Abstract
The preschool years offer an opportunity to interrupt the trajectory toward obesity in black children. The Hip-Hop to Health Jr. Obesity Prevention Effectiveness Trial was a group-randomized controlled trial assessing the feasibility and effectiveness of a teacher-delivered weight control intervention for black preschool children. The 618 participating children were enrolled in 18 schools administered by the Chicago Public Schools. Children enrolled in the 9 schools randomized to the intervention group received a 14-week weight control intervention delivered by their classroom teachers. Children in the 9 control schools received a general health intervention. Height and weight, physical activity, screen time, and diet data were collected at baseline and post-intervention. At post-intervention, children in the intervention schools engaged in more moderate-to vigorous physical activity than children in the control schools (difference between adjusted group means=7.46 min/day, p=.02). Also, children in the intervention group had less total screen time (−27.8 min/day, p=.05). There were no significant differences in BMI, BMI Z score, or dietary intake.
It is feasible to adapt an obesity prevention program to be taught by classroom teachers. The intervention showed positive influences on physical activity and screen time, but not diet. Measuring diet and physical activity in preschool children remains a challenge, and interventions delivered by classroom teachers require both intensive initial training and ongoing individualized supervision.
Keywords: childhood obesity, prevention, minorities, diet, physical activity
INTRODUCTION
Obesity is a potentially debilitating condition, and many obesity-related risk factors and diseases are strikingly apparent in minority populations. (1) An expert committee convened by the American Medical Association (2) recommended defining obesity in children as a body mass index (BMI) at or above the 95th percentile for age and sex. (3) Using this definition, for non-Hispanic black children, 11.4% of 2-5 year olds, 19.4% of 6-11 year olds, and 24.4% of 12-19 year olds were obese in 2007-2008. (4) Therefore, the preschool years may represent a crucial time for interventions designed to alter the trajectory toward obesity in black children.
The Hip-Hop to Health Jr. Obesity Prevention Effectiveness Trial builds on the results of a successful efficacy trial, Hip-Hop to Health Jr. (5-7) In that study, specially trained early childhood educators visited preschools and taught either a 14-week nutrition and physical activity intervention or a general health intervention. Results showed that children in the intervention group had significantly smaller increases in BMI than children in the control group at Year 1 and Year 2 follow-up. (7) However, an intervention taught by visiting educators is potentially difficult to disseminate. Therefore, we designed a similar intervention that could be integrated into the everyday preschool curriculum and delivered by classroom teachers. The primary aim of this study is to compare BMI and BMI Z score changes in the intervention and control groups one year after the intervention. Secondary aims include comparing physical activity, screen time, and diet in the two groups at the post-intervention visit and at the 1-year follow-up visit. Analyses for the primary outcome are in progress. This article describes the study design, characteristics of the participants at baseline, feasibility of teacher training and session completion, and changes in BMI, physical activity, screen time and diet at the post-intervention visit.
METHODS AND PROCEDURES
Design and Setting
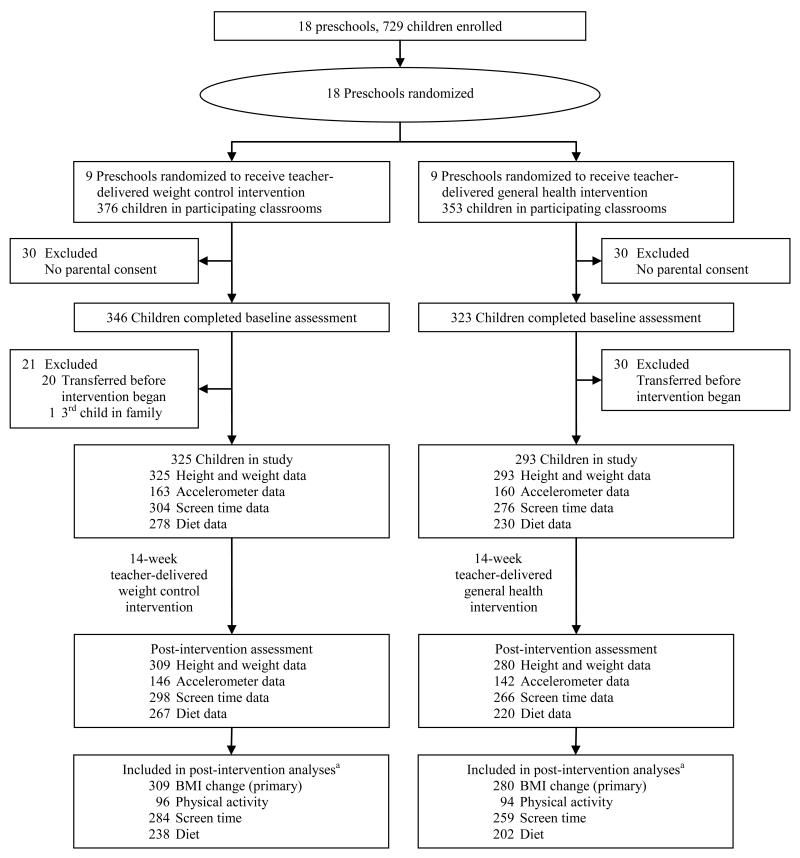
The Hip-Hop to Health Jr. Obesity Prevention Effectiveness Trial is a randomized controlled intervention trial that targets 3-5 year old children enrolled in 18 Head Start programs administered through the Chicago Public Schools. The Institutional Review Boards at the University of Illinois at Chicago and the Chicago Public Schools approved this study. Eighteen schools were randomly assigned to a teacher-delivered weight control intervention group (TD-WCI) or a teacher-delivered general health intervention control group (TD-GHI). The study design through the post-intervention visit is shown in Figure 1.
Figure 1.
Recruitment, enrollment, and retention through the post-intervention visit, Hip-Hop to Health Jr. Obesity Prevention Effectiveness Trial
aOnly children with valid data for the relevant variables at baseline and post-intervention were included in post-intervention analyses (BMI change, physical activity, screen time, and diet)
Eligibility
Since the interventions were conducted during regular class time, all children in the participating classrooms received one of the interventions. However, data were only collected from children whose parent or guardian provided informed consent. The classroom teachers who participated also gave informed consent. Up to 2 children per family were eligible to participate.
Theoretical Framework
The conceptual framework guiding the development and delivery of the intervention was based on Social Cognitive Theory (SCT) (8) and self-determination theory (9) For both nutrition and physical activity, social cognitive theory suggests that modeling helps children try new foods as well as engage in new activities. Past research has shown that children are more apt to eat new foods if they see an adult model eating the food, (10) and children who are repeatedly exposed to new foods are more likely to increase their consumption of those foods. (11) Also, parents who are active are more apt to have children who are active. (12) Self-determination theory distinguishes between behaviors that an individual performs freely and those that an individual feels coerced to do. (13)
Interventions
Teacher Training
The participating teachers and teachers’ aides attended an initial training session. For both the TD-WCI and the TD-GHI groups, the initial training sessions were three hours long. Following the first formal session, the intervention coordinator conducted 3 in-school training sessions for the intervention teachers and 1 in-school session for the control teachers. Over the course of the 14-week intervention, the intervention coordinator met on an individual basis weekly with each teacher/teacher aide in the TD-WCI group and monthly with each teacher/teacher aide in the TD-GHI group.
TD-WCI
A full description of the WCI on which the TD-WCI was based is provided elsewhere. (5) Briefly, the curriculum is 14 weeks in length, with two sessions each week. In the efficacy trial, the intervention was delivered three times per week. However, in response to teacher feedback regarding scheduling, we adapted the curriculum so that teachers were asked to teach two weekly sessions, with the option of including a third session if they chose. Each week focused on a particular theme with a specific objective (see Table 1). Each session included a 20-minute lesson related to healthy eating and exercise, as well as a 20-minute physical activity component. Lessons featured the colorful “Pyramid Puppets” that represent the seven food groups of the food pyramid. In addition, the intervention incorporated songs and raps that were included on a CD for teachers to play for their students. The CD also included two fully scripted exercise routines.
Table 1.
Weekly themes for weight control intervention, Teacher-Delivered Hip-Hop to Health
| Week | Lesson | Week | Lesson |
|---|---|---|---|
| 1 | Go, Grow vs. Slow Foods | 8 | Protein |
| 2 | Food Pyramid | 9 | Heart Healthy Exercise |
| 3 | Portions | 10 | Instead of TV, I Could… |
| 4 | Grains | 11 | Healthy Snacks |
| 5 | Fruits | 12 | Five a Day |
| 6 | Vegetables | 13 | Review |
| 7 | Milk--Switching to 1% | 14 | Healthy Me |
Parents in the TD-WCI classrooms received a weekly newsletter that paralleled the children’s curriculum in content and included a homework assignment. Parents received $5 for each of the homework assignments that they completed and returned. Each parent also received the same CD that the teacher used in the classroom so that the nutrition concepts and importance of physical activity could be reinforced in the home.
TD-GHI
The TD-GHI was based on the control intervention used in the efficacy trial. It was 14 weeks long and taught once per week. The children learned a variety of health concepts, including car seat and seat belt safety, immunizations, dental health, and the procedures for calling 911. Parents received a weekly newsletter that mirrored the weekly theme of the school-based curriculum but were not asked to complete homework assignments.
Cultural Adaptations
In our original WCI and in the current TD-WCI, we targeted six areas related to cultural practices and beliefs: food, family, music, community, social roles and relationships. Cultural considerations included targeting culturally relevant foods and augmenting traditional recipes to be low-fat; including family members through the parent newsletters; using culturally relevant music and dance; addressing cognitive (knowledge and attitudes) and environmental (social support, unsafe neighborhoods, economic restrictions, conflicting responsibilities) barriers to regular physical activity and healthful eating, and facilitating social support and self-efficacy in making changes in diet and physical activity.
Measures
All questionnaires were administered by trained interviewers. Because of the study design, both parents and interviewers were aware of group assignments.
Sociodemographic Variables
At baseline, parents completed a sociodemographic questionnaire.
Anthropometric Variables
Children’s height and weight were measured at baseline and post-intervention. Parents’ height was measured at baseline, and weight was measured at baseline and post-intervention. Height was measured using a Seca 214 portable stadiometer (Seca, Hanover, MD). Weight was measured using a Tanita BWB-800 digital scale (Tanita Corporation of America, Inc., Arlington Heights, IL). Participants removed their shoes and any heavy outer clothing for the anthropometric measurements. Both height and weight were measured twice, to the nearest 0.1 cm and 0.1 kg respectively. If the two height measurements were more than 0.5 cm apart or if the two weight measurements were more than 0.2 kg apart, a third measurement was taken. The mean of the two closest measurements was used for analysis. BMI was computed from height and weight. BMI Z scores and BMI percentiles for age and sex were calculated for each child based on the 2000 Centers for Disease Control and Prevention (CDC) Growth Charts, (3) using a SAS program provided by the CDC. [http://www.cdc.gov/nccdphp/dnpao/growthcharts/resources/sas.htm. Accessed 7/22/2010.]
Physical Activity
The ActiGraph GT1M activity monitor (ActiGraph, Pensacola, FL) was used to measure the children’s physical activity at baseline and post-intervention. The ActiGraph is a small, lightweight uniaxial accelerometer designed to detect normal body motion and filter out motion from other sources. The acceleration signal is sampled 30 times per second, and signals are summed at the end of a specified period (15 seconds for this study) and stored in non-volatile flash memory. Children were asked to wear the ActiGraph on a belt around the waist during waking hours for seven days. Study staff called the parents each morning during the 7-day period to remind them to place the accelerometer on the child and to answer any questions or concerns.
Activity counts were downloaded from the accelerometers using ActiLife GT1M software (ActiGraph, Pensacola, FL), and the resulting text files were read and analyzed using SAS for Windows v 9.1 (SAS Institute Inc., Cary, NC). For each day in the record, the amount of time the accelerometer was actually worn was estimated. Time not worn was defined as at least 60 minutes with 0 activity counts, allowing for interruptions of up to 2 consecutive minutes with counts ≤ 100. (14) Only days with at least 8 hours of wear were included in the main analyses, and participants with fewer than 4 valid days were excluded. Time spent in moderate, vigorous, and moderate-to-vigorous physical activity (MVPA) was calculated using count thresholds from a calibration study conducted with preschool children. (15) The threshold for moderate activity was 420 counts/15 seconds, equivalent to oxygen consumption (VO2) of 20 mL/kg per min, and the threshold for vigorous activity was 842 counts/15 seconds, equivalent to VO2 = 30 mL/kg per min. Minutes of MVPA, moderate activity, and vigorous activity were calculated for each day, then averaged across all of the child’s valid days. In addition, the total number of minutes of MVPA in each record was divided by the total hours worn to calculate mean minutes of MVPA per hour worn for each child. Finally, for an estimate of activity independent of any particular calibration equation, the total number of accelerometer counts measured was divided by the total number of minutes worn on valid days to calculate mean counts per minute.
Television Viewing and Screen Time
At baseline and post-intervention, parents were asked to report the amount of time their child spent watching television (broadcast, cable, or satellite), watching DVDs or videotapes, playing video games, or using a computer on an average school day and on an average weekend day. (16) Parents were also asked how much time they spent in each of these activities on an average weekday and an average weekend day. Time spent watching television and total screen time in minutes/day were calculated using a weighted average of time spent on school days or weekdays and weekend days.
Dietary Intake
A single 24-hour diet record was collected for each child at baseline and post-intervention, using a combination of in-school observations and food records or recalls completed by the parent.
Meal Observation at Preschool
Breakfast, lunch, and a snack were served family-style in the preschool classrooms each day. Research staff unobtrusively documented the amount of food served to and consumed by 3-5 children/classroom each day over a 3-5 day period at each school. All leftover food remaining on the trays was labeled and measured with utensils and a digital ounce/gram scale that was calibrated daily prior to each use. The amount of food/beverages eaten by each child was determined by calculating the difference between the amount of food served and the amount discarded.
Foods Consumed Outside of Preschool
The day before a child was to be observed, the child’s parent/guardian was given a packet containing a food record form for recording meals and snacks consumed outside of school, a food portion visual guide to assist in estimating the amount of food eaten, and a product identification notebook. The parents were asked to record all food and drinks consumed by the child outside of school that afternoon/evening and the following morning prior to school. On the morning that the child was observed, this record was collected and reviewed by the research staff for completeness. A single day’s classroom observation plus the parent’s record or recall represented 24 hours of nutrient intake. The dietary intake data were processed using the Nutrition Data System for Research (NDS-R, Nutrition Coordinating Center, University of Minnesota). The food group variables created by NDS-R were used to calculate consumption of fruit, 100% fruit juice, and vegetables. The fruit variable includes citrus and non-citrus fruits and excludes juices, avocado, fried fruits, and fruit-based savory snacks. The vegetable variable includes dark green and deep yellow vegetables, tomatoes, white potatoes and other starchy vegetables, legumes, and other vegetables, and excludes fried potatoes, other fried vegetables, and vegetable juice.
Teacher Lesson Completion
Along with the intervention materials, teachers were given 14 lesson completion forms, which they were asked to fill out each week. Teachers reported whether each nutrition and physical activity lesson was completed, partially done, or not done, and they reported whether the Hip-Hop to Health CD was used for the physical activity lesson. The lesson completion forms were collected at the end of the intervention.
Statistical Analyses
Differences in baseline characteristics between the intervention and control groups and between participants with and without valid data for physical activity or diet were tested for significance using the Wilcoxon rank sum test for income, t-tests for all other continuous variables, and chi-square tests for categorical variables. Chi-square tests were used to test for differences between schools and between intervention groups in the proportion of children with valid baseline and post-intervention data. Pearson and Spearman correlation coefficients were used to test for associations between BMI and other variables, and t-tests were used to test for differences between obese and non-obese children. To test for differences between groups in BMI and BMI Z score change at post-intervention, we used both mixed-model analysis of variance, controlling for school and classroom nested within school, and mixed model analysis of covariance, controlling for school, classroom nested within school, the baseline value, and baseline age. Change from baseline to post-intervention was the dependent variable. We used mixed-model analysis of covariance to test for differences between groups in physical activity, screen time, and diet at post-intervention, controlling for school, classroom nested within school, the baseline value, and baseline age. For these analyses, the post-intervention value was the dependent variable. Because only 17 of the 18 schools participated in diet data collection, test statistics for the diet analyses had 15 degrees of freedom, while test statistics for the BMI change, physical activity and screen time analyses had 16 degrees of freedom. (17) Only participants with height and weight measurements, valid accelerometer records, complete screen time data, or valid diet data at baseline and post-intervention were included in the post-intervention analyses. All analyses were conducted using SAS version 9.1 (SAS Institute Inc., Cary, NC).
RESULTS
Baseline Data
As shown in Figure 1, there were 729 students enrolled in the 18 participating preschools during baseline data collection. Baseline data were collected for the 669 children (92%) whose parents signed consent forms allowing them to participate in the study. However, 50 of these children were excluded from the study because they transferred out of the participating schools before the intervention began, and one child was excluded because he was the third child in a participating family. A total of 618 children and 590 parents and guardians participated in the study; 28 parents had 2 children participating.
There were 323 children with valid accelerometer records at baseline. Of the 295 children who did not have a valid record, 114 did not wear an accelerometer, usually because their parents could not be reached on the day before the accelerometers were distributed. Fifteen children lost their accelerometers, and 7 switched with another child during the data collection period. Data from 34 accelerometers were lost due to equipment malfunctions, generally battery interruptions, and data from 3 were lost due to operator error. An additional 122 children had accelerometer records that were not valid by our definition, at least 4 days with at least 8 hours of wear per day. There were 580 children with screen time data at baseline. Screen time data were missing for children whose parents did not complete the baseline interview. There were 508 children with valid diet records at baseline. Diet data were not collected at one school (N=33) because school personnel were concerned that the in-school diet observations would be disruptive. The parents of 67 children could not be reached for the diet recall. Two records were excluded because the child’s in-school intake was not observed, and 8 were excluded because insufficient information was provided during the diet recall to complete the record.
Intervention and Control Group Comparability at Baseline
Characteristics of the participating children at baseline are shown in Table 2. There were no significant differences between groups in gender, BMI, or BMI Z score at baseline. Children in the intervention group were significantly younger than children in the control group at baseline (mean of 50.7 months vs. 51.9 months, p=.03). They also weighed less (p=.03) and were shorter (p=.02), but these differences were no longer significant when adjusted for age.
Table 2.
Characteristics of participating children at baseline, Teacher-Delivered Hip-Hop to Health
| Intervention | Control | All | ||||
|---|---|---|---|---|---|---|
| N | Mean (SD) |
N | Mean (SD) |
N | Mean (SD) |
|
| Female, no. (%) | 325 | 168 (52%) | 293 | 161 (55%) | 618 | 329 (53%) |
| Race, no. (%) | 325 | 293 | 618 | |||
| Black | 314 (97%) | 266 (91%) | 580 (94%) | |||
| Latino | 4 (1%) | 14 (5%) | 18 (3%) | |||
| Multiracial/other | 7 (2%) | 13 (4%) | 20 (3%) | |||
| Age, months | 325 | 50.7 (6.8) | 293 | 51.9 (6.3) | 618 | 51.3 (6.6) |
| BMI, kg/m2 | 325 | 16.5 (1.6) | 293 | 16.6 (2.2) | 618 | 16.6 (1.9) |
| BMI Z score for age and sex |
325 | 0.6 (1.0) | 293 | 0.7 (1.1) | 618 | 0.6 (1.0) |
| BMI percentile for age and sex, no. (%) |
325 | 293 | 618 | |||
| < 5th | 2 (1%) | 4 (1%) | 6 (1%) | |||
| 5th – < 85th | 216 (66%) | 189 (65%) | 405 (66%) | |||
| 85th – < 95th | 62 (19%) | 63 (22%) | 125 (20%) | |||
| 95th – < 99th | 34 (10%) | 21 (7%) | 55 (9%) | |||
| ≥ 99th | 11 (3%) | 16 (5%) | 27 (4%) | |||
| Weight, kg | 325 | 18.1 (3.0) | 293 | 18.7 (3.8) | 618 | 18.4 (3.5) |
| Height, cm | 325 | 104.7 (6.0) | 293 | 105.8 (5.7) | 618 | 105.2 (5.9) |
| MVPA, min/day | 163 | 98.6 (30.2) | 160 | 98.8 (26.0) | 323 | 98.7 (28.1) |
| Counts/min | 163 | 625 (160) | 160 | 631 (148) | 323 | 628 (154) |
| TV viewing, hr/day | 304 | 2.8 (1.6) | 277 | 2.7 (1.7) | 581 | 2.7 (1.7) |
| Screen timea, hr/day | 304 | 5.2 (2.8) | 276 | 4.7 (2.7) | 580 | 4.9 (2.8) |
| Energy, kcal | 278 | 1620 (548) | 230 | 1503 (479) | 508 | 1567 (521) |
| Total fat, % kcal | 278 | 32.6 (7.0) | 230 | 32.7 (6.5) | 508 | 32.7 (6.7) |
| Fruitb, servings/day | 278 | 0.9 (0.9) | 230 | 1.0 (0.9) | 508 | 1.0 (0.9) |
| 100% fruit juice, servings/day |
278 | 1.4 (1.6) | 230 | 1.2 (1.4) | 508 | 1.3 (1.5) |
| Vegetablesc, servings/day |
278 | 1.2 (1.2) | 230 | 1.1 (1.1) | 508 | 1.2 (1.1) |
SD, standard deviation; BMI, body mass index; MVPA, moderate-to-vigorous physical activity.
Time spent watching television, DVDs or videos, playing video games, or using a computer.
Excludes juices, avocado, fried fruits, and fruit-based savory snacks.
Includes dark green and deep yellow vegetables, tomatoes, white potatoes and other starchy vegetables, legumes, and other vegetables; excludes fried potatoes, other fried vegetables, and vegetable juice.
There were no significant differences between groups in physical activity at baseline for the 323 children with valid accelerometer records at baseline or for the 190 children with valid accelerometer records at baseline and post-intervention. There was no significant difference between groups in time spent watching television at baseline, but children in the intervention group had more total screen time per day (time spent watching television, DVDs or videos, playing video games, or using a computer) than children in the control group (p=.01). This was also true for the 543 children with screen time data at baseline and post-intervention; there was not a significant difference in television viewing time, but the intervention group had more total screen time than the control group: mean (SD) = 5.2 (2.8) hr vs. 4.7 (2.7) hr, p=.03.
There were no differences between groups at baseline in consumption of fat (% kcal), fruit, 100% fruit juice, or vegetables. However, energy intake was higher (p=.01) and fiber intake was lower (p=.05) in the intervention group than in the control group at baseline. Among the 440 children with valid diet records at baseline and post-intervention, there was a significant difference between groups in energy intake (mean (SD) = 1597 (511) kcal in the intervention group and 1493 (490) kcal in the control group, p=.03), but no significant differences between groups in fat, fiber, fruit, 100% fruit juice, or vegetable consumption.
Characteristics of parents and guardians at baseline are shown in Table 3. The child’s mother was usually the participating parent (83%). There was no difference between groups at baseline in parents’ gender, age, median income, marital status, full-time employment; BMI, weight, height, obesity prevalence, or hours/day spent watching television. Parents in the intervention group reported more children under 18 years in the house than parents in the control group (p=.02). Parents of children in the intervention group also had significantly fewer years of education (p=.005) and somewhat higher total screen time (p=.03) than parents of children in the control group.
Table 3.
Characteristics of participating adults at baseline, Teacher-Delivered Hip-Hop to Health
| Intervention | Control | All | ||||
|---|---|---|---|---|---|---|
| N | Mean (SD) | N | Mean (SD) | N | Mean (SD) | |
| Relationship to childa, no. (%) |
299 | 273 | 572 | |||
| Mother | 243 (81%) | 229 (84%) | 472 (83%) | |||
| Father | 28 (9%) | 22 (8%) | 50 (9%) | |||
| Grandparent | 13 (4%) | 13 (5%) | 26 (5%) | |||
| Other | 15 (5%) | 9 (3%) | 24 (4%) | |||
| Female, no. (%) | 307 | 275 (90%) | 283 | 258 (91%) | 590 | 533 (90%) |
| Age, years | 296 | 30.5 (8.9) | 273 | 31.3 (8.3) | 569 | 30.9 (8.6) |
| Education, years | 296 | 12.1 (1.5) | 272 | 12.5 (1.9) | 568 | 12.3 (1.7) |
| Income, $, median | 288 | 15,000 | 262 | 15,000 | 550 | 15,000 |
| Married or living with a partner, no. (%) |
297 | 60 (20%) | 273 | 63 (23%) | 570 | 123 (22%) |
| Employed full-time, no. (%) |
297 | 97 (33%) | 273 | 108 (40%) | 570 | 205 (36%) |
| Children <18 yrs in household |
297 | 2.9 (1.7) | 273 | 2.6 (1.5) | 570 | 2.8 (1.6) |
| Other adults in household |
297 | 1.1 (1.0) | 273 | 1.1 (1.0) | 570 | 1.1 (1.0) |
| BMI, kg/m2 | 208 | 31.7 (7.9) | 204 | 32.0 (8.7) | 412 | 31.9 (8.3) |
| Weight, kg | 208 | 86.8 (24.1) | 204 | 87.0 (25.6) | 412 | 86.9 (24.8) |
| Height, cm | 208 | 165.1 (8.0) | 204 | 164.6 (7.8) | 412 | 164.9 (7.9) |
| BMI categoriesb, no. (%) |
208 | 204 | 412 | |||
| Underweight | 3 (1%) | 2 (1%) | 5 (1%) | |||
| Normal weight | 41 (20%) | 48 (24%) | 89 (22%) | |||
| Overweight | 54 (26%) | 46 (23%) | 100 (24%) | |||
| Obesity Class I | 48 (23%) | 37 (18%) | 85 (21%) | |||
| Obesity Class II | 24 (12%) | 36 (18%) | 60 (15%) | |||
| Obesity Class III | 38 (18%) | 35 (17%) | 73 (18%) | |||
| Concerned about child becoming overweight, no. (%) |
289 | 267 | 556 | |||
| Unconcerned or slightly unconcerned |
94 (33%) | 105 (39%) | 199 (36%) | |||
| Neutral | 12 (4%) | 11 (4%) | 23 (4%) | |||
| Concerned or slightly concerned |
183 (63%) | 151 (57%) | 334 (60%) | |||
| TV viewing, hr/day | 289 | 3.3 (2.3) | 268 | 3.1 (2.4) | 557 | 3.2 (2.3) |
| Screen time, hr/dayc | 289 | 7.6 (4.3) | 268 | 6.8 (3.8) | 557 | 7.2 (4.1) |
SD, standard deviation; BMI, body mass index.
Only one child per family is included.
Underweight: < 18.5 kg/m2, normal weight: 18.5-<25 kg/m2, overweight: 25-<30 kg/m2, obesity class I: 30-<35 kg/m2, obesity class II: 35-<40 kg/m2, obesity class III: ≥ 40 kg/m2.
Time spent watching television, DVDs or videos, playing video games, or using a computer.
Associations with BMI at Baseline
Among participating children, baseline BMI and BMI Z score were associated with maternal BMI (BMI: r=.22, p<.001; BMI Z score: r=.25, p<.001; N=333 mothers). The children of obese mothers (BMI ≥ 30 kg/m2) were also more likely to be obese (BMI ≥ 95th percentile) than the children of non-obese mothers (20% vs. 9%, p=.009). Baseline BMI and BMI Z score were not associated with the child’s age, or with minutes of MVPA per day. Activity was not significantly different among obese and non-obese children. BMI and BMI Z score were also not associated with children’s television viewing or screen time, and television viewing and screen time were similar among obese and non-obese children. Finally, BMI and BMI Z score were not associated with the child’s energy, fat, fiber, fruit, 100% fruit juice, or vegetable consumption at baseline. The diet of obese children was not significantly different from the diet of non-obese children.
Teacher Lesson Completion
The TD-WCI curriculum consisted of 28 nutrition lessons and 28 exercise sessions (2 per week for 14 weeks). Teachers reported completing or partially completing a mean of 26.6 (SD=1.9) of the 28 nutrition lessons and 27.1 (1.7) of the 28 exercise sessions. Seven of the 18 teachers (39%) taught all of the nutrition lessons, and 10 (56%) of the teachers completed all of the exercise sessions. All teachers completed at least 21 of the nutrition and exercise lessons. The curriculum also included 14 optional lessons that teachers could use if time permitted. On average, teachers completed 8.8 (3.0) of the 14 optional nutrition lessons and 11.4 (1.7) of the 14 optional exercise sessions. All of the teachers taught at least some of the optional nutrition lessons, and all of the teachers completed at least half of the optional exercise sessions. The Hip-Hop to Health CD was used in almost all (94%) of the exercise sessions.
Parent Homework Completion
On average, the 307 parents in the intervention group completed 5.0 (SD = 4.5) of the 13 homework assignments. Twenty (7%) of the parents completed all 13 assignments. One hundred fifteen parents (37%) completed more than half of the homework assignments, and 238 (78%) completed at least one assignment.
Post-Intervention Data
Post-intervention height and weight were measured for 589 children (95%). The screen time questionnaire was completed for 564 children post-intervention, and 543 children had screen time data at baseline and post-intervention.
Valid accelerometer records were collected for 288 children at the post-intervention visit, and 190 children had valid accelerometer records at baseline and post-intervention. The proportion of children with valid records differed by school (highest=48%, lowest=7%, p=.007) but not by intervention group (p=.49). The 190 children with valid records were not significantly different from the other children in gender, race, age, BMI, BMI Z score, weight, or height. Parents of the 190 children with valid accelerometer data were older than parents of children without valid data: mean (SD) = 32.2 (9.6) years vs. 30.3 (8.1) years, p=.02. They also reported somewhat more education: mean (SD) = 12.5 (1.6) years vs. 12.2 (1.7) years, p=.04. There were no significant differences in parent gender, median income, marital status, full-time employment, BMI, height, or weight.
Valid diet records were collected for 487 children at the post-intervention visit, and 440 children had valid diet records at both the baseline and post-intervention visits. The proportion of children with valid records differed by school (highest=94%, lowest=55%, p<.001) but not by intervention group (p=.24). The 440 children who had valid diet records at both visits did not differ significantly from the other 178 children in gender, race, age, BMI, BMI Z score, weight, or height. There was also no significant difference in parents’ gender, age, education, median income, marital status, full-time employment, BMI, height, or weight.
BMI Outcomes
Changes in BMI, BMI Z score, weight and height at the post-intervention visit are shown in Table 4. As expected, there were no significant differences between groups immediately post-intervention.
Table 4.
Adjusteda change in child BMI, BMI Z score, weight, and height at post-intervention follow-up, Teacher-Delivered Hip-Hop to Health
| Intervention | Control | |||
|---|---|---|---|---|
| (N=309) | (N=280) | Difference | ||
| Mean | Mean | (WCI-GHI) | ||
| change (SE) | change (SE) | (95% CI) | p | |
| BMI (kg/m2)b | 0.11 (0.05) | 0.22 (0.05) | −0.11 (−0.26 to 0.05) | .17 |
| Adjusted BMI (kg/m2)c | 0.13 (0.05) | 0.21 (0.05) | −0.08 (−0.23 to 0.07) | .28 |
| BMI Z score | 0.08 (0.03) | 0.12 (0.03) | −0.04 (−0.13 to 0.05) | .39 |
| Adjusted BMI Z scorec | 0.07 (0.03) | 0.12 (0.03) | −0.05 (−0.14 to 0.04) | .23 |
| Weight (kg) | 1.52 (0.10) | 1.75 (0.10) | −0.24 (−0.54 to 0.07) | |
| Height (cm) | 3.86 (0.23) | 4.02 (0.23) | −0.17 (−0.84 to 0.51) |
SE, standard error; CI, confidence interval; WCI=weight control intervention; GHI=general health intervention.; BMI, body mass index.
Adjusted for preschool and classroom using SAS Proc Mixed.
For children with post-intervention anthropometric data, the unadjusted mean (SD) BMI at baseline was 16.5 (1.7) kg/m2 in the intervention group and 16.7 (2.2) kg/m2 in the control group. At post-intervention, the unadjusted mean (SD) was 16.6 (1.9) kg/m2 in theintervention group and 16.9 (2.5) kg/m2 in the control group.
Adjusted for baseline value, baseline age (years), preschool and classroom using SAS Proc Mixed.
Physical Activity Outcomes
As shown in Table 5, children in the intervention schools engaged in more moderate-to-vigorous physical activity (MVPA) than children in the control schools, controlling for baseline activity, baseline age, school, and classroom. The difference between groups was significant whether MVPA was expressed as minutes/day or as minutes/hour worn (in both cases, p=.02 for difference between groups). Both moderate (p=.05) and vigorous (p=.03) activity were higher in the intervention group than in the control group. Mean accelerometer counts per minute were higher in the intervention group, but the difference was not statistically significant (672.6 vs. 640.1 counts per minute, p=.06).
Table 5.
Adjusteda child physical activity, screen time, and diet at post-intervention follow-up, Teacher-Delivered Hip-Hop to Health
| Intervention | Control | Difference | ||
|---|---|---|---|---|
| Mean (SE) | Mean (SE) | (WCI-GHI) (95% CI) |
p | |
| Physical activity | N=96 | N=94 | ||
| MVPA, min/day | 109.9 (2.0) | 102.5 (2.0) | 7.46 (1.41 to 13.51) | .02 |
| MVPA, min/hour worn | 8.5 (0.1) | 7.9 (0.1) | 0.53 (0.09 to 0.97) | .02 |
| Moderate activity, min/day |
79.0 (1.6) | 74.2 (1.6) | 4.78 (0.10 to 9.45) | .05 |
| Vigorous activity, min/day |
31.0 (0.8) | 28.2 (0.8) | 2.83 (0.36 to 5.29) | .03 |
| Counts/min worn | 672.6 (11.4) | 640.1 (11.5) | 32.6 (−1.8 to 66.9) | .06 |
| Screen time | N=284 | N=259 | ||
| Hr/day | Hr/day | Min/day | ||
| TV viewing | 2.4 (0.1) | 2.6 (0.1) | −10.2 (−24.9 to 4.6) | .16 |
| Screen timeb | 4.7 (0.1) | 5.2 (0.2) | −27.8 (−55.1 to −0.5) | .05 |
| Diet | N=238 | N=202 | ||
| Energy, kcal | 1632 (57) | 1552 (61) | 79.9 (−97.5 to 257.3) | .35 |
| Fat, % kcal | 33.3 (0.7) | 32.2 (0.7) | 1.17 (−0.94 to 3.27) | .26 |
| Fiber, g/1000 kcal | 7.1 (0.2) | 7.2 (0.2) | −0.06 (−0.76 to 0.64) | .86 |
| Fruitc, servings/day | 1.0 (0.1) | 0.9 (0.1) | 0.08 (−0.31 to 0.46) | .69 |
| 100% fruit juice, servings/day |
1.4 (0.1) | 1.1 (0.2) | 0.32 (−0.12 to 0.75) | .15 |
| Vegetablesd, servings/day | 1.2 (0.1) | 1.2 (0.1) | 0.06 (−0.17 to 0.30) | .58 |
SE, standard error; CI, confidence interval; WCl=weight control intervention; GHI=general health intervention; MVPA, moderate-to-vigorous physical activity
Adjusted for baseline value, baseline age (years), preschool and classroom using SAS Proc Mixed.
Time spent watching television, DVDs or videotapes, playing video games, or using a computer.
Excludes juices, avocado, fried fruits, and fruit-based savory snacks.
Includes dark green and deep yellow vegetables, tomatoes, white potatoes and other starchy vegetables, legumes, and other vegetables; excludes fried potatoes, other fried vegetables, and vegetable juice.
Screen Time Outcomes
As shown in Table 5, children in the intervention group had significantly less total screen time than children in the control group (p=.05) at post-intervention. However, there was no significant difference between groups in television viewing.
Diet Outcomes
At the post-intervention visit, there were no significant differences between groups in energy intake, dietary fat, dietary fiber, or consumption of fruit, 100% fruit juice, or vegetables, controlling for the baseline value, age, school, and classroom (see Table 5).
DISCUSSION
Racial/ethnic disparities in obesity, particularly among females, are apparent by adolescence (4) and begin to become evident by 6 - 11 years of age. (4) Therefore, early intervention during the formative preschool years is viewed as a critical step in halting the obesity epidemic. School-based programs are often seen as an ideal setting for prevention efforts because most children attend school, and minority children, who are at highest risk, can participate at no cost. (18)
The Hip-Hop to Health Jr. Obesity Prevention Effectiveness Trial was designed to test an adapted version of an intervention that was shown to be successful. In an efficacy trial (5-7), specially trained early childhood educators on the study staff delivered the intervention; in the current trial, the intervention was adapted so that it could be taught by classroom teachers. For reasons of both sustainability and cost, it is necessary to conduct translational research to demonstrate how to effectively move successful interventions from experimental studies to real-world settings, especially settings that serve high-risk and underserved populations. Thus, this study can be viewed as an important step in determining the feasibility of translating a successful preschool-based, minority-focused obesity prevention program into a form that is potentially easier to disseminate widely.
The current results support the feasibility of training classroom teachers to deliver an evidence-based intervention, since the teachers were able to incorporate the interventions into their daily schedule. Most teachers reported completing almost all of the 28 nutrition and exercise lessons, and all teachers completed at least 21 nutrition lessons and 21 exercise lessons.
Training and supervision of the teachers, however, proved more time-intensive than we initially anticipated. As in other teacher-delivered obesity prevention interventions, (19, 20) the classroom teachers received several training sessions and were provided with detailed dietary and physical activity curricula. From the beginning, the teachers were more comfortable delivering the didactic nutrition information, but wanted more guidance in how to structure the delivery of the physical activity segments. The teachers expressed difficulty in delivering the physical activity for two primary reasons. First, many of the children were initially resistant to engaging in activity for a full 20 minutes and became distracted as they grew tired. Second, many of the teachers were not accustomed to engaging in exercise themselves, and some had physical limitations that made exercise challenging. Therefore, we needed to provide weekly individualized supervision to discuss strategies for engaging the children in exercise, as well as any other difficulties the teacher was experiencing. We then decided to create a CD that mirrored the weekly curriculum so that the teachers could improve their delivery of the intervention. This need for more in-depth work with the teachers was unexpected, but a very rewarding aspect of the intervention. It served to strengthen our relationships not only with the individual teachers, but with the larger school environment.
Since the WCI was an obesity prevention intervention rather than an obesity treatment intervention, we did not expect to see a difference between groups in BMI change or BMI Z score change at the post-intervention visit. In the original efficacy trial, (7) we observed significant differences between groups at 1-year and 2-year follow-up. If this intervention is successful, we expect to see a significant difference between groups at the 1-year follow-up visit.
Overall, our results show that the teacher-delivered intervention increased the children’s post-intervention physical activity. Unfortunately, it is difficult to compare these results to the results of the original efficacy trial, due primarily to measurement differences. (7) In the efficacy trial, parents reported the frequency and intensity of the child’s current physical activity, (7) but in the current study we used accelerometers, which are now the most commonly used objective method of physical activity. (21) However, the translation of “movement counts” derived from accelerometers into an estimate of physiological activity intensity is a hotly debated topic (22) and intensity thresholds for moderate and vigorous physical activity, derived specifically for use in young people, vary widely. (22) In our analyses, we used count thresholds for moderate and vigorous physical activity derived from a calibration study in which 29 preschool children (45% male, 55% black) performed structured and unstructured activities while wearing an ActiGraph accelerometer and an apparatus that measured oxygen consumption by indirect calorimetry. (15) These thresholds were also used in the Children’s Activity and Movement Preschool Study (CHAMPS). (23, 24) The definition of a valid record accelerometer record for children is still an open question. (14, 23) In the absence of a clear consensus, we defined a valid record as ≥ 4 days with ≥ 8 hours of wear. To put our results in some context, Williams and colleagues (2008) reported 90 min/day of MVPA in an ethnically diverse group of 198 children aged 3-4 years, somewhat lower than the 98.7 min/day found in our study at baseline. (23) In another report from CHAMPS, (24) 331 children aged 3-5 years engaged in 7.6 min/hr of MVPA, similar to the 7.8 min./hr in our sample. Although our intervention may have led to improved levels of MVPA, the children’s post-intervention activity levels are still below the recent recommendations of 120 minutes of MVPA daily, consisting of 60 minutes of structured activity and 60 minutes of unstructured free play. (25)
Overall, while the opportunity to gather objective data on physical activity has the potential to be extremely powerful, collecting accelerometer data involves a higher participant burden than collecting basic anthropometric or questionnaire data. Very few children refused to wear the accelerometer, and parents were generally receptive. However, even when parents agreed to participate and were called daily for 7 days to remind them to place the accelerometer on the child, our data clearly show that they found it difficult to comply with this protocol. Still, the percentage of baseline records that were valid 323/445 (73%) is actually fairly similar to the percentage of valid records reported by NHANES for adults and children ≥ 6 years: 4867/6832 (71%). (14) While the NHANES definition of a valid record (≥ 4 days with ≥ 10 hours of wear) was more stringent than ours, the relatively high level of non-compliance suggests that wearing an accelerometer consistently can be challenging for many people.
Our intervention also appears to have had a positive impact on the screen time of the children. Television viewing and other sedentary screen time (i.e., video and computer games) has been implicated in the increasing prevalence of childhood obesity. (26) Reported television viewing time was similar for both our efficacy trial (7) and this trial. However, in the original efficacy trial, we only measured TV viewing and did not assess additional screen time. Our curriculum stresses a number of enjoyable activities that a child can engage in rather than watching television or playing video games, since this is an area where even a young child can potentially exert control and make more independent choices. Although children in the intervention group reported less total screen time than children in the control group post-intervention, it is important to note that the American Academy of Pediatrics recommends at most 2 hours of total screen time per day for children, (27) and mean screen time in the intervention group was 4.7 hr/day. Although we did not find a significant correlation between BMI and screen time at baseline, Jago and colleagues (28) found that TV viewing at age 3 to 4 was significantly and positively correlated with higher BMI two years later. Thus, there may be a delayed effect of TV viewing on body fatness that may not be apparent when examining cross-sectional data. (29) Some data suggest that limiting children’s TV viewing to 2 or fewer hours each day could reduce their future risk of obesity. Given the high level of screen time (7.2 hours) reported by the parents at baseline, reducing family screen time could be beneficial in preventing excessive weight gain as children age and should be addressed in future interventions. (30)
Our results do not show any dietary differences between groups at post-intervention, which is similar to the results of our efficacy trial. (7) Given that more than 50% of the parents were obese, we suspect that this may be related in part to the lack of a strong parental intervention component. Unlike screen time choices, where children may have more autonomy, parents are usually the gatekeepers for food and beverage availability and accessibility. (31) Although few programs have assessed home-based interventions designed to influence dietary intake, a recent study by Haire-Joshu and colleagues (32) shows the potential for home-based interventions to improve the dietary intake of both parents and young children. Providing a home-based component as an adjunct to a successful school-based intervention could improve both outcomes and sustainability.
There are several limitations to this study that should be acknowledged. Although we had trained diet staff to observe the children eating while in school, accurate reporting of food intake in this age group is especially challenging when multiple care-givers or random unobserved snacking may go undocumented. The measurement of physical activity can be viewed as both a limitation and strength of this study. The amount of missing accelerometer data is potentially a cause for concern, although there were no obvious differences between children who had valid accelerometer records and those who did not. Finally, we did not collect data on the social context in which people were living and making decisions related to their health and the health of their children. This rich area of research is increasingly recognized as crucial in order to better understand how to design interventions and interpret results. (33)
Overall, the results of this effectiveness trial suggest that an evidence-based intervention tested in an efficacy trial can be adapted for delivery by classroom teachers and can produce changes in physical activity and screen time. The final test of the intervention will be whether we observe differences in BMI and BMI Z score changes between the intervention and control groups at the one-year follow-up visit. Our results underscore the need to expand our interventions outside the classroom and to understand how best to accommodate low-income families in obesity prevention efforts.
ACKNOWLEDGEMENTS
The Hip-Hop to Health Obesity Prevention Effectiveness Trial was supported by the National Heart, Lung and Blood Institute (HL081645). We would like to thank the Chicago Public Schools Early Childhood Education Program, the families and teachers who participated in this project, and the principals who supported the project. We would also like to thank Lara Blumstein, the project coordinator, as well as Sarah Ford Thompson, the intervention coordinator, and the dedicated data collectors. We would like to thank Guadalupe Compean for her technical assistance. Finally we would like to thank the entire project staff for their dedication and belief in the importance of understanding more about health promotion and obesity prevention in very young minority children.
Footnotes
DISCLOSURE
No financial disclosure information.
REFERENCES
- 1.Ogden CL, Yanovski SZ, Carroll MD, Flegal KM. The epidemiology of obesity. Gastroenterology. 2007;132(6):2087–2102. doi: 10.1053/j.gastro.2007.03.052. [DOI] [PubMed] [Google Scholar]
- 2.Barlow SE, Expert Committee Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007;120(Suppl 4):S164–192. doi: 10.1542/peds.2007-2329C. [DOI] [PubMed] [Google Scholar]
- 3.Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, Mei Z, et al. CDC growth charts for the United States: methods and development. Vital Health Stat. 2000;2002;11(246):1–190. [PubMed] [Google Scholar]
- 4.Ogden CL, Carroll MD, Curtin LR, Lamb MM, Flegal KM , 2007-2008. JAMA. 2010;303(3):242–249. doi: 10.1001/jama.2009.2012. [DOI] [PubMed] [Google Scholar]
- 5.Fitzgibbon ML, Stolley MR, Dyer AR, Van Horn L, KauferChristoffel K. A community-based obesity prevention program for minority children: rationale and study design for Hip-Hop to Health Jr. Prev Med. 2002;34:289–297. doi: 10.1006/pmed.2001.0977. [DOI] [PubMed] [Google Scholar]
- 6.Stolley MR, Fitzgibbon ML, Dyer A, Van Horn L, KauferChristoffel K, Schiffer L. Hip-Hop to Health Jr., an obesity prevention program for minority preschool children: baseline characteristics of participants. Prev Med. 2003;36(3):320–329. doi: 10.1016/s0091-7435(02)00068-3. [DOI] [PubMed] [Google Scholar]
- 7.Fitzgibbon ML, Stolley MR, Schiffer L, Van Horn L, KauferChristoffel K, Dyer A. Two year follow-up results for Hip-Hop to Health Jr.: a randomized controlled trial for overweight prevention in preschool minority children. J Pediatr. 2005;146(5):618–625. doi: 10.1016/j.jpeds.2004.12.019. [DOI] [PubMed] [Google Scholar]
- 8.Bandura A. Self-efficacy: the exercise of control. W.H. Freeman and Company; New York: 1997. [Google Scholar]
- 9.Deci EL, Renninger KA. The relation of interest to the motivation of behavior: a self-determination theory perspective. In: Hidi S, Krapp A, editors. The Role of Interest in Learning and Development. Lawrence Erlbaum Associates; Hillsdale: 1992. pp. 43–70. [Google Scholar]
- 10.Highberger R, Carothers L. Modification of eating behavior of toddlers in a day care setting. Family and Consumer Sciences Research Journal. 1977;6(1):48–51. [Google Scholar]
- 11.Birch LL, Marlin DW. I don’t like it; I never tried it: Effects of exposure on two-year-old children’s food preferences. Appetite. 1982;3(4):353–360. doi: 10.1016/s0195-6663(82)80053-6. [DOI] [PubMed] [Google Scholar]
- 12.Trost SG, Sirard JR, Dowda M, Pfeiffer KA, Pate RR. Physical activity in overweight and nonoverweight preschool children. Int J Obes Relat Metab Disord. 2003;27(7):834–839. doi: 10.1038/sj.ijo.0802311. [DOI] [PubMed] [Google Scholar]
- 13.Deci EL, Ryan RM. A motivational approach to self: Integration in personality. In: Dienstbier R, editor. Perspectives on Motivation. University of Nebraska Press; Lincoln: 1991. pp. 237–288. Nebraska Symposium on Motivation, 1990, Vol.38. [PubMed] [Google Scholar]
- 14.Troiano RP, Berrigan D, Dodd KW, Mâsse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40(1):181–188. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- 15.Pate RR, Almeida MJ, McIver KL, Pfeiffer KA, Dowda M. Validation and calibration of an accelerometer in preschool children. Obesity. 2006;14(11):2000–2006. doi: 10.1038/oby.2006.234. [DOI] [PubMed] [Google Scholar]
- 16.Borzekowski DL, Robinson TN. The remote, the mouse, and the no. 2 pencil: the household media environment and academic achievement among third grade students. Arch Pediatr Adolesc Med. 2005;159(7):607–613. doi: 10.1001/archpedi.159.7.607. [DOI] [PubMed] [Google Scholar]
- 17.Murray DM. Design and Analysis of Group-Randomized Trials. Oxford University Press; New York: 1998. [Google Scholar]
- 18.Story M. School-based approaches for preventing and treating obesity. Int J Obes Relat Metab Disord. 1999;23(2):S43–S51. doi: 10.1038/sj.ijo.0800859. [DOI] [PubMed] [Google Scholar]
- 19.Gittelsohn J, Davis SM, Steckler A, Ethelbah B, Clay T, Metcalfe L, et al. Pathways: lessons learned and future directions for school-based interventions among American Indians. Prev Med. 2003;37(6 Pt 2):S107–112. doi: 10.1016/j.ypmed.2003.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Resnicow K, Cohn L, Reinhardt J, Cross D, Futterman R, Kirschner E, et al. A three-year evaluation of the Know Your Body program in inner-city school children. Health Educ Q. 1992;19(4):463–480. doi: 10.1177/109019819201900410. [DOI] [PubMed] [Google Scholar]
- 21.Rowlands AV. Accelerometer assessment of physical activity in children: an update. Pediatr Exerc Sci. 2007;19(3):252–266. doi: 10.1123/pes.19.3.252. [DOI] [PubMed] [Google Scholar]
- 22.Guinhouya CB, Hubert H, Soubrier S, Vilhelm C, Lemdani M, Durocher A. Moderate-to-vigorous physical activity among children: discrepancies in accelerometry-based cut-off points. Obesity. 2006;14(5):774–777. doi: 10.1038/oby.2006.89. [DOI] [PubMed] [Google Scholar]
- 23.Williams HG, Pfeiffer KA, O’Neill JR, Dowda M, McIver KL, Brown WH, et al. Motor skill performance and physical activity in preschool children. Obesity. 2008;16(6):1421–1426. doi: 10.1038/oby.2008.214. [DOI] [PubMed] [Google Scholar]
- 24.Pfeiffer KA, Dowda M, McIver KL, Pate RR. Factors related to objectively measured physical activity in preschool children. Pediatr Exerc Sci. 2009;21(2):196–208. doi: 10.1123/pes.21.2.196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.National Association for Sport and Physical Education . Moving into the Future: National Standards of Physical Education. 2nd ed. National Association for Sport and Physical Education; Reston: 2004. [Google Scholar]
- 26.Andersen RE, Crespo CJ, Bartlett SJ, Cheskin LJ, Pratt M. Relationship of physical activity and television watching with body weight and level of fatness among children: results from the Third National Health and Nutrition Examination Survey. JAMA. 1998;279(12):938–942. doi: 10.1001/jama.279.12.938. [DOI] [PubMed] [Google Scholar]
- 27.Committee on Public Education Children, Adolescents, and Television. Pediatrics. 2001;107(2):423–426. doi: 10.1542/peds.107.2.423. [DOI] [PubMed] [Google Scholar]
- 28.Jago R, Baranowski T, Baranowski JC, Thompson D, Greaves KA. BMI from 3-6 y of age is predicted by TV viewing and physical activity, not diet. Int J Obes Relat Metab Disord. 2005;29(6):557–564. doi: 10.1038/sj.ijo.0802969. [DOI] [PubMed] [Google Scholar]
- 29.Krahnstoever Davison K, Francis LA, Birch LL. Reexamining obesigenic families: parents’ obesity-related behaviors predict girls’ change in BMI. Obes Res. 2005;13(11):1980–1990. doi: 10.1038/oby.2005.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ventura AK, Birch LL. Does parenting affect children’s eating and weight status? Int J Behav Nutr Phys Act. 2008;5:15. doi: 10.1186/1479-5868-5-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Birch LL, Davison KK. Family environmental factors influencing the developing behavioral controls of food intake and childhood overweight. Pediatr Clin North Am. 2001;48(4):893–907. doi: 10.1016/s0031-3955(05)70347-3. [DOI] [PubMed] [Google Scholar]
- 32.Haire-Joshu D, Elliott MB, Caito NM, Hessler K, Nanney MS, Hale N, et al. High 5 for Kids: the impact of a home visiting program on fruit and vegetable intake of parents and their preschool children. Prev Med. 2008;47(1):77–82. doi: 10.1016/j.ypmed.2008.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sorensen G, Stoddard AM, Dubowitz T, Barbeau EM, Bigby J, Emmons KM, et al. The influence of social context on changes in fruit and vegetable consumption: results of the Healthy Directions Studies. Am J Public Health. 2007;97(7):1216–1227. doi: 10.2105/AJPH.2006.088120. [DOI] [PMC free article] [PubMed] [Google Scholar]