Abstract
Background
European studies have shown that itch is a widespread symptom, yet little is known about its frequency in the U.S.
Objective
To describe ambulatory care visits to clinicians in the U.S. for which itch was coded as a patient symptom.
Methods
This study uses retrospective data from the National Ambulatory Medical Care Survey from 1999–2009.
Results
Itch was coded as a symptom for an average of 7 million visits per year or approximately 1% of all outpatient visits, which was nearly 40% of the number of visits for the symptom of low back pain. Patients seen in visits for itch were more likely to be black or Asian than other patients (20% vs. 14%). They were also more likely than other patients to receive a new medication (68% vs. 36%) and were over twice as likely to receive two or more new medications (31% vs. 14%).
Limitations
Secondary datasets may not optimally capture patient reports and some of the procedures or medications may have been ordered for reasons other than itch.
Conclusion
Visits to clinicians for itch represent a sizeable proportion of ambulatory care visits in the US, and research on the epidemiology, treatments, and causes of itch should be a priority.
Keywords: itch, pruritus, skin, NAMCS, National Ambulatory Medical Care Survey, epidemiology, outpatient, clinic, clinic visits, quality of life
INTRODUCTION
Itching can arise from many common disease processes and be very bothersome to patients.1, 2 Although European studies suggest that itching is widespread,3–9 little is known about the frequency of itch as a complaint in outpatient offices in the United States.2, 10 Our goal was to estimate the frequency of itch that clinicians’ offices judged as a symptom associated with an outpatient visit in the U.S. from 1999–2009, and to describe aspects of the care delivered in these visits.
METHODS
Compilation of study sample
We studied data from the National Ambulatory Medical Care Survey (NAMCS), a nationally representative survey conducted by the US National Center for Health Statistics within the Centers for Disease Control and Prevention. This ongoing, annual survey samples outpatient visits by non-federally employed office-based physicians who are predominantly involved in direct patient care.11 The survey defines geographical segments (counties, groups of counties, county equivalents) within the U.S. as its primary sampling unit (PSU) and uses a multistage probability design of PSUs, physician practices within PSUs, and patient visits within these practices as its first, second, and third stage probability samples, respectively.12
Item response rates for NAMCS surveys are generally 95% or higher. All survey coding were subject to quality control measures involving a 10% independent sample verification procedure. For nonmedical coding items, the coding error rate was 0.1 percent. For items which required medical coding, coding error rates ranged between 0.2 and 0.5 percent.
To respond to the NAMCS, the physician or office staff records information about patients and the clinical encounter, including demographics, source of payment, presenting symptom, diagnoses, diagnostic tests and procedures ordered or performed, referrals made, and medications prescribed.13 We applied patient visit weights adjust for sampling probability and clustering effects to create nationally representative estimates of outpatient visits.14 Any population estimates with a standard error of greater than 30% or with fewer than 30 observations were considered unreliable and are not reported.
We compiled data from the 11-year period from 1999–2009 for this study. For analysis of medications and procedures, we used data from only 2005–2009 because survey questionnaires in 2005 started to include a variety of procedural data and whether a medication was new or continued. All reported results are weighted to represent an annual average of patient visits in the overall US population, though we have also included absolute survey visit numbers in our tables for reference.
Definition of visit for itch
A visit for itch was defined (Table 1) in this analysis if it met either of the following criteria: 1) if any of the three patient-reported presenting symptoms included the word “itching,” whether it was listed as the primary complaint or not or 2) if any of the diagnosis codes were classified under the category “Pruritus and related disorders” by the International Classification of Disease, 9th Edition, Clinical Modification (ICD-9-CM) (698.0, 698.1, 698.2, 698.3, 698.8, 698.9).15 The category does not include many diagnoses that are often associated with itch, like atopic dermatitis or urticaria. A visit was excluded as a visit for itch if any of the patient-reported reasons for visit included throat itching, ocular itching, or Dermatitis factitia, which we regarded as distinct from cutaneous itching.
Table 1.
Definition of a Visit for Itch
| Reason for visit:
|
OR | ICD-9-CM Diagnosis Code:
|
|---|---|---|
| 1870.2: Skin itching | 698.0: Pruritus ani | |
| 1890.4: Scalp itching | 698.1: Pruritus of genital organs | |
| 1340.2: Eyelid itching | 698.2: Prurigo | |
| 1365.1: Ear itching | 698.3: Lichenification and lichen simplex chronicus | |
| 1605.4: Anal/rectal itching | ||
| 1715.4: Scrotal itching | 698.8: Other specified pruritic conditions | |
| 1765.3: Vaginal itching | 698.9: Unspecified pruritic disorder | |
| 1770.1: Vulvar itching |
Analytic strategy
The unit of analysis was the patient visit. To interpret the estimate of prevalence of visits for itch, we compared it to that for another common symptom, low back pain. We defined low back pain as either a reason for visit of low back pain, ache, soreness, or discomfort (reason for visit classification code 1910.1) or a diagnosis of low back pain, low back syndrome, or lumbalgia, (ICD-9-CM code of 724.2).
To understand more about the clinical encounters, we focused on three components of visits for itch. First, we described demographic characteristics of patients who presented to their physicians for itch. Second, we described the clinical services provided to the patient, including the most frequent diagnoses, procedures, and medications. Third, we described the plans for follow-up after these patient visits.
We compared characteristics of patient visits for itch to those of patient visits that were not for itch and calculated Pearson’s chi-squared tests for statistical significance. We assessed chronicity of the presenting symptom by calculating visits that were for an acute problem (less than three months onset) or a chronic problem (greater than three months onset, either routine follow-up or flare-up). We examined seasonal variation of visits for itch based on meteorological definitions of seasons: March 1 to May 31 is spring, June 1 to August 31 is summer, September 1 to November 30 is fall, and December 1 to February 28 is winter.
Though our definition for a visit for itch included visits that had either a presenting symptom or a diagnosis of itch, we were also interested in the clinician’s ultimate diagnosis for patients with a presenting symptom of itch. In order to determine the most common diagnoses for these patients presenting with itch, we analyzed all visits where itch was a presenting symptom (without using the diagnosis code for inclusion in this group) and rank ordered these visits by their primary diagnoses. For clinical services, we calculated the frequency of new medication prescriptions, blood tests, biopsies, wound care, and excisions. New medication prescriptions included both prescription and over-the-counter drugs that were newly ordered, administered, or supplied during the visit. Data from the 2004 U.S. Census (midway point between 1999 and 2009) were used to calculate per capita estimates.16
NAMCS uses the Multum Lexicon Drug Database to classify its medications. We rank ordered new medication prescriptions both based on their categorizations as defined in the Multum Lexicon Drug Database17, 18 and based on the following subgroups that we created specifically relevant to itch: topical steroids, topical steroids with anti-infectives, topical anti-infectives, other topical dermatological agents, antibiotics, and systemic steroids.
RESULTS
There were a total of 77 million visits for itch in the U.S. from 1999–2009, with an average of 7 million visits per year in the US over the 11 year period studied. The majority of visits (58.6%) were for a new problem lasting less than three months, but for nearly one third (32.0%), the major reason for the visit was described as chronic. Overall, approximately 0.8% of all physician visits per year were for itch. In comparison, 1.8% of all visits were for low back pain.
Demographics
Table 2 shows characteristics of visits for itch. Compared to patients seen for other reasons, a greater proportion of patients seen in visits for itch were between the ages of 25–44 years and greater than 75 years and were more often female. Patients seen in visits for itch were more likely to be black/African American or Asian than patients seen in visits for other reasons. For example, the patient was black/African American in 12% of visits for itch, compared with 10% of other visits. With respect to physician specialty, 28% of all visits for itch were seen by dermatologists, 36% by generalists, and 14% by gynecologists. However patients seen in visits for itch were similar to patients seen in other visits in terms of payment method and geographic location. The proportion of visits for itch compared to visits not for itch was higher in the summer (27.3% vs. 23.7%, p=0.02) and lower in the spring (25.1% vs. 27.9%, p=0.02), with no difference in visits in the fall (23.2% vs. 24.6%, p=0.34) or winter (24.5% vs. 23.8%, p=0.63).
Table 2.
Characteristics of Visits for Itch in the United States (1999–2009)
| Characteristics | % of Visits for Itch (95% CI) (N=2,423) | % of Visits Not for Itch (95% CI) (N=298,156) | P-value |
|---|---|---|---|
|
| |||
| Patient Age- years | |||
| Under 15 | 14.0 (12.1–16.2) | 16.5 (15.8–17.1) | 0.02 |
| 15 – 24 | 8.2 (6.8–9.8) | 7.8 (7.5–8.0) | 0.62 |
| 25 – 44 | 25.1 (22.7–27.7) | 21.6 (21.1–22.1) | <0.01 |
| 45 – 64 | 26.6 (24.4–29.0) | 28.4 (28.0–28.9) | 0.14 |
| 65 – 74 | 10.5 (9.0–12.2) | 12.6 (12.2–13.0) | 0.02 |
| ≥ 75 | 15.6 (13.8–17.7) | 13.2 (12.7–13.6) | 0.01 |
|
| |||
| Patient Sex | |||
| Female | 65.7 (62.8–68.6) | 59.0(58.6–59.4) | <0.01 |
| Male | 34.3 (31.4–37.2) | 41.0 (40.6–41.4) | <0.01 |
|
| |||
| Patient Racea | |||
| White | 79.8 (76.8–82.5) | 85.5 (84.4–86.6) | 0.01 |
| Black/African American | 12.3 (10.2–14.8) | 9.8 (9.0–10.7) | 0.01 |
| Asian/Native Hawaiian/Other Pacific Islander | 7.6 (5.6–10.0) | 4.0 (3.3–4.7) | <0.01 |
| American Indian/Alaska Native | 0.1 (.03–.5) | 0.4(.3–.5) | 0.10 |
| More than one race reported | 0.2 (.1–.6) | 0.3 (.2–.3) | 0.61 |
|
| |||
| Geographic Region | |||
| Northeast | 22.0 (18.5–25.9) | 20.2 (17.7–23.1) | 0.20 |
| Midwest | 20.0 (16.8–23.8) | 21.6 (18.5–25.0) | 0.30 |
| South | 37.5 (33.1–42.1) | 36.7 (33.0–40.6) | 0.60 |
| West | 20.5 (17.5–23.8) | 21.5 (18.9–24.3) | 0.51 |
|
| |||
| Physician Specialty | |||
| General medicine b | 35.9 (32.5–39.4) | 39.2 (37.7–40.8) | 0.04 |
| Dermatology | 27.8 (24.8–31.0) | 3.5 (3.2–3.8) | <0.01 |
| Surgery c | 5.2 (4.3–6.2) | 17.3 (16.6–18.0) | <0.01 |
| Ob/gyn | 13.6 (11.7–15.9) | 7.7 (7.3–8.2) | <0.01 |
| All otherd | 17.5 (15.1–20.1) | 32.2 (31.1–33.4) | <0.01 |
|
| |||
| Type of Payment | |||
| Private | 56.2 (53.2–59.3) | 55.3 (54.1–56.5) | 0.51 |
| Medicaree | 21.8 (19.6–24.3) | 22.0 (21.1–22.8) | 0.92 |
| Medicaid/SCHIP | 11.4 (9.56–13.4) | 10.5 (9.8–11.2) | 0.35 |
| Worker’s Compensation | 0.2 (.07–.7) | 1.4 (1.3–1.6) | <0.01 |
| Self-Pay | 5.4 (4.0–7.1) | 4.4 (4.1–4.7) | 0.16 |
| No Charge | 0.5 (.2–.9) | 0.4 (.3–.5) | 0.87 |
| Other/Unknown | 4.5 (3.5–5.9) | 6.0 (5.6–6.5) | 0.03 |
|
| |||
| All Patients | 7,002,352 | 911,025,555 | |
Based on data from 1999–2008 because of change in NAMCS’ reporting of race
Includes family medicine and internal medicine.
Includes general surgery, orthopedic surgery, urology, ophthalmology, otolaryngology
Includes pediatrics, cardiovascular medicine, psychiatry, neurology, and all other specialties not mentioned above
Dual eligible (Medicare and Medicaid) patients were counted as Medicaid
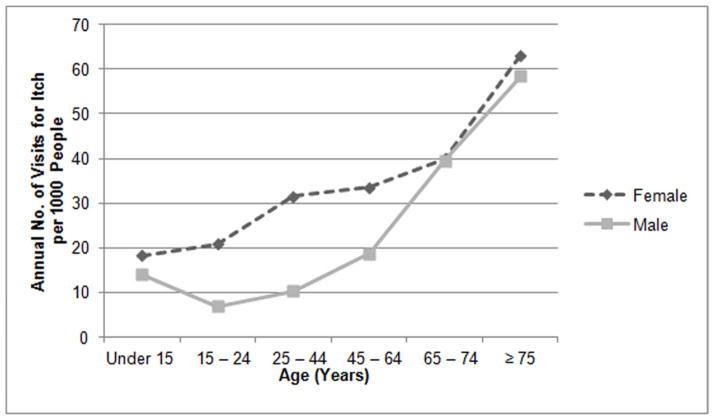
We then explored the relationship by age and visits for itch by sex and race. Figure 1 shows that while women are more likely than men to go to a clinic for itch up through age 65, the rates of visits between men and women are comparable after age 65. Figure 2 shows that Asians/Native Hawaiians/ Pacific Islanders are over three times more likely than whites or blacks to visit a clinic for itch as they age.
Figure 1.
Annual Number of Visits for Itch per 1000 People by Patient Age and Sex
Figure 2.
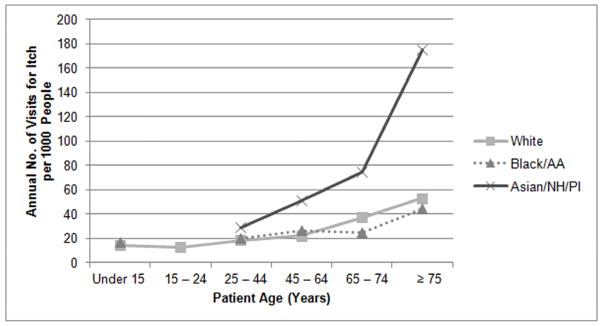
Annual Number of Visits for Itch per 1000 People by Patient Age and Race Abbreviations: AA, African American; NH, Native Hawaiian; PI, Pacific Islander. Certain data points for Black/AA and Asian/NH/PI are not shown because there were too few observations to draw reliable estimates. Two racial groups, “American Indian/Alaskan Native” and “More than one race,” are not shown because of inadequate numbers of observations.
Clinical services
Diagnoses
For the subgroup of visits included because of a symptom of itch rather than the ICD-9 diagnoses of itch, in which patients who presented with a symptom of itch (without classifying them based on their ultimate diagnosis), the frequencies of itching by body location were: skin (63.4%), vagina (17.1%), ear (5.2%), scalp (4.8%), vulva (3.8%), anus (3.2%), and eyelid (1.9%). The most common primary diagnoses were contact dermatitis (12.8%), vaginitis and vulvovaginitis (6.4%), candidiasis of the vulva and vagina (3.6%), rash and other nonspecific skin eruption (3.5%), unspecified pruritic disorder (2.9%), urticaria (2.7%), contact dermatitis and other eczema due to plants (2.0%), seborrheic dermatitis (1.7%), other psoriasis—psoriasis NOS, acrodermatitis continua, dermatitis repens (1.7%), actinic keratosis (1.5%), and other atopic dermatitis and related conditions (1.5%). The remainder of visits was for a variety of nonspecific or less common diagnoses. When we compared most common primary diagnoses by age group, there was no single condition that was the most common primary diagnosis for more than 20% of patients, but eczematous dermatitis was the most commonly noted in all age groups (in 16.4%, 12.3%, 10.3%, and 11.4% in patients < 15 years, 15–44 years, 45–64 years, and > 65 years, respectively).
Treatment/Intervention
With respect to clinical services, biopsies and excisions were more likely and blood tests were less likely to be performed during visits for itch than during visits for other reasons (Table 3). Clinicians were much more likely not only to prescribe a new medication but also to prescribe two or more new medications during visits for itch than during visits for other reasons (68% vs. 36% and 31% vs. 14%, respectively). In the subgroup of visits to dermatologists for itch, biopsies were performed in 12% and excisions in 21% of visits.
Table 3.
Characteristics of Clinical Care in Visits for Itch (2005–2009)
| % of Visits for Itch (95% CI) (N=1,120) | % of Visits Not for Itch (95% CI) (N=147,737) | P-value | % of Visits to Dermatologists for Itch (95% CI) (N=370) | |
|---|---|---|---|---|
|
| ||||
| Frequency of services | ||||
| New prescription | 68.1 (64.1–71.9) | 35.8 (34.7–36.8) | <0.01 | 61.1 (53.2–68.4) |
| Blood testa | 12.3 (9.5–15.7) | 20.4 (19.6–21.2) | <0.01 | 2.3b (1.3–3.9) |
| Biopsy | 4.4 (3.2–6.1) | 1.3 (1.1–1.4) | <0.01 | 12.4 (8.8–17.1) |
| Wound Care | 2.3 (1.5–3.6) | 1.9 (1.7–2.1) | 0.43 | 4.7b (2.6–8.4) |
| Excision | 6.7 (5.3–8.6) | 2.1 (1.9–2.3) | <0.01 | 21.0 (16.7–25.9) |
|
| ||||
| Number of new medications prescribed (N=148,857) | ||||
| 0 | 31.9 (28.1–35.9) | 64.3 (63.2–65.3) | <0.01 | 38.9 (31.6–46.8) |
| 1 | 37.0 (33.1–41.1) | 21.9 (21.4–22.5) | <0.01 | 33.6 (27.9–39.8) |
| 2+ | 31.1 (27.1–35.5) | 13.8 (13.1–14.5) | <0.01 | 27.5 (21.4–34.5) |
Includes CBC, electrolytes, cholesterol, glucose, HgA1C, PSA, and other blood tests
Number of observations is too small to be reliable
The most frequently prescribed new medications in visits for itch from 2005–2009 were topical steroids (13.3%), other topical dermatological agents (8.2%), systemic antibiotics (7.2%), anxiolytics (7.1%), non-topical anti-histamines (6.8%), systemic anti-fungals (5.6%), systemic steroids (5.6%), topical anti-infectives (4.3%), topical steroids with an anti-infective (3.8%), vaginal preparations (3.6%), miscellaneous uncategorized agents (3.6%), and respiratory inhalants (2.9%).
Follow-up
Plans for follow-up after visits for itch were analyzed by clinician specialty (Figure 3). Dermatologists were more likely than other specialties to schedule a follow-up appointment after visits for itch, even after considering the rate of referral among general medicine patient visits.
Figure 3.
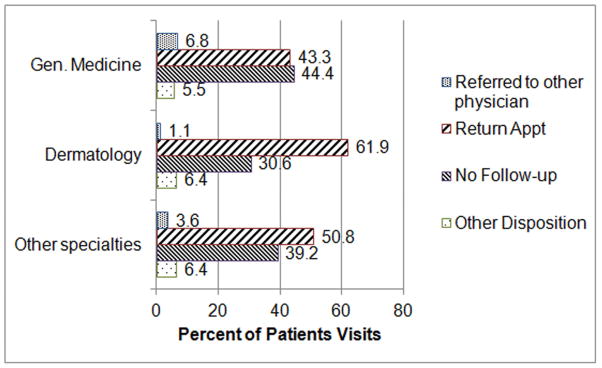
Plans for Follow-up after Visits for Itch by Clinician Specialtya
a No follow-up includes: no follow-up, return as needed, and no disposition recorded (<3% of all visits). Other disposition includes: returned to referring physician, telephone follow-up, referred to the ED, admitted to hospital, and others.
DISCUSSION
Our study adds to the global data on the epidemiology of itch by providing the first US-based, nationally representative estimates of the symptom of itch. We found that itch is a very common symptom leading to over 7 million clinician visits in America each year. Patients with itch were more likely to be older, and itch was more common among Black and Asian patients. Patients presenting for itch were more likely to receive a biopsy or surgical procedure, as well as multiple medication prescriptions. Overall, our findings provide insight on the high burden/severe impact of itch for both the healthcare system, as well as for individual patients.
The population-based prevalence of itch has been estimated by several prior European studies, and ranges from 8.2 to 22%.3–9 We believe that our estimate of 7 million annual visits for itch is an underestimate of the true burden of itch on the US because not all patients with this symptom visit a physician for this problem. In fact previous studies estimate that only half of patients ever see a physician for this complaint.3, 7, 8 Furthermore, we chose not to include specific diagnoses of conditions that typically itch (like atopic dermatitis or tinea pedis) since patient experiences of diseases may vary.
Our findings identified variations in the demographics of itch and confirm the experience of practicing clinicians. For example, we found that itch was more common among blacks and Asians, consistent with a Norwegian study that found that itch was more prevalent among people of East Asian descent and US study showing higher prevalence of atopic dermatitis among Asians.19, 20 Furthermore, our data show that elderly Asians visit clinicians for itch over three times more frequently than either whites or blacks. We found a peak in office visits for itch among patients older than 75, consistent with prior studies showing that itching is common in the geriatric population,21–24 and may increase with age.7, 22, 23
Compared to other ambulatory visits, visits for itch more frequently resulted in procedures, and the prescription of multiple medications. In looking at the treatment of itch, we found that, not-surprisingly, topical steroids were the most common medications given, which is consistent with the study by Duque et al. that also looked NAMCS data and found that the most common over-the-counter antipruritic medications given were hydrocortisone and diphenhydramine from 1995–2000.25 However, patients were also frequently prescribed antibiotics, antihistamines, and antianxiolytics. We cannot be certain that these medications were prescribed specifically for itching, but the variety of prescribed medications may suggest both the broad impact of itch on patients’ quality of life, and the difficulty of treating this symptom.
Limitations
Our study has several limitations. First, itch is difficult to study because it is a patient experience rather than a diagnosis, and secondary datasets may not be optimally designed to capture patient reports.26, 27 Secondly, because physicians often address several different patient complaints in a single visit, it is possible that some of the procedures or medications ordered were for reasons other than itch. As with any survey, there may be incomplete forms or incorrect information. However, the non-response rate for most items was less than 5% and the National Center for Health Statistics takes steps to reduce non-responsiveness, encourage uniform reporting, and perform quality control measures.28 Additionally, it is possible that physicians may not record over-the-counter medications as accurately as prescription medications. It is important to note that our study examines the symptom of itch in the outpatient setting, which has a relationship to but is not a direct estimate of population prevalence.
In summary, this is the first nationally representative study of the frequency of itch in the United States. In addition to confirming prior global estimates of the high prevalence of itch, our study validates the experience of practicing clinicians worldwide who have long understood this is a major problem for their patients. Among the strengths of this study are the use of a large, nationally-representative database of outpatient visits and the focus on a patient symptom. However, areas for future research include conducting itch-specific surveys of patients to evaluate key characteristics of pruritus and quality of life. Further, we propose that additional resources should be directed towards discovering effective and targeted treatments for this very common and burdensome problem.
Capsule Summary.
European studies show that itch is a widespread symptom.
There were an average of 7 million outpatient visits per year where itch was a symptom—nearly 40% of the number for low back pain—with patients more likely to be Black or Asian.
Visits for itch in the US are common and may require intensive management.
Acknowledgments
Funding Sources: This work was supported in part by a grant from the National Institute of Arthritis and Musculoskeletal and Skin Diseases, National Institutes of Health (K24 AR052667, Dr. Chren)
We are indebted to Dr. John McDonough, Dr. Mike Steinman, Yinghui Miao, and Rupa Parvataneni for their invaluable help and support. This work was supported in part by a grant from the National Institute of Arthritis and Musculoskeletal and Skin Diseases, National Institutes of Health (K24 AR052667, Dr. Chren)
Abbreviations
- NAMCS
National Ambulatory Medical Care Survey
- PSU
Population Sampling Unit
- ICD-9-CM
International Classification of Disease, 9th Edition, Clinical Modification
Footnotes
Statement on financial disclosure/conflict of interest: Dr. Chren serves as a consultant to Genentech, Inc., and Dr. Berger serves as a consultant to Prescription Solutions. The other authors report no financial disclosures.
Statement on prior presentation: This study has previously been presented in abstract form at the symposium entitled Scratching the Surface: Frontier in Itch from Skin to Brain at Washington University in St. Louis.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Desai NS, Poindexter GB, Monthrope YM, Bendeck SE, Swerlick RA, Chen SC. A pilot quality-of-life instrument for pruritus. J Am Acad Dermatol. 2008;59:234–44. doi: 10.1016/j.jaad.2008.04.006. [DOI] [PubMed] [Google Scholar]
- 2.Kini SP, DeLong LK, Veledar E, McKenzie-Brown AM, Schaufele M, Chen SC. The impact of pruritus on quality of life: the skin equivalent of pain. Arch Dermatol. 2011;147:1153–6. doi: 10.1001/archdermatol.2011.178. [DOI] [PubMed] [Google Scholar]
- 3.Matterne U, Apfelbacher CJ, Loerbroks A, Schwarzer T, Buttner M, Ofenloch R, et al. Prevalence, correlates and characteristics of chronic pruritus: a population-based cross-sectional study. Acta Derm Venereol. 2011;91:674–9. doi: 10.2340/00015555-1159. [DOI] [PubMed] [Google Scholar]
- 4.Dalgard F, Svensson A, Holm JO, Sundby J. Self-reported skin morbidity in Oslo. Associations with sociodemographic factors among adults in a cross-sectional study. Br J Dermatol. 2004;151:452–7. doi: 10.1111/j.1365-2133.2004.06058.x. [DOI] [PubMed] [Google Scholar]
- 5.Matterne U, Strassner T, Apfelbacher CJ, Diepgen TL, Weisshaar E. Measuring the prevalence of chronic itch in the general population: development and validation of a questionnaire for use in large-scale studies. Acta Derm Venereol. 2009;89:250–6. doi: 10.2340/00015555-0641. [DOI] [PubMed] [Google Scholar]
- 6.Rea JN, Newhouse ML, Halil T. Skin disease in Lambeth. A community study of prevalence and use of medical care. Br J Prev Soc Med. 1976;30:107–14. doi: 10.1136/jech.30.2.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stander S, Schafer I, Phan NQ, Blome C, Herberger K, Heigel H, et al. Prevalence of chronic pruritus in Germany: results of a cross-sectional study in a sample working population of 11,730. Dermatology. 2010;221:229–35. doi: 10.1159/000319862. [DOI] [PubMed] [Google Scholar]
- 8.Wolkenstein P, Grob JJ, Bastuji-Garin S, Ruszczynski S, Roujeau JC, Revuz J. French people and skin diseases: results of a survey using a representative sample. Arch Dermatol. 2003;139:1614–9. doi: 10.1001/archderm.139.12.1614. discussion 9. [DOI] [PubMed] [Google Scholar]
- 9.Dalgard F, Svensson A, Holm JO, Sundby J. Self-reported skin complaints: validation of a questionnaire for population surveys. Br J Dermatol. 2003;149:794–800. doi: 10.1046/j.1365-2133.2003.05596.x. [DOI] [PubMed] [Google Scholar]
- 10.Seidler AM, Kini SP, DeLong LK, Veledar E, Chen SC. Preference-based measures in dermatology: an overview of utilities and willingness to pay. Dermatol Clin. 2012;30:223–9. xiii. doi: 10.1016/j.det.2011.12.002. [DOI] [PubMed] [Google Scholar]
- 11.Tenney J, White K, Williamson J. National Ambulatory Medical Care Survey: Background and Methodology: United States, 1967–72. Vital Health Statistics Series. 1974;2:76. [PubMed] [Google Scholar]
- 12.Centers for Disease Control and Prevention. [Accessed July 23, 2012];Ambulatory Health Care Data: Scope and Sample Design. Available at: http://www.cdc.gov/nchs/ahcd/ahcd_scope.htm.
- 13.Centers for Disease Control and Prevention. [Accessed July 14, 2012];Ambulatory Health Care Data: About the Ambulatory Health Care Surveys. Available at: http://www.cdc.gov/nchs/ahcd/about_ahcd.htm.
- 14.Centers for Disease Control and Prevention. [Accessed July 23, 2012];Using Ultimate Cluster Models with NAMCS and NHAMCS Public Use Files. 2004 Available at: www.cdc.gov/nchs/data/ahcd/ultimatecluster.pdf.
- 15.Centers for Disease Control and Prevention. [Accessed July 23, 2012];International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) Available at: http://www.cdc.gov/nchs/icd/icd9cm.htm.
- 16.Population Division U.S. Census Bureau. [Accessed July 25, 2012];Vintage 2005: National Tables. Available at: http://www.census.gov/popest/data/historical/2000s/vintage_2005/index.html.
- 17.Centers for Disease Control and Prevention. [Accessed September 1, 2012];Trend Analysis Using NAMCS and NHAMCS Drug Data. Available at: http://www.cdc.gov/nchs/ahcd/trend_analysis.htm.
- 18.Centers for Disease Control and Prevention. [Accessed July 24, 2012];The New Ambulatory Care Drug Database System. Available at: http://www2.cdc.gov/drugs/applicationnav1.asp.
- 19.Janumpally SR, Feldman SR, Gupta AK, Fleischer AB., Jr In the United States, blacks and Asian/Pacific Islanders are more likely than whites to seek medical care for atopic dermatitis. Arch Dermatol. 2002;138:634–7. doi: 10.1001/archderm.138.5.634. [DOI] [PubMed] [Google Scholar]
- 20.Dalgard F, Holm JO, Svensson A, Kumar B, Sundby J. Self reported skin morbidity and ethnicity: a population-based study in a Western community. BMC Dermatol. 2007;7:4. doi: 10.1186/1471-5945-7-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Patange VS, Fernandez RJ. A study of geriatric dermatoses. Indian J Dermatol Venereol Leprol. 1995;61:206–8. [PubMed] [Google Scholar]
- 22.Yalcin B, Tamer E, Toy GG, Oztas P, Hayran M, Alli N. The prevalence of skin diseases in the elderly: analysis of 4099 geriatric patients. Int J Dermatol. 2006;45:672–6. doi: 10.1111/j.1365-4632.2005.02607.x. [DOI] [PubMed] [Google Scholar]
- 23.Liao YH, Chen KH, Tseng MP, Sun CC. Pattern of skin diseases in a geriatric patient group in Taiwan: a 7-year survey from the outpatient clinic of a university medical center. Dermatology. 2001;203:308–13. doi: 10.1159/000051778. [DOI] [PubMed] [Google Scholar]
- 24.Beauregard S, Gilchrest BA. A survey of skin problems and skin care regimens in the elderly. Arch Dermatol. 1987;123:1638–43. [PubMed] [Google Scholar]
- 25.Duque MI, Vogel CA, Fleischer AB, Jr, Yosipovitch G. Over-the-counter topical antipruritic agents are commonly recommended by office-based physicians: an analysis of US practice patterns. J Dermatolog Treat. 2004;15:185–8. doi: 10.1080/09546630410027337. [DOI] [PubMed] [Google Scholar]
- 26.Chen SC. Pruritus. Dermatol Clin. 2012;30:309–21. ix. doi: 10.1016/j.det.2011.11.012. [DOI] [PubMed] [Google Scholar]
- 27.Weisshaar E, Gieler U, Kupfer J, Furue M, Saeki H, Yosipovitch G. Questionnaires to Assess Chronic Itch: A Consensus Paper of the Special Interest Group of the International Forum on the Study of Itch. Acta Derm Venereol. 2012 doi: 10.2340/00015555-1402. [DOI] [PubMed] [Google Scholar]
- 28.Centers for Disease Control and Prevention. [Accessed July 23, 2012];Data Collection and Processing. Available at: http://www.cdc.gov/nchs/ahcd/ahcd_data_collection.htm.