Abstract
Background and Objective:
Acute exacerbation of chronic obstructive pulmonary disease (COPD) leads to increased morbidity, mortality and requirement of invasive mechanical ventilation (MV). The aim of this study was to identify predictors of need of MV in these patients.
Materials and Methods:
Clinical symptomatology, demographic profile, biochemical parameters including renal functions, liver functions and acid base parameters, and acute physiology and chronic health evaluation II (APACHE II) score at the time of admission were recorded in 100 patients of COPD exacerbation. Various parameters were compared between patients in whom MV was required with those managed with medical therapy.
Results:
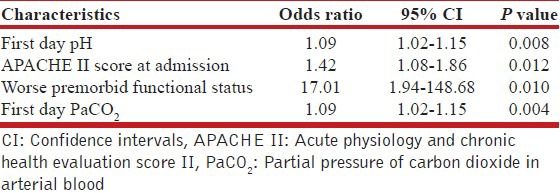
MV was required in 73% of the patients. Parameters found to be independent predictors of need of MV were: Admission APACHE-II score ≥ 11.5 {adjusted odds ratio (OR) [95% confidence interval (CI)]: 1.42 [1.08-1.86]; P = 0.012}, first day pH ≤ 7.28 (adjusted OR [95% CI]: 1.09 [1.02-1.15]; P = 0.008), first day PaCO2 ≥ 68.6 mmHg (adjusted OR [95% CI]: 1.09 [1.02-1.15]; P = 0.004) and worse premorbid functional status (adjusted OR [95% CI]: 17.01 [1.95-148.68]; P = 0.01).
Conclusions:
Underlying disease severity as assessed by premorbid functional status and APACHE-II score, and the acuity of respiratory system decompensation as assessed by the admitting arterial pH and PaCO2, are independent predictors of need of MV in patients with exacerbation of COPD.
KEY WORDS: Acute exacerbation, chronic obstructive pulmonary disease, intubation, mechanical ventilation, predictors
INTRODUCTION
Chronic obstructive pulmonary disease (COPD) is a leading cause of morbidity and mortality worldwide.[1] COPD is the fourth leading cause of mortality and the 12th leading cause of disability. The worldwide prevalence of COPD in 1990 was estimated at 9.34/1000 in men and 7.33/1000 in women.[2] A review of 11 studies involving patients of COPD with acute respiratory failure found a combined mortality rate of 20.3% and mechanical ventilation (MV) rates in the range of 9.8-67.6%.[3] In resource-limited settings such as India, there is perennial shortfall in health care resources. Well-equipped critical care beds are at a premium, and the available numbers fall well short of the number of patients that could potentially benefit by admission to these units. Such a scenario makes appropriate utilization of resources, including the critical care beds, imperative. It stands to reason in such a scenario to offer intensive care unit admission to the patients that are at a higher risk of developing complications, including need of MV. Apart from ensuring close monitoring with prompt intervention as needed, such an approach may even aid in obviating the need of MV in some of these patients. The current study was conducted to identify independent predictors of need of MV in patients with exacerbation of COPD admitted to a tertiary care center.
MATERIALS AND METHODS
This was a prospective study conducted during the period 2003-2005 at a tertiary care center in North India. All patients admitted with a primary admitting diagnosis of acute exacerbation of COPD were eligible for inclusion. All patients had to have a prior confirmed diagnosis of COPD on the basis of fixed airway obstruction on spirometry. All patients with spirometry had FEV1/FVC < 0.70. Exacerbation of COPD was diagnosed on the basis of worsening of at least one of these respiratory symptoms, i.e., dyspnea, cough and/or sputum production, leading to change in medical therapy.[4,5] Patients with underlying COPD admitted with another primary admitting diagnosis (e.g., Accidents, Stroke, Acute Myocardial Infarction) were excluded from the study. Similarly, patients with acute respiratory failure secondary to bronchiectasis, bronchial asthma, active/inactive tuberculosis, pneumothorax, pulmonary embolism, pulmonary edema and neurologic/myopathic causes were also excluded. Informed consent was obtained from the patients or the next of kin.
Clinical and demographic profile at the time of admission, including age, sex, smoking data/status and evidence of cor-pulmonale with or without congestive heart failure, were recorded. Findings on clinical examination including heart rate, respiratory rate and mean blood pressure were recorded. Premorbid functional status was recorded according to the modified Menzies criteria.[6,7] Patients themselves provided information regarding functional status. Spouse/close relatives provided this information in situations where the patient was unable to provide the same for any reason. Acute physiology and chronic health evaluation II (APACHE II) score was recorded at the time of admission.[8] Acid-base abnormalities were analyzed by recording the arterial blood gas analysis and serum electrolytes (estimations done on AVL 995S). Renal functions and liver functions performed at the time of admission were also recorded. Requirement of invasive or non-invasive ventilation (NIV) was recorded. Developments of other complications in the form of acute respiratory distress syndrome (ARDS), sepsis and various types of organ failure were also documented. Days on ventilator were recorded for all patients.
The patients were managed by a team of physicians. The management strategy was decided by the treating physician, and it was individualized for each patient according to the patient's clinical status. All patients received regular nebulized bronchodilators including salbutamol, ipratropium bromide and intravenous steroids. All patients also received antibiotics. Spontaneously breathing patients were administered controlled oxygen therapy (2-3 L/min). Endotracheal intubation was performed for standard indications like respiratory arrest, deteriorating level of consciousness, exhaustion, progressive hypoxemia, hypercapnia and deteriorating acidemia despite maximal level of medical treatment. NIV was used as the initial strategy wherever it was feasible. It was employed for indications as per standard recommendations.[9] Because availability of the non-invasive ventilators was limited at the time the study was conducted, logistics and feasibility regarding NIV significantly impacted the decision to institute NIV. This study was a prospective observational study; therefore, no new drugs or devices were used and no new investigations were carried out other than those that were required during the course of disease management and which were standard of care and were recommended by various medical bodies for managing such patients. This study was approved by the departmental thesis committee consisting of faculty members.
Statistical analysis
Analysis was done using the statistical software “SPSS version 17.0” (SPPS Corp., Chicago, IL, USA). Descriptive analysis consisted of mean with standard deviation and range for various parameters. The study group was divided on the basis of primary outcome of the study (need of intubation). Various parameters were compared between the two groups to identify the predictors of intubation. Continuous variables were analyzed using Student's t-test whereas Fisher's exact test was used to compare the ordinal variables. Parameters found to be significant in univariate analysis were evaluated using multivariate logistic regression analysis to determine independent predictors of need of MV. All the statistical tests performed were two tailed; P < 0.05 was considered statistically significant.
RESULTS
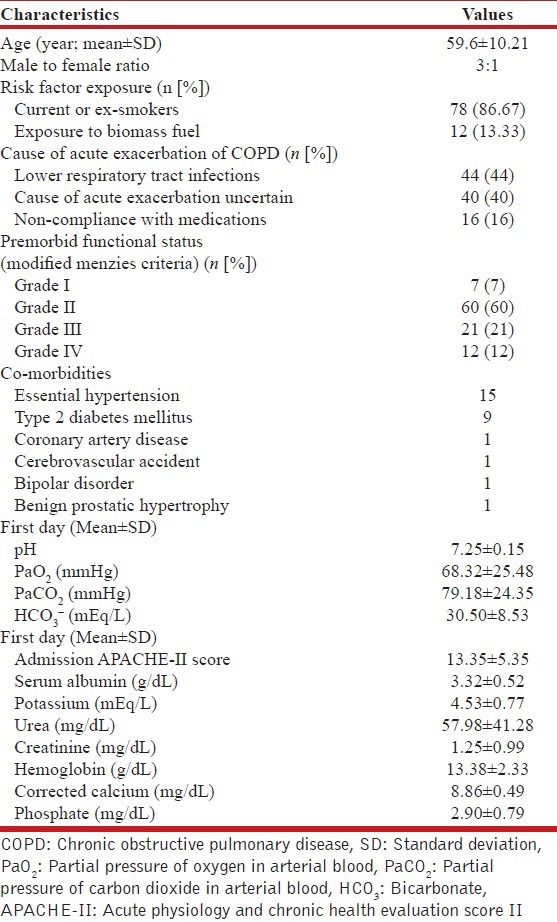
The study group consisted of 100 patients with acute respiratory failure secondary to COPD exacerbation (mean age 59.6 ± 10.21 years, range 40-85 years; M:F 75:25). Majority of the patients (90%) had history of exposure to risk factors for the development of COPD. Majority of men smoked biddi (70%). Almost all patients (97%) had type-II respiratory failure at presentation. Forty-one patients had clinical and ECG changes suggestive of cor-pulmonale while chest X-ray done at the time of admission showed infiltrates in 44% of the patients. Details of baseline characteristics of 100 patients of COPD with acute respiratory failure have been further elaborated in Table 1.
Table 1.
Base line characteristics of 100 patients of chronic obstructive pulmonary disease with acute respiratory failure
Majority of the patients (98.63%) requiring invasive MV had grades-II, III and IV premorbid functional status according to the modified Menzies criteria, while 21 patients (77.73%) managed with only medical care had these grades of functional status. Among the eight patients initially managed with NIV, four had grade III and two each had grades IV and II premorbid functional state.
Ten patients had evidence of sepsis, but none had ARDS at the time of admission. Overall, 73% of the patients required invasive MV. Mean number of days on MV was 10.81 ± 8.40 days. Patients with high admission APACHE-II score; low pH, high PaCO2, low calcium and low corrected serum albumin on first day; and worse premorbid functional status were more likely to need MV in univariate analysis [Table 2]. Of the patients with first day pH < 7.35, 79.7% required MV, with need of MV going up to 85% when the first day pH was < 7.26. In the subgroup of patients with first day pH < 7.20, 88.9% of the patients required invasive MV. Independent predictors of need of MV were admission APACHE-II score ≥ 11.5 {odds ratio [95% confidence interval (CI)]: 1.42 [1.08-1.86]; P = 0.012}, first day pH ≤ 7.28 {odds ratio (95% CI): 1.09 (1.02-1.15); P = 0.008}, first day PaCO2 ≥ 68.6 mmHg {odds ratio (95% CI): 1.09 (1.02-1.15); P = 0.004} and worse premorbid functional status {odds ratio (95% CI): 17.01 (1.94-148.68); P = 0.010} [Table 3]. Thirty-six (36%) patients had in-hospital mortality. The predominant cause of death was septicemia (72%). Ten patients needed reintubation after planned extubation.
Table 2.
Predictors for intubation in patients of chronic obstructive pulmonary disease with acute exacerbation
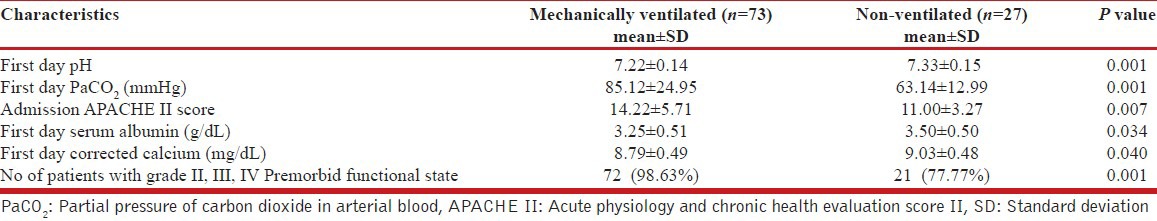
Table 3.
Logistic regression of variables predictive of requirement of mechanical ventilation in patients admitted with acute exacerbation of chronic obstructive pulmonary disease
DISCUSSION
The current study identified independent predictors of need of MV in the group of COPD exacerbation patients with acute respiratory failure admitted to a tertiary care center in North India. The course of COPD is marked by progressive deterioration in lung function and functional status punctuated by episodes of acute exacerbation. These patients with acute exacerbation frequently require ventilatory support. The incidence of need of invasive MV in patients with exacerbation of COPD has varied from 9.8% to 67.6%.[3] The huge variation in the earlier studies is likely due to the variability in the illness severity among the patients included. In our series, an even higher proportion of patients (73%) required invasive MV. This is likely due to an inherent selection bias in the current study. The study group consisted of a highly selected population of COPD patients. Several patients with exacerbation of COPD presenting to our medical center are unable to get admitted due to a perennial paucity of beds. Many such patients who are stable enough to be transferred are referred to other institutions, thereby leaving behind mostly the sickest and unstable patients for admission to our Institute. The severity of the illness of these COPD exacerbation patients is of the highest order. A high mean APACHE II score at admission and a much higher incidence of need of MV are reflective of the same. This fact also makes the current study unique from earlier studies by showing the predictive capability of commonly used predictor variables such as APACHE II score and simple physiological measurements among patients with the most severe forms of COPD exacerbation.
Patients with higher first day APACHE-II score, acidemia, hypercarbia and worse premorbid functional status were more likely to need MV on multivariate analysis. Arterial pH has been reported as independent predictor of need of MV in earlier studies as well. Khilnani et al.[10] Hoo et al.[11] and Sluiter et al.[12] have earlier reported association of worse acidemia with higher intubation rates. They also described a threshold pH below which the rate of intubation was remarkably high in COPD patients with acute exacerbation with respiratory failure. Khilnani et al.[10] and Hoo et al.[11] identified a threshold of 7.25. In the study by Hoo et al.[11] the rate of intubation was the highest in patients having pH of < 7.20. They also noted that in more acidemic patients, there was a shorter time gap between the presentation of patient to hospital and the time of intubation. Sluiter and colleagues[12] noted that the intubation rates were 85% in patients with a pH of < 7.20 and 63% in patients with pH between 7.21 and 7.40. In our study, a similar trend was noted with 79.7% of patients having first day pH of < 7.35 requiring MV, with requirement of MV going up to 85% when the first day pH was < 7.26. In the subgroup of patients who had first day pH of < 7.20, 88.9% of the patients required invasive MV. Arterial PCO2 at presentation was also an independent predictor of requirement of MV. PaCO2 was also found to be significantly higher in patients requiring invasive MV in a study by Vitacca et al.[13] The observation that the patients having greater degree of acidosis and hypercarbia need MV more frequently stands to reason. Acute exacerbation of COPD leads to increase in ventilation perfusion mismatch due to airway narrowing induced by inflammation, bronchospasm, mucus secretion, increased intrinsic positive end expiratory pressure and/or gas trapping and dynamic hyperinflation. Besides ventilation perfusion mismatch, development of respiratory muscle fatigue due to tachypnea and decreased skeletal muscle mass and alveolar hypoventilation also contribute to raised PaCO2 and more acidotic pH.[14,15,16] Worsening acidosis with hypercapnia is an objective indicator of ineffective alveolar ventilation, regardless of the underlying mechanism, and is often a prelude to frank respiratory failure and/or arrest.
High APACHE-II score on admission, indicating the greater severity of acute physiologic dysfunction, was an independent predictor of MV. Vitacca et al.[13] showed in their study that higher APACHE-II score had a high predictive value for need of MV. Ucgun et al.[17] also demonstrated that high APACHE II score was one of the independent predictors of need of MV. Further, in the study by Hoo et al.,[11] mechanically ventilated patients had significantly higher APACHE-II score. Seneff et al.[18] also noted a significantly higher APACHE-II score in mechanically ventilated patients.
Premorbid functional status is a good summary measure influenced by many clinical factors. It indicates the condition of the patient in terms of severity of dyspnea, level of independence in doing activities of daily living reflecting potential severity of underlying COPD and other associated conditions. In a study by Menzies et al., premorbid functional status was more strongly associated with outcome measure than any other single measure. According to them, this may reflect the limitations of current physiologic measures in assessing the impact of disease fully.[6] In our study, worse premorbid functional status was independently associated with greater likelihood of MV. This is an intriguing finding and suggests that need of MV is as much influenced by the underlying chronic disease severity as by the acute insult of the exacerbation. The major strength of this study is the prospective nature of the study. Further, the current study also validates the predictive capability of commonly used variables in a sicker group of COPD patients. This study has got few limitations as well. The biggest limitation of this study was the low use of NIV, as availability of the NIV was limited at the time the study was conducted. The logistics and feasibility regarding NIV significantly impacted the decision to institute NIV. Another limitation of this study is inclusion of patients with pulmonary infiltrates.
In conclusion, underlying disease severity as assessed by premorbid functional status and APACHE-II score, and the acuity of respiratory system decompensation as assessed by the admitting arterial pH and PaCO2 are independent predictors of need of MV in patients with exacerbation of COPD.
ACKNOWLEDGMENT
Contribution of staff of respiratory lab and all patients who participated in this study is greatly acknowledged.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Hurd S. The impact of COPD on lung health worldwide: Epidemiology and incidence. Chest. 2000;1:1S–4. doi: 10.1378/chest.117.2_suppl.1s. [DOI] [PubMed] [Google Scholar]
- 2.Murray CJ, Lopez AD. Cambridge, MA: Harvard University Press; 2006. The global burden of disease: A comprehensive assessment of mortality and disability from diseases, injuries and risk factors in 1990 and projected to 2020; pp. 325–97. [Google Scholar]
- 3.Weiss SM, Hudson LD. Outcome from respiratory failure. Crit Care Clin. 1994;10:197–215. [PubMed] [Google Scholar]
- 4.American Thoracic Society. Standards for the diagnosis and care of patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1995;152:S77–121. [PubMed] [Google Scholar]
- 5.Global Initiative for Chronic Obstructive Lung Disease: Global strategy for the diagnosis, management and prevention of Chronic Obstructive pulmonary disease. Updated. 2005. [Last accessed on 2007 Nov 20]. http://www.goldcopd.org/Guidelineitem .
- 6.Menzies R, Gibbons W, Goldberg P. Determinants of weaning and survival among patients with COPD who require mechanical ventilation for acute respiratory failure. Chest. 1989;95:398–405. doi: 10.1378/chest.95.2.398. [DOI] [PubMed] [Google Scholar]
- 7.Breen D, Churches T, Hawker F, Torzillo PJ. Acute respiratory failure secondary to chronic obstructive pulmonary disease treated in the intensive care unit: A long term follow up study. Thorax. 2002;57:29–33. doi: 10.1136/thorax.57.1.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Knaus WA, Draper EA, Wagner DP, Zimmerman JE. Prognosis in acute organ-system failure. Ann Surg. 1985;202:685–93. doi: 10.1097/00000658-198512000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.British Thoracic Society Standards of Care Committee. Non-invasive ventilation in acute respiratory failure. Thorax. 2002;57:192–211. doi: 10.1136/thorax.57.3.192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Khilnani GC, Banga A, Sharma SK. Predictors of need of mechanical ventilation and reintubation in patients with acute respiratory failure secondary to chronic obstructive pulmonary disease. Indian J Crit Care Med. 2006;10:88–94. [Google Scholar]
- 11.Hoo GW, Hakimian N, Santiago SM. Hypercapnic respiratory failure in COPD patients: Response to therapy. Chest. 2000;117:169–77. doi: 10.1378/chest.117.1.169. [DOI] [PubMed] [Google Scholar]
- 12.Sluiter HJ, Blokzijl EJ, van Dijl W, van Haeringen JR, Hilvering C, Steenhuis EJ. Conservative and respirator treatment of acute respiratory insufficiency in patients with chronic obstructive lung disease. A reappraisal. Am Rev Respir Dis. 1972;105:932–43. doi: 10.1164/arrd.1972.105.6.932. [DOI] [PubMed] [Google Scholar]
- 13.Vitacca M, Clini E, Porta R, Foglio K, Ambrosino N. Acute exacerbations in patients with COPD: Predictors of need for mechanical ventilation. Eur Respir J. 1996;9:1487–93. doi: 10.1183/09031936.96.09071487. [DOI] [PubMed] [Google Scholar]
- 14.Barberà JA, Roca J, Ferrer A, Félez MA, Díaz O, Roger N, et al. Mechanisms of worsening gas exchange during acute exacerbations of chronic obstructive pulmonary disease. Eur Respir J. 1997;10:1285–91. doi: 10.1183/09031936.97.10061285. [DOI] [PubMed] [Google Scholar]
- 15.Emerman CL, Connors AF, Lukens TW, Effron D, May ME. Relationship between arterial blood gases and spirometry in acute exacerbations of chronic obstructive pulmonary disease. Ann Emerg Med. 1989;18:523–7. doi: 10.1016/s0196-0644(89)80837-6. [DOI] [PubMed] [Google Scholar]
- 16.Rossi A, Gottfried SB, Higgs BD, Zocchi L, Grassino A, Milic-Emili J. Respiratory mechanics in mechanically ventilated patients with respiratory failure. J Appl Physiol. 1985;58:1849–58. doi: 10.1152/jappl.1985.58.6.1849. [DOI] [PubMed] [Google Scholar]
- 17.Ucgun I, Metintas M, Moral H, Alatas F, Yildirim H, Erginel S. Predictors of hospital outcome and intubation in COPD patients admitted to the respiratory ICU for acute hypercapnic respiratory failure. Respir Med. 2006;100:66–74. doi: 10.1016/j.rmed.2005.04.005. [DOI] [PubMed] [Google Scholar]
- 18.Seneff MG, Wagner DP, Wagner RP, Zimmerman JE, Knaus WA. Hospital and 1-year survival of patients admitted to intensive care units with acute exacerbation of chronic obstructive pulmonary disease. JAMA. 1995;274:1852–7. [PubMed] [Google Scholar]


