Abstract
Despite the substantial amount of data supporting a link between HPA-axis functioning and depression, the ontogeny of this association is not known. The aim of the present study was to contribute data on the developmental interface of HPA-axis functioning and depression in girls by testing associations between repeated measures of depression symptoms and cortisol levels in childhood and early adolescence. Girls (N= 232) and their mothers, who were participating in a longitudinal study, were interviewed about depression symptoms annually from ages 9 to 12 years. Cortisol was assayed from saliva at ages 10 and 12 years upon arrival to the lab and following administration of the cold pressor task (CPT). Time of day of collection of saliva and level of pubertal development were included as covariates in model testing. Although most girls did not show an increase in cortisol in response to the CPT, lower levels of output during the CPT were associated with higher levels of depression symptoms. These findings were observed only for cortisol levels assessed at age 12 years. Girls with low levels of cortisol output at age 12, and decreases in output from ages 10 to 12, had stable or slightly increasing depression symptoms from ages 9 to 12 years. We conclude that associations between HPA-axis functioning and depression emerge as early as age 12. However, individual differences in cortisol levels at age 12 also were associated with depression symptoms at earlier ages. The data suggest two possibilities: 1) that childhood depression is associated with HPA-axis dysregulation, but that age related changes in the sensitivity or plasticity of the HPA-axis may result in a delay in the emergence of such an association, or 2) that dysregulation of the functioning of the HPA-axis develops following repeated experience of depression symptoms.
Keywords: cortisol, depression, childhood, girls, development
Introduction
A substantial amount of data exists linking the functioning of the HPA-axis to depression in adults (see Plotsky, Owens & Nemeroff, 1998, for a review), leading to the hypothesis that glucocorticoids play a role in the pathophysiology of depression. Moreover, developmental and sex differences in functioning of the HPA-axis mirrors those observed for depression. Sex differences in depression symptoms or disorders are generally not evident until adolescence, at which point increases in depression are evident for girls but not for boys (Keenan & Hipwell, 2005). Similar sex by age effects are observed in HPA-axis functioning. In terms of diurnal levels and awakening response, Shirtcliff and colleagues (2012) collected three saliva samples across the day (after awakening, in the late afternoon and before bed) from approximately 300 children every two years from ages 9 to 15 years. Girls had higher cortisol levels at awakening and steeper slopes across the day. Significant age by sex effects were observed for awakening cortisol level, which declined within individual across age, but significantly less so for girls than for boys. Platje et al. (2013) reported sex differences in the cortisol awakening response at ages 15, 16, and 17 years; girls had higher cortisol levels than boys at 30 and 60 minutes post-awakening, and by age 17 the CAR for girls was in a positive direction (i.e., increase in cortisol following awakening) whereas boys continued to show a decrease in cortisol following awakening.
Sex and age or pubertal effects are also found for cortisol reactivity to a stressor. Stroud et al. (2011) used a corticotropin releasing hormone (CRH) challenge in children and adolescents and reported that stage of pubertal development was associated with the pattern of response in girls, characterized primarily as a slowing of the recovery to baseline response with more advanced maturation: stage of pubertal development was not associated with cortisol response among boys.
The effects of age and puberty and sex on stress response also are evident in animal models. Pubertal female rats have prolonged corticosterone release in response to restraint stress compared to adult females (Romeo et al., 2004). Compared to controls, females rats exposed to chronic social stress during adolescence did not habituate to the stressor, showed a prolonged corticosterone response to a subsequent heterotypic stressor, and were more likely to engage in depression-like behavior during a forced swim test (e.g., less time climbing and more time immobile). Males habituated to the repeated social stressor, had an increase in corticosterone level but no difference in shape of response, and demonstrated no difference in behavior during the forced swim test as a function of social stress (Matthews et al, 2008).
The possibility that the HPA axis is maximally sensitive to experiences during adolescence has implications for psychopathology, especially for females, who demonstrate increased risk for distress disorders during adolescence (Keenan & Hipwell, 2005). Specifying the developmental interface between HPA-axis functioning and depression in humans, however, has been challenging. The use of cross sectional designs is not highly informative regarding the timing and direction of effect. Moreover, because base rates of depression symptoms and disorders are low in childhood (Son & Kirchner, 2000; Kessler et al., 2001), tests of association between cortisol levels and depression are often conducted later in adolescence. Among the few studies in which child participants were included no association between cortisol levels assessed in response to a challenge, such as CRH, and depression symptoms was observed (e.g., Birmaher et al., 1996; Puig-Antich et al., 1989).
In contrast, studies in which the association between cortisol levels and depression participants were assessed during mid- to late adolescence typically yield significant associations. Cortisol levels among depressed adolescents in response to a social stressor were elevated and slower to return to baseline compared to non-depressed adolescents (Rao et al., 2008). Higher and flatter diurnal rhythms were observed among adolescents with high depression scores (n=9) compared to adolescents with moderate (n=12) or low (n=45) scores (Van den Bergh & Van Calster, 2009). Adam and colleagues (2010) reported that a higher baseline CAR was associated with the incidence of major depressive disorder one year later in a sample of 230 17-year olds, many of whom had a history of mood and anxiety disorders based on retrospective report.
In others studies the pattern of association between cortisol output and depression is a negative one. Results from a study on diurnal cortisol in a sample of youth whose mental health had been assessed longitudinally since childhood revealed that childhood internalizing behaviors, but not externalizing behaviors, were prospectively associated with lower morning cortisol levels in early adolescence (Ruttle et al., 2011). Measures of cortisol functioning in childhood, however, were not available for the sample. Badanes and colleagues (2011) also reported significant associations between low cortisol output and depression scores. In that study, cortisol levels for children in grades 3, 6, and 9 were operationalized as the average of five samples taken before and after a social stress test. Effects of age were not tested.
In summary, the pattern of association between depression symptoms, scores or disorders and cortisol reactivity, awakening response, or diurnal rhythm during adolescence is typically positive. The pattern of association involving assessment of depression in children, in contrast is inconsistent: typically no effects have been observed between depression and cortisol reactivity, and a negative association has been observed between childhood internalizing problems and cortisol levels in adolescence.
Further probing of age-related changes in the association between cortisol and depression are important for understanding the pathophysiology of depression, especially with regard to potential phenotypic differences between depression that is manifest prior to the completion of pubertal development and depression that occurs post-pubertal development. Kaufman and colleagues (2001) concluded from reviewing the available literature that depressed children differ from depressed adults on measures of basal cortisol secretion, and in response to a corticotropin releasing hormone (CRH) challenge. These differences along with others in neurobiology and treatment response suggested to the authors that depression in adults may be phenotypically different from childhood depression. For example, replicated findings of differences in changes in electroencephalographic (EEG) sleep associated with depression in adults and adolescents are generally not present in studies of depressed and non-depressed children (Kaufmann et al., 2001). Most of the research reviewed by Kaufman and colleagues, however, was cross-sectional in design. Longitudinal research is needed to address whether associations between HPA-axis functioning and depression emerges over time.
In the present study, we provide data that expands and extends the existing research by examining the interrelations among depression symptoms and cortisol levels in the same individuals at ages 10 and 12 years. We test concurrent and longitudinal associations between depression symptoms and cortisol to provide support for the hypothesis that there are age related changes in depression-cortisol associations. In addition, we explore whether dysregulation of the HPA-axis occurs after an extended period of exposure to depressive symptoms by examining depression symptoms measured over four years, from ages 9–12 years, as a function of cortisol levels and changes in cortisol output from ages 10–12 years.
Method
Sampling of participants
Participants for the present study were recruited from the Pittsburgh Girls Study (PGS) (Keenan et al., 2010). The PGS sample was formed following an enumeration of households in the city of Pittsburgh. Of the 2,992 eligible families 2,451 (85%) were successfully re-contacted and agreed to participate in a longitudinal study with annual in-home interviews. Girls selected for participation in the Emotions sub-study (PGS-E) were from the youngest participants in the PGS who either screened high on measures of depressive symptoms at age 8, or who were included in a random selection from the remaining 8-year old girls. Girls whose scores fell at or above the 75th percentile by their own report on the Short Moods and Feelings Questionnaire (SMFQ) (Angold et al., 1995) and/or by their mother’s report on the Child Symptom Inventory (CSI) (Gadow & Sprafkin, 1996) comprised the screen high group (n=135). There were significantly more African American than European American girls in the screen high group. Thus, the girls selected from the remainder were matched to the screen-high group on race. Of the 263 families eligible to participate, 232 (88.2%) agreed to participate and completed the first laboratory assessment when the girls were nine years of age. Retention in each year was at above 95%. The Institutional Review Boards at the Universities of Pittsburgh and Chicago approved all study procedures. Written informed consent from the mother and assent from the youth were obtained.
Measures
Depression symptoms
Current symptoms of depression (i.e., past month) were measured in each year using the Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL) (Kaufman et al., 1997), a semi-structured diagnostic interview, which was administered separately to the mother and the girl. Each of the nine symptoms of depression was assessed regardless of whether disturbance in mood or anhedonia were endorsed, thereby providing a continuous measure of depression symptom counts. Twenty-five percent of the girls’ interviews were randomly selected and coded for assessing interrater reliabilty. For youth-report data, the average intraclass correlation coefficient for total number of symptoms was .96. For caregiver report intraclass correlation coefficients for total number of symptoms was .95. A symptom was considered present if it was endorsed by either informant. At each wave of data collection the alpha coefficient for the nine depression symptoms based on the combined informants was greater than 0.7. To reduce the skew in depression symptoms, a constant of 1 was added to each score followed by a log10 transformation.
Cortisol levels
Cortisol levels were assessed at ages 10 and 12 years approximately 10 minutes following arrival to the lab and then in response to the Cold Pressor Task (CPT) (von Baeyer et al., 2005). The average time of day for collection of the first saliva sample was 13:42 (range = 08:41 – 16:25) and 13:22 (range = 08:30 – 16:46) at ages 10 and 12, respectively (see Table 1). During the CPT, participants were asked to submerge their dominant arms in a tank of cold water, and instructed to keep the arm in the water for as long as possible but to remove it if it became too uncomfortable. The participant first immersed her dominant arm in a tank of warm water (37°C) for 2 minutes, to control for differences in baseline body temperature, and then in the tank of cold water (10°C) for a maximum of 3 minutes. This is the most commonly used protocol with pediatric participants (Birnie et al., 2012). In order to maintain the temperature in the latter tank, water was circulated through ice by a pump. Saliva samples were collected at 20 and 45 minutes post completion of the CPT.
Table 1.
Descriptive statistics for raw depression symptoms and cortisol levels
| Depression symptoms | Mean | SD | range |
| Age 9 | 2.42 | 2.04 | 0 – 8 |
| Age 10 | 2.06 | 1.79 | 0 – 7 |
| Age 11 | 1.99 | 1.96 | 0 – 9 |
| Age 12 | 1.83 | 1.76 | 0 – 7 |
| Cortisol levels (µg/dL) at age 10 | Mean | SD | range |
| Time of first collection | 13:42 | 02:49 | 08:41 – 18:25 |
| 10 mins post arrival | 0.13 | 0.09 | 0.02 – 0.66 |
| 20 mins post-CPT | 0.10 | 0.06 | 0.01 – 0.47 |
| 45 mins post-CPT | 0.08 | 0.05 | 0.02 – 0.35 |
| AUCg | 4.48 | 2.77 | 0.65 – 19.18 |
| AUCi | −1.13 | 1.90 | −15.40 – 4.38 |
| Cortisol levels (µg/dL) at age 12 | Mean | SD | range |
| Time of first collection | 13:22 | 03:02 | 08:30 – 18:46 |
| 10 mins post arrival | 0.15 | 0.12 | 0.01 – 0.75 |
| 20 mins post-CPT | 0.10 | 0.07 | 0.01 – 0.44 |
| 45 mins post-CPT | 0.08 | 0.05 | 0.01 – 0.30 |
| AUCg | 4.88 | 3.30 | 0.68 – 21.38 |
| AUCi | −1.76 | 2.47 | −15.91 – 3.85 |
Note: CPT = Cold pressor task; AUCg = area under the curve with respect to ground; AUCi = area under the curve with respect to increase.
To collect saliva samples, an absorbent salivette was applied to the tongue, cheek, and gums for approximately 1 minute. Salivettes were placed in a labeled plastic tube and then transferred to a freezer and stored at −20° C until assayed. Samples were shipped to the Behavioral Endocrinology Laboratory at Pennsylvania State University. On the day of testing, samples were thawed, centrifuged at 3,000 rpm for 10 minutes and clear samples were pipetted into appropriate test wells. Samples with sufficient saliva were assayed in duplicate using the Salimetrics HS Salivary Cortisol EIA Kit for unbound cortisol. This assay has a lower limit of sensitivity from .007 to 1.2 ug/dL. The average between-assay variance is 3.9% and 7.1%, and the average within-assay variance is 6.7% and 6.9% for high and low concentrations, respectively. Log10 transformations were applied to all cortisol measures to reduce skewness. There was one extreme outlier at each age after transforming the values, and these subjects were removed from the analytic sample.
Pubertal development
Stage of pubertal development was assessed via self-ratings performed with the aid of schematic drawings of secondary sexual characteristics (Morris & Udry, 1980). Scores for breast and pubic hair were scored at 5 stages of development, in order to approximate Tanner Staging. Growth in breasts and pubic hair were modeled separately, as previous research has indicated that characterizing the pathways to pubertal maturation may be important for understanding risk for behavioral and emotional problems (Biro et al., 2008).
Results
Descriptive statistics
for DSM-IV depression symptoms and cortisol levels at ages 10 and 12 are presented in Table 1. On average girls reported approximately 2 symptoms of depression at each age. The pattern of cortisol levels was characterized by a decrease over the course of the administration of the CPT, as one would expect in the later afternoon. Thus, the CPT as a stimulus did not, for the most part elicit a cortisol response (i.e., increase). Area under the curve with respect to ground (AUCg) and increase (AUCi) were calculated as an indices of cortisol output that is appropriate regardless of whether an increase is observed (Pruessner et al., 2003): 15.7% of the sample at age 10 years and 13.0% of the sample at age 12 years had positive AUCi values. Time of day was significantly associated with AUCg (r = −.25, p < .001 and r = −.32, p < .001 at ages 10 and 12 years, respectively) and AUCi (r = .12, p < .05 and r = .21 p < .01 at ages 10 and 12 years, respectively); depression symptoms were not significantly associated with time of day.
Associations between depression symptoms and cortisol levels
The association between depression symptoms at ages 9 through 12 years and cortisol levels taken upon arrival to the lab and cortisol output during the CPT was examined by computing Pearson correlation coefficients. As shown in Table 2, no significant association between cortisol levels at age 10 years and depression symptoms were observed. Cortisol levels at age 12 years as quantified by AUCg were modestly but significantly associated with depression symptoms at ages 10, 11, and 12 years: all associations were in the direction of lower cortisol levels being associated with higher levels of depression symptoms (Table 2). Comparisons of the correlations between AUCg at ages 10 and 12 and depression symptoms were tested using r to t transformations for dependent correlations. Significant differences were observed for the association between cortisol levels at ages 10 and 12 and depression at ages 12 (t [205]=−2.22, p = .014) and 11 (t [205] = −1.83, p = .034), but not at age 10.
Table 2.
Associations between cortisol levels at ages 10 and 12 years and depression symptoms
| Cortisol (µg/dL) | Cortisol (µg/dL) | |||
|---|---|---|---|---|
| Age 10 years | Age 12 years | |||
| Depression symptoms | AUCg | AUCi | AUCg | AUCi |
| Age 9 | −.017 | .018 | .037 | −.044 |
| Age 10 | −.069 | .015 | −.139* | .113 |
| Age 11 | −.014 | −.054 | −.172* | .051 |
| Age 12 | .003 | .010 | −.198** | .108 |
Note: cortisol values and depression symptoms are log10 transformed; Significance of Pearson correlation coefficients
p < .05,
p < .01
To test whether cortisol levels explained unique variance in concurrent and earlier depression, linear regression models were computed with depression symptoms as the dependent measures, cortisol levels at 12 years as the independent measure, controlling for pubertal status, time of day, and cortisol levels at age 10. As shown in tables 3 and 4, cortisol levels at age 12, as measured by AUCg explained variance in depression symptoms at ages 12 and 11 years, controlling for stage of pubertal development, time of day of sampling, and age 10 cortisol levels. No significant associations between cortisol levels at age 12 and depression symptoms at ages 9 and 10 were observed (data not shown).
Table 3.
Association between cortisol levels and depression symptoms at age 12 years
| Dependent Variable: Depression symptoms at age 12 | ||
| Step 1 | t value | p level |
| Breast development | 1.664 | .098 |
| Growth in pubic hair | 0.694 | .489 |
| Time of sampling (linear) | −0.408 | .684 |
| Time of sampling (quadratic) | 0.315 | .753 |
| Step 2 | ||
| Cortisol (µg/dL) AUCg at age 10 | 0.874 | .383 |
| Step 3 | ||
| Cortisol (µg/dL) AUCg at age 12 | −3.060 | .003 |
Overall F (6, 198) = 2.823, p = .012, Adjusted R Square = .052
Table 4.
Associations between cortisol levels and depression symptoms at 11 years
| Dependent Variable: Depression symptoms at age 11 | ||
| Step 1 | t value | p level |
| Breast development | 0.358 | .721 |
| Growth in pubic hair | 1.821 | .070 |
| Time of sampling (linear) | −0.820 | .424 |
| Time of sampling (quadratic) | 0.714 | .472 |
| Step 2 | ||
| Cortisol (µg/dL) AUCg at age 10 | 0.710 | .478 |
| Step 3 | ||
| Cortisol (µg/dL) AUCg at age 12 | −2.995 | .003 |
Overall F (6, 198) = 2.510, p = .023, Adjusted R Square = .044
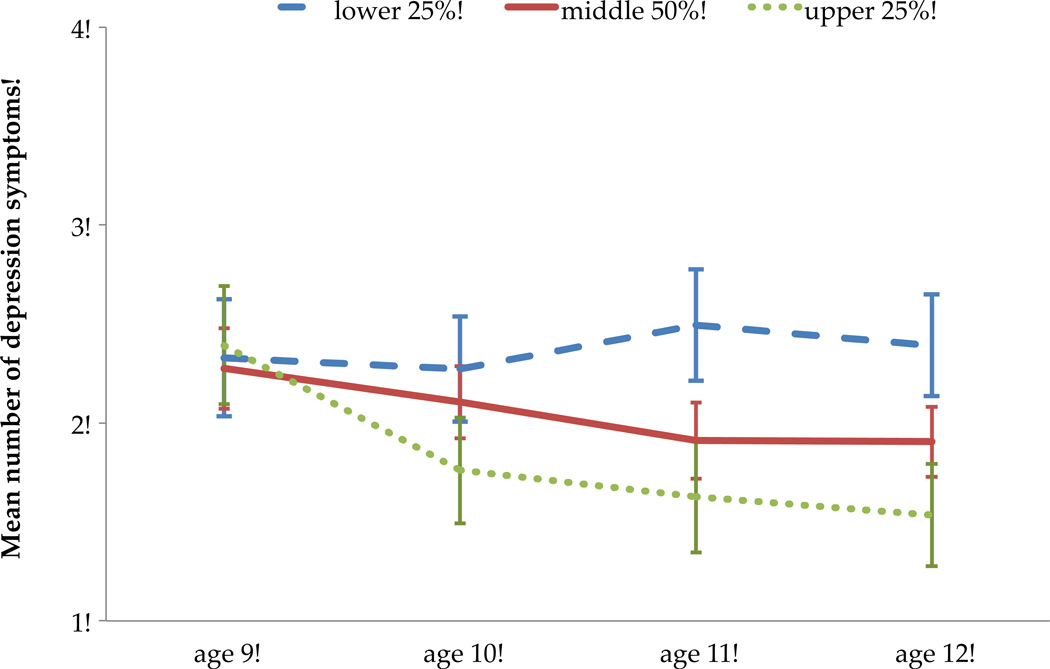
To test whether cortisol levels at age 12 differed as a function of exposure to depression symptoms over time, a generalized linear model (GLM) was computed for the four annual assessments of depression symptoms from ages 9 through 12 years, with AUCg at age 12 years as the independent variable and time of day of sampling and pubertal stage as covariates. The assumption of sphericity was not met and therefore the Greenhouse-Geisser correction was used. Cortisol levels were significantly associated with depression over time (F [2.86, 541.23] = 6.476, p = .001). These results are depicted in Figure 1, using non-transformed scores for depression symptoms and plotting depression symptoms at each age for girls at the upper 25%, middle 50% and lower 25% of the distribution of AUCg scores for ease of explication. As shown in Figure 1, depression symptoms assessed in the first wave of assessment at age 9, did not differ as function of age 12 cortisol levels. Over time, however, girls with the highest levels of cortisol output evidenced a decrease in depression symptoms, whereas girls with the lowest levels of output had either stable or slight increases in depression symptoms.
Figure 1. Depression symptoms from age 9–12 years as a function cortisol levels at age 12 years!
Note: Controlling for time of day of saliva collection and stage of pubertal development, depression symptoms vary over time as a function of age 12 cortisol levels cortisol levels as measured by AUCg, here depicted by the lower 25%, middle 50% and upper 25% of the distribution of AUCg scores and non-transformed depression symptoms for ease of explication.!
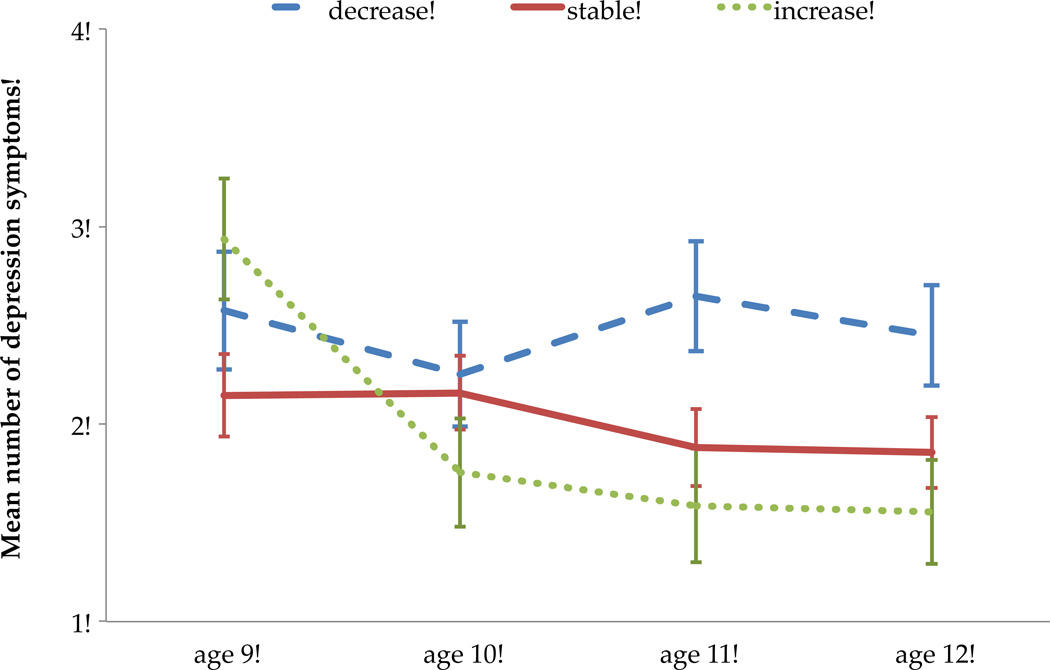
To explore whether maturation of the HPA-axis, as assessed by changes in cortisol output from ages 10–12 years, was associated with depression over time a similar GLM model as that described above was computed. Change in cortisol output from ages 10–12 years was associated with depression symptoms over time (F [5.688, 541.23] = 2.74, p = .014); results are depicted in Figure 2. Girls with decreases in cortisol output from ages 10–12 years continued to endorse between 2 and 3 symptoms of depression, on average, over the 4 years. In contrast, girls who showed an increase in cortisol output from ages 10–12 years reported decreasing levels of depression symptoms over time.
Figure 2. Depression symptoms from age 9–12 years as a function change in cortisol output from ! 10 to 12 years!
Note: Controlling for time of day of saliva collection and stage of pubertal development, depression symptoms vary over time as a function of age change in cortisol output as measured by AUCg from ages 10 – 12 years, here depicted by the lower 25% (decrease), middle 50% (stable) and upper 25% (increase) of the distribution of change scores, and non-transformed depression symptoms for ease of explication.!
Discussion
The data from the present study add to the building evidence that developmental changes in the sensitivity of HPA-axis functioning occur during adolescence, and that such changes are likely relevant for the pathophysiology of depression. Controlling for pubertal stage and time of day of saliva collection, concurrent and earlier symptoms of depression were significantly associated with cortisol levels measured at age 12. In contrast, cortisol levels obtained at age 10 were unrelated with concurrent or longitudinal measures of depression symptoms. Our results are consistent with those from other studies in which no association between cortisol measured during childhood and depression symptoms was observed (e.g., Puig-Antich et al., 1989; Birmaher et al., 1996). The results from the present study, however, suggest that the lack of association between cortisol and depression in childhood may not be due to phenotypic or etiologic differences between childhood and adolescent or adult depression, but may be due to developmental changes in the HPA-axis. In fact, changes in cortisol output from ages 10–12 years were inversely associated with depression over time; decreases in output were associated with stable or slight increases in symptoms, whereas increased in output were associated with decreases in symptoms. This pattern is consistent with data from cross-sectional and longitudinal studies in humans and animals reviewed in this paper indicating that increases with age in cortisol output (e.g., morning levels, reactivity) is normative among females. Additional data are needed to fully test the direction of effect, but at least two hypotheses are plausible: 1) increasing cortisol output from childhood to adolescence reduces the risk of depression onset in adolescence, even among children at risk; and 2) specific depression phenotypes in childhood are prospectively associated with disruptions in maturation of the HPA-axis.
Our data also support the hypothesis that repeated exposure to depression symptoms may lead to alterations in set points and/or patterns of stress reactivity as has been found in non-human species (e.g., Yoshihara & Yawaka, 2008), especially among females (Slotten et al., 2006). Thus, consistent and extended exposure to depression symptoms may be needed before a disruption in cortisol output or regulation is observed. The fact that lower levels of cortisol were associated with depression symptoms over time is consistent with research on the heterogeneity of cortisol patterns associated with stress and distress. Among depression researchers, dysregulation of the HPA-axis is most commonly defined as hyper-reactivity or elevations in cortisol (Pariante & Lightman, 2008). Dysregulation of the HPA axis can also take the form of hypo-activity or reactivity, a pattern of dysregulation that has been associated with distress disorders in adults (Fries et al., 2005). Recent evidence also supports an association between low levels of cortisol and depression in children. Badanes and colleagues (2011) reported that low cortisol output across the day was associated with higher scores on a measure of emotional distress in a sample of preschoolers, and Sontag-Padilla et al. (2012) observed that self-reported distress symptoms were negatively associated with cortisol reactivity to a pain stressor among girls who had evidence of early adrenarche. Furthermore, our results on the association between low cortisol output and exposure to depression over time are consistent with a recently published study of adolescents, for whom depression scores were obtained at ages 11, 13, and 16 years of age (Booij et a l., 2013). In that study, high cortisol output in response to a social stressor at age 16 was associated with past year depression, whereas adolescents who had experienced chronic depression symptoms from 11 to 16 year of age had lower and flatter cortisol output during and after exposure to the social stressor.
Low cortisol output in the morning and across the day has been linked to the cooccurrence of depressed mood with perceived stress, fatigue, and pain (Gur et al., 2004; Hellhamer et al., 2004), a constellation of symptoms that are not uncommon among adolescent females (Egger et al., 1999; LeResche et al., 2005; Brun Sundblad et al., 2007). Low base rates of major depression in our data prevented us from generating depression subtypes, but this would be an important next step given reported differences in HPA-axis functioning among subtypes of depression in adults (Antonijevic, 2008; Bremmer et al., 2007). Given that the parent study from which the participants were recruited was oversampled for low-income environments, the depression phenotype represented in our sample may be a chronic low-grade depression associated with exposure to stressors. In the context of such a phenotype, dysregulation of the HPA axis, in the form of blunted or down-regulation may have developed from prolonged exposure to stressors.
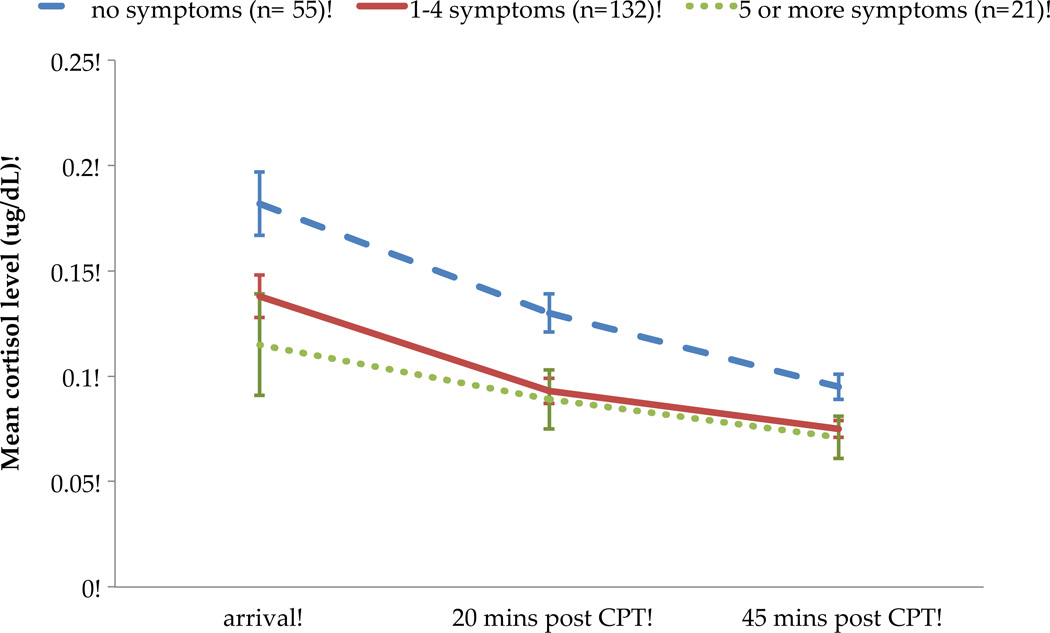
One might question the clinical significance of identifying associations between cortisol and low levels of depression symptoms. Minor depression (defined in the DSM as depressed mood or anhedonia plus one additional symptom) appears to be equivalent to major depression in term of prognosis regarding impairment, use of mental health services, future major depressive episodes and suicidality (Fergusson et al., 2005; Gonzalez-Tejera et al., 2005). We have previously provided evidence for the clinical significance of having even 1–2 symptoms of depression during childhood in the present sample; the level of impairment among girls who met criteria for minor depression was significantly different from girls without a depressive diagnosis and did not differ from girls with a diagnosis of major depression (Keenan et al., 2008). In the present study, cortisol levels at age 12 years did not differ between girls with 1–4 symptoms and those with 5 or more symptoms, but both groups differed from girls with no symptoms (see Figure 3). Again, this sample was not adequately powered to rigorously compare subthreshold and full depression, but preliminary evidence provides additional support for the contention that minor and major depression fall along a continuum of a single clinical disorder (Judd et al., 1998).
Figure 3. Cortisol levels as a function of depression symptoms at age 12 years!
Note: Mean cortisol values plotted for ease of explication; significant effects tested using log transformed cortisol values: group effect of depression symptoms on cortisol level (F [2,204] = 5.89, p = .003).!
Several limitations to the present study need to be acknowledged. First, an increase in cortisol in response to the administration of the CPT was not observed. In general, cortisol concentrations increase significantly following the administration of the CPT in adult samples (al'Absi, Petersen, & Wittmers, 2002; Dixon, Thorn & Ward, 2004). In children and adolescents, it is not unusual to observe a decrease in cortisol from pre- to post-physical stressor including the CPT (Gump et al., 2008; Allen et al., 2009). Obtaining multiple baseline measures as opposed to a single pre-CPT measure of cortisol and using a social evaluation as opposed to a pain stressor may have provided an opportunity to observe an increase in cortisol for a greater number of individuals.
Second, aspects of the study design including the fact that we had a relatively broad range of time of day of saliva collection and the lack of a prolonged habituation period after arrival to the laboratory may have negatively impacted our ability to discern associations with depression symptoms. Although the study design with respect to cortisol collection was similar across the two ages, there may have been differential impact of the inconsistent sampling times on testing of cortisol-depression associations at each age.
Third, it is possible that assessment of diurnal cortisol, as opposed to a laboratory assessment, would have revealed individual differences that are relevant to depression at younger ages. There are a few studies to suggest that this may be the case. Children with a history of maltreatment who also evidenced internalizing problems had higher levels of cortisol in the morning and across the day than other groups of children (Cicchetti & Rogosch, 2001). Ashman et al. (2002) reported that maternal depression in early childhood was associated with higher basal cortisol levels in 7 to 8-year olds among those children who also had symptoms of anxiety and depression. Integrating methods that differentially probe the functioning of the HPA-axis will be an important step towards clarifying the potential etiologic role in the development of depression.
Finally, although the present study included multiple assessments of cortisol and depression, the age range was still relatively narrow. Extending the assessment to post-pubertal period would provide an important test of potential interactions among depression symptoms, pubertal tempo and timing and HPA-axis functioning. The brain undergoes significant changes in morphology and function during adolescence (Sisk & Zehr, 2005; Casey et al., 2008). Pruning of brain regions involved in emotion regulation and higher cognitive functioning during adolescence may result in period of sensitization to the effects of hormones and stressors (Schulz et al., 2009; McCormick et al., 2010).
In conclusion, results from the present study indicate that concurrent associations between HPA-axis functioning and depression emerge as early as age 12 years. Importantly, however, individual differences in cortisol levels at age 12 and the change in cortisol output from ages 10 to 12 years were associated with depression symptoms at earlier ages. These data suggest that childhood depression is associated with HPA-axis dysregulation, but that age related changes in the sensitivity or plasticity of the HPA-axis that occur during adolescence may be required before such an association can be observed. Alternatively, repeated exposure to depression symptoms may be required before alterations in HPA-axis functioning can be observed. Extending the window of assessment into later adolescence and including multiple probes of the HPA-axis will further elucidate the temporal associations between depression and HPA-axis functioning.
Acknowledgements
This study was supported by NIMH grants R01 MH66167 and R03 MH084073 to Dr. Keenan. We thank the families participating in the Learning about Girls’ Emotions Study.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest
None of the authors report conflicts of interest with the data presented in this paper
Contributors
Kate Keenan, Department of Psychiatry and Behavioral Neuroscience, University of Chicago
Alison Hipwell, Department of Psychiatry, University of Pittsburgh
Dara Babinski, Department of Psychology, Florida International University
Jenna Bortner, Department of Occupational Therapy, Chatham College
Angela Henneberger, Curry School of Education, University of Virgina
Amanda Hinze, Department of Psychiatry, University of Pittsburgh
Susan Klostermann, Department of Psychology, Case Western Reserve University
Michal Rischall, Department of Psychology Northwestern, University Medical School
Brenna Sapotichne, Department of Psychiatry, University of New Orleans
References
- Adam EK, Doane LD, Zinbarg RE, Mineka S, Craske MG, Griffith JW. Prospective prediction of major depressive disorder from cortisol awakening responses in adolescence. Psychoneuroendocrinology. 2010;35:921–931. doi: 10.1016/j.psyneuen.2009.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- al'Absi M, Petersen KL, Wittmers LE. Adrenocortical and hemodynamic predictors of pain perception in men and women. Pain. 2002;96:197–204. doi: 10.1016/s0304-3959(01)00447-x. [DOI] [PubMed] [Google Scholar]
- Allen LB, Lu Q, Tsao JC, Worthman CM, Zeltzer LK. Sex differences in the association between cortisol concentrations and laboratory pain responses in healthy children. Gend. Med. 2009;6:193–207. doi: 10.1016/j.genm.2009.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Angold A, Costello EJ, Messer SC, Pickles A. Development of a short questionnaire for use in epidemiological studies of depression in children and adolescents. Int. J. Methods Psychiatr. Res. 1995;5:237–249. [Google Scholar]
- Antonijevic I. HPA axis and sleep: Identifying subtypes of major depression. Stress. 2008;11:15–27. doi: 10.1080/10253890701378967. [DOI] [PubMed] [Google Scholar]
- Ashman S, Dawson G, Panagiotides H, Yamada E, Wilkinson C. Stress hormone levels of children of depressed mothers. Dev. Psychopathol. 2002;14:333–349. doi: 10.1017/s0954579402002080. [DOI] [PubMed] [Google Scholar]
- Badanes LS, Watamura SE, Hankin BL. Hypocortisolism as a potential marker of allostatic load in children: Associations with family risk and internalizing disorders. Dev. Psychopathol. 2011;23:881–896. doi: 10.1017/S095457941100037X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birmaher B, Dahl RE, Perel J, Williamson DE, Nelson B, Stull S, Kaufman J, waterman GS, Rao U, Nguyen N, Puig-Antich J, Ryan ND. Corticotropin-releasing hormone challenge in prepubertal major depression. Biol. Psychiatry. 1996;39:267–277. doi: 10.1016/0006-3223(95)00177-8. [DOI] [PubMed] [Google Scholar]
- Birnie KA, Petter M, Boerner KE, Noel M, Chambers CT. Contemporary use of the cold pressor task in pediatric pain research: A systematic review of methods. J. Pain. 2012;13:817–826. doi: 10.1016/j.jpain.2012.06.005. [DOI] [PubMed] [Google Scholar]
- Biro FM, Huang B, Daniels SR, Lucky AW. Pubarche as well as thelarche may be a marker for the onset of puberty. J. Pediatr. Adolesc. Gynecol. 2008;21:323–328. doi: 10.1016/j.jpag.2007.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Booij SH, Bouma EM, de Jonge P, Ormel J, Oldehinkel AJ. Chronicity of depressive problems and the cortisol response to psychosocial stress in adolescents: The TRAILS study. Psychoneuroendocrinology. 2013;38:659–666. doi: 10.1016/j.psyneuen.2012.08.004. [DOI] [PubMed] [Google Scholar]
- Bremmer MA, Deeg DJ, Beekman AT, Penninx BW, Lips P, Hoogendijk WJ. Major depression in late life is associated with both hypo- and hypercortisolemia. Biol. Psychiatry. 2007;62:479–486. doi: 10.1016/j.biopsych.2006.11.033. [DOI] [PubMed] [Google Scholar]
- Brun Sundblad GM, Saartok T, Engström LM. Prevalence and co-occurrence of self-rated pain and perceived health in school-children: Age and gender differences. Eur. J. Pain. 2007;11:171–180. doi: 10.1016/j.ejpain.2006.02.006. [DOI] [PubMed] [Google Scholar]
- Casey BJ, Jones RM, Hare TA. The adolescent brain. Ann. N. Y. Acad. Sci. 2008;1124:111–126. doi: 10.1196/annals.1440.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicchetti D, Rogosch FA. The impact of child maltreatment and psychopathology on neuroendocrine functioning. Dev. Psychopathol. 2001;13:783–804. [PubMed] [Google Scholar]
- Cohen J, Cohen P. Applied Multiple Regression/correlation Analysis for the Behavioral Sciences: Correlation Analysis for the Behavioral Sciences. Lawrence Erlbaum; 1983. [Google Scholar]
- Dixon KE, Thorn BE, Ward L. An evaluation of sex differences in psychological and physiological responses to experimentally-induced pain: A path analytic description. Pain. 2004;112:188–196. doi: 10.1016/j.pain.2004.08.017. [DOI] [PubMed] [Google Scholar]
- Egger HL, Costello EJ, Erkanli A, Angold A. Somatic complaints and psychopathology in children and adolescents: Stomach aches, musculoskeletal pains, and headaches. J Am. Acad. Child. Adolesc. Psychiatry. 1999;38:852–860. doi: 10.1097/00004583-199907000-00015. [DOI] [PubMed] [Google Scholar]
- Fries E, Hesse J, Hellhammer J, Hellhammer DH. A new view on hypocortisolism. Psychoneuroendocrinology. 2005;30:1010–1016. doi: 10.1016/j.psyneuen.2005.04.006. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Horwood L, Ridder EM, Beautrais AL. Subthreshold depression in adolescence and mental health outcomes in adulthood. Arch. Gen. Psychiatry. 2005;62:66–72. doi: 10.1001/archpsyc.62.1.66. [DOI] [PubMed] [Google Scholar]
- Gadow KD, Sprafkin J. Child Symptom Inventory. Stony Brook, NY: State University of New York at Stony Brook; 1996. [Google Scholar]
- Gonzalez-Tejera G, Canino G, Ramirez R, Chavez L, Shrout P, Bird H, et al. Examining minor and major depression in adolescents. J. Child Psychol. Psychiatry. 2005;46:888–899. doi: 10.1111/j.1469-7610.2005.00370.x. [DOI] [PubMed] [Google Scholar]
- Gump BB, Stewart P, Reihman J, Lonky E, Darvill T, Parsons PJ, Granger DA. Low-level prenatal and postnatal blood lead exposure and adrenocortical responses to acute stress in children. Environ. Health Perspect. 2008;116:249–255. doi: 10.1289/ehp.10391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gur A, Cevik R, Sarac AJ, Colpan L, Em S. Hypothalamic-pituitary-gonadal axis and cortisol in young women with primary fibromyalgia: the potential roles of depression, fatigue, and sleep disturbance in the occurrence of hypocortisolism. Ann. Rheum. Dis. 2004;63:1504–1506. doi: 10.1136/ard.2003.014969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hellhammer J, Schlotz W, Stone AA, Pirke KM, Hellhammer D. Allostatic load, perceived stress, and health: a prospective study in two age groups. Ann. N. Y. Acad. Sci. 2004;1032:8–13. doi: 10.1196/annals.1314.002. [DOI] [PubMed] [Google Scholar]
- Judd LL, Akiskal HS, Maser JD, Zeller PJ, Endicott J, Coryell W, Paulus MP, Kunovac JL, Leon AC, Mueller TI, Rice JA, Keller MB. A prospective 12-year study of subsyndromal and syndromal depressive symptoms in unipolar major depressive disorders. Arch. Gen. Psychiatry. 1998;55:694–700. doi: 10.1001/archpsyc.55.8.694. [DOI] [PubMed] [Google Scholar]
- Kaufman J, Martin A, King RA, Charney D. Are child-, adolescent-, and adult-onset depression one and the same disorder? Biol. Psychiatry. 2001;49:980–1001. doi: 10.1016/s0006-3223(01)01127-1. [DOI] [PubMed] [Google Scholar]
- Kaufman J, Birmaher B, Brent DA, Rao U, Flynn C, Moreci P, Williamson D, Ryan N. Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version K-SADS-PL): Initial Reliability and Validity Data. J Am. Acad. Child. Adolesc. Psychiatry. 1997;36:980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- Keenan K, Hipwell AE. Preadolescent clues to understanding depression in girls. Clin. Child Fam. Psychol. Rev. 2005;8:89–105. doi: 10.1007/s10567-005-4750-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keenan K, Hipwell AE, Chung T, Stepp S, Loeber R, Stouthamer-Loeber M, McTigue K. The Pittsburgh Girls Studies: Overview and initial findings. J. Clin. Child Adolesc. Psychol. 2010;39:506–521. doi: 10.1080/15374416.2010.486320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keenan K, Hipwell AE, Feng X, Hinze AE, Babinski DE, Henneberger A, Rischall M. Subthreshold symptoms of depression in girls are stable and predictive of depressive disorders. J Am. Acad. Child. Adolesc. Psychiatry. 2008;47:1433–1442. doi: 10.1097/CHI.0b013e3181886eab. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Avenevoli S, Merikangas KR. Mood disorders in children and adolescents: An epidemiologic perspective. Biol. Psychiatry. 2001;49:1002–1014. doi: 10.1016/s0006-3223(01)01129-5. [DOI] [PubMed] [Google Scholar]
- LeResche L, Mancl LA, Drangsholt MT, Saunders K, Von Korff M. Relationship of pain and symptoms to pubertal development in adolescents. Pain. 2005;118:201–209. doi: 10.1016/j.pain.2005.08.011. [DOI] [PubMed] [Google Scholar]
- McCormick CM, Mathews IZ, Thomas C, Waters P. Investigations of HPA function and the enduring consequences of stressors in adolescence in animal models. Brain Cogn. 2010;72:73–85. doi: 10.1016/j.bandc.2009.06.003. [DOI] [PubMed] [Google Scholar]
- Mathews IZ, Wilton A, Styles A, McCormick CM. Increased depressive behaviour in females and heightened corticosterone release in males to swim stress after adolescent social stress in rats. Behav. Brain Res. 2008;26:33–40. doi: 10.1016/j.bbr.2008.02.004. [DOI] [PubMed] [Google Scholar]
- Morris NM, Udry JR. Validation of a self-administered instrument to assess stage of adolescent development. J. Youth Adolesc. 1980;9:271–280. doi: 10.1007/BF02088471. [DOI] [PubMed] [Google Scholar]
- Pariante CM, Lightman SL. The HPA axis in major depression: Classical theories and new developments. Trends Neurosci. 2008;31:464–468. doi: 10.1016/j.tins.2008.06.006. [DOI] [PubMed] [Google Scholar]
- Platje E, Vermeiren RR, Branje SJ, Doreleijers TA, Meeus WH, Koot HM, Frijns T, van Lier PA, Jansen LM. Long-term stability of the cortisol awakening response over adolescence. Psychoneuroendocrinology. 2013;38:271–280. doi: 10.1016/j.psyneuen.2012.06.007. [DOI] [PubMed] [Google Scholar]
- Plotsky PM, Owens MJ, Nemeroff CB. Psychoneuroendocrinology of depression: hypothalamic-pituitary-adrenal axis. Psychiatr. Clin. North Am. 1998;21:293–307. doi: 10.1016/s0193-953x(05)70006-x. [DOI] [PubMed] [Google Scholar]
- Pruessner JC, Kirschbaum C, Meinlschmid G, Hellhammer DH. Two formulas for computation of the area under the curve represent measures of total hormone concentration versus time-dependent change. Psychoneuroendocrinology. 2003;28:916–931. doi: 10.1016/s0306-4530(02)00108-7. [DOI] [PubMed] [Google Scholar]
- Puig-Antich J, Dahl R, Ryan N, Novacenko H, Goetz D, Goetz R, Twomey J, Klepper T. Cortisol secretion in prepubertal children with major depressive disorder. Episode and recovery. Arch. Gen. Psychiatry. 1989;46:801–809. doi: 10.1001/archpsyc.1989.01810090043008. [DOI] [PubMed] [Google Scholar]
- Rao U, Hammen C, Ortiz LR, Chen LA, Poland RE. Effects of early and recent adverse experiences on adrenal response to psychosocial stress in depressed adolescents. Biol. Psychiatry. 2008;64:521–526. doi: 10.1016/j.biopsych.2008.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romeo RD, Lee SJ, McEwen BS. Differential stress reactivity in intact and ovariectomized prepubertal and adult female rats. Neuroendocrinology. 2004;80:387–393. doi: 10.1159/000084203. [DOI] [PubMed] [Google Scholar]
- Ruttle PL, Shirtcliff EA, Serbin LA, Fisher DB, Stack DM, Schwartzman AE. Disentangling psychobiological mechanisms underlying internalizing and externalizing behaviors in youth: longitudinal and concurrent associations with cortisol. Horm. Behav. 2011;59:123–132. doi: 10.1016/j.yhbeh.2010.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulz KM, Molenda-Figueira HA, Sisk CL. Back to the future: The organizational-activational hypothesis adapted to puberty and adolescence. Horm. Behav. 2009;55:597–604. doi: 10.1016/j.yhbeh.2009.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slotten HA, Kalinichev M, Hagan JJ, Marsden CA, Fone KC. Long-lasting changes in behavioural and neuroendocrine indices in the rat following neonatal maternal separation: Gender-dependent effects. Brain Res. 2006;1097:123–132. doi: 10.1016/j.brainres.2006.04.066. [DOI] [PubMed] [Google Scholar]
- Shirtcliff EA, Allison AL, Armstrong JM, Slattery MJ, Kalin NH, Essex MJ. Longitudinal stability and developmental properties of salivary cortisol levels and circadian rhythms from childhood to adolescence. Dev. Psychobiol. 2012;54:493–502. doi: 10.1002/dev.20607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sisk CL, Zehr JL. Pubertal hormones organize the adolescent brain and behavior. Front. Neuroendocrinol. 2005;26:163–167. doi: 10.1016/j.yfrne.2005.10.003. [DOI] [PubMed] [Google Scholar]
- Son SE, Kirchner JT. Depression in children and adolescents. Am. Fam. Physician. 2000;62:2297–2308. 2311–2. [PubMed] [Google Scholar]
- Sontag-Padilla LM, Dorn LD, Tissot A, Susman EJ, Beers SR, Rose SR. Executive functioning, cortisol reactivity, and symptoms of psychopathology in girls with premature adrenarche. Development and Psychopathology. 2012;24:211–223. doi: 10.1017/S0954579411000782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stroud LR, Papandonatos GD, Williamson DE, Dahl RE. Sex differences in cortisol response to corticotropin releasing hormone challenge over puberty: Pittsburgh Pediatric Neurobehavioral Studies. Psychoneuroendocrinology. 2011;36:1226–1238. doi: 10.1016/j.psyneuen.2011.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van den Bergh BR, Van Calster B. Diurnal cortisol profiles and evening cortisol in post-pubertal adolescents scoring high on the Children’s Depression Inventory. Psychoneuroendocrinology. 2009;34:791–794. doi: 10.1016/j.psyneuen.2008.12.008. [DOI] [PubMed] [Google Scholar]
- von Baeyer CL, Piira T, Chambers CT, Trapanotto M, Zeltzer LK. Guidelines for the Cold Pressor Task as an experimental pain stimulus for use with children. J. Pain. 2005;6:218–227. doi: 10.1016/j.jpain.2005.01.349. [DOI] [PubMed] [Google Scholar]
- Yoshihara T, Yawaka Y. Repeated immobilization stress in the early postnatal period increases stress response in adult rats. Physiol. Behav. 2008;93:322–326. doi: 10.1016/j.physbeh.2007.09.004. [DOI] [PubMed] [Google Scholar]