Abstract
The apolitical legitimacy of "evidence-based medicine" offers a practical means for ethnography and critical social-science-and-humanities-of-health theory to transfer survival resources to structurally vulnerable populations and to engage policy and services audiences with urgent political problems imposed on the urban poor in the United States that harm health: most notably, homelessness, hyperincarceration, social service cut-backs and the War on Drugs. We present four examples of collaborations between ethnography and clinical research projects that demonstrate the potentials and limits of promoting institutional reform, political debate and action through distinct strategies of cross-methodological dialogue with epidemiological and clinical services research. Ethnographic methods alone, however, are simply a technocratic add-on. They must be informed by critical theory to contribute effectively and transformatively to applied health initiatives. Ironically, technocratic, neoliberal logics of cost-effectiveness can sometimes render radical service and policy reform initiatives institutionally credible, fundable and capable of generating wider political support, even though the rhetoric of economic efficacy is a double-edged sword. To extend the impact of ethnography and interdisciplinary theories of political-economic, cultural and disciplinary power relations into applied clinical and public health research, anthropologists--and their fellow travelers--have to be able to strategically, but respectfully learn to see through the positivist logics of clinical services research as well as epidemiological epistemology in order to help clinicians achieve--and extend--their applied priorities. In retrospect, these four very differently-structured collaborations suggest the potential for "good-enough” humble scientific and political strategies to work for, and with, structurally vulnerable populations in a punitive neoliberal era of rising social inequality, cutbacks of survival services, and hyperincarceration of the poor.
Introduction
Anthropology’s version of participant-observation ethnographic methods has carved out a productive space within the social sciences as a creative, but unruly, stepchild. Anthropologists maintain their methodological feet very much on the ground but keep their theoretical head in the thin, provocative, air that straddles the social sciences and the humanities. In the health sciences, however, participant-observation is not, for the most part, on the radar screen and qualitative methods remain underdeveloped and, for the most part, subordinated or openly distrusted. Quantitative experimental methods are the basis for clinical scientific credibility. To be considered valid, replicable and generalizable, research measures must be conceptually focused and unambiguously quantifiable--preferably based on biological endpoints: sero-markers rather than behavioral self-report. The gold-standard arbiter of modern evidence-based medicine is the double-blind randomized controlled trial (RCT) which stratifies research subjects to two or more treatment alternatives with a placebo arm in order to test the most basic questions of relative effectiveness of specific behavioral, pharmacological, and or/technological therapies.
In public health and medicine, the methodological term "ethnography" when it is used at all, generally refers to a standardized research protocol that would not be recognized by most anthropologists as valid: One-shot, enumerated, formal interviews conducted in an unnatural office environment that is often hampered by the bizarre hoops of arcane regulatory protocols that limit access to "human subjects." Health researchers often use vague, somewhat oxymoronic or even Rorschach terms to describe their version of ethnographic interviews, including "semi-structured" and "guided by grounded theory." To an anthropologist this would raise concerns that the interviews might promote impressions management discourses.
In contrast, anthropology's version of ethnographic methods strives to document context, process and meaning. Methodologically, the goal of clinical research is to rule out alternative explanations, while ethnography is attuned to the contradictory nature of social life. In fact, during the 1980s/1990s with the rise of post-modern critiques of facticity, Euro-centric discourses of linear progress (Clifford & Marcus, 1986), and the brutal legacy of colonialism in North/South relations (Asad, 1973), anthropologists, if anything, over-developed their self-critical faculties teetering on practical, collaborative and political paralysis. They are great at documenting the contradictions of power constraints, exceptionalisms, complications, ambiguities and the positionalities of all research participants, including both the subjects and the practitioners. Some epidemiologists might interpret these valuable self-critical theoretical anthropological concerns over the social constructedness of truth as potentially useful for identifying systemic bias or confounding variables, but many quantitative researchers simply ignore ambiguity and inconsistency by dismissing it as statistical noise that can be "controlled for" with a large enough sample size determined through a statistical technique called "power analysis." In this techno-scientific epistemology, there is little room for thinking about "power" in terms of social relations that affect health outcomes. Instead, the epidemiological term "power" is limited to statistical measurement practices. In fact, to receive National Institutes of Health (NIH) funding most quantitative studies must justify the value of their science with a "statistical power analysis."
Despite these deep epistemological differences, there exists the potential for productive scientific and political engagement in cross-methodological collaboration with ethnography's ability to contribute to a more complexly robust “best practices research” alert to history, social structure and the unequal power relations that damage health. The case studies that follow seek to highlight both the potential and limits of anthropological engagement with the positivist logics of quantitative epidemiology and even, at times, with cost-benefit analysis. For social scientists studying the roots of poverty in the long shadow of the punitive neoliberal turn since the 1980s, such collaboration can, in certain instances, allow for meaningful improvements in the lives of the poor and marginalized.
For the past two-and-a-half decades, Philippe Bourgois (PB), an anthropologist located in medical schools, has been attempting to bring participant-observation anthropological methods and critical theory--at times openly but sometimes by stealth--into direct, practical dialogue with epidemiology and clinical research. Most challenging, but potentially most productive have been collaborations with random controlled public health trials and large exploratory prospective studies of medically underserved indigent populations. We present four case studies where distinct strategies of ethnographic engagement with different types of clinical, service, research and policy reform initiatives promoted institutional and political changes with varying success.
The first two ethnographic initiatives contributed to the initiation of quantitatively-organized clinical pilot-tests of new medical procedures and service deliveries for indigent patients in the San Francisco County Hospital. The third initiative is a still-ongoing randomized controlled HIV-prevention behavioral trial testing a Paolo Freire educational model of critical consciousness-raising among inmates cycling through Philadelphia’s county jails system. The fourth initiative, in alliance with community-based AIDS activists, used a technical review by medical students of the “evidence-based scientific literature” on "best-medical-practices for the destitute sick," to pressure politicians to allocate funds for subsidized housing for the HIV-positive homeless.
Case 1: Founding an Outpatient Abscess Clinic at the San Francisco County Hospital
From 1994 through 2007 PB was conducting participant-observation ethnographic fieldwork in the homeless encampments of an extended social network of heroin injectors and crack smokers in San Francisco. Consistent with the HIV-prevention mandate of his NIH mandate, he and his ethnographic team focused their observations on the micro-details of potentially risky injection practices. They added a photo-ethnographic component to document practices visually in real time in the natural environment (Philippe Bourgois & Schonberg, 2009). Their first medically-applied observation was that, in contrast to East Coast cities where white powder heroin prevailed, the heroin in San Francisco consisted exclusively of “Mexican black tar” and appeared to be generating severe soft-tissue infections among chronic street-based injectors. They soon realized that "abscesses" were the health pathology of primary concern to local injectors, and were the main reason the homeless sought care in the County Hospital emergency department. Unfortunately, systematic hospital records of this major health problem were not being tabulated, and no national or international best-practices standard existed for the surgical care for soft-tissue infection caused by injection drug use. Virtually the entire San Francisco ethnographic cohort complained that surgeons at the County Hospital had cut into them without anesthesia and refused to prescribe them painkillers for aftercare. They bore extensive bodily evidence of post-operative consequences from clearly invasive procedures (scars and open wounds). Sympathetic nurses in the emergency department confirmed that occasionally clinicians refused to provide patients with analgesia and cut more widely and deeply than necessary. Usually this kind of purposefully punitive care was delivered by physicians in training who were unprepared to treat intoxicated patients and had become angry at seeing so many patients with self-inflicted pathologies.
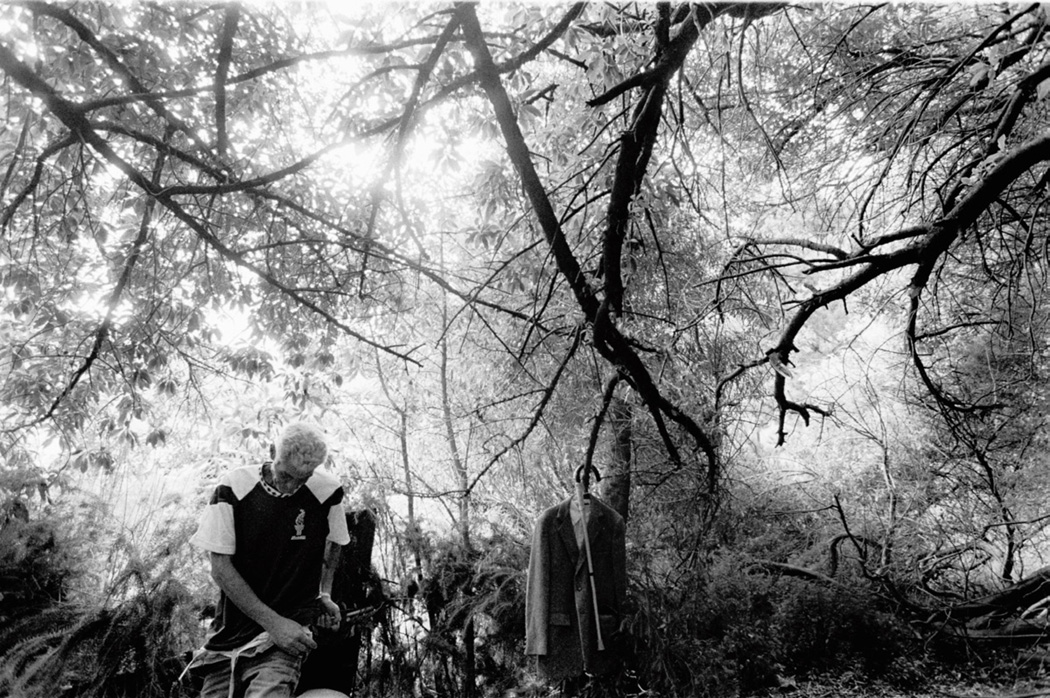
A fieldnote with the accompanying photograph (see photograph 1: "Sonny seeks help from Spider-Bite Lou for post-surgical pain and infection after his release from the County Hospital") illustrates the human cost of this pattern of iatrogenic wounding:
[Ethnographic Team Fieldnote]
Sonny was released from the hospital two days ago following an overnight abscess surgery. He cringes from pain every time a gust of wind passes over his open gash. [INSERT Copy Editor Please Wrap text of fieldnote around Photo 1]
The surgeon refused to provide Sonny with a prescription for painkillers on the grounds that they are “medically contra-indicated for heroin addicts” and neglected to provide him with an extra bandage.
Lou, a newcomer to the encampment, with a big "spider bite abscess" on the back of his neck, digs a small medical kit out of his shopping cart, overflowing with the aluminum cans he fished out of the gutter this morning. His hands are black with grease and dirt, but he does not pause to wash them. (There is no soap or running water available.) He delicately picks the lint out of Sonny’s wound and dabs it with antibiotic ointment. He then wraps Sonny’s biceps with a shred of gauze and reassures
Sonny, 'I know how much it hurts! They done that to me too. I packed it lightly to keep the wind out.' (Philippe Bourgois & Schonberg, 2009:101-106).
Photograph 1.
"Sonny seeks help from Spider-Bite Lou for post-surgical pain and infection after his release from the County Hospital" © Jeff Schonberg
Not surprisingly, in response to this hospital-based mistreatment, drug users routinely lanced their own abscesses in unsterile homeless encampments and delayed seeking professional care. When they eventually reached the hospital their pathologies were often more severe, resulting in prolonged, painful and expensive stays in the intensive care unit.
Alarmed, the ethnographic team began documenting soft-tissue infections photographically (see Photographs 1 and 2) and PB contacted Dan Ciccarone (DC), a Family and Community Physician with a Masters in Public Health known for his culturally competent clinical expertise in caring for injectors. DC began delivering urgent care to this grossly underserved population in their natural environment. Surprised by what appeared to be systemic mistreatment by surgeons at the County Hospital, DC consulted the hospital's database and calculated that "soft-tissue infections" represented the largest single admissions category in the hospital (over 4,000 per year) and incision-and-drainage, the typical surgical procedure, was the most frequent of all procedures. The protocol at the time involved a deep debridement of the surrounding tissue that required general anesthesia and an expensive overnight inpatient stay. The outcome was often painful, disfiguring and prolonged post-operative recovery. Surgeons considered this wide excision necessary, nevertheless, to minimize the risk of necrotizing fasciitis, a rare but potentially fatal condition. In contrast, in the homeless shooting encampments DC engaged in a minimally invasive incision-and-drainage procedure that effectively healed all of the cases he encountered with negligible scarring (Ciccarone et al., 2001). (See Photo 2: Photograph 2: "PB comforts Spider-Bite Lou while DC, under a street lamp, treats the neck infection that earned Lou his nickname".) [Copyeditor INSERT Photo 2 HERE]
Photograph 2.
"PB comforts Spider-Bite Lou while DC, under a street lamp, treats the neck infection that earned Lou his nickname" © Jeff Schonberg
From 1998 through the early 2000s, PB and DC began presenting these findings, including the photographs in hospital grand rounds and medical school lectures. In late 2000, two surgeons at the County Hospital invited PB and DC to be advisors on a quantitative pilot study using a one-group pre-post design in which treatment for patients with abscesses was transitioned to a simple incision-and-drain procedure performed in a specialized outpatient soft-tissue clinic. They prioritized pain management and recruited experienced clinicians committed to what they called "compassionate" healthcare for injection drug-users. The surgeons initially expressed interest in a simultaneous qualitative study of their new clinic to complement their statistical outcomes data. They objected, however, to DC’s suggestion we measure the size of their incisions to make it an outcome statistic capable of documenting quantitatively the objective details of the transformation of their surgical procedure and our interface with the pilot was curtailed.
Instead, the surgeons kept a careful record of the financial savings produced by shifting from an inpatient to an outpatient surgical procedure and their exclusively quantitative results were uniformly positive. There were no after-care complications with the new simple incision-and-drain procedure. In the twelve months after the creation of the outpatient clinic, emergency department visits to the County Hospital decreased 33.9%, and inpatient operating room procedures decreased 71% (producing a net savings of approximately $8.77 million dollars), and patient satisfaction was 86%. Exceptionally few patients were deemed “treatment failures” (2%) and relatively few were "lost to follow-up” (14%). Given this patient population’s vulnerability to negative institutional interactions with healthcare providers (30% homeless, 62% either had Hepatitis B, Hepatitis C or HIV), these quantitative outcomes were considered remarkably successful. A formal “Integrated Soft-Tissue Infection Services” outpatient clinic was immediately founded. The surgeons published the positive quantitative findings in the leading surgical peer-reviewed journal (Harris & Young, 2002), presenting their minimally invasive pain-free incision-and-drain outpatient procedure with emphasis on local analgesics as an evidence-based best-clinical practice to establish a national standard of specialized outpatient care for underserved injectors.
This case study demonstrates a positive change in surgical practice and medical care stemming from an indirect and aborted research collaboration between ethnography and cost-effective analysis. The ethnographic research preceded the quantitative and clinical initiative. The presentation of several years of photographically-documented ethnographic data prompted the statistical recognition of the problem and may have played a role in the technical design of the pilot. The cross-methodological dialogue with epidemiology, however, only occurred at the outset when the soft tissue statistics were identified and tabulated in the unwieldy and difficult-to-access County Hospital database by DC. This collaboration was not a randomized controlled-trial, or a cohort study, or even a case-control study—in fact, there was no control group. The decisiveness of cost savings and excellent quantifiable clinical outcomes was sufficient to render the change in practice self-evident and permanent. In the next study, the same combination of preliminary ethnography followed by best-medical-practices and quantitative clinical cost-effectiveness research initiated institutional change--but with disappointing longevity.
Case 2: Establishing Wider Spectrum Social Services through the Emergency Department
The same ethnographic data that prompted PB and DC to collaborate and reach out to surgeons to alter medical care practices revealed the need for a more fundamental change in institutional practice in primary care at the County Hospital to promote systematic medical attention to the socio-economic conditions both inside and outside the hospital that were turning predictably vulnerable patients into victims of useless suffering suspended in a near-death limbo. Federal reductions in Medicare reimbursements initiated in 1997 were propelling county hospitals across the country into financial crisis. The San Francisco County Hospital responded by imposing “early release plans” onto expensive, uninsured patients and instituting a prescription co-payment for indigent outpatients (Philippe Bourgois & Schonberg, 2009). During that period, PB was Chair of a department in the medical school that staffed the County Hospital.
[PB Fieldnote]:
At this month’s Department Chairs’ Meeting, the Medical School’s Chief Hospital Administrator presents an Armageddon scenario of finances. The County Hospital is having trouble retaining doctors and nurses because “of burnout;” a medical staff shortage has caused them to divert 41% of emergency medical vehicles to other sites. There is no longer any trash pickup in non-patient areas. An epidemic of antibiotic-resistant streptococcus erupted in the Intensive Care Unit, forcing them to shut down cleaning services in the rest of the hospital in order to assign all the limited cleaning personnel to the ICU (Bourgois and Schonberg 2009, 236).
The negative health outcomes of these budget cuts were "ethnographically visible" among the homeless heroin injectors the ethnographic team was following on the street. One of the team's research participants, Hank, began cycling in-an-out of the County Hospital's emergency rooms, largely because he could not access sanitary shelter and minimal sustenance or drug treatment that could have curbed the opiate withdrawal symptoms that compelled him to continue heavy manual labor despite suffering from a spinal infection, double pneumonia, and seizures. Each time he was admitted through the emergency room, he would qualify temporarily for state-of-the-art, expensive, high-tech medical care (e.g. CAT scans, MRIs, biopsies) in the intensive care unit. As soon as his fever was stabilized, however, his clinicians ordered his early release in accordance with the new cost-accounting protocols instituted by the hospital's "utilization review" administrators. Hank would hobble back to his homeless encampment under the freeway, with a brand-new cane, issued by the hospital because his x-rays revealed fractured vertebrae. Sometimes he was also given clean clothes but often no medication or analgesic therapy. [Copyeditor INSERT PHOTO 3 HERE] (See Photograph 3: "Hank injecting in his camp immediately after his early releases from the hospital with a new cane, a suit of clothes but no pain relief prescription".) Predictably, Hank was unable to meet the hospital's new co-pay requirements for his spinal infection medication, and he was immediately lost to follow-up after each release. Eventually his fever would flare up again sufficiently for him to collapse in a seizure on the street qualifying him for another round of high-tech inpatient care at the County Hospital (Philippe Bourgois & Schonberg, 2009).
Photograph 3.
"Hank injecting in his camp immediately after his early releases from the hospital with a new cane, a suit of clothes but no pain relief prescription" © Jeff Schonberg
The ethnographic team's findings on the link between the absence of outpatient social service follow-up and the pattern of repeat cycling by the homeless through high tech emergency services were introduced into the new required curricula on “socially vulnerable populations” that was being developed for residents and medical students at the County Hospital (King & Wheeler, 2007). One of the innovations of this new curriculum on the social determinants of health was to bring an "attending anthropologist" as a faculty member into the case conference presentations by medical residents on "patients with conditions complicated by substance use." Coincidentally one of the cases presented by a senior primary care resident were Hank’s repeated cycles of "loss to follow-up care" prompting an anthropologically-informed discussion of practical clinical strategies to remedy the mismatch of high-tech care and rachitical basic survival services.
During this period (in 2001) a High Utilizer Case Management program was created at the County Hospital to address the “bio-psycho-social needs” of high-frequency users of the emergency room through the intensive case management model. The program selected patients with the most serious and chronic conditions including congestive heart failure, emphysema requiring oxygen therapy, renal failure requiring dialysis, or cirrhosis. An evaluation survey from 2004 documented that two-thirds of the High Utilizer patients were homeless or unstably housed; 70% had concomitant mental illness; and 80% had alcohol and substance use problems. The initiative was justified to administrators and funding agencies by the hypothesis that intensive case management would reduce costs and improve patient outcomes by addressing the lack of coordination between high-tech medical care and social service provision. The High Utilizer program assigned each patient an interdisciplinary team that included a social worker, a public health nurse, a psychiatrist, an internist, and clerks who met twice weekly to formulate individualized treatment plans. The team's priority was to connect patients to safe and adequate housing, job opportunities, reliable transportation, and community-based, primary-care clinical and social services. The coordinator of the program, probably not coincidentally, was the former senior resident who had presented Hank's case a few years earlier when PB was participating as an attending anthropologist at one of the case conferences on patients with substance abuse complications.
The clinicians conducted a quantitative and clinical case-history study of an initial year-long cohort of 15 patients in the High Utilizer program documenting dramatic decreases per patient in the median number of Emergency Room visits (from 4 to 2) and median in-patient hospital days (from 23 to 10). Linkage to primary care increased as did median outpatient clinical visits (from 2 to 16). In the 2005 annual report, the High Utilizer program director presented socio-economically complex clinical case histories of patients as evidence of the improvement in the quality of care (Schneidermann, 2005):
Mr. DG is a 22-year-old African American male who is paraplegic secondary to a gunshot wound suffered four years ago when he was fleeing from a gang related incident and was shot by police. Since becoming paralyzed, DG has been hospitalized multiple times for debridement… [and] again for another gunshot wound inflicted by a rival gang member in 2002. When DG was referred to HUCM [High Utilizer Case Management], he reported that he was homeless and living in his car, unable to find wheelchair accessible housing (page 6).
The team responded to this kind of social structural challenge by obtaining:
Section 8 housing. DG now lives in [a] neighborhood, safely housed away from gang territory." They also liaised with "legal representation to find an equitable sentence… [allowing the team] to attend to medical issues… coordinate plastic surgery and orthopedics follow-up, [including] In- Home-Support-Services… daily living needs [assistance], paratransit taxi vouchers… weekly delivery of medication., etc (page 6).
The report demonstrated the ability of clinicians to engage with diverse institutional services outside the confines of the hospital to improve both biological and quality-of-life outcomes. Although initially justified as a resource-saving endeavor, the program was not able to save the hospital money consistently each year and the initiative was one of the first line items cut from the hospital budget during the 2007–2008 recession.
The next two case studies demonstrate different modes of collaboration between ethnography and quantitative epidemiology. Both are self-consciously political: the first is an RCT to test the effects of political critique and mobilization on carceral-to-community reentry outcomes; the second, and last, was a political mobilization in the name of evidence-based science for more housing resources for the homeless ill. These collaborations began with very different strategies of interdisciplinary alliance-building. Both embraced quantitative epidemiology from the start. The RCT collaboration strives to produce new, original research data that expands the limits of traditional quantitative behavioral health services science to address structural and political-level challenges. INSERT PB In contrast, in the first two case studies already presented a preliminary independent anthropological critique of existing services only subsequently prompted institutional change. Ironically, the ethnographic/quantitative dialogue in those first two relatively successful institutional-reform cases was arguably more passive-aggressive than it was methodologically complementary or collaborative.
Case 3: Teach Inside, Teach Outside (TITO) in the Philadelphia County Jail
This collaboration is a, still on-going, HIV-prevention motivational behavioral change RCT for an exceptionally politically and medically vulnerable population: US jail inmates. They suffer from 300 percent higher HIV infection rates than the general population, and most are also chronic consumers of illegal drugs (Maruschak, 2008). Jeff Draine (JD), a social work professor trained as a quantitative health services researcher, approached an activist community-based HIV-rights organization, Philadelphia FIGHT, to adapt their already existing infrastructure and pedagogy into a community re-entry intervention capable of accommodating the rapid turnover of the jail system (Draine et al., 2011). Their pilot program, TITO, framed its HIV prevention program as an anti-carceral political consciousness-raising intervention modeled on the pedagogy of Paulo Freire (1970) to identify the political-economic structural determinants of ill health among jail inmates.
Prevailing public health programs in jails rely on individual-level case management to facilitate linkages to treatment and services. Social work referral processes, however, normally take longer than the modal jail stay of two days. The hostile overcrowded jail environment further hinders case-finding as inmates are loath to reveal health problems--especially HIV--in a chaotic, often homophobic jail context. Furthermore, existing carceral services are underfunded and overburdened. The RCT strives to reach out to this vulnerable population with a radical political message about the structural injustice of black hyperincarceration. Its quantifiable outcomes measure the prevention of HIV, substance abuse, violence, carceral recidivism and successful graduation from the program (Draine et al., 2011).
JD anticipated the difficulty of evaluating a socially complex and purposefully charismatic behavioral RCT through discrete quantifiable outcome measures. He was concerned that if the RCT collected solely conventional quantitative outcome measurements, the study might confirm a null hypothesis finding confounded by the nonlinear complexity of potentially partially beneficial, but inconsistent or inadequately supported, measurement of the transformative impact of the intervention (Draine et al., 2011). Furthermore, inspirational motivational protocols are by definition, vulnerable to the effects of service-provider charisma/skill that can render quantification artificial and unrealistic. Consequently, JD invited PB to integrate a participant-observation ethnographic component spanning all stages of the project. The goal was to document the "logics for social processes" generated by political activism/consciousness-raising as well as the interface of participants with the larger "structural HIV risk-environment" of the Philadelphia region. This allowed the researchers to extend the ethnography into the natural environment of recently incarcerated and released participants to better explain and contextualize the meaning and potential causal pathways of the quantitative data being collected.
The NIH funded this purposeful political health activism project, including its robust ethnographic component, for five years. To our surprise, in the mayhem of the Philadelphia County Jail's intake units, researchers and service-providers find themselves side-by-side explaining to inmates the institutional racism of US carceral policies through the zero-tolerance "War on Drugs." In these classes, inmates, service providers and formerly imprisoned peer-leaders discuss legal rights, human rights, positive experiences of political activism and self-determination, and practical strategies for negotiating or circumventing carceral bureaucratic obstacles. The inmates are invited to continue these discussions upon their release in a twelve-week curriculum for recently released arrestees. The “outside classes” deliver preventative health messages, facilitate access to social services, host individualized strategy sessions and organize support groups. They also claim to establish a safe space to address the trauma of lives trapped in chronic bouts of incarceration. Occasionally participants burst into tears and hug one-another. Sadly, however, relatively few are obtaining employment, stable housing and treatment and too many are falling victim sooner, rather than later, to re-incarceration.
The unusual methodological prominence of participant-observation in JD’s NIH proposal prompted multiple requests for written clarifications by the NIH study section as a condition for releasing funding for the research. In contrast, no questions were asked about the anti-carceral, anti-racist, anti-big-business-profiteering political content of the seminars. The project is still ongoing, but its determination to marry two methods commonly viewed as insoluble in the health services field offers an especially productive space for anthropological collaboration beyond that of the first two cases where an externally-positioned sequential deployment of anthropological critique was followed by anthropologically-inspired but independently operationalized epidemiological analysis and clinical intervention.
Case 4: Housing for People Living with HIV in Philadelphia
The final initiative was not technically speaking a cross-methodological collaboration to generate new research data. It was designed as a political intervention and we include it in this discussion because it strategically combined already-existing quantitative medical data with ethnographic accounts of personal suffering to create an ostensibly neutral best-practices-medicine consensus statement (Consensus Statement HIV/AIDS in Philadelphia, 2010). That document mobilized doctors and public health workers to pressure the Mayor's office of Philadelphia to allocate money for emergency housing for indigent people living with AIDS.
In 2010, ACT-UP Philadelphia, an AIDS activist group with a long history of direct action (and an overlapping relationship with Philadelphia FIGHT, the organization administering TITO), began an advocacy campaign to end the waitlist for housing-support for low-income Philadelphians living with HIV. The effort was spurred, in part, by the personal narrative of a charismatic member of ACT-UP, Cliff Williams, who had been chronically homeless. Cliff recounted how after losing their home he and his wife, both HIV positive, had moved between homeless shelters and sidewalks. Sleeping in communal bedrooms in the city’s shelters, he contracted scarlet fever and his CD4 count dropped to 203. His antidepressant medicines were stolen, and he faced discrimination from other residents when his HIV status was disclosed by staff insisting he declare the contents of his medication.
Years later he recounted the difficulty of adhering to medication while homeless:
"Living a transient lifestyle like I was, moving from place to place, you might not be able to find water, or just a private place to hash out all those pills…When I was on the streets and the temperature went down to 30 degrees, it kicked my neuropathy off. (Martin, 2011).
After the death of his wife and another eighteen months of homelessness, Cliff finally secured housing from a publicly funded mental health program. He responded well to AIDS medication and became an activist in ACT-UP. The organization collected several accounts by survivors with stories similar to Cliff's that demonstrated the link between health and subsidized housing. During the late 2000s and early 2010s, at any given time between 100 and 200 people living with full-blown AIDS found themselves on Philadelphia's two-year-long waitlist for federally-financed housing subsidies--too many continued to die on the streets (City of Philadelphia, 2012). Furthermore, city regulations excluded HIV-positive individuals from the waitlist until they could prove a diagnosis of full-blown AIDS. Active drug and alcohol users were also disqualified from housing assistance. Several large US cities (New York, Boston, San Francisco) in the late 2000s already supplemented federal funding for housing the HIV-positive indigent with local municipal funds to reduce waiting times.
ACT-UP published their qualitative findings in an advocacy report distributed to community organizations, homeless shelters, and government offices. In keeping with the group’s commitment to direct action, they organized protests and demanded to meet with the Mayor of Philadelphia. They were ignored, however, and sought an alternative strategy to leverage political officials. Luke Messac (LM), a medical student and member of ACT-UP, offered to conduct a Pubmed literature search of the relationship between housing status and HIV treatment. The quantitative literature is large and virtually all studies revealed a significant, positive relationship effect of housing status on HIV health outcomes (For a meta-review see Leaver et al., 2007).
Combining the ethnographic data from ACT-UP’s qualitative interviews with his review of the quantitative health literature, LM asked PB to circulate a "Medical and public health consensus statement on housing as treatment and prevention for HIV/AIDS in Philadelphia” to his colleagues at the University of Pennsylvania Medical School. Within less than 3 weeks over 80 physicians and public health professionals in Philadelphia signed the statement which was later published as an opinion-editorial in the Philadelphia Inquirer (Philippe Bourgois & Nunn, 2010). The op-ed presented the "scientific basis for housing assistance as a cost-effective treatment and prevention measure for HIV," and advised the Mayor to authorize municipal funds to address this "medical emergency."
The local media was sympathetic to this "declaration of best clinical practices” and published several follow-up articles. Speaking to the media during demonstrations outside City Hall, Cliff proved politically potent for the housing campaign. [Copyeditor INSERT PHOTO 4 HERE] (See Photograph 4: "Biopolitics in action: Cliff in front of the Mayor's Office demanding, in the name of health, housing for the structurally vulnerable".) The politically and institutionally imposed suffering in Cliff's struggle to survive with AIDS on the streets outraged fellow ACT UP members, while the gentleness of his presentation style and the positive outcome of his medical case made him an easy, worthy ally for social scientists averse to confrontation and wary of social pathology.
Photograph 4.
""Biopolitics in action: Cliff in front of the Mayor's Office demanding, in the name of health, housing for the structurally vulnerable" © ACT-UP Philly
Personal (ethnography-style) narrative and quantitative epidemiology, when deployed together, proved more potent than either alone. All of a sudden professors, students along with formerly homeless ACT-UP activists living-with-AIDS found themselves meeting in City Hall as a delegation with the Mayor's office and Philadelphia’s city councilors. City policy was changed in accordance with ACT-UP’s housing first, harm reduction demands: 1) criteria for entering the city-run, federally-funded Housing Opportunities for Persons with AIDS (HOPWA) program were loosened to include HIV-positive individuals without full-blown AIDS; 2) an independent comprehensive needs-assessment for unstably housed people living with HIV was established; and 3) active drug and alcohol users were allowed access to housing vouchers. Unfortunately, however, the City failed to allocate additional municipal funds to supplement the already existing federal housing assistance budget for people with HIV.
Discussion: The Political Neutrality of Quantitative Research
The four case studies above outline diverse strategies for bringing ethnography and critical social-science-and-humanities-of-health theory into dialogue with clinical research methods. They reveal how the health community's commitment to “best clinical practices” can: 1) promote resource transferal and service delivery to the poor; 2) enable practical institutional policy reform; and 3) generate public political debate to wider audiences without distracting polemics. Ethnography played very different roles as a research method in each case and achieved different types of limited, but overall positive, applied results in each case.
The first case of the founding of the outpatient soft-tissue clinic for indigent injectors and the establishment of a national standard of care for treating abscesses through a minimal incision-and-drain procedure complemented by adequate analgesics had the most immediate and long-term practical effect on the lives of the indigent poor, but it was the least political and most immediately cost-effective in the short-term. Ethnography in that collaboration prompted the compilation of the basic clinical statistics that rendered objectively visible to administrators and clinicians the fact that abscesses represented the single largest admissions category at the County Hospital. The multiple hospital-based grand-rounds presenting photo-ethnographic documentations of the deep wounds of homeless injectors also identified the systematic and costly iatrogenic pain suffered by a pariah population in urgent need of more effective and compassionate medical care. At a more basic science level, the simple ethnographic identification of the prevalence of black tar on the West Coast of the United States expanded clinical understandings of the important, logistical health effects caused by the chemical differences in the types of heroin distributed across the United States by organized crime (Mexican black tar versus Colombian white powder) (Ciccarone & Bourgois, 2003).
We should be wary, however, about overstating the impact of ethnography in the hospital institutional context. Independent, cost-cutting logics rendered the San Francisco County Hospital administration receptive to establishing an outpatient abscess clinic: Over 4,000 surgical in-patient procedures per year performed almost exclusively on uninsured patients represented a financial burden. Furthermore, although PB and DC were initially consulted by the surgeons in the design of the clinic, the project was not a collaboration. The surgeons were offended by DC's suggestion that they document the decrease in the size of the incision and ethnographic access to data collection inside the new outpatient clinic was not facilitated. In the official surgical publication, there is no mention of the large and painful iatrogenic wounds of the hospital's former in-patient procedure. The potential for an institutional critique and the reconceptualization of medical care for a vulnerable population was lost. Instead, the technical expertise of the surgeons was reaffirmed, and any contribution of anthropology or ethnography was forgotten or ignored.
The second case at the same County Hospital of the initiation of a High Utilizer pilot program that delivered multidisciplinary, integrated care to (expensive) vulnerable patients proved institutionally fragile because of its inability to document consistent cost-effectiveness despite excellent clinical outcomes. The collaboration, however, may have at the very least contributed to a more robust, longer-term political-pedagogical commitment by County Hospital clinicians to extend the biomedical gaze to the larger community through the development of a new required curriculum for socially vulnerable populations. Once again, the initial exploratory ethnography identified--or at least rendered more visible to the hospital--the painful mismatch between social work outpatient services and high-tech medical care. Like the first case, this collaboration was a more sequential anthropological-clinical dialogue rather than a complementary quantitative/qualitative research project. Nevertheless, the curriculum for socially vulnerable populations continues to be one of the San Francisco County Hospital’s defining features, attracting outstanding medical students and residents from around the country. At the very least, this case illustrates the practical political, pedagogical and support service potential for an anthropological/clinical critically theoretically applied dialogue based on mutual trust and shared commitment to the underserved.
Once again, however, we should be wary of overstating the capacity for anthropology and ethnography to impact medical institutions. The San Francisco County Hospital has always attracted physicians who are exceptionally politically-committed and dedicated to underserved pariah populations. These kinds of clinicians are inherently receptive to cultural and political-economic critiques of the reductionist biological gaze of modern medicine (Farmer, 2006; Kleinman, 1995). Nevertheless, the complex case history of the gunshot-disabled gangster, “DG,” presented in the annual report of the High Utilizer team demonstrates the potential for health professionals to reach well beyond the boundaries of the clinic. Most impressive was the ability of the clinicians caring for the patient DG to subordinate law enforcement priorities to the needs of state-of-the-art community-based, interdisciplinary medical care at a moment in US history when the US carceral population was rising exponentially.
The ability of the disciplines of health services and clinical treatment to compete with law enforcement and over-rule punitive priorities in favor of managing the pathologies of poverty supportively was most dramatically illustrated in the TITO collaboration, which enabled researchers and service providers--even those with felony records--to circulate through the Philadelphia County Jail with ease to administer the behavioral HIV-prevention RCT for inmates. On this research project, we have been allowed to meet privately with inmates in virtually any part of the sprawling Philadelphia County Jail system seven days a week from 8:00am to 11:00pm. These interviews are conducted in the "official visit" room reserved for lawyers, clergy and other professional visitors. No time limits are placed on the sessions. Frequently the guards supervising the visiting rooms praise their work. They believe TITO's therapeutic outreach project makes their jobs easier by calming and focusing potentially volatile inmates on positive health messages. They do not interpret the intervention as politically subversive. In retrospect, this finding is not surprising. It is theoretically insightful. The project's positive relationship to many of the guards offers a post-social-welfare-state illustration of Foucault's insights on the normalizing effects of “biopower” within the complex processes of modern “governmentality.” We became unwitting agents of a punitive governmentality within the micro-apparatus of the County Jail despite, perhaps naively, initially thinking of ourselves as promoting an anti-carceral politics.
Foucault’s understanding of the rise of the importance of rehabilitative biopower in the emergence of the modern state (Foucault, 1995) helps us understand why the quantitative scientific neutrality of RCTs and epidemiological research are so politically disarming. Foucault argued that the development of population statistics laid the basis for modern clinical and epidemiological science as well as for the disciplines of economics, criminology, social work, psychiatry and related social service fields that "subjectivate" (Butler 1997) populations. Health statistics were especially important in the long-term transition to the modern state during the eighteenth and nineteenth centuries shifting from a logic of "sovereignty" that exacts obedience through bloody repression, to one of biopower that monitors, organizes and promotes the health and wellbeing of obedient citizens (Foucault 1978):140-144). Power operates through infinite webs of governmentality that may continue to include physical repression (punitive law-enforcement) but are primarily deployed through categorizing (i.e. diagnosis in the discipline of medicine) in order to regulate large population groups. Most notably this takes the positive, or neutral, form of vaccination campaigns, censuses, declarations of best-clinical-practices, but it also identifies non-normative populations for confinement and punishment--or more ambiguously, for rehabilitation.
Foucault's conceptualization of how the "knowledge/power" nexus subtly and unconsciously disciplines citizens by promoting rights, responsibilities and exclusions is useful for comprehending the ostensibly neutral potential for the high stakes political persuasiveness of RCT research. The double-blind quantitative research model involves an especially radical “disappearance of the self” in a discourse of knowledge that mimics the logics of laboratory science, centered on "impersonal and disinterested procedures (Porter, 1992:31)". RCTs require an elaborate administrative personnel to conduct representative sampling, bureaucratic consenting procedures, random assignation to placebo-arms, equivalently standardized logistics, and protection from the contamination-effects of subjective bias on both experimental subjects and researchers. This complex anti-subjective methodology is central to the "rhetorical power" of RCTs as being politically neutral, objective arbiters. Furthermore, in their cost-effective pursuits of magic-bullet solutions the health sciences bias themselves against complicated structural interventions and erase the political context of health and science production. This explains why the NIH did not critique the TITO project for its political education component but rather for its unusual interdisciplinary method of robust participant-observation throughout all stages of an RCT identifying structural risk-environment forces.
A growing body of public health literature critiques the limitations of quantitative measurement and advocates for structural-level interventions (Quesada et al., 2011; Rhodes et al., 2005). Researchers increasingly recognize that local policy environments and other structural factors external to an RCT's experimental design may alter outcomes and obscure intervention effects. Statistically discrete variables by definition confound complex social processes--especially those laden with the complicated power relations and cultural ideologies that characterize substance abuse and poverty (Philippe Bourgois & Hart, 2011). The often contradictory effects of overlapping social power vectors are unlikely to have linear health effects. Ethnography is ideally situated to collect precisely these kinds of complex “process data” (Smyth & Schorr, 2009; Toroyan et al, 2004; Wolff, 2000). It can identify the systemic bias, contamination and other intervention effects that confound epidemiologists. Most importantly, when guided by critical social science understandings of power relations and subjectivity formation in historical and contemporary context, a processual qualitative analysis can enhance explanatory power, explain causality and recognize the logic for unforeseen outcomes. It can also propose new hypotheses and themes for ongoing inquiry. Arguably, the ethnographic/epidemiological cross-methodological collaboration has the most potential for generating new scientific data in a format comprehensible to epidemiologists in the case of the ongoing jail-based RCT.
The last case of ACT-UP’s Philadelphia HIV-housing initiative was an indirect outcome of TITO’s political idealism, highlighting the potential of ethnography’s subjects to be agents of social change. Many of the formerly homeless people-with-HIV whose stories were chronicled in ACT-UP’s reports and publications were leaders in the campaign to expand city funding for housing. Some of these subject-activists were graduates of Project TEACH, an earlier iteration of TITO. Furthermore, the critical medical anthropology concept of structural vulnerability (Quesada et al., 2011), supplemented by a Foucauldian understanding of the potential of a politicized subjectivation (Butler 1997) through demands for biological citizenship (Kalofonos, 2010; Petryna, 2002), along with the example of solidary health-services practice by the anthropologist-physician Paul Farmer and his Partners-in-Health human rights movement (Kidder, 2003) inspired both the medical students and PB to engage with Philadelphia housing politics with the HIV-homeless. Nevertheless, it was the dispassionate voice of quantitative evidence--especially the RCT literature cited in the medical consensus statement--that rendered the Philadelphia initiative of the homeless advocate movement successful. It would have been impossible to mobilize over 80 medical school faculty, students and health professionals on such short notice by circulating a best-clinical-practices statement based on ethnographic evidence. The media followed and politicians were obliged to make modest public policy changes in the midst of a recession. Once again, the collaboration was strictly politically-instrumental to increase access to health services for the HIV-homeless. It was not designed as a research or scientific knowledge production project.
Despite their very different interfaces with the cross-methodological production of clinical services dialogue these ethnographic cases all demonstrate that supportive social services for vulnerable populations framed as cost-effective, best-clinical-practices validated by quantitative scrutiny, are capable of mobilizing surprisingly broad support for distributing resources for the "unworthy poor" in the neoliberal era. However, all these case studies also demonstrate the heavy fist of cost-effectiveness as a central disciplining force of contemporary biopower. The line-item termination of the San Francisco County Hospital's High Utilizer program and the city of Philadelphia’s unwillingness to allocate more funding to reduce the homeless housing waitlist demonstrates that, for public health and clinical interventions involving social services, the most intransigent obstacle is not the “diffusion” of progressive scientific evidence to policymakers or administrators of clinical services but rather the political will and funding criteria of municipal government (see distinctions raised by Green et al., 2009). The preeminent logic in both cases proved to be a certain kind of cost-effectiveness, one whose short time horizon does not allow for the realization of preventive benefits amply documented by "the science," i.e., RCTs and quantitatively-measured statistically significant outcomes.
The early twentieth century pioneers of cost-benefit analysis were life insurance actuaries and academic economists who used their method to argue that state investments in public heath would produce a net economic benefit by increasing production (Porter, 1992). By contrast, in the post-industrial neoliberal era the same calculations are deployed to justify reductions in social service spending. Cost-effectiveness needs to be recognized as anti-ethical. For example, Philadelphia’s Commissioner of Public Health dismissed ACT-UP's evidence that city funding for housing would ultimately save public spending on hospital visits by the uninsured, because the hyper-local vision of bureaucratic funding streams allocate certain city housing costs from the municipal budget, while hospital savings accrue to federally-financed health programs.
Conclusion: The Good-Enough Politics of Clinical Science for the Specific Intellectual in the Contemporary Neoliberal Era
Bringing participant-observation methods into conversation with epidemiological data enables an analysis that is richer than the sum of the parts and benefits both sides of an unfortunate qualitative versus quantitative research divide. Clinically oriented participant-observation research can enable epidemiological findings to develop "socially plausible causal explanations for quantitative associations (Bourgois et al., 2006:1811; see also Ciccarone 2003)" by documenting contextual and processual data that are too complex for measurement as individual quantitative variables. Ethnographic fieldwork requires long-term interpersonal contact with research participants in their natural environment and obliges academics to straddle social power divides. It often involves the purposeful violation of de facto apartheid divisions of social class, ethnicity and normativity that structure many, if not all, societies to greater or lesser extents and that profoundly affect health and quality-of-life chances. When combined with anthropology’s basic heuristic principle of cultural relativism, the result can be inherently destabilizing to power, privilege, and fossilized common sense (Bourgois, 2011). In the discipline of anthropology, ethnographic methods also benefit from the guidance of critical social-science-and-humanities theory. In the four cases presented, we build on insights from Foucault’s concepts of governmentality, biopower, the disciplinary knowledge/power nexus and the clinical gaze, as well as political-economy interpretations of class-based structural vulnerability, rising social inequality and political hostility toward the “unworthy poor” under contemporary neoliberalism. Notwithstanding this theoretical armature we demonstrated the strategic political and scientific value of a humble hands-on practical service engagement with quantitatively-oriented clinical and health behavior science on its own atheoretical positivist terms to help it understand its own statistics more usefully.
Unfortunately, when standing alone, ethnographic data and critical theoretical analysis have little credibility in larger policy debates and appear to be politically biased. When brought into collaborative dialogue with quantitative health and social services data, however, they achieve a much wider political reach. Ironically, it is precisely the failure to recognize social context and politics on the part of the clinical gaze, and the experimental quantitative research model that opens a creative political space for the delivery of valuable resources to the poor through the logics of best-clinical practices. Critical insights on social inequality and health achieve a much wider credibility when in dialogue with epidemiological data derived from controlled experiments because this form of quantitative health science research has convinced both its practitioners and the general public that its methods are "evidence-based" positioning it above-politics.
Few policy/service arenas in the United States generate more polarization than harm reduction for injection drug users, subsidies for HIV treatment/prevention and homelessness, and critiques of the hyperincarceration of poor African Americans. Nevertheless, our four ethnographic/epidemiological collaborative/dialogue initiatives raised no political anxieties. The RCT format and quantitative cost-benefit analysis proved to be the most politically neutral format, but all four projects, even the ones that arguably failed, exposed wider medical and social services audiences to radical alternative political and policy debates in a non-polemical format. The projects, at the very least, also distributed some economic resources, services and accompaniment to underserved, stigmatized populations: the homeless, illegal drug injectors, the indigent ill, and prisoners.
The practical and deeper epistemological barriers to cross-methodological and interdisciplinary theoretical dialogue between anthropology and the clinical and health services sciences need to be acknowledged. Epidemiologists seek to eradicate subjectivity while ethnographers base their science on a critical self-awareness of positionality. Furthermore, few researchers on either side of the methodological divide are fully literate in one another's disciplinary logics. To quantitative health researchers, ethnographic data and critical theory often appear to be politically biased and anecdotal. Vice versa to ethnographers, epidemiologists often appear naively blind to theory and oblivious to how they shape their quantitative data by the way they conceptualize, phrase and administer their questionnaires. The easiest way to bridge the disciplinary theoretical and methodological gulf between anthropologists and quantitative health researchers is to recognize the practical win/win benefits of augmenting the "validity and generalizability" of one another's data. As we have argued, the cross-methodological dialogue can be especially productive for RCT behavioral health trials that generate large quantities of federal research funding to support complex logistics for distributing services and resources to often underserved populations. In fact, an argument can be made that the current design of most behavioral health RCTs may be wasting the productive scientific potential of the research funds invested in them. Too often they document the null hypothesis because the non-linear complexity of social processes affecting individual behavior change defy statistical significance at the level of discrete outcome variables.
An additional valuable analytical and representational/methodological finding that emerged unexpectedly from these collaborations is the power of photo-ethnography both as a documentary tool and as an effective means of representation that carries exceptional political, emotional and analytical valence. Early into his ethnography of homeless heroin injectors in San Francisco, PB sought out a photo-ethnographer as a long-term collaborator and co-author because he feared that his field-notes would not be believable. The routinized, everyday physical suffering and health risks faced by indigent drug users were too extreme to be conveyed through text alone. Furthermore, public health and hospital grand rounds presentations, unlike those in anthropology settings, have to be delivered with PowerPoints to have scientific credibility. We included three examples of the kinds of photos that several of the co-authors have used in presentations to clinicians. They provide visual corroboration of the practices and conditions described in ethnographic fieldnotes to clinicians whose access to vulnerable populations is limited to the safe, clean and controlled confines of clinics or hospital beds. The photographs also serve as a historical record. For example, had we not documented the excessive surgical carving--misnomered debridement--that was being performed on the soft tissue infections of homeless injectors during the 1990s at the San Francisco County Hospital (see Photograph 1) there would be no historical memory of that routinized iatrogenic wounding. Furthermore, exposure to the painful content of photographs of indigent addiction serves a political function in-and-of-itself by unveiling the public secret of homelessness that most people in the United States walk, or drive by, every day without noticing.
Because of the marginality of qualitative research in policy debates, ethnographers who want to reach beyond the boundaries of their disciplines have to be the ones who take the first step to reach out to their quantitative colleagues. It is surprising that more anthropologists, especially those in the growing interdisciplinary field of ‘Science Studies’ do not make more of an effort to enter the world of positivist researchers with strategic humility. This should be especially easy for anthropologists who only need to expand their disciplinary tenet of cultural relativism that respects the logics of ‘exotic others’ to the world of medical science researchers. By respectfully withholding disciplinary judgments anthropologists can, temporarily at least, see the world through the quantitative logics of epidemiologists and clinical service providers. Furthermore on a practical level, to have full access to the universe of a quantitative researcher, anthropologists have to roll up their sleeves and engage with a hermeneutics of generosity in the practices of daily life among the people they study--just as they might do to access any interesting social or cultural setting. In the case of cross-methodological collaborations this requires jumping into the hard work of improving health outcomes and demonstrating credible results in the quantitative terms believed, as a matter of scientific common sense by their interlocutors: their collaborators' deeply held cultural web of highly-valued meaning--to borrow phrases from Geertz (1973). In fact, anthropologists must self-consciously and self-critically avoid appearing discipline-centric in order for collaborations to succeed. They have to resist the easy temptation to aggressively deconstruct facts or problematize reality in a manner that will appear disrespectful or competitive to epidemiologists. The magic of anthropology is precisely its ability to self-critically live with the almost schizophrenic contradiction of adhering to two worlds simultaneously. Anthropologists are trained to remain self-critical outsiders in the new insider’s world that they temporarily strategically--even emotionally--embrace to study. One of the more creative challenges, consequently, is to translate complex, epistemologically threatening anthropological insights on the social construction of facts and the partiality of reality (and the subjectivity-producing effects of power) into practical terms useful to quantitative researchers. Our experience suggests this dialogue can be fun even as it is useful to push epidemiologists to recognize more of the meaning in their already existing data, and expand their definition of legitimate data.
Moving away from the practical compromise of dialogue we can combine insights from Foucault and political-economy with the self-critical insights of postmodernism and anthropological cultural relativism, to critique the limitations of most conventional health promotion interventions in the United States that primarily target individuals by promoting behavior change at the individual level through imparting knowledge, skills and motivation. These kinds of psychological behavioral interventions may save many individual lives but they leave untouched the systematic production of new generations of structurally vulnerable populations. It is time for a long-term theoretical paradigm shift in the applied fields of health promotion to return epidemiology to its mid-19th century roots in social medicine and focus on the pathological health effects of both the material political-economic infrastructure and the symbolic contours of social inequality (Quesada et al., 2011; Rhodes et al., 2005).
The biggest contradiction we confronted in our four collaborations, however, was not methodological, epistemological or theoretical. It was political, driven by the cost-benefit analysis increasingly imposed onto public health research and clinical services by neoliberal forms of governmentality. Ultimately in almost every case, except that of the outpatient abscess clinic, our strategic embrace of cost-effectiveness rhetoric to generate institutional interest and research funding ultimately backfired. The San Francisco County Hospital's High Utilizer Program, successfully reduced inpatient hospitalizations and improved quality-of-life for the indigent by increasing access to services, (Schneidermann 2005; see also Okin et al., 2000)--but it was terminated by budget cuts (Schneidermann 2012). It is cheaper to let the uninsured indigent die painfully and ultimately that bottom line appeals to institutions governed by neoliberal logics.
As Farmer (2006) has argued persuasively, health must be conceptualized as a universal human right. Rather than righteously disengaging with the limits of the cost-effective hegemony in public health, however, we follow Foucault's (1984:71) call for “specific intellectuals” to take political positions through their ability to navigate “technico-scientific” practical details at the interstices of biopower and governmentality. We are also extending Nancy Scheper-Hughes' (1992:28) call for anthropologists to break out of the political paralysis of the insights of postmodern self-criticism/ deconstruction and instead "practice… a 'good-enough' ethnography" that combines the scientific and political potentials of collaborative, cross-methodological public health research. To borrow a phrase from Foucault's tongue-and-cheek lecture series title, "structurally vulnerable populations must be defended." The punitive neoliberal turn in US politics since the 1980s increasingly defines the non-normative poor as being unworthy of public services. Clinical collaborations provide uniquely neutral opportunities to redefine indigent pariahs as society's most immediate practical and political responsibility.
Collaborating with quantitative research extends political impact of anthropology
Ethnographic/quantitative methodological dialogue expands data collection potential
Critical social science theory expands political impact of clinical research
RCT format enables resource distribution to underserved stigmatized populations
Behavioral RCTs benefit from ethnography to document socially-complex processes
Cross-methodological dialogue in health research is especially productive for RCTs
Acknowledgements
Primary research funding provided by National Institutes of Health grants: DA010164, DA027204, DA27599. Comparative and background data supported by grants: AA020331, DA027689, MH076068. Editorial assistance by Keahnan Washington.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Luke Messac, Email: lukemessac@gmail.com, University of Pennsylvania, Department of History and Sociology of Science.
Dan Ciccarone, Email: Ciccaron@fcm.ucsf.edu, University of California San Francisco, Department of Family & Community Medicine.
Jeffrey Draine, Email: jeffdraine@temple.edu, Temple University, Department of Social Work.
Philippe Bourgois, Email: pbourgois@gmail.com, University of Pennsylvania, Departments of Anthropology and Family Medicine & Community Health.
References
- Asad T, editor. Anthropology & the colonial encounter. London: Ithaca Press; 1973. [Google Scholar]
- Bourgois P. Lumpen abuse. City and society. 2011;23:2–12. doi: 10.1111/j.1548-744X.2011.01045.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bourgois P, Hart LK. The structural vulnerability imposed by hypersegregated US inner city neighborhoods. Addiction. 2011;106:1975–1977. doi: 10.1111/j.1360-0443.2011.03615.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bourgois P, Nunn A. Too long a wait for housing. Philadelphia inquirer. 2010 [Google Scholar]
- Bourgois P, Schonberg J. Righteous dopefiend. Berkeley: UC Press; 2009. [Google Scholar]
- Bourgois P, Martinez A, Kral A, Edlin B, Schonberg J, Ciccarone D. Reinterpreting ethnic patterns among white and African American men who inject heroin. PLoS Medicine. 2006;3:1805–1815. doi: 10.1371/journal.pmed.0030452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butler J. The psychic life of power. Stanford University Press; 1997. [Google Scholar]
- Ciccarone D. With both eyes open. International Journal of Drug Policy. 2003;14:115–118. [Google Scholar]
- Ciccarone D. Heroin in brown, black and white. International Journal of Drug Policy. 2009;20:277–282. doi: 10.1016/j.drugpo.2008.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ciccarone D, Bamberger J, Kral A, Edlin B, Hobart C, Moon A, et al. Soft tissue infections among injection drug users--San Francisco, California, 1996–2000. Morbidity and Mortality Weekly Report. 2001;50:381–384. [PubMed] [Google Scholar]
- Ciccarone D, Bourgois P. Explaining the geographical variation of HIV among injection drug users. Substance Use & Misuse. 2003;38:2049–2063. doi: 10.1081/JA-120025125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- City of Philadelphia. City of Philadelphia homeless death review, 2009–2010. Philadelphia: 2012. < www.phila.gov>. [Google Scholar]
- Clifford J, Marcus G. Writing culture. Berkeley: UC Press; 1986. [Google Scholar]
- Consensus Statement HIV/AIDS in Philadelphia. Medical and Public Health Consensus Statement on Housing as Treatment and Prevention for HIV/AIDS in Philadelphia. Philadelphia: 2010. < http://www.housingistreatment.org/>. [Google Scholar]
- Draine J, McTighe L, Bourgois P. Education, empowerment and community-based structural reinforcement. International Journal of Law and Psychiatry. 2011;34:295–302. doi: 10.1016/j.ijlp.2011.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farmer P. Never Again? Tanner Lectures on Human Values. 2006;26:137–187. [Google Scholar]
- Foucault M. History of sexuality. New York: Pantheon Books; 1978. [Google Scholar]
- Foucault M. Birth of the clinic. New York: Vintage Books; 1994. [Google Scholar]
- Foucault M. Discipline and punish. New York: Vintage Books; 1995. [Google Scholar]
- Freire P. Pedagogy of the Oppressed. New York: Continuum; 1970. [Google Scholar]
- Geertz C. The interpretation of cultures. New York: Basic Books; 1973. [Google Scholar]
- Green L, Ottoson J, García C, Robert H. Diffusion theory and knowledge dissemination. Annual review public health. 2009;30:151. doi: 10.1146/annurev.publhealth.031308.100049. [DOI] [PubMed] [Google Scholar]
- Harris H, Young D. Care of Injection Drug Users with Soft Tissue Infections. Archives of Surgery. 2002;137:1217–1222. doi: 10.1001/archsurg.137.11.1217. [DOI] [PubMed] [Google Scholar]
- Kalofonos I. 'All I Eat Is ARVs'. Medical Anthropology Quarterly. 2010;24:363–380. doi: 10.1111/j.1548-1387.2010.01109.x. [DOI] [PubMed] [Google Scholar]
- Kidder T. Mountains beyond mountains. New York: Random House; 2003. [Google Scholar]
- King T, Wheeler MB, editors. Medical management of vulnerable and underserved patients. New York: McGraw-Hill Medical Pub. Division; 2007. [Google Scholar]
- Kleinman A. Writing at the margin. Berkeley: UC Press; 1995. [Google Scholar]
- Leaver C, Bargh G, Dunn JR, Hwang S. The effects of housing status on people living with HIV. AIDS and Behavior. 2007;11:85–100. doi: 10.1007/s10461-007-9246-3. [DOI] [PubMed] [Google Scholar]
- Martin S. Shelter from the storm. POZ magazine. 2011 Jun; Online. [Google Scholar]
- Maruschak L. Medical problems of prisoners. Bureau of Justice Statistics. 2008 http://bjs.ojp.usdoj.gov/content/pub/pdf/mpp.pdf.
- Okin R, Boccellari A, Azocar F, Shumway M, O'Brien K, Gelb A, et al. The effects of clinical case management on hospital service use among ED frequent users. American Journal of Emergency Medicine. 2000;18:603–608. doi: 10.1053/ajem.2000.9292. [DOI] [PubMed] [Google Scholar]
- Petryna A. Life exposed. Princeton: Princeton University Press; 2002. [Google Scholar]
- Porter T. Objectivity as standardization. Annals of Scholarship. 1992;9:19–59. [Google Scholar]
- Quesada J, Hart L, Bourgois P. Structural vulnerability. Medical Anthropology. 2011;30:339–362. doi: 10.1080/01459740.2011.576725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhodes T, Singer M, Bourgois P, Friedman S, Strathdee S. The social structural production of HIV risk among injecting drug users. Social science & medicine. 2005:1026–1044. doi: 10.1016/j.socscimed.2004.12.024. [DOI] [PubMed] [Google Scholar]
- Scheper-Hughes N. Death without weeping. Berkeley: UC Press; 1992. [Google Scholar]
- Schneidermann M. Annual Report: High User Case Management Program (July 2003 to December 2004) San Francisco: San Francisco General Hospital; 2005. [Google Scholar]
- Schneidermann M. E-mail communication, October 8, 2012. 2012 [Google Scholar]
- Smyth K, Schorr L. A call to rethink “evidence” for social interventions that work. Harvard Kennedy School Working Paper Series. 2009 < www.hks.harvard.edu/socpol/publications_main.html>.
- Torassa U. San Francisco Examiner, Page A1. 2000. Abscesses plague addicts, ravage city's health budget. [Google Scholar]
- Toroyan T, Oakley A, Laing G, Roberts I, Mugford M, Turner J. The impact of day care: the use of process evaluation within an RCT. Child: Care, Health and Development. 2004;30:691–698. doi: 10.1111/j.1365-2214.2004.00481.x. [DOI] [PubMed] [Google Scholar]
- Wolff N. Using RCTs to evaluate socially complex services. The Journal of Mental Health Policy and Economics. 2000;3:97–109. doi: 10.1002/1099-176x(200006)3:2<97::aid-mhp77>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]