Abstract
Objective. In developed countries, the functional status scores of patients with poor preoperative scores undergoing total joint replacement (TJR) improve more following TJR than those for patients with better preoperative scores. However, those with better preoperative scores achieve the best postoperative functional outcomes. We determined whether similar associations exist in a developing country.
Methods. Dominican patients undergoing total hip or knee replacement completed WOMAC and SF-36 surveys preoperatively and at 12-month follow-up. Patients were stratified into low-, medium- and high-scoring preoperative groups based on their preoperative WOMAC function scores. We examined the associations between the baseline functional status of these groups and two outcomes—improvement in functional status over 12 months and functional status at 12 months—using analysis of variance with multivariable linear regression.
Results. Patients who scored the lowest preoperatively made the greatest gains in function and pain relief following their TJRs. However, there were no significant differences in pain or function at 12-month follow-up between patients who scored low and those who scored high on preoperative WOMAC and SF-36 surveys.
Conclusion. Patients with poor preoperative functional status had greater improvement but similar 12-month functional outcomes compared with patients who had a higher level of function before surgery. These results suggest that a policy of focusing scarce resources on patients with worse functional status in developing countries may optimize improvement following TJR without threatening functional outcome. Additional research is needed to confirm these findings in other developing countries and to understand why these associations vary between patients in the Dominican Republic and patients from developed countries.
Keywords: international, joint replacement, medical mission, knee hip arthroplasty, improvement patterns
Introduction
As longevity increases sharply in developing countries, the global burden of chronic disease, including OA and other joint disease, will rise concurrently [1]. In many developed countries, people with severe functional limitation and joint destruction often opt for total joint replacement (TJR), a procedure that improves function [2], decreases pain and increases quality of life and satisfaction [3]. Although these procedures are cost effective [4, 5], their high costs are difficult to finance in developing countries. To address this growing burden of joint disease in developing countries, medical mission organizations like Operation-Walk (Op-Walk) Boston provide TJRs at no cost to qualifying patients from the developing world. In addition, some developing countries are currently establishing and evaluating their own TJR programmes [6]. Although many medical mission organizations provide clinical services, few document and assess the outcomes of the services they provide, despite increasing scrutiny about outcomes of care provided by short-term medical mission teams [7]. Quality and safety have been assessed for some medical mission trips [8, 9], but there is currently a dearth of outcomes analyses from orthopaedic mission trips.
To assess TJR outcomes in developed countries, pain and functional status are typically recorded before and after surgery with validated patient surveys [10, 11] such as the WOMAC and the Short Form-36 Health Survey (SF-36). These instruments measure pain and functional limitations related to lower extremity arthritis (WOMAC) and overall health status (SF-36). In developed countries, people with worse functional status scores before surgery made the greatest gains in these scores following TJR, but their final scores (at 1 or 2 years postoperatively) were worse than those of individuals who had better preoperative scores. Thus, operating earlier in the course of functional decline appears to result in better outcomes [12]. These findings have led to a gradual reappraisal of optimal timing for TJR, with TJR offered earlier in the process of functional decline to reduce the period of disability and to improve the functional outcome [13]. In previously reported research from the Dominican Republic, the Op-Walk Boston team demonstrated that patients’ WOMAC and SF-36 scores improve dramatically following their TJRs [14]. Associations between preoperative WOMAC/SF-36 surveys and ultimate TJR outcomes in the Dominican Republic, and in other developing countries, have not been studied.
Using data from the WOMAC and SF-36 scores taken preoperatively and at 1-year follow-up, we evaluated the improvement patterns of 97 low-income patients from the Dominican Republic who received total knee and hip replacement during Op-Walk Boston’s 2009, 2010 and 2011 trips to the Dominican Republic. By assessing associations between patients’ preoperative WOMAC and SF-36 scores and their ultimate TJR outcomes, we evaluated whether score improvement patterns in developing countries match patterns observed in developed countries. Insight into the associations between preoperative WOMAC and SF-36 scores and TJR outcomes may help leaders of TJR programmes in developing countries better understand the optimal point at which to operate during the process of functional decline, informing the allocation of these programmes’ limited resources.
Patients and methods
Setting
Although the Dominican Republic has a publically funded health care plan, low-income citizens typically lack resources for highly complex and high-cost medical interventions [15], including joint replacement. To address these unmet needs, the Op-Walk Boston team travels annually to La Hospital General de la Plaza de la Salud in Santo Domingo, a private hospital, to perform total knee and hip replacement for qualifying participants.
Participant selection
From 2009 to 2011, physicians from the Orthopaedic Department at the Hospital General de la Plaza de la Salud assembled a group of low-income patients who had advanced arthritis and joint destruction. Prior to the Op-Walk team’s departure from Boston, Op-Walk’s surgical team reviewed patients’ radiographic images and medical records to confirm appropriateness for total hip or knee replacement. When the Op-Walk team arrives in the Dominican Republic, Op-Walk’s surgical team performs a detailed preoperative assessment of all patients to finalize surgical plans and obtain informed consent for surgery. This study was approved by the institutional review boards at both the Brigham and Women’s Hospital in Boston and the Hospital General de la Plaza de la Salud in Santo Domingo.
Survey information
The pre- and postoperative surveys incorporated Spanish versions [16, 17] of the SF-36 [18] physical activity and mental health subscales and the WOMAC [19, 20]. These instruments have been validated previously and are widely used for evaluating TJR outcomes [21, 22]. To simplify interpretation, we transformed the SF-36 and WOMAC scores to a 0- to 100-point scale, with 100 representing the best score. Cronbach’s alpha coefficients were previously reported to exceed 0.75 in the Dominican cohort for each of the WOMAC and SF-36 subscales included in the surveys [14]. This level of reliability exceeds the commonly accepted threshold of 0.70, supporting the internal consistency of these scales in the Dominican cohort [23].
In addition to the SF-36 and WOMAC instruments, the preoperative surveys also requested patients’ demographic information (age, education level, gender, employment and living arrangements) as well as their perception that TJR would relieve their pain or lead to operative complications. The postoperative survey also asked questions related to surgical outcome satisfaction and quality of life improvements.
Preoperative and postoperative data collection
During the preoperative evaluation, the research team provided patient fact sheets about the study and patients were offered the opportunity to opt out. Research associates then administered the surveys to consenting participants. Patients who underwent TJR in 2009, 2010 and 2011 were asked each year to return to the hospital for annual follow-up appointments. During this appointment, the patients filled out WOMAC/SF-36 follow-up forms. All surveys are written in Spanish and research associates provided assistance with reading and interpreting the survey, when necessary.
Statistical analysis
The knee replacement and hip replacement cohorts had similar baseline and 1-year follow-up characteristics (supplementary Tables S1 and S2, available at Rheumatology Online). Because of these similarities, we combined the knee and hip groups together in our analyses. To determine whether patients who started with lower function level improved more than those who started at a higher level of function, patients were stratified into tertiles using their preoperative WOMAC functional status scores. For each outcome we investigated the association between preoperative functional status tertile and both the 12-month score and the score improvement. We calculated the mean in each group and used one-way analysis of variance to test for overall group differences. Tukey’s studentized range test was used to perform pairwise comparisons when the overall test was statistically significant.
We used multivariable linear regression models to adjust for sex, procedure (bilateral vs unilateral), joint (knee vs hip) and education. Separate models of hip and knee replacement yielded similar results, so we provided data on the combined hip and knee replacement cohorts to achieve more stable estimates.
Results
Recruitment
In 2009, 2010 and 2011, a total of 130 patients were invited to participate in our study. A total of 123 patients agreed to participate and subsequently completed baseline forms. Of the patients who completed baseline forms, 97 attended their 1-year follow-up visit and completed a follow-up form. There were no differences in demographic or baseline clinical characteristics between patients who attended follow-up and patients who did not attend follow-up.
Demographic data
The majority of patients were female (81.4%) and the mean age was 60.9 (s.d. = 11.8). Total knee replacement was performed in 72.9% of patients and the remainder received total hip replacement (one patient received both total knee replacement and total hip replacement); 61.5% of cases were unilateral. The majority (75%) of patients had less than a high school education, 19.6% were working at the time of the survey and 92.7% lived with friends or family members. The mean ASA score was 2.2 (s.d. = 0.5) and the average BMI was 28.9 (s.d. = 5.7). The majority (76.6%) of patients believed that the surgery had a >90% chance of relieving their pain and 58.7% of patients believed that there was <1% chance that they would experience some kind of complication (Table 1).
Table 1.
Patient demographics for all Op-Walk patients
| Demographic | Overall (n = 97) | Highest (best) tertile (n = 33) | Medium tertile (n = 32) | Lowest (worst) tertile (n = 32) |
|---|---|---|---|---|
| Female sex | 79 (81.4) | 21 (63.6) | 28 (87.5) | 30 (93.8) |
| Age, n; mean (s.d.), years | 97; 60.9 (11.8) | 33; 62.0 (8.8) | 32; 58.0 (13.4) | 32; 62.8 (12.6) |
| Education, completed secondary school or higher | 24 (25.3) | 11 (33.3) | 8 (25.8) | 5 (16.1) |
| Currently working | 19 (19.6) | 12 (36.4) | 5 (15.6) | 2 (6.3) |
| Living with friends or family members | 89 (92.7) | 29 (87.9) | 31 (100.0) | 29 (90.6) |
| ASA, n; mean (s.d.) | 90; 2.2 (0.5) | 30; 2.1 (0.5) | 29; 2.1 (0.5) | 31; 2.2 (0.4) |
| BMI, n; mean (s.d.) | 79; 28.9 (5.7) | 28; 28.6 (5.6) | 24; 29.2 (6.3) | 27; 29.0 (5.4) |
| BMI > 35 | 10 (12.7) | 4 (14.3) | 2 (8.3) | 4 (14.8) |
| Health ≥ good | 47 (50.5) | 17 (54.8) | 15 (50.0) | 15 (46.9) |
| Surgery > 90% chance of relieving pain | 72 (76.6) | 23 (71.9) | 22 (71.0) | 27 (87.1) |
| Chance of major surgical complication <1% | 54 (58.7) | 15 (48.4) | 16 (53.3) | 23 (74.2) |
| Procedure, knee | 70 (72.9) | 24 (72.7) | 20 (62.5) | 26 (83.9) |
| Procedure, hip | 26 (27.1) | 9 (27.3) | 12 (37.5) | 5 (16.1) |
| Procedure, unilateral | 59 (61.5) | 28 (84.8) | 18 (56.3) | 13 (41.9) |
| Procedure, bilateral | 37 (38.5) | 5 (15.2) | 14 (43.8) | 18 (58.1) |
Data are n (%) unless stated otherwise.
Pain and function scores
Before undergoing TJR, patients had, on average, poor baseline WOMAC function (mean = 33.6, s.d. = 23.3) and SF-36 physical function (mean = 15.5, s.d. = 17.4) scores [13]. The cohort also had poor baseline WOMAC stiffness scores (mean = 35.3, s.d. = 26.2). By contrast, the cohort had good SF-36 mental health scores (mean = 75.0, s.d. = 16.6).
Following surgery, patients improved substantially from their baseline WOMAC function (cohort mean improvement = 53.3, s.d. = 26.0), SF-36 physical function (cohort mean improvement = 56.7, s.d. = 24.3), WOMAC pain (cohort mean improvement = 47.8, s.d. = 31.0) and WOMAC stiffness (cohort mean improvement = 47.9, s.d. = 33.9) scores. SF-36 mental health scores also improved modestly (cohort mean = 6.5, s.d. = 21.3) (Table 2).
Table 2.
Baseline and 12-month WOMAC and SF-36 scores stratified by baseline WOMAC function score
| Overall | Highest (best) tertile | Medium tertile | Lowest (worst) tertile | Unadjusted P | Adjusted Pa | |
|---|---|---|---|---|---|---|
| WOMAC function scores | ||||||
| Baseline WOMAC function | 97; 33.6 (23.3) | 33; 60.5 (15.0) | 32; 29.2 (7.4) | 32; 10.1 (5.9) | ||
| Follow-up WOMAC function | 94; 86.5 (13.1) | 32; 90.0 (11.8) | 30; 83.0 (14.8) | 32; 86.2 (11.9) | 0.089 | 0.051 |
| Change in WOMAC function | 94; 53.3 (26.0) | 32; 29.2 (19.5) | 30; 54.5 (17.5) | 32; 76.2 (14.9) | <0.001 | <0.001 |
| SF-36 physical function scores | ||||||
| Baseline SF-36 physical function | 94; 15.5 (17.4) | 32; 27.2 (22.8) | 30; 11.2 (10.8) | 32; 7.7 (7.4) | ||
| Follow-up SF-36 physical function | 91; 72.1 (20.4) | 32; 77.7 (17.0) | 29; 65.0 (21.4) | 30; 73.1 (21.2) | 0.053 | 0.043 |
| Change in SF-36 physical function | 88; 56.7 (24.3) | 31; 49.3 (22.5) | 27; 55.9 (24.6) | 30; 65.1 (23.9) | 0.047 | 0.108 |
| WOMAC pain score | ||||||
| Baseline WOMAC pain | 91; 37.0 (22.0) | 30; 55.2 (19.6) | 30; 37.0 (14.4) | 31; 19.5 (15.4) | ||
| Follow-up WOMAC pain | 93; 85.0 (17.5) | 32; 88.9 (12.9) | 30; 80.2 (22.3) | 31; 85.6 (15.8) | 0.114 | 0.150 |
| Change in WOMAC pain | 87; 47.8 (31.0) | 29; 33.4 (24.8) | 28; 42.6c (33.2) | 30; 66.7 (25.0) | <0.001 | 0.001 |
| WOMAC stiffness scores | ||||||
| Baseline WOMAC stiffness | 92; 35.3 (26.2) | 31; 55.2 (20.6) | 31; 35.1 (24.5) | 30; 15.0 (15.5) | ||
| Follow-up WOMAC stiffness | 94; 83.8 (19.9) | 33; 85.6 (16.6) | 29; 80.2 (25.3) | 32; 85.2 (17.5) | 0.472 | 0.374 |
| Change in WOMAC stiffness | 89; 47.9 (33.9) | 31; 30.6a (26.0) | 28; 42.9b (35.9) | 30; 70.4 (26.8) | <0.001 | <0.001 |
| SF-36 mental health scores | ||||||
| Baseline SF-36 mental health | 97; 75.0 (16.6) | 33; 74.7 (15.2) | 32; 72.0 (15.0) | 32; 78.3 (19.2) | ||
| Follow-up SF-36 mental health | 93; 81.5 (18.8) | 31; 81.3 (17.8) | 32; 78.5 (21.2) | 30; 85.1 (17.1) | 0.456 | 0.165 |
| Change in SF-36 mental health | 93; 6.5 (21.3) | 31; 7.4 (25.2) | 32; 6.5 (19.5) | 30; 5.7 (19.3) | 0.973 | 0.753 |
Values are n; mean (s.d.) unless otherwise stated. Significant pairwise comparisons from adjusted analysis were found in change in WOMAC function (all comparisons), change in WOMAC pain (H vs L; M vs L) and change in WOMAC stiffness (H vs L; M vs L). aAdjusted for sex, education, procedure (unilateral vs bilateral) and joint (hip vs knee).
Association between preoperative function group and outcomes
Unadjusted analysis
When broken into tertiles based on preoperative WOMAC function scores, the highest functioning tertile had a mean score of 60.5 (range 43–94), the middle tertile had a mean score of 29.2 (range 19–42) and the lowest tertile had a mean score of 10.1 (range 0–18). When each tertile’s 1-year follow-up scores were compared with their corresponding preoperative scores, the lowest functioning tertile made the greatest WOMAC function gains (mean improvement = 76.2, s.d. = 14.9) when compared with the middle (mean = 54.5, s.d. = 17.5) and highest functioning tertiles (mean = 29.2, s.d. = 19.5) (P < 0.001). Significant pairwise differences were found between all groups (data not shown, only the adjusted pairwise comparisons are displayed in Table 2). SF-36 function scores (P = 0.047), WOMAC pain (P < 0.001) and WOMAC stiffness (P < 0.001) all show similar patterns in which the lowest tertile groups improved more than the highest tertile groups. There was no significant difference in improvement patterns in SF-36 mental health scores between the tertiles (P = 0.973) (Table 2).
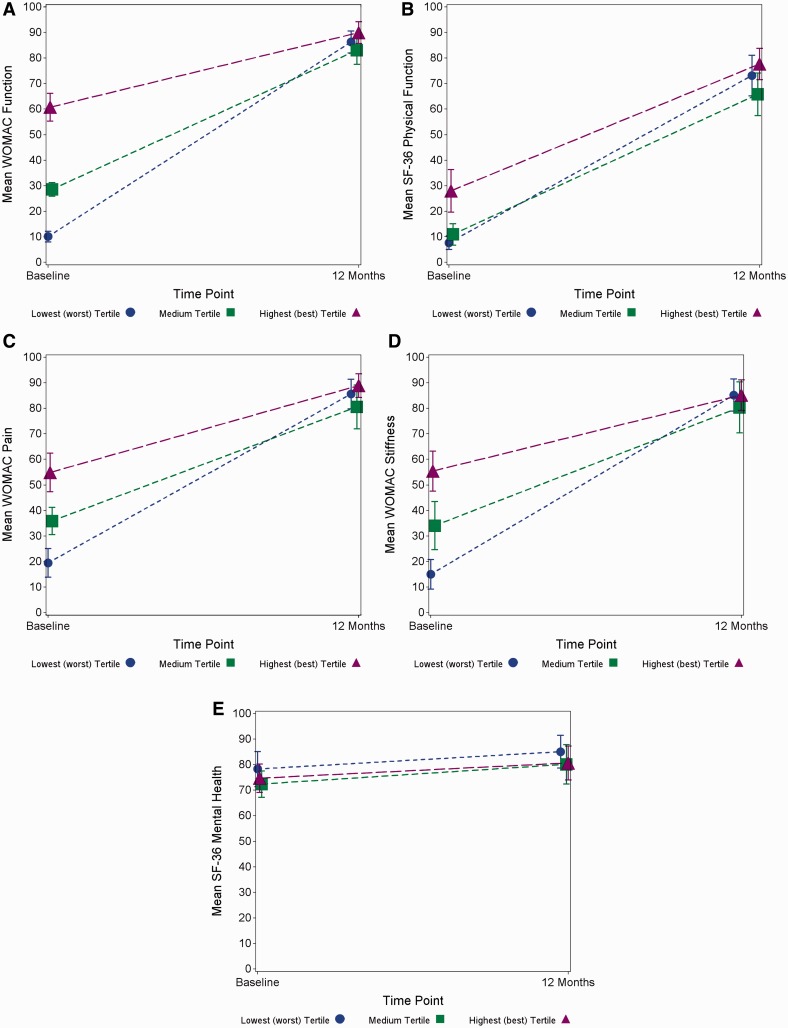
There was no difference in 1-year follow-up scores between the patients in the lowest tertile of preoperative function scores and those in the highest tertile (P = 0.089, Fig. 1A). Similarly, the three groups did not differ in 1-year SF-36 physical function score (P = 0.053, Fig. 1B), WOMAC pain score (P = 0.114, Fig. 1C), WOMAC stiffness score (P = 0.472, Fig. 1D) or SF-36 mental health (P = 0.456, Fig. 1E).
Fig. 1.
Baseline and 12-month WOMAC and SF-36 scores with 95% CI, stratified by baseline WOMAC function score.
Each line represents a different group: blue dots are patients in the lowest (worst) baseline WOMAC function tertile; green squares are patients in the medium baseline WOMAC function tertile; purple triangles are patients in the highest (best) baseline WOMAC function tertile. The x-axis has the two time points: baseline and 12 months. The y-axis has the mean outcome measured at each time point. Each symbol represents the mean outcome score for that particular group at that time point, with a 95% CI. (A) WOMAC function scores. Mean WOMAC function is the outcome and is along the y-axis. (B) SF-36 physical function scores. Mean SF-36 physical function is the outcome and is along the y-axis. (C) WOMAC pain scores. Mean WOMAC pain score is the outcome and is along the y-axis. (D) WOMAC stiffness scores. Mean WOMAC stiffness is the outcome and is along the y-axis. (E) SF-36 mental health scores. Mean SF-36 mental health is the outcome and is along the y-axis.
Multivariable analysis
There was little change in the statistical significance observed between the tertiles in the univariate analyses and in a multivariate analyses that adjusted for sex, education, procedure (unilateral vs bilateral) and joint (knee vs hip; Table 2).
Discussion
In this study, we investigated patterns between preoperative WOMAC and SF-36 function scores and 12-month functional outcomes in patients undergoing TJR in the Dominican Republic. Patients with the worst preoperative WOMAC function scores improved more than those with the best preoperative scores, which is consistent with observations made in developed countries [12, 13]. We also observed that each tertile had similar outcomes at 12-month follow-up, contrasting with patterns seen in developed countries [12, 13] and suggesting that a low baseline WOMAC function score did not compromise the TJR outcome.
Our first finding, that the lowest-scoring preoperative tertile improves more than the highest-scoring preoperative tertile, is consistent with a large study that included patients from three developed countries: the USA, the UK and Australia [13]. Our second finding, that all tertiles have similar outcomes at 12-month follow-up, contrasts with observations from developed countries, which have shown that patients with lower preoperative WOMAC function scores have worse functional outcomes at 12-month follow-up than patients who start at a higher baseline functional level [12, 13]. It should be noted that our cohort’s mean baseline WOMAC function score (33.6) was lower than the mean baseline WOMAC function scores observed in cohorts from developed countries, which ranged from 42.3 [13] to 54.0 [12]. Since lower baseline scores are typically associated with greater gains [12, 13], this baseline difference in WOMAC function scores could explain our cohorts’ relatively large improvements. Our observation that Dominican patients with very low preoperative WOMAC scores nevertheless attain good postoperative scores is not observed in joint replacement cohorts from other countries, but the reason for this difference is not clear.
One potential explanation may be due to differences in patients’ motivation to improve after surgery. The Dominican patients are notably enthusiastic and highly motivated to regain function following surgery. It is known that living alone leads to worse functional outcomes [11], but a relatively high percentage of our patients live with friends or family members (Table 1), so this demographic difference may lead to our patients’ large improvements. Due to the level of complexity of TJR and the limited resource context in which the Op-Walk team works, the Dominican patients are screened carefully before being accepted into the programme. Therefore there may also be selection bias for patients who have better overall health, which may lead to greater improvement following surgery. Finally, patients’ average age (60.9) is almost 10 years less than the average age (70.7) of the combined cohorts used in the literature from developed countries. Although age did not seem to be a confounder in our study, it was noted that higher age predicts lower SF-36 functional scores at 2-year follow-up [13] and worse postoperative function [11], so it is possible that our patients’ younger age helps them to achieve better outcomes, regardless of their baseline status. Additional research is required to more rigorously test these hypotheses.
Regardless of the reasons for the observed difference, our study suggests that in developing countries, operating on patients at a lower level of functional status may not compromise their end result. Although this practice would increase patients’ period of arthritis-associated disability, a policy of waiting longer to operate will optimize the amount of improvement patients experience from TJR without threatening the functional outcome. This information may be especially important to policymakers from developing countries, as it will allow them to thoughtfully allocate their countries’ limited resources.
Our study is limited because it only examines patient outcomes from the Dominican Republic. Additional work is needed to see if the observed pattern occurs in other developing countries. The small sample size (97) and low proportion of subjects who received hip replacement also limit the scope of inferences permitted by our data. For example, a larger sample would have supported analysis of quartiles instead of tertiles, providing a richer comparison. Our work suggests, however, that surgical patterns observed in developed countries vary from patterns observed in developing countries. With medical mission trips growing in prevalence, it will become increasingly important for mission groups to track their outcomes and to have dedicated research teams that analyse outcomes data to see if country- or region-specific variations in patients’ surgical indicators and surgical outcomes exist. Better understanding these differences may have important policy implications for developing health care systems and the mission groups that work in these countries.
Rheumatology key messages.
This is the first study to investigate improvement patterns following joint replacement in a developing country.
Improvement patterns following joint replacement in the Dominican Republic vary from patterns observed in developed countries.
Funding: This work was supported by the American College of Rheumatology Research and Education Foundation, Harvard Medical School, National Institutes of Health (T32 AR 055885, P60 AR47782), Department of Orthopedic Surgery and Brigham and Women’s Hospital.
Disclosure statement: The authors have declared no conflicts of interest.
Supplementary data
Supplementary data are available at Rheumatology Online.
References
- 1.Brooks PM. The burden of musculoskeletal disease—a global perspective. Clin Rheumatol. 2006;25:778–81. doi: 10.1007/s10067-006-0240-3. [DOI] [PubMed] [Google Scholar]
- 2.Hawker G, Wright J, Coyte P, et al. Health-related quality of life after knee replacement. J Bone Joint Surg Am. 1998;80:163–73. doi: 10.2106/00004623-199802000-00003. [DOI] [PubMed] [Google Scholar]
- 3.Heck DA, Robinson RL, Partridge CM, et al. Patient outcomes after knee replacement. Clin Orthop Relat Res. 1998;356:93–110. doi: 10.1097/00003086-199811000-00015. [DOI] [PubMed] [Google Scholar]
- 4.Higashi H, Barendregt JJ. Cost-effectiveness of total hip and knee replacements for the Australian population with osteoarthritis: discrete-event simulation model. PLoS One. 2011;6:e25403. doi: 10.1371/journal.pone.0025403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Losina E, Walensky RP, Kessler CL, et al. Cost-effectiveness of total knee arthroplasty in the United States: patient risk and hospital volume. Arch Intern Med. 2009;169:1113–21. doi: 10.1001/archinternmed.2009.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lubega N, Mkandawire NC, Sibande GC, et al. Joint replacement in Malawi: establishment of a National Joint Registry. J Bone Joint Surg Br. 2009;91:341–3. doi: 10.1302/0301-620X.91B3.21706. [DOI] [PubMed] [Google Scholar]
- 7.DeCamp M. Scrutinizing global short-term medical outreach. Hastings Cent Rep. 2007;37:21–2. doi: 10.1353/hcr.2007.0096. [DOI] [PubMed] [Google Scholar]
- 8.Eberlin KR, Zaleski KL, Snyder HD, et al. Quality assurance guidelines for surgical outreach programs: a 20-year experience. Cleft Palate Craniofac J. 2008;45:246–55. doi: 10.1597/07-094.1. [DOI] [PubMed] [Google Scholar]
- 9.Sykes KJ, Le PT, Sale KA, et al. A 7-year review of the safety of tonsillectomy during short-term medical mission trips. Otolaryngol Head Neck Surg. 2012;146:752–6. doi: 10.1177/0194599812437317. [DOI] [PubMed] [Google Scholar]
- 10.Benroth R, Gawande S. Patient-reported health status in total joint replacement. J Arthroplasty. 1999;14:576–80. doi: 10.1016/s0883-5403(99)90080-3. [DOI] [PubMed] [Google Scholar]
- 11.Braeken A, Lochhass-Gerlach J, Gollish J, et al. Determinants of 6–12 month postoperative functional status and pain after elective total hip replacement. Int J Qual Health Care. 1997;9:413–8. doi: 10.1093/intqhc/9.6.413. [DOI] [PubMed] [Google Scholar]
- 12.Fortin PR, Penrod JR, Clarke AE, et al. Timing of total joint replacement affects clinical outcomes among patients with osteoarthritis of the hip or knee. Arthritis Rheum. 2002;46:3327–30. doi: 10.1002/art.10631. [DOI] [PubMed] [Google Scholar]
- 13.Lingard EA, Katz JN, Wright EA, et al. Predicting the outcome of total knee arthroplasty. J Bone Joint Surg Am. 2004;86-A:2179–86. doi: 10.2106/00004623-200410000-00008. [DOI] [PubMed] [Google Scholar]
- 14.Niu NN, Collins JE, Thornhill TS, et al. Pre-operative status and quality of life following total joint replacement in a developing country: a prospective pilot study. Open Ortho J. 2011;5:307–14. doi: 10.2174/1874325001105010307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Dominican Republic. Pan American Health Organization, World Health Organization. http://www.paho.org/English/DD/AIS/cp_214.htm (16 April 2013, date last accessed)
- 16.Batlle-Gualda E, Esteve-Vives J, Piera MC, et al. Adaptación transcultural del cuestionario womac específico para artrosis de rodilla y cadera. Rev Esp Reumatol. 1999;26:38–45. [Google Scholar]
- 17.Alonso J. Cuestionario de salud sf-36. Barcelona, Spain, 1999. http://www.chime.ucla.edu/measurement/SF-36%20Spain.pdf (1 November 2009, date last accessed) [Google Scholar]
- 18.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–83. [PubMed] [Google Scholar]
- 19.Bellamy N, Buchanan WW, Goldsmith CH, et al. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833–40. [PubMed] [Google Scholar]
- 20.Bellamy N. WOMAC osteoarthritis index: a user's guide. London, ON, Canada: University of Western Ontario; 1995. [Google Scholar]
- 21.Fortin PR, Clarke AE, Joseph L, et al. Outcomes of total hip and knee replacement: preoperative functional status predicts outcomes at six months after surgery. Arthritis Rheum. 1999;42:1722–8. doi: 10.1002/1529-0131(199908)42:8<1722::AID-ANR22>3.0.CO;2-R. [DOI] [PubMed] [Google Scholar]
- 22.Katz JN, Phillips CB, Baron JA, et al. Association of hospital and surgeon volume of total hip replacement with functional status and satisfaction three years following surgery. Arthritis Rheum. 2003;48:560–8. doi: 10.1002/art.10754. [DOI] [PubMed] [Google Scholar]
- 23.Nunnally JC. Psychometric theory. 2nd edn. New York: McGraw-Hill; 1978. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.