Abstract
Objective
To determine whether borderline personality disorder (BPD) and bipolar II disorder can be differentiated from each other and from major depressive disorder (MDD) by comparing depression severity, impulsiveness, and hostility in mood disorder patients with and without BPD.
Method
One hundred seventy-three patients with either MDD or bipolar II disorder were enrolled from a larger sample admitted to a multisite project on mood disorders and suicidal behavior conducted from June 1996 through June 2006. Patients were divided into 4 groups: MDD with BPD, MDD without an Axis II diagnosis, bipolar II disorder with BPD, and bipolar II disorder without an Axis II diagnosis. All diagnoses were based on DSM-IV criteria. Depression was assessed using the 17-item Hamilton Rating Scale for Depression (HAM-D) and the self-rated Beck Depression Inventory (BDI). Impulsiveness was assessed using the Barratt Impulsiveness Scale, and hostility was assessed using the Buss-Durkee Hostility Inventory.
Results
Patients with BPD reported higher levels of impulsiveness (p = .004) and hostility (p = .001), independent of Axis I diagnosis. Bipolar II patients reported greater attentional impulsiveness (p = .008) than MDD patients, independent of BPD status, while BPD patients reported greater nonplanning impulsiveness than patients without BPD, independent of Axis I diagnosis (p = .02). For motor impulsiveness, there was a main effect for Axis I diagnosis (p = .05) and Axis II diagnosis (p = .002). The bipolar II + BPD group scored the highest, suggesting a compound effect of comorbidity. There were no differences in depression severity when measured with the HAM-D, although the BPD groups reported more severe depression on the BDI, independent of their Axis I diagnosis (p = .05). The BPD groups scored higher on the cognitive factor (p = .01) and anxiety factor (p = .03) of the HAM-D.
Conclusion
Results suggest that there is a unique symptom and trait profile associated with BPD that distinguishes the diagnosis from bipolar II disorder. Results also suggest that impulsiveness is an important aspect of both disorders and that there is a compounding effect associated with a diagnosis of bipolar II disorder with comorbid BPD.
Borderline personality disorder (BPD) and bipolar affective disorders have a high rate of comorbidity.1 The frequent co-occurrence of these disorders and the similarities between some of their diagnostic criteria have led to a debate over their relationship. While several researchers have concluded that BPD is a distinct condition,2,3 others have suggested that it coexists along a spectrum of cyclical affective disorders.4–6 Some investigators subscribing to this latter view have suggested that BPD may be better conceptualized as an ultra-rapid cycling form of bipolar II disorder.6
The debate stems, in part, from a relatively small area of overlap between the diagnostic criteria sets for BPD and bipolar II disorder. Both are characterized by increased levels of impulsive behavior, affective lability, and irritability. Careful examination of the criteria suggests these traits would appear distinct when comparing the disorders. For example, BPD is characterized by the trait of “affective instability,” which is generally defined as a persisting reactivity of mood and tendency toward “intense episodic dysphoria, irritability, or anxiety,”7 whereas bipolar II disorder is characterized by recurrent and episodic mood states with less reactivity. Impulsiveness is also considered to be a relatively stable aspect of BPD, but is considered to be an episode-dependent criterion of hypomanic, but not major depressive, episodes.
In practice, however, attempting to classify the features of these disorders within the dichotomy of Axis I and Axis II quickly leads to the realization that they sometimes do not fall neatly into state- and trait-like categories. Research with these diagnostic groups has also shown this to be the case. For example, while impulsiveness is considered to be a stable aspect of BPD, longitudinal research has shown that behavioral impulsiveness is the BPD feature that is most likely to remit.8 In contrast, while impulsiveness in bipolar II disorder would be expected to be episodic in nature, recent research has shown that some aspects of impulsiveness are relatively stable across manic and euthymic mood states in bipolar patients.9 Because of these ambiguities, distinguishing BPD and bipolar II disorder, particularly when assessing these patients cross-sectionally, can sometimes be challenging.
The aim of this research was to determine whether BPD and bipolar II disorder can be differentiated by comparing mood disorder patients (major depressive disorder [MDD] and bipolar II disorder) with and without BPD on both trait and symptom measures using a factorial design. By comparing these 4 groups, we attempted to answer 3 main research questions: (1) whether bipolar II disorder was similar to, or distinguishable from, another affective disorder (MDD); (2) whether the bipolar II–only group was similar to, or distinguishable from, the BPD groups; and (3) whether there was any compounding effect that resulted from a diagnosis of bipolar II disorder with comorbid BPD. In addition, by studying the groups while all participants were in a major depressive episode and thus standardizing their mood symptoms, we were able to study the bipolar patients while they were not reporting any Axis I hypomanic symptoms, as well as control for the effects of depression.
We hypothesized that the patients with both mood disorders and BPD would be distinguishable from MDD and bipolar II patients without personality disorders by the trait indicators of impulsiveness and hostility, as well as by more severe self-reported depression. Since all groups were in a major depressive episode, we expected no differences between the MDD groups and the bipolar II groups, independent of their Axis II status. We chose to examine subjective and objective ratings of depression severity (and the discrepancy between the 2) as proxy variables for emotional sensitivity. We have argued elsewhere10 that unipolar depressed BPD patients experience more severe cognitive symptoms of depression compared to patients without personality disorders because of an extreme sensitivity to negative emotional states. We anticipated this sensitivity to be a distinguishing factor of bipolar II patients with BPD, as well.
METHOD
Participants and Procedures
Research participants were enrolled from a larger sample admitted to a multisite project on mood disorders and suicidal behavior conducted from June 1996 through June 2006. One hundred seventy-three patients with either MDD or bipolar II disorder were included in the analyses. All participants were in a major depressive episode. Seventy-four percent of the sample were admitted to an inpatient research unit at the time of assessment, while the remaining 26% were assessed on an outpatient basis. Inpatients were interviewed after a medication washout period and were all medication-free at the time of assessment. Participants were divided into 4 groups: MDD with BPD, MDD without an Axis II diagnosis, bipolar II disorder with BPD, and bipolar II disorder without an Axis II diagnosis. All the patients met DSM-IV7 criteria for either bipolar II disorder (N = 30) or MDD (N = 143). Overall, 87 of the patients were diagnosed with DSM-IV BPD, while the remaining 86 had no Axis II diagnosis.
Exclusion criteria were the presence of a current substance abuse or dependence diagnosis, the presence of persisting psychotic symptoms or a psychotic disorder diagnosis, history of severe head trauma, or the presence of mental retardation or any cognitive impairment that might interfere with the completion of the assessments or the obtaining of informed consent. Participants ranged in age from 19 to 56 years, had a mean age of 35.2 (SD = 10.2) years, and were 66.5% female. Participants were predominantly white (74.6%) and single (50.3%). A majority had at least some education at the college level (77.5%), with 43.9% of the total sample having obtained a college degree. The study was approved by all local institutional review boards, and all participants provided written informed consent.
Diagnoses were determined using the Structured Clinical Interview for DSM-III-R/DSM-IV (SCID-I), Patient Edition,11 and the Structured Clinical Interview for DSM-IV Axis II Personality Disorders (SCID-II).12 Depressive symptomatology was assessed in 2 ways. Clinician ratings were conducted with the 17-item Hamilton Rating Scale for Depression (HAM-D),13 administered in a semistructured interview format. In addition to the clinical ratings, the participants completed the Beck Depression Inventory (BDI),14 a 21-item self-report measure of depressive symptomatology. Impulsiveness was determined using an early draft of the eleventh version of the Barratt Impulsiveness Scale (BIS-11),15 a 30-item self-report questionnaire designed to measure levels of trait impulsiveness, with demonstrated reliability and validity. Hostility was assessed using the Buss-Durkee Hostility Inventory (BDHI),16 a 75-item self-report questionnaire designed to measure several aspects of hostility. The scale contains 7 subscales (66 items) plus an additional Guilt subscale (9 items) that is not included in the total score. The BDHI is also a very widely used measure of hostility, with demonstrated reliability and validity. All interviews were conducted by doctoral-level clinicians with specific training in the use of the SCID instruments and clinical measures. Interviewers were trained to a criterion level of interrater reliability that varied according to the reliability co-efficients reported for each measure. Recent reliability studies with the interview measures used in this research yielded the following intraclass correlation coefficients (ICCs) (criterion levels are shown in parentheses): Axis I diagnosis/SCID-I, ICC = 0.80 (0.70); Axis II diagnosis/SCID-II, ICC = 0.70 (0.70); BPD diagnosis, ICC = 0.89 (0.70); clinician ratings of depression/24-item HAM-D, ICC = 0.97 (0.90).
Data Analysis
Means and standard deviations were computed for all variables in the analyses, and all variables were checked for normality and outliers. In order to test for group differences on the demographic variables, χ2 was computed for gender, education, race, and marital status, and the t test for independent samples was computed for age. Two-way factorial analysis of covariance (ANCOVA) was used to test for differences between the patient groups, with mood disorder diagnosis and BPD presence or absence as factors. Age and gender were included in the analyses due to the evidence in the literature for their effects on impulsiveness.17,18 Suicide-attempter status was also included as a covariate initially because of differences in the number of suicide attempters between the groups. Attempter status was not significant in any of the analyses and was excluded (results not reported). Each of the 4 dependent variables was analyzed with a separate equation. We also conducted post hoc ANCOVAs of the 3 BIS-11 subscales, as well as the 6 HAM-D factor scores originally published by Hamilton.19
RESULTS
Participant Demographics
Demographic information comparing the 4 groups is presented in Table 1. The 4 diagnostic groups did not differ in education level or race. With respect to marital status, the BPD groups were more likely to be single. The BPD groups were also younger than the groups without Axis II diagnoses. Gender proportion did not differ between the groups, with all 4 groups having more women. There was no difference in the percentage of inpatients in each group. The scores for the combined groups on the depression scales were mean ± SD = 19.9 ± 5.5 for the HAM-D and mean ± SD = 28.9 ± 10.9 for the BDI. Overall, the participants were moderately depressed. In addition, approximately 34% of the participants were diagnosed with a comorbid anxiety disorder. There was no significant difference in comorbidity between the groups.
Table 1.
Demographic Characteristics by Diagnostic Group
| Characteristic | Bipolar II/BPD (N = 15) | MDD/BPD (N = 72) | Bipolar II Only (N = 15) | MDD Only (N = 71) | Statistics | |
|---|---|---|---|---|---|---|
|
| ||||||
| χ2 Test | df | |||||
| Age, mean ± SD, y** | 33.0 ± 10.8 | 32.4 ± 8.8 | 37.7 ± 11.1 | 38.0 ± 10.5 | ||
| Inpatient, N (%) | 7 (46.7) | 54 (75.0) | 11 (73.3) | 56 (78.9) | 6.74a | 3 |
| Female, % | 60.0 | 76.4 | 66.7 | 57.7 | 5.85 | 3 |
| Education, N | 22.35 | 15 | ||||
| Some high school | 0 | 4 | 1 | 3 | ||
| High school graduate | 2 | 11 | 1 | 14 | ||
| Some college | 5 | 30 | 3 | 20 | ||
| College graduate | 5 | 19 | 4 | 15 | ||
| Postgraduate | 2 | 8 | 5 | 18 | ||
| Race/Ethnicity, N | 6.17 | 12 | ||||
| White | 12 | 52 | 12 | 53 | ||
| African American | 1 | 10 | 2 | 4 | ||
| Asian | 0 | 1 | 0 | 1 | ||
| Hispanic | 2 | 8 | 1 | 10 | ||
| Other | 0 | 1 | 0 | 3 | ||
| Marital status, N | 17.97* | 9 | ||||
| Single | 8 | 47 | 7 | 25 | ||
| Married/cohabiting | 5 | 9 | 5 | 25 | ||
| Separated/divorced | 2 | 16 | 3 | 20 | ||
| Anxiety disorder comorbidity, N (%) | 6 (40.0) | 26 (36.1) | 5 (33.3) | 21 (29.6) | < 1.00 | 3 |
p < .10.
p < .05.
p < .001, t = −3.65, df = 171 for patients with BPD versus those without an Axis II disorder; because of the similarity of mean ages within each factor, the t test was computed for the mean ages of the participants with a BPD diagnosis (32.5 ± 9.1 years) and the participants without an Axis II diagnosis (38.0 ± 10.5 years).
Abbreviations: BPD = borderline personality disorder, MDD = major depressive disorder.
Impulsiveness and Hostility
In the analysis of the BIS-11 total scores (Table 2), there was a significant main effect for Axis II diagnosis (F = 8.75, df = 1, p = .004) but not for Axis I diagnosis. Age was significant (F = 4.34, df = 1, p = .04). The patients with a BPD diagnosis reported significantly more impulsiveness than patients without BPD, even after controlling for age.
Table 2.
Self-Rated Impulsivity and Hostility Measures by Diagnostic Group
| Scale | Bipolar II/BPD (N = 15) | Bipolar II Only (N = 15) | MDD/BPD (N = 72) | MDD Only (N = 71) | Total |
|---|---|---|---|---|---|
| BIS-11 score, mean ± SD | 63.6 ± 12.6 | 54.1 ± 14.1 | 58.8 ± 16.5 | 47.5 ± 15.3 | 54.2 ± 16.5 |
| BDHI score, mean ± SD | 38.9 ± 7.6 | 29.4 ± 10.2 | 36.6 ± 11.9 | 26.0 ± 9.9 | 31.8 ± 11.8 |
Abbreviations: BDHI = Buss-Durkee Hostility Inventory; BIS-11 = Barratt Impulsiveness Scale, version 11; BPD = borderline personality disorder; MDD = major depressive disorder.
In the analysis of the BDHI total scores (Table 2), again there was a significant main effect for Axis II diagnosis only (F = 19.87, df = 1, p = .001). Both age (F = 5.74, df = 1, p = .02) and gender (F = 9.77, df = 1, p = .002) were significant. Patients with a BPD diagnosis reported more hostility than patients without an Axis II diagnosis, even after controlling for age and gender differences.
We conducted post hoc analyses of the 3 BIS-11 subscales: attentional impulsiveness, motor impulsiveness, and nonplanning impulsiveness (Table 3 and Figure 1). For attentional impulsiveness, there was a significant main effect for Axis I diagnosis only (F = 7.23, df = 1, p = .008). Bipolar patients scored higher than MDD patients on this subscale, independent of their Axis II status. For nonplanning impulsiveness, there was a significant main effect for Axis II diagnosis only (F = 5.18, df = 1, p = .02). Patients with BPD scored higher on this subscale, independent of their Axis I diagnosis. Motor impulsiveness had a significant main effect for Axis I diagnosis (F = 4.06, df = 1, p = .05) as well as Axis II diagnosis (F = 10.24, df = 1, p = .002), with the bipolar groups scoring higher than the MDD groups, and the BPD groups scoring higher than the groups without BPD. The interaction effect was not significant. Age was significant in the motor impulsiveness analysis (F = 3.92, df = 1, p = .05). Neither age nor gender was significant in the attentional impulsiveness or nonplanning impulsiveness analyses.
Table 3.
BIS-11 Subscale Scores by Diagnostic Group
| Subscale | Bipolar II/BPD (N = 15) | Bipolar II Only (N = 15) | MDD/BPD (N = 72) | MDD Only (N = 71) | Total |
|---|---|---|---|---|---|
| Attentional impulsiveness score, mean ± SD | 18.9 ± 5.6 | 16.6 ± 4.8 | 15.4 ± 5.2 | 14.5 ± 5.4 | 15.4 ± 5.4 |
| Motor impulsiveness score, mean ± SD | 20.3 ± 5.9 | 16.9 ± 7.0 | 18.9 ± 7.0 | 12.9 ± 6.5 | 16.4 ± 7.3 |
| Nonplanning impulsiveness score, mean ± SD | 24.2 ± 7.8 | 20.7 ± 6.5 | 24.5 ± 8.6 | 20.1 ± 7.5 | 22.4 ± 8.1 |
Abbreviations: BIS-11 = Barratt Impulsiveness Scale, version 11; BPD = borderline personality disorder; MDD = major depressive disorder.
Figure 1. BIS-11 Subscale Scores by Diagnostic Group.
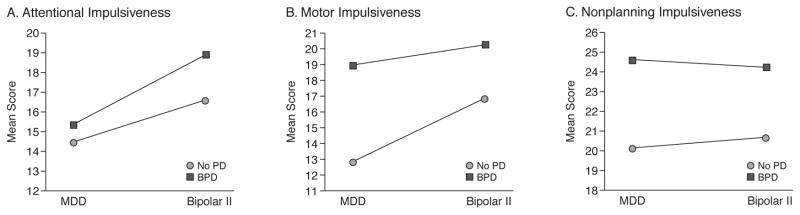
Abbreviations: BIS-11 = Barratt Impulsiveness Scale, version 11; BPD = borderline personality disorder; MDD = major depressive disorder; PD = personality disorder.
Depression Severity
Comparing the patient groups' clinician-rated depression severity in the analysis of the HAM-D (Table 4), there were no significant main effects for either Axis I or Axis II diagnosis. Neither age nor gender was significant. All 4 of the patient groups were rated as experiencing depressive symptoms of approximately equal severity. In the analysis of the BDI (Table 4), there was a main effect for Axis II diagnosis only (F = 3.87, df = 1, p = .05). The groups with an additional BPD diagnosis reported more severe depressive symptomatology than the patients without an Axis II diagnosis, regardless of their Axis I diagnosis. Gender was significant (F = 4.33, df = 1, p = .04).
Table 4.
Clinician-Rated and Self-Rated Depression Severity by Diagnostic Group
| Scale | Bipolar II/BPD (N = 15) | Bipolar II Only (N = 15) | MDD/BPD (N = 72) | MDD Only (N = 71) | Total |
|---|---|---|---|---|---|
| HAM-D score, mean ± SD | 19.0 ± 7.4 | 19.1 ± 5.7 | 19.7 ± 5.1 | 20.4 ± 5.5 | 19.9 ± 5.5 |
| BDI score, mean ± SD | 31.2 ± 12.8 | 27.2 ± 9.3 | 31.7 ± 10.0 | 26.1 ± 11.1 | 28.9 ± 10.9 |
Abbreviations: BDI = Beck Depression Inventory, BPD = borderline personality disorder, HAM-D = Hamilton Rating Scale for Depression, MDD = major depressive disorder.
We also conducted post hoc analyses on 6 factor scores for the HAM-D (computed from the 24-item measure) (Table 5). There were significant group differences on 2 of 5 factors. On the cognitive factor, there was a main effect for Axis II diagnosis only (F = 6.19, df = 1, p = .01). On average, the BPD groups scored higher on the cognitive symptoms factor, independent of Axis I diagnosis. On the anxiety factor, there was a main effect for Axis II diagnosis (F = 5.12, df = 1, p = .03), as well as a significant interaction effect (F = 8.37, df = 1, p = .004). While the bipolar II + BPD patients reported significantly more anxiety-related symptoms than the bipolar II patients without BPD, there was no difference between the MDD patients with and without BPD. Both age (F = 4.40, df = 1, p = .04) and gender (F = 6.09, df = 1, p = .02) were significant in the anxiety analysis. The initial HAM-D analysis was repeated with both the 21-item total score and the 24-item total score because of the results for the cognitive factor. As with the 17-item analysis, there were no significant differences between any of the groups in either analysis (results not shown).
Table 5.
HAM-D Factor Scores by Diagnostic Groupa
| Factor | Bipolar II/BPD (N = 15) | Bipolar II Only (N = 15) | MDD/BPD (N = 72) | MDD Only (N = 71) | Total |
|---|---|---|---|---|---|
| Anxiety | 1.2 ± 0.5 | 0.8 ± 0.3 | 1.0 ± 0.4 | 1.0 ± 0.4 | 1.0 ± 0.4 |
| Weight change | 0.6 ± 0.9 | 0.8 ± 1.0 | 0.8 ± 1.1 | 0.7 ± 1.1 | 0.8 ± 1.1 |
| Cognitive | 0.5 ± 0.5 | 0.2 ± 0.2 | 0.5 ± 0.4 | 0.3 ± 0.4 | 0.4 ± 0.4 |
| Diurnal variation | 0.5 ± 0.8 | 1.0 ± 1.0 | 1.1 ± 1.0 | 1.3 ± 0.9 | 1.2 ± 0.9 |
| Retardation | 1.7 ± 0.7 | 1.9 ± 0.7 | 1.5 ± 0.6 | 1.8 ± 0.6 | 1.7 ± 0.6 |
| Sleep disturbance | 1.1 ± 0.6 | 1.2 ± 0.5 | 1.0 ± 0.6 | 1.0 ± 0.6 | 1.0 ± 0.6 |
All factor scores are shown as mean ± SD.
Abbreviations: BPD = borderline personality disorder, HAM-D = Hamilton Rating Scale for Depression, MDD = major depressive disorder.
DISCUSSION
The aim of this study was to determine whether BPD patients and bipolar II patients could be differentiated from each other and from patients with MDD. The first hypothesis of the study, that BPD groups would be distinguishable by impulsiveness and hostility, was supported. Patients with BPD reported higher levels of impulsiveness and hostility than patients without BPD across Axis I diagnostic groups, even after controlling for age and gender. This finding is in agreement with several previously published studies.3,20 These 2 traits are commonly associated with BPD and have a demonstrated relationship with the self-destructive behaviors often seen in these patients.21 While the pattern of group means on the BDHI suggests that elevated hostility is a trait that is more descriptive of BPD patients, the BIS-11 scores suggest a more complex relationship between impulsiveness and the syndromes being compared. Results showed that bipolar II patients tended to be more impulsive than MDD patients overall but also that the MDD/BPD group was slightly more impulsive than the bipolar II group without a BPD diagnosis (58.8 vs. 54.1, respectively, t = 1.14, p = .27). Because of the ambiguity of the relationship between impulsiveness and the diagnostic syndromes, we chose to conduct the post hoc analyses described above.
In our analyses of the 3 BIS-11 subscales, each of the diagnostic syndromes was related to a different aspect of impulsiveness. While bipolar II disorder was uniquely associated with increased levels of attentional impulsiveness, BPD was uniquely associated with an increase in nonplanning impulsiveness. Motor impulsiveness was associated with both diagnoses, although both BPD groups had higher scores than either of the groups without BPD.
Patton, Stanford, and Barratt22 originally derived the subscales through a factor analysis of the BIS-11. In that analysis, each of the 3 subscales comprised 2 lower-order subsets of items. Attentional impulsiveness comprised subsets labeled attention and cognitive instability; motor impulsiveness comprised subsets labeled motor impulsiveness and perseverance; and nonplanning impulsiveness comprised subsets labeled self-control and cognitive complexity. That the bipolar patients would be distinguished by increased levels of attentional impulsiveness, which has been defined as a lack of ability to focus on a task and a tendency toward racing thoughts and distractibility,22 is not surprising. Bipolar disorders, but not BPD, are often characterized by the disturbances of cognition captured by the attentional impulsiveness subscale. Conversely, higher levels of nonplanning impulsiveness, defined by Patton and colleagues as a difficulty with planning actions carefully and thinking about consequences of actions,22 might be expected with BPD patients, who are often characterized in part by impulsive behaviors with high likelihood of self-harm.
Evidence from studies of neuropsychological deficits associated with each of the disorders also lends support to the differences found between BPD and bipolar II disorder. For example, deficits in sustained attention are typically seen in both manic23 and euthymic24 bipolar patients but not in uncomplicated BPD patients.25 In contrast, executive functioning deficits are characteristic of BPD.25 Although the literature is mixed,26 some recent studies have shown that the severity of executive functioning deficits in bipolar patients varies with mood state27 and episode type (mania versus hypomania).28 In addition, motor control may be related to what is generally referred to as behavioral disinhibition, a trait hypothesized to create a predisposition to disruptive behavior disorders and, perhaps, also bipolar disorders and BPD.29
The second hypothesis, that there would be group differences on the measure of subjective depression severity only, was also supported. When symptoms of depression were rated by a clinician, both MDD and bipolar II patients were rated as similarly depressed. The additional diagnosis of BPD did not appear to have an effect on clinician-rated symptom severity. This approximate equivalence of clinician-rated depression severity between diagnostic groups has also been demonstrated by previous research with bipolar I patients30 and bipolar II patients,31 when compared to patients with unipolar depression. In contrast, when symptoms were assessed with a self-report measure, both of the BPD-diagnosed groups reported more severe symptoms of depression than the patients without Axis II diagnoses. In order to better understand the differences between the groups, we conducted post hoc analysis of 6 factor scores computed for the HAM-D. We found that the discrepancy between the clinician-rated depression scores and the self-report scores could mainly be accounted for by higher severity scores on 2 factors. The BPD groups experienced higher levels of cognitive symptoms (guilt, suicidal ideation, depersonalization, paranoid ideation, and obsessional thoughts) and higher levels of anxiety-related symptoms than patients without BPD.
These findings support the notion that depressed BPD patients may have a distinct depressive syndrome that distinguishes them from patients without personality disorders, regardless of whether they are diagnosed with MDD or bipolar depression. A key feature of this syndrome seems to be a more severe subjective experience of their symptoms. This finding is supported by research that has demonstrated the unique pattern of affective symptoms typically seen in BPD patients,32,33 as well as the various deficits in emotion regulation that are characteristic of BPD, particularly those that show an increased sensitivity to negative emotional states.34 In a recent article,10 we have also argued that BPD patients have a unique experience of depression. We compared depression severity in MDD patients with and without BPD and reported a similar discrepancy in an unrelated sample.10 Overall, the findings suggest that bipolar II patients are not distinguishable from patients with MDD when assessed for depression severity and that there are unique mood-related phenomena associated with BPD that distinguish BPD patients from patients without personality disorders.
To summarize, while hostility does appear to fully distinguish patients with BPD from those with bipolar II disorder, the presence of both BPD and bipolar II disorder seems to be associated with a higher level of impulsiveness than either diagnosis independently. However, while the data suggest that impulsiveness is an important aspect of both disorders, it appears that BPD is associated with a higher level of impulsiveness overall than bipolar II disorder. The results of the depression scale analyses suggest that BPD patients can be distinguished from patients without personality disorders regardless of the nature of the Axis I pathology. Taken together, the results of this investigation suggest that there is a unique symptom and trait profile uniquely associated with BPD that distinguishes the diagnosis from bipolar II disorder.
Although several studies have concluded that impulsiveness distinguishes BPD patients from bipolar II patients,3,35 our findings suggest that different facets of impulsiveness are associated with each diagnostic syndrome, and, more importantly, that there is a compounding effect associated with a diagnosis of both bipolar II disorder and BPD. This finding not only suggests a degree of independence between the diagnoses but also suggests that patients with this combination of disorders could have a particularly high risk for self-destructive or damaging behavior, such as suicide attempts and self-injury. Impulsiveness predicts severity of suicide attempts in bipolar patients36 and is a prospective predictor of suicidal behavior in BPD patients.37
There are several limitations to this research. First, the sample is relatively small, particularly the bipolar groups. Future studies with larger sample sizes will be important in validating these findings. In addition, the fact that there was an unequal distribution of inpatients and outpatients in the groups also may have undermined the reliability of the findings. A study including an equal percentage of inpatients and outpatients, across groups, would increase the generalizability of the conclusions of this research. Moreover, we did not include a group with BPD alone. Although this group is relatively rare, as 80% or more of those with BPD have comorbid mood disorders, it may be useful to have this group as a comparison group. Finally, this research relies primarily on self-report measures of depression, impulsiveness, and hostility. As we have previously demonstrated that self-report measures of depression severity may be discrepant with clinician-rated measures,10 the possibility exists that the same discrepancies could be present between self-reports and more objective measures of impulsiveness (e.g., neuropsychological performance) or hostility (e.g., measures of aggressive behavior). Future research comparing self-rated and objective measures of traits such as these will be of great value in further clarifying the distinction between the disorders.
Despite the aforementioned limitations, the results of this research provide further evidence that bipolar II disorder and BPD are distinct diagnostic entities and that the presence of both disorders leads to a compounding effect that increases the severity of some types of symptoms. In addition, our finding that each diagnosis is associated uniquely with a different facet of impulsiveness suggests that there may be distinct neuropathology underlying each disorder. Additional research is needed if we are to fully understand the differences between these disorders.
Acknowledgments
This work was funded in part by grants MH 48514, MH 62185, MH 59710, MH 61017, and MH 62665 from the National Institute of Mental Health and grant AA 15630 from the National Institute on Alcohol Abuse and Alcoholism.
Footnotes
The authors of this article report no financial or other relationships relevant to the subject matter of this research or the results described herein.
References
- 1.Brieger P, Ehrt U, Marneros A. Frequency of comorbid personality disorders in bipolar and unipolar affective disorders. Compr Psychiatry. 2003;44:28–34. doi: 10.1053/comp.2003.50009. [DOI] [PubMed] [Google Scholar]
- 2.Atre-Vaidya N, Syed H. Borderline personality disorder and bipolar mood disorder: two distinct disorders or a continuum? J Nerv Ment Dis. 1999;187:313–315. doi: 10.1097/00005053-199905000-00010. [DOI] [PubMed] [Google Scholar]
- 3.Henry C, Mitropoulou V, New AS, et al. Affective instability and impulsivity in borderline personality and bipolar II disorders: similarities and differences. J Psychiatr Res. 2001;35:307–312. doi: 10.1016/s0022-3956(01)00038-3. [DOI] [PubMed] [Google Scholar]
- 4.Delito J, Martin L, Riefkohl J, et al. Do patients with borderline personality disorder belong to the bipolar spectrum? J Affect Disord. 2001;67:221–228. doi: 10.1016/s0165-0327(01)00436-0. [DOI] [PubMed] [Google Scholar]
- 5.Perugi G, Toni C, Travierso MC, et al. The role of cyclothymia in atypical depression: toward a data-based reconceptualization of the borderline-bipolar II connection. J Affect Disord. 2003;73:87–98. doi: 10.1016/s0165-0327(02)00329-4. [DOI] [PubMed] [Google Scholar]
- 6.MacKinnon DF, Pies R. Affective instability as rapid cycling: theoretical and clinical implications for borderline personality and bipolar spectrum disorders. Bipolar Disord. 2006;8:1–14. doi: 10.1111/j.1399-5618.2006.00283.x. [DOI] [PubMed] [Google Scholar]
- 7.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- 8.Zanarini MC, Frankenburg FR, Hennen J, et al. The McLean Study of Adult Development (MSAD): overview and implications of the first six years of prospective follow-up. J Personal Disord. 2005;19:505–523. doi: 10.1521/pedi.2005.19.5.505. [DOI] [PubMed] [Google Scholar]
- 9.Swann AC, Pazzaglia P, Nicholls A, et al. Impulsivity and phase of illness in bipolar disorder. J Affect Disord. 2003;73:105–111. doi: 10.1016/s0165-0327(02)00328-2. [DOI] [PubMed] [Google Scholar]
- 10.Stanley B, Wilson ST. Comparing subjective and clinician ratings of depression in borderline personality disorder. J Personal Disord. 2006;20:307–318. doi: 10.1521/pedi.2006.20.4.307. [DOI] [PubMed] [Google Scholar]
- 11.Spitzer RL, Williams JBW, Gibbon M, et al. Structured Clinical Interview for DSM-III-R/DSM-IV. New York, NY: New York State Psychiatric Institute; 1990. Patient Edition. [Google Scholar]
- 12.First MB, Spitzer RL, Gibbon M, et al. Structured Clinical Interview for DSM-IV Axis II Personality Disorders. New York, NY: New York State Psychiatric Institute; 1996. [Google Scholar]
- 13.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Beck AT, Ward CH, Mendelson M, et al. An inventory for measuring depression. Arch Gen Psychiatry. 1965;12:63–70. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 15.Barratt ES. Impulsivity: integrating cognitive, behavioral, biological, and environmental data. In: McCown WB, Johnson LJ, Sure MB, editors. The Impulsive Client: Theory, Research, and Treatment. Washington, DC: American Psychological Association; 1994. pp. 39–56. [Google Scholar]
- 16.Buss AH, Durkee A. An inventory for assessing different kinds of hostility. J Consult Psychol. 1957;21:343–349. doi: 10.1037/h0046900. [DOI] [PubMed] [Google Scholar]
- 17.Stevenson J, Meares R, Comerford A. Diminished impulsivity in older patients with borderline personality disorder. Am J Psychiatry. 2003;160:165–166. doi: 10.1176/appi.ajp.160.1.165. [DOI] [PubMed] [Google Scholar]
- 18.Soloff PH, Kelly TM, Strotmeyer SJ, et al. Impulsivity, gender, and response to fenfluramine challenge in borderline personality disorder. Psychiatry Res. 2003;119:11–24. doi: 10.1016/s0165-1781(03)00100-8. [DOI] [PubMed] [Google Scholar]
- 19.Hamilton M. The Hamilton Rating Scale for Depression. In: Guy W, editor. ECDEU Assessment Manual for Psychopharmacology. Rockville, Md: US National Institute of Health, Psychopharmacology Research Branch; 1976. pp. 179–190. [Google Scholar]
- 20.Paris J, Zweig-Frank H, Ng Ying Kin NMK, et al. Neurobiological correlates of diagnosis and underlying traits in patients with borderline personality disorder compared with normal controls. Psychiatry Res. 2004;121:239–252. doi: 10.1016/s0165-1781(03)00237-3. [DOI] [PubMed] [Google Scholar]
- 21.Skodal AE, Gunderson JG, Pfohl B, et al. The borderline diagnosis 1: psychopathology, comorbidity, and personality structure. Biol Psychiatry. 2002;51:936–950. doi: 10.1016/s0006-3223(02)01324-0. [DOI] [PubMed] [Google Scholar]
- 22.Patton JH, Stanford MS, Barratt ES. Factor structure of the Barratt Impulsiveness Scale. J Clin Psychol. 1995;51:768–774. doi: 10.1002/1097-4679(199511)51:6<768::aid-jclp2270510607>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- 23.Clark L, Goodwin GM. State- and trait-related deficits in sustained attention in bipolar disorder. Eur Arch Psychiatry Clin Neurosci. 2004;254:61–68. doi: 10.1007/s00406-004-0460-y. [DOI] [PubMed] [Google Scholar]
- 24.Clark L, Kempton MJ, Scarnà A, et al. Sustained attention-deficit confirmed in euthymic bipolar disorder but not in first-degree relatives of bipolar patients or euthymic unipolar depression. Biol Psychiatry. 2005;57:183–187. doi: 10.1016/j.biopsych.2004.11.007. [DOI] [PubMed] [Google Scholar]
- 25.Lenzenweger MF, Clarkin JF, Fertuck EA, et al. Executive neurocognitive functioning and neurobehavioral systems indicators in borderline personality disorder: a preliminary study. J Personal Disord. 2004;18:421–438. doi: 10.1521/pedi.18.5.421.51323. [DOI] [PubMed] [Google Scholar]
- 26.Malhi GS, Ivanovski B, Szekeres V, et al. Bipolar disorder: it's all in your mind? the neuropsychological profile of a biological disorder. Can J Psychiatry. 2004;49:813–819. doi: 10.1177/070674370404901204. [DOI] [PubMed] [Google Scholar]
- 27.Malhi GS, Ivanovski B, Hadzi-Pavlovic D, et al. Neuropsychological deficits and functional impairment in bipolar depression, hypomania and euthymia. Bipolar Disord. 2007;9:114–125. doi: 10.1111/j.1399-5618.2007.00324.x. [DOI] [PubMed] [Google Scholar]
- 28.Torrent C, Martínez-Arán A, Daban C, et al. Cognitive impairment in bipolar II disorder. Br J Psychiatry. 2006;189:254–259. doi: 10.1192/bjp.bp.105.017269. [DOI] [PubMed] [Google Scholar]
- 29.Hirshfeld-Becker DR, Biederman J, Calltharp S, et al. Behavioral inhibition and disinhibition as hypothesized precursors to psychopathology: implications for pediatric bipolar disorder. Biol Psychiatry. 2003;53:985–999. doi: 10.1016/s0006-3223(03)00316-0. [DOI] [PubMed] [Google Scholar]
- 30.Mitchell PB, Wilhelm K, Parker G, et al. The clinical features of bipolar depression: a comparison with matched major depressive disorder patients. J Clin Psychiatry. 2001;62:212–216. [PubMed] [Google Scholar]
- 31.Benazzi F. Prevalence of bipolar II disorder in outpatient depression: a 203-case study in private practice. J Affect Disord. 1997;43:163–166. doi: 10.1016/s0165-0327(96)01421-8. [DOI] [PubMed] [Google Scholar]
- 32.Abela JRZ, Payne AVL, Moussaly N. Cognitive vulnerability to depression in individuals with borderline personality disorder. J Personal Disord. 2003;17:319–329. doi: 10.1521/pedi.17.4.319.23968. [DOI] [PubMed] [Google Scholar]
- 33.Bellodi L, Battaglia M, Gasperini M, et al. The nature of depression in borderline depressed patients. Compr Psychiatry. 1992;33:128–133. doi: 10.1016/0010-440x(92)90010-n. [DOI] [PubMed] [Google Scholar]
- 34.Wagner AW, Linehan MM. Facial expression recognition ability among women with borderline personality disorder: implications for emotion regulation. J Personal Disord. 1999;13:329–344. doi: 10.1521/pedi.1999.13.4.329. [DOI] [PubMed] [Google Scholar]
- 35.Benazzi F. Borderline personality–bipolar spectrum relationship. Prog Neuropsychopharmacol Biol Psychiatry. 2006;30:68–74. doi: 10.1016/j.pnpbp.2005.06.010. [DOI] [PubMed] [Google Scholar]
- 36.Swann AC, Dougherty DM, Pazzaglia PJ, et al. Increased impulsivity associated with severity of suicide attempt history in patients with bipolar disorder. Am J Psychiatry. 2005;162:1680–1687. doi: 10.1176/appi.ajp.162.9.1680. [DOI] [PubMed] [Google Scholar]
- 37.Yen S, Shea MT, Sanislow CA, et al. Borderline personality disorder criteria associated with prospectively observed suicidal behavior. Am J Psychiatry. 2004;161:1296–1298. doi: 10.1176/appi.ajp.161.7.1296. [DOI] [PubMed] [Google Scholar]


