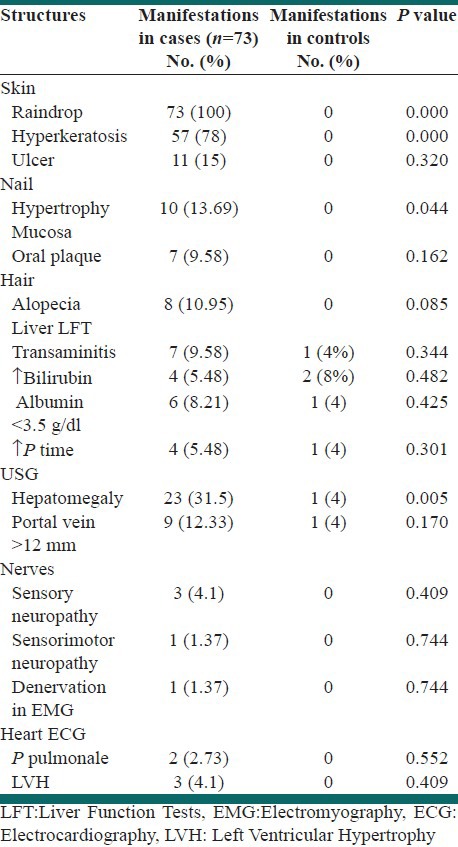
Cases were diagnosed primarily by cutaneous, oromucosal, and nail lesions. Raindrop pigmentation was seen in all the cases. Hyperkeratosis of palm and sole was found in 57 (78%) cases; hepatomegaly was the third most common finding and was seen in 23 (31.5%) cases. However, sonographic evidence of portal hypertension was found in 9 (12.33%) cases only. Systemic manifestations other than pulmonary are detailed in Table 1.
Table 1.
Extrapulmonary manifestations
The most common pulmonary symptom was cough, mostly nonproductive, i.e., in 36 (49.31%) cases (P value 0.000). Shortness of breath was found in 17 (23.28%) cases (P=0.003). CXR abnormalities were found in 8 (10.95%) cases and none of the controls. Spirometric abnormalities were found in 43 (58.91%) cases and 13 (52%) controls. However, only restriction (mild to moderate) in 11 (15.06%) cases was significant (P=0.031) [Table 2]. Bronchiectasis was found in both lungs in 4 (5.47%) and mass in 2 (2.73%) cases histologically confirmed as squamous cell carcinoma. Mild interstitial fibrosis was observed in 2 (2.73%) cases involving lower zones in CXR.
Table 2.
Pulmonary manifestations matched with control
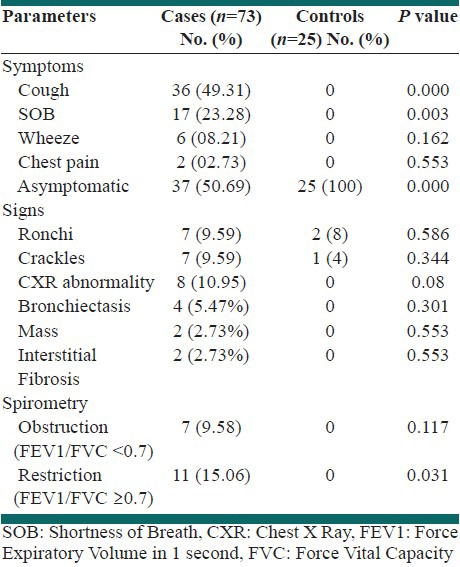
Raindrop pigmentation of skin, hyperkeratosis, nail hypertrophy, hepatomegaly, and mild to moderate restriction in spirometry were significant (P<0.05). Among the controls, no abnormality was detected other than some hepatic manifestations, spirometric abnormalities, and nonspecific chest findings in a few cases.
DISCUSSION
Features of chronic arsenicosis among the residents of different districts of West Bengal, India, one of the most affected areas globally, were studied. Affected persons were predominantly middle-aged males. Arsenic level in the consumed water directly and linearly correlated with that in the hair and nail. Skin lesions and hepatomegaly were significant. Neuropathy, hepatic dysfunction, alopecia, oral plaque, and ECG abnormalities were present only in a small number of patients. Nonproductive cough was the predominant chest symptom. Similar observations were found in two previous studies conducted in West Bengal earlier.[6,8] Lab features were less extensively studied earlier. Compared to other test modalities, spirometric abnormalities were more prevalent but less specific. Contrary to the observation made by De et al., where airway obstruction was the predominant abnormality, restrictive change was little more than obstruction among the cases and the only significant spirometric finding was restriction.[8] Findings of bronchiectasis and bronchogenic carcinoma were lesser and comparable with the said study, but the number of interstitial lung disease cases was much lesser, i.e., 2 (2.73%) versus 9 (8.41%).
CONCLUSION
Chronic arsenic poisoning is mostly due to drinking contaminated water. West Bengal in India is one among the commonest affected geographic areas. Skin and mucosal lesions were most common. These lesions and hepatomegaly were the only significant extrapulmonary manifestations. In pulmonary involvement, nonproductive cough appeared as the commonest symptom. Restrictive change in spirometry was significant. Larger number of cases and equal number of controls need to be studied to delineate different lesions and know their importance.
ACKNOWLEDGEMENT
The author is indebted to all staff of Arsenic Clinic and laboratory personnel of IPGMER, Kolkata, and also staff of Department of Biochemistry, School of Tropical Medicine, Kolkata, India.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Dhar RK, Biswas BK, Samanta G, et al. Groundwater arsenic calamity in Bangladesh. Current Sci. 1997;73:48–59. [Google Scholar]
- 2.Biswas BK, Dhar RK, Samanta G, et al. Detailed study report of Samta, one of the arsenic affected villages of Jessore district, Bangladesh. Current Sci. 1998;74:134–45. [Google Scholar]
- 3.Das D, Chatterjee A, Samanta G, Mandal B, Chowdhury TR, Samanta G, et al. Arsenic contamination in ground water in six districts of West Bengal, India: The biggest arsenic calamity in the World. Analyst. 1994;119:168N–70N. doi: 10.1039/an994190168n. [DOI] [PubMed] [Google Scholar]
- 4.Chatterjee A, Das D, Mandal BK, Roy Chowdhury T, Samanta G, et al. Arsenic in ground water in six districts of West Bengal, India: The biggest calamity in the World, part I: Arsenic species in drinking water and urine of the affected people. Analyst. 1995;120:917–24. doi: 10.1039/an9952000917. [DOI] [PubMed] [Google Scholar]
- 5.Santra A, Das Gupta J, De BK, Roy B, Mazumder DN. Hepatic manifestations in chronic arsenic toxicity. Indian J Gastroenterol. 1999;18:152–5. [PubMed] [Google Scholar]
- 6.Majumder DN, Haque R, Ghosh N, De BK, Santra A, Chakraborti D, et al. Arsenic in drinking water and the prevalence of respiratory effects in West Bengal, India. Int J Epidemiol. 2000;29:1047–52. doi: 10.1093/ije/29.6.1047. [DOI] [PubMed] [Google Scholar]
- 7.Zaldivar R, Ghai GL. Clinical epidemiological study on endemic chronic arsenic poisoning in children and adults, including observations on children with high and low intake of dietary arsenic. Zentralbl Bakteriol B. 1980;170:409–21. [PubMed] [Google Scholar]
- 8.De BK, Majumdar, Sen S, Guru S, Kundu S. Pulmonary involvement in chronic arsenic poisoning from drinking contaminated ground water. J Assoc Physicians India. 2004;52:395–400. [PubMed] [Google Scholar]
- 9.Zaldivar R. A morbid condition involving cardio-vascular, broncho-pulmonary, digestive and neural lesions in children and young adults after dietary arsenic exposure. Zentralbl Bakteriol B. 1980;170:44–56. [PubMed] [Google Scholar]


